Abstract
Background
Botanical therapies are often used by breast cancer patients yet few clinical trials have evaluated their safety and efficacy. We studied mechanisms of activity and performed a phase I clinical trial in patients with advanced breast cancer to evaluate BZL101, an aqueous extract from Scutellaria barbata.
Methods
Preclinical studies were conducted in vitro to characterize cell death induced by BZL101. In a phase I trial, eligible patients had histologically confirmed, measurable metastatic breast cancer. Treatment consisted of 350 ml per day of oral BZL101, administered as sole cancer therapy until disease progression, toxicity or personal preference to discontinue. Primary endpoints were safety, toxicity and tumor response.
Results
BZL101 extract induced strong growth inhibition and apoptosis of breast cancer cell lines. In the phase I trial, 21 patients received BZL101. Mean age was 54 years (30–77) and mean number of prior treatments for metastatic disease was 3.9 (0–10). There were no grade III or IV adverse events (AEs). The most frequently reported BZL101-related grade I and II AEs included: nausea (38%), diarrhea (24%), headache (19%) flatulence (14%), vomiting (10%), constipation (10%), and fatigue (10%). Sixteen patients were evaluable for response. Four patients had stable disease (SD) for >90 days (25%) and 3/16 had SD for >180 days (19%). Five patients had objective tumor regression, one of which was 1 mm short of a PR based on RECIST criteria.
Conclusions
BZL 101 inhibits breast cancer cell lines by inducing apoptosis. In a phase I clinical trial, BZL101 was safe and had a favorable toxicity profile. BZL101 demonstrated encouraging clinical activity in this heavily pretreated population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
While advances in early detection and adjuvant therapy for breast cancer have had a favorable impact on survival, locally advanced or metastatic breast cancer remains incurable. Commonly used hormonal and chemotherapeutic agents can lead to transient regression of tumors and palliate symptoms related to cancer. However, these treatments are often accompanied by significant toxicities and eventually become ineffective in controlling advanced stage breast cancer and its symptoms. Improvements in survival are modest even with newer targeted biological agents that are also associated with toxicities. To this end, novel therapies with minimal toxicities are clearly needed, and initial testing in advanced disease can improve available options for this population.
More than 60% of all chemotherapeutic agents used in the treatment of breast cancer are derived from natural substances [1]. Although the development of taxanes from the Pacific yew tree, Taxus brevifolia is fairly recent, interest in botanicals as a source of drug development has fallen. Throughout the world, it is estimated that approximately 80% of the world population still rely on botanical medicine as their primary source of therapy [2]. In the West, botanical medicine is considered a popular form of complementary and alternative medicine among individuals diagnosed with cancer [3]. Biological effects of single natural or synthetic compounds may differ considerably from the effects of an array of substances found in botanical extracts. Few clinical trials have been conducted to firmly assess the safety and efficacy of botanical agents for the treatment of breast cancer despite numerous documented anecdotal case reports of clinical and symptomatic efficacy in women who have relied solely on botanical medicine for treatment [4].
BZL101 is an aqueous extract of the aerial part of Scutellaria barbata (Chinese pin yin transliteration-Ban Zhi Lian). The plant is grown mainly in areas southeast of the Yellow River and is harvested in late summer and early autumn after it blooms. The aerial part is cut from the root and used for BZL101. The herb is identified through botanical, morphological and chemical characteristics to ensure purity and consistency. The active ingredients in BZL101 are unknown but several bioactive chemical compounds in the plant have been identified including scutellarin, scutelarein, carthamidin, isocarthamidin and wagonin [5].
We have previously shown that an aqueous extract of Scutellaria Barbata results in >50% growth inhibition in four of five breast cancer cell lines evaluated in vitro [6]. BZL101 at the same dose did not cause >50% growth inhibition of normal human mammary epithelial cells (HuMEC) or normal human fibroblasts [7]. BZL101 was active orally in preventing tumor formation in a mouse xenograft model (unpublished data). We describe here the preclinical data evaluating mechanism of action and the results of a Phase I clinical trial of BZL101.
Methods
In vitro methods
For the analysis of cell cycle and DNA fragmentation cells were collected with trypsin, washed, fixed in cold 70% ethanol and kept at 4°C. Prior to analysis, cells were pelleted, washed in PBS and resuspended in PBS containing 20 μg/ml propidium iodide (PI) and 20 μg/ml DNase free RNAse. After at least 20 min incubation at room temperature, cells were analyzed on a Becton Dickinson FACScan using CellQuest software. Human breast cancer (BT474, Du4475, MDA MB 231, MDA MB 361, MDA MB 435, MDA MB 453, MDA MB 468, MCF7, and SKBR3) and normal fibroblast (IMR90) cell lines were used.
