Abstract
In a previous study, using differential display reverse transcriptase-PCR (DDRT-PCR) we showed that down-regulation of the PHLDA1 (pleckstrin homology-like domain, family A, member 1; also named TDAG51) mRNA was down-regulated in breast tumors compared with normal breast tissue. The present study was conducted to determine the expression pattern and predictive prognostic value of PHLDA1 in breast cancer. A series of 720 primary invasive breast tumors were examined for PHLDA1 expression. PHLDA1 mRNA expression was determined in 74 breast tumors using quantitative Real Time PCR analysis (qPCR). PHLDA1 protein expression was evaluated by immunohistochemistry (IHC) using Tissue Microarrays (TMA) containing 699 primary invasive breast tumors. Reduced PHLDA1 mRNA expression was identified in 72% (53/74) of the primary breast tumors analyzed. Seventy-three percent (512/699) of cases analyzed showed negative PHLDA1 protein expression. Down-regulation of PHLDA1 protein was a strong predictor of poor prognosis for breast cancer patients. Breast cancer patients with tumors that were negative for PHLDA1 protein expression had shorter disease free survival (P < 0.001) and overall survival (P < 0.001) than patients with tumors that were positive for PHLDA1 protein expression. In addition patients with tumors exhibiting reduced PHLDA1 expression and paucity for ER had the worse outcome (P < 0.001). Multivariate analysis indicated that PHLDA1 protein expression is an independent prognostic factor of patient survival. To our knowledge, the expression pattern of PHLDA1 in breast cancer has not previously been investigated. Our results provide strong evidence that reduced PHLDA1 expression is important in breast cancer progression and could serve as useful prognostic marker of disease outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Invasive breast cancer is one of the leading causes of cancer morbidity and mortality for women worldwide [1]. As for other types of solid tumors, breast cancer development and progression is associated with the accumulation of several genetic and epigenetic alterations resulting in differences in gene expression between tumor and normal cells. Various molecular technologies that allow high throughput analysis of gene expression profiling have been used to identify gene expression changes associated with breast cancer. Interesting results from these studies have shown that differentially expressed genes can be used for classification, disease prognostication and therapeutic response [2, 3, 4]. However, despite of the effort devoted to defining breast cancer molecular profile only few of the differentially expressed genes identified so far have been validate. Currently, the only recommended prognostic and predictive markers in breast cancer are estrogen and progesterone receptors (ER and PR) and the ERBB2/Her 2 oncogene [5].
In a previous study using differential display technique (DDRT-PCR) we identified a set of genes differentially expressed in breast tumors regarding the presence or absence of the ER and PR [6]. In addition, a set of genes that are differentially expressed was also identified between normal and tumor tissues regardless the ER status. Among those genes we identified down-regulation of the PHLDA1 gene transcripts in breast tumors compared with the normal breast tissue. The PHLDA1 (pleckstrin homology-like domain, family A, member 1; also named TDAG51) is located on chromosome 12q15 and encodes a protein of 262 amino acid that is a member of the pleckstrin homology-related domain family [7, 8]. PHLDA1 expression was first associated with restoration of activation-induced apoptosis by coupling T-cell receptor stimulation to Fas expression in T cell hybridoma [7]. In cultured hippocampal neuronal cells, microinjection or transient expression of PHLDA1 enhanced cell death, but without Fas induction [9]. In cultured vascular endothelial cells PHLDA1 expression is induced by homocysteine and other agents including dithiothreitol and tunicamycin and its transient over-expression induced anoikis [10]. On the other hand, IGF-I induces PHLDA1 expression in NIH3T3 cells over-expressing IGF-IR and PHLDA1 siRNA expression abolished the ability of IGF-I to rescue cells from serum starvation-induced apoptosis [11]. Although the exact biochemical and biological function of PHLDA1 is still unknown, its expression is induced by a variety of external stimuli and there is evidence showing that it might act as a mediator of apoptosis.
The present study was performed in an attempt to determine the expression pattern of PHLDA1 in primary breast tumors and to evaluate the contribution of altered PHLDA1 expression to breast cancer progression. To accomplish this, the expression of the PHLDA1 protein was determined in a large series of primary breast tumors by immunohistochemistry (IHC) on tissue microarrays (TMA). We were able to confirm our previous results and provide strong evidence that PHLDA1 down-regulation is a frequent event associated with a more aggressive breast cancer phenotype, and could be considered as useful prognostic marker of the disease.
Material and methods
Tissue samples and patients characteristics
Tissue samples were obtained from 720 breast cancer patients at the Department of Pathology of the Medical and Research Center Hospital do Cancer, São Paulo, Brazil. For total RNA extraction, 74 fresh tumor samples and 20 fresh adjacent normal tissue samples were obtained from 74 breast cancer patients. For TMA construction, formalin-fixed, paraffin-embedded tissue blocks containing invasive breast cancer tissue from 699 patients were retrieved from the archives. All the patients were treated at our institution, and the primary treatment was radical mastectomy, modified radical mastectomy or breast-conserving surgery including axillary lymph node dissection. One hundred sixty-five patients received neoadjuvant chemotherapy. In these cases, IHC was performed on the biopsy sample taken before chemotherapy. None of the patients received radiotherapy before the biopsy/mastectomy procedure. The median age of the patients investigated was 54 years (average 54.61 years, range 28–92 years); 285 patients belonged to the premenopausal group, 411 to the postmenopausal group, and no menopausal information was available for 3 patients. The sizes of the tumors ranged from 0.4 to 16 cm. All tumors were invasive; 662 tumors were of the ductal type, 28 were lobular, 5 were papillary, and 4 were of the mucinous type. The histological grading according to the Nottingham system were G1 (n = 144), G2 (n = 386), G3 (156), and in 13 cases the grade was not assessed. The nuclear grade was G1 (n = 29), G2 (n = 273), G3 (n = 392), and the grade was not assessed in 13 cases. One hundred eighty two patients were node-negative and 514 patients were positive for lymph node metastasis. Lymph node status was not available for 3 patients. Clinical stage was assessed in 663 patients as follow: stage I, 22 patients; stage IIA, 117 patients; IIB, 171 patients; IIIA, 91 patients; IIIB, 232 patients; and IV, 66 patients. Finally, ER status was negative in 356 cases, positive in 308 cases, and not available in 35 patients.
Estrogen and progesterone receptor binding assays were performed by the classical dextran-coated-charcoal method (DCC) as previously described [12].
The Institutional Ethics Committee approved this study and all subjects provided informed consent.
RNA extraction
Tissue specimens were pulverized under liquid nitrogen and total RNA was isolated according to the guanidine isothiocyanate method [13]. The quality of the RNA samples was determined by 1% agarose gel electrophoresis and ethidium bromide staining. All RNA samples were treated with DNaseI for 30 min at 37°C to eliminate genomic DNA contamination.
Differential display analysis and cDNA cloning
The DDRT-PCR technique was performed using the RNAimage kit (GenHunter Corp., Nashiville, TM) following the manufacturer instruction manual. Total RNA from 3 ER-/PR- breast tumors, 3 ER + /PR + breast tumors and the corresponding normal breast tissues of each were pooled and analyzed by DDRT-PCR as previously described [6].
Quantitative real-time PCR (qPCR)
Ten micrograms of total RNA were reverse transcribed using High Capacity cDNA Archive Kit (Applied Biosystems). PCR amplification was performed using an Applied Biosystems PRISM 5700 Sequence Detector, using the Platinum SYBR Green qPCR SuperMix-UDG kit (Invitrogen). PCR reactions were carried out in a total volume of 50 μl according to the manufacturer’s instructions. Experiments were performed in duplicate. The PCR primers used for PHLDA1 were forward primer 5′-CCACATCCACATCCACACTCT-3′ and reverse primer 5′-AGGTGCTGCGGAGAAGCCGGT-3′; and for glyceraldehyde-3-phosphate dehydrogenase (GAPDH), the forward primer was 5′-CCTCCAAAATCAAGTGGGGCG-3′ and the reverse primer was 5′-GGGGCAGAGATGATGACCCTT-3′. The relative expression was calculated by 2−ΔΔCT (CT = fluorescence threshold value; ΔCT = CT of the target gene − CT of the reference gene (GADPH); ΔΔCT = ΔCT of the tumor sample − ΔCT of the reference sample). The average value of two pools, which were composed of 10 normal tissue samples each served as the reference sample.
Tissue array (TMA) construction
For the construction of the breast tissue arrays, a new section was obtained from the representative paraffin donor blocks, stained with H&E, and an area was circled using a permanent marker. The corresponding paraffin block was also marked, and core biopsies were taken using a Tissue Microarrayer (Beecher Instruments ®, Silver Springs, USA). We have constructed three TMA paraffin-blocks, with 256, 246 and 197 cores. Each sample was arrayed once with 1.0-mm diameter core spaced 0.2-mm apart. A map showing the detailed identification of each core was made in an Excel® sheet such that each case was identified with precision.
After cutting the recipient block and transferring the tissue to coated slides with an adhesive tape for subsequent UV cross-linkage (Instrumedics Inc®, Hackensack, NJ), the slides were dipped in a layer of paraffin to prevent oxidation, and kept in a −20°C freezer. The slides were taken from the freezer 24 h before the immunohistochemical procedure.
Immunohistochemistry of TMA
We performed IHC for PHLDA1 using 3 slides (3 cores/case). For the immunohistochemical studies of paraffin-TMAs, 3-μm- thick sections were deparaffinized then rinsed 3 times in a xylene solution for 5 min, 4 times in a solution of absolute methanol for 30 s, then washed with water for 5 min. Slides were placed in 3% hydrogen peroxide 3 times for 5 min, then washed with water for 5 min. Afterwards the slides were incubated for 1 day in a humidified chamber with a 1:100 dilution of the primary antibody. The slides were washed in PBS and subsequently incubated with biotinylated swine antigoat IgG for 20 min, then with streptavidin–biotin peroxidase LSAB + kit (Dako®, Carpinteria, USA) in a humidified chamber. Immunostaining was performed by incubating the slides in diaminobenzidine (Dako) solution containing 1 μl of chromogen for every 50 μl of buffer substrate, for 5 min. After chromogen development, the slides were washed, dehydrated with alcohol and xylene, and mounted with cover slips using a permanent mounting medium. The primary antibody was a goat polyclonal that recognizes the carboxy terminus of PHLDA1 (Santa Cruz Biotech Inc, USA) concentration of 200 μg/ml IgG. The antibody was used at a final working solution of 1:100.
Evaluation of immunohistochemistry
Tissue cores with <50% of the original tissue left on the slides after immunohistochemistry were not used for the scoring of the stains. In cores that remained intact after staining, a semi-quantitative analysis was done by one observer (FAS) who had no knowledge of the clinical and pathological parameters. A case was considered positive if there was cytoplasmic staining for PHLDA1. The immunostainings was graded in relation to the intensity of staining (IS, 0–3) and number of stained cells (NCS, 0–4). The intensity of the staining reaction was divided in two groups (positive and negative) in consideration of the cytoplasmic or nucleari staining: 0 (no signal); 1 (weak); 2 (moderate) and 3 (strong). Number of positive cells: 0 (no cell); 1 (less than 10%); 2 (10–50%); 3 (51–90%) and 4 (more than 90% of cells). A combined final score was obtained by multiplying the number of cells versus the IS. Since we had 3 cores per case, we arrived at a summary score per patient by calculating the mean value. Combined mean scores were considered negative (0–3) or positive (more than 3).
Statistical methods
Analyses of the association between the PHLDA1 levels and the demographic and clinicopathological characteristics of the patients were performed by the Chi-square test. Disease-free survival and overall survival probabilities were calculated based on the Kaplan-Meier method. Cox proportional hazards model was used for multivariate analysis. The significance level was 5% for all the tests. The statistical analyses were performed using SPSS software 13.0 (SPSS Inc., Chicago, IL).
Results
In this study, we analyzed the mRNA expression level of PHLDA1, by quantitative real-time PCR (qPCR), in 74 primary breast tumors. The relative expression of the target gene was determined in n-fold differences relative to the normalized reference samples (2 pools of normal breast tissue samples) using GAPDH as calibrator gene. In the group of breast tumor examined 21 (28%) displayed PHLDA1 mRNA expression levels comparable to normal breast and 53 (72%) showed down-regulation of the PHLDA1 transcripts (more than a 2-fold decrease compared with normal breast tissue) (Fig. 1). We found no statistically significant associations between PHLDA1 mRNA expression and patient characteristics, such as age, clinical stage, tumor size or steroid hormone receptors status.
Expression analysis of the PHLDA1 (pleckstrin homology-like domain, family A, member 1; also named TDAG51) gene in 74 primary breast tumors. The relative expression was determined by qPCR normalized to GAPDH as the reference gene. The height of the bars represents the relative gene expression for individual tumors taking normal breast tissue as calibration samples
PHLDA1 protein expression was assessed by IHC on TMAs containing a panel of 699 breast tumors. IHC was performed using a antibody for the PHLDA1 protein and immunoreactivity scoring was based on the number of tumor cells displaying cytoplasmic PHLDA1 immunostaining (Fig. 2). The IHC results showed that 512 of the 699 cases analyzed (73%) showed negative staining, whereas 187 of the cases (27%) showed positive staining for PHLDA1. Fifty-three of the breast tumors analyzed by qPCR were represented on the TMA. Overall, tumors that were negative for PHLDA1 protein by IHC also showed low levels of PHLDA1 mRNA expression. The results of the analysis of PHLDA1 protein expression by IHC on TMAs containing a large series of breast tumors largely substantiates the real time PCR indicating that loss of PHLDA1 protein expression is a frequent event in breast cancer.
Expression of PHLDA1 protein in breast tumors studied by immnohistochemistry (IHC) on tissue microarrays (TMAs). Representative TMA elements stained with antibody to PHLDA1. Examples of negative staining (panels A/B, original magnification 40x and 400x respectively) and positive staining (panels C/D, original magnification 40× and 400× respectively)
In order to evaluate the potential contribution of PHLDA1 protein expression to the development and progression of breast cancer, the clinicopathological characteristics of the cases showing negative citoplasmic staining for PHLDA1 were compared with those exhibiting positive staining. PHLDA1 protein expression was significantly correlated with higher nuclear grade (P = 0.03). There was no significant correlation between PHLDA1 protein expression and the menopausal status of the patients (P = 0.93), clinical stage (P = 0.08), nodal status (P = 0.40) or ER status (0.36) (Table 1).
The impact of PHLDA1 down-regulation on patient’s survival was estimated by Kaplan–Meier analysis. Breast cancer patients with tumors showing reduced PHLDA1 protein expression had a significantly worse prognosis than those with tumors positive for PHLDA1 protein expression. As shown in Fig. 3, significant differences among survival curves by log-rank test were observed for both disease free survival (Fig. 3A, P < 0.001) and overall survival (Fig. 3B, P < 0.001).
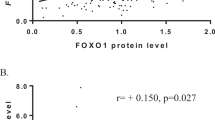
Univariate analysis revealed a significant correlation between advanced clinical stage (P < 0.001), lymph nodes involvement (P < 0.001), nuclear grade (P < 0.001), PHLDA1 protein down-regulation (P < 0.001) and overall survival at 5 years (Table 2). Further multivariate analysis based on Cox proportional hazard’s model revealed that clinical stage (HR, 2.8; 95% CI, 2.1–3.6), lymph nodal status (HR, 1.5; 95% CI, 1.1–2.1), and PHLDA1 protein expression (HR, 2.2; 95% CI, 1.6–3.0) were independent prognostic factors for the overall survival outcome of breast cancer patients (Table 3). When we combined the PHLDA1 and ER expression statuses for the comparison, tumors showing PHLDA1 down-regulation and paucity for ER had an unfavorable outcome (Table 4; Fig. 4).
Kaplan–Meier curves for long-term overall survival in breast cancer patients, stratified according to PHLDA1 protein expression and ER status. Tumors were classified in four categories according to the protein immunostaining of PHLDA1 and ER status: PHLDA1−/ER−; PHLDA1−/ER+; PHLDA1+/ER−; PHLDA1+/ER+
Discussion
To our knowledge no previous study has investigated the expression pattern of PHLDA1 in breast cancer. In the present study which, examined the PHLDA1 mRNA and protein expression in a larger series of primary breast tumors, we confirmed our previous DDRT-PCR results and provide strong evidence that PHLDA1 expression is frequently down-regulated in primary breast tumors and has a predictive prognostic value.
Our study demonstrated that PHLDA1 correlate independently with overall survival in patients with breast carcinomas. The only other independent predictors were clinical stage and lymph node status. Consistent with our DDRT-PCR results no associations were found between PHLDA1 protein expression and ER positivity in the group of primary breast tumors analyzed. However, when the expression level of PHLDA1 and ER status were combined, a striking statistically significant correlation with survival was observed. Patients with tumors showing loss of PHLDA1 expression and paucity for ER had the worst outcome. Interestingly, patients with ER-negative breast tumors expressing PHLDA1 showed a more favorable outcome than patients with ER-positive breast tumors positive for PHLDA1 protein expression. The underlying biological events leading to the more indolent clinical behavior of ER-negative breast tumors are no doubt complex, and demand further investigation.
PHLDA1 expression has been associated with increased susceptibility to apoptosis in T cell hybridomas, neuronal and melanoma cells [7, 9, 14]. Hardy et al. (2005) provided evidence that PHLDA1 expression may prime primary human mammary fibroblasts for apoptosis during senescence [15]. Apoptosis plays a critical role during ductal mammary development, maintenance and involution after lactation and its impaired control plays a critical role in breast cancer development and progression [16]. However, the mechanisms or genes associated with the subversion of apoptosis during breast cell malignant transformation are still poorly understood. The mammary morphogenesis and maintenance requires a complex interplay of the cells with the BM basement membrane (BM) and extra-cellular matrix (ECM) that provides a complex network of signals such as hormones and growth factors [17]. Vascular endothelial cells over-expressing PHLDA1 display changes in cell morphology, decreased cell adhesion and detachment-induced apoptosis (anoikis) [10]. Anoikis is the process observed during mammary morphogenesis to the terminal endbud formation and mammary gland involution after lactation, that may occur due to the loss of cell-BM and cell-ECM interactions [16]. It is possible that PHLDA1 could be involved in this process, however, without functional studies related to PHLDA1 expression in normal or breast cancer cells, we can only speculate that PHLDA1 may play a role in the mammary gland morphogenesis, priming cells for apoptosis during endbud formation and involution, and that its down-regulation could play a role in malignant transformation of the breast.
Down-regulation of PHLDA1 protein expression was consistently associated with increased risk of death and was observed in 80% of the early stage breast carcinomas analyzed. Although this data requires further validation in a larger series of early stage breast carcinomas it is relevant and indicates that changes in PHLDA1 expression is a signal for a biologically aggressive phenotype that occurs relatively early in the tumorigenic process of the breast. There is limited information available in the literature concerning the role of PHLDA1 in cancer. Loss of PHLDA1 expression has been associated with the progression of malignant melanomas and constitutive PHLDA1 expression in melanoma cells was associated with increased sensitivity to apoptosis induced by exposure to doxorubicin and camptothecin [14] suggesting that loss of PHLDA1 expression may confer a proliferative advantage and apoptosis resistance that contribute to the tumorigenic process. However, an in vivo study showed that PHLDA1−/− mice are healthy and show no gross developmental abnormalities [18]. In spite of that, of particular interest is that PHLDA1 has been shown to act as a cell death mediator that does not directly trigger apoptosis, but rather sensitizes cells to apoptosis [7, 14, 15]. Therefore, changes in PHLDA1 expression may lead to the disruption of cell survival signaling, which could play a role in tumor development and progression and chemotherapeutic drug sensitivity.
In the present study, the application of TMA technology allowed us to define the expression pattern and clinical relevance of the PHLDA1 in breast cancer. Although further experimental studies are needed to better understand the role of PHLDA1 in normal mammary gland and breast cancer, our data suggest that PHLDA1 could serve as a useful tool to better define the prognosis and directed therapeutic intervention in breast cancer.
References
Boyle P (2005) Breast cancer control: signs of progress, but more work required. Breast 14(6):429–438
Van ‘t Veer LJ, Dai H, et al (2002) Gene expression profiling predicts clinical outcome of breast cancer. Nature 415(6871):530–536
Rouzier R, Perou CM, Symmans WF et al (2005) Breast cancer molecular subtypes respond differently to preoperative chemotherapy. Clin Cancer Res 15:11(16):5678–5685
Folgueira MA, Carraro DM, Brentani H et al (2005) Gene expression profile associated with response to doxorubicin-based therapy in breast cancer. Clin Cancer Res 11(20):7434–7443
Duffy MJ (2005) Predictive markers in breast and other cancers: a review. Clin Chem 51(3):494–503
Nagai MA, Ros N, Bessa SA et al (2003) Differentially expressed genes and estrogen receptor status in breast cancer. Int J Oncol 23(5):1425–1430
Park CG, Lee SY, Kandala G et al (1996) A novel gene product that couples TCR signaling to Fas(CD95) expression in activation-induced cell death. Immunity 4(6):583–591
Kuske MD, Johnson JP (2000) Assignment of the human PHLDA1 gene to chromosome 12q15 by radiation hybrid mapping. Cytogenet Cell Genet 89(1–2):1
Gomes I, Xiong W, Miki T et al (1999) A proline- and glutamine-rich protein promotes apoptosis in neuronal cells. J Neurochem 73(2):612–622
Hossain GS, van Thienen JV, Werstuck GH et al (2003) TDAG51 is induced by homocysteine, promotes detachment-mediated programmed cell death, and contributes to the development of atherosclerosis in hyperhomocysteinemia. J Biol Chem 278(32):30317–30327
Toyoshima Y, Karas M, Yakar S et al (2004) TDAG51 mediates the effects of insulin-like growth factor I (IGF-I) on cell survival. J Biol Chem 279(24):25898–25904
Brentani MM, Nagai MA, Fujyama CT et al (1981) Steroid receptors in a group of Brazilian breast cancer patients. J Surg Oncology 18:431–439
Chomczynski P, Sacchi N (1987) Single-step method of RNA isolation by acid guanidinium thiocyanate-phenol-chloroform extraction. Anal Biochem 162:156–159
Neef R, Kuske MA, Prols E et al (2002) Identification of the human PHLDA1/TDAG51 gene: down-regulation in metastatic melanoma contributes to apoptosis resistance and growth deregulation. Cancer Res 62(20):5920–5929
Hardy K, Mansfield L, Mackay A et al (2005) Transcriptional networks and cellular senescence in human mammary fibroblasts. Mol Biol Cell 16(2):943–953
Green KA, Streuli CH (2004) Apoptosis regulation in the mammary gland. Cell Mol Life Sci 61(15):1867–1883
Fata JE, Werb Z, Bissell MJ (2004) Regulation of mammary gland branching morphogenesis by the extracellular matrix and its remodeling enzymes. Breast Cancer Res 6(1):1–11
Rho J, Gong S, Kim N et al (2001) TDAG51 is not essential for Fas/CD95 regulation and apoptosis in vivo. Mol Cell Biol 21(24):8365–8370
Acknowledgment
This work was supported by grants 03/13170–0 and 04/04607–8 from FAPESP.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nagai, M.A., Fregnani, J.H.T.G., Netto, M.M. et al. Down-regulation of PHLDA1 gene expression is associated with breast cancer progression. Breast Cancer Res Treat 106, 49–56 (2007). https://doi.org/10.1007/s10549-006-9475-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-006-9475-6