Apoptotic cell death was distinguished from necrotic death through staining with Annexin V-Alexa Fluor 488 (Molecular Probes) as described in the manufacturer manual. Cells were analyzed on FACScan immediately after staining. Only cells that bound Annexin V conjugate, but did not take up PI, were considered to be apoptotic.
Mitochondrial transmembrane potential (MTP) in live cells was analyzed using the potential-sensitive cationic dye JC-1 (Molecular Probes) by adding 2 μM JC-1 to the growth media for 30 min. Cells were washed and the ratio of red fluorescence to green fluorescence was determined on FACScan or fluorescence plate reader. Carbonyl cyanide 3-chlorophenylhydrazone (CCCP) at 50 μM was used as a positive control for the disruption of MTP.
Generation of the reactive oxygen species (ROS) in cells incubated with BZL101 was detected by incubation of cells in the growth medium with 10 μM of hydroethidine for 30 min. Cells were washed and analyzed for increase in red fluorescence on FACScan or fluorescence plate reader.
Caspase activity in treated cells was analyzed using the Vibrant FAM Caspase Assay kit (InVitrogen) according to manufacturer’s manual. Cells were stained with FAM-VAD-FMK reagent that specifically binds to activated caspases -1, −3, −4, −5, −6, −7, −8 and −9. After counterstaining with PI to detect dead cells, cells were analyzed on FACscan.
Patients and phase I study design
Patients were enrolled at the University of California, San Francisco Carol Franc Buck Breast Care Center and the Cancer Research Network in Plantation, Florida between August 2001 and November 2004. All patients signed an informed consent approved by the local institutional review board and were ≥18-years-old with a histologically confirmed diagnosis of breast cancer and clinical evidence of locally advanced or metastatic disease. Patients with solitary metastases required biopsy confirmation of metastatic disease. All patients had adequate time to recover sufficiently from the toxicities associated with prior anticancer treatments. A life expectancy of 6 months and Karnofsky performance score of 80% or better were required. Nutritional or up to five times recommended daily allowance (RDA) vitamin supplementation was permitted but concomitant use of non-study herbal agents was not allowed. Patients were excluded from the study for the following: extensive liver involvement (>50% of liver parenchyma), lymphangitic pulmonary involvement, central nervous system involvement or spinal cord compression not stabilized by therapy for >3 months, a history of multiple or severe food or medicine allergies and organ or marrow dysfunction as defined by creatinine >2.0 mg/dl, total bilirubin >1.7 mg/dl, white blood cell count <2,500 cells/mcl and platelet count <75,000 mm3.
Safety monitoring was done on a continuous basis and patients were seen for a clinical examination at study start and then every 4 weeks until treatment was discontinued. Adverse events were graded using National Cancer Institute, Common Toxicity Criteria, Version 2, assigned a category by organ system and coded in relation to study drug as remotely, possibly, probably or definitely related. Baseline tumor assessments were done within 14 days of initiation of study drug and then every 3 months. Response was assessed using Response Evaluation Criteria in Solid Tumors (RECIST) criteria [8]. Responses were categorized as not-evaluable (NE), progressive disease (PD), stable disease (SD), partial remission (PR), complete remission (CR) and minimal response (MR). Any decrease in measurable tumor diameter that was >0% and <30% was categorized as a minimal response. Study drug was distributed and compliance was assessed with patient logs at each clinic visit. BZL101 was packaged as a liquid extract in a sealed and labeled aluminum can. Daily treatment with BZL101 was administered until determination of tumor progression, dose limiting toxicity was encountered or the patient decided to voluntarily discontinue, in which case, the reason for discontinuation was obtained.
Statistical analysis
Prior to data analysis, a comprehensive descriptive and exploratory examination was conducted to identify gross errors and potential outliers, and describe the distribution of the variables in the study sample, both overall and with respect to several key variables. Means, medians, ranges, and standard deviations for continuous variables, and frequency distributions for categorical variables were calculated for the entire sample and within sub-samples of interest (e.g., by symptoms).
To determine whether there were differences between baseline and monthly measures, repeated measure analysis of variance using the general linear model was applied [9]. Differences between means for continuous variables were compared with t-tests, either within (dependent) or between (independent) groups.
To examine the distribution of times between two events in the presence of censored cases (cases for which the second event has not been recorded), the Kaplan–Meier procedure was used. The Kaplan–Meier model is based on estimating conditional probabilities at each time point when an event occurs and taking the product limit of those probabilities to estimate the “survival rate” at each point in time [10].
Study medication
A single dose of BZL101 is made through the following procedure under FDA IND #59,521 (Bionovo, Inc., Emeryville, CA):
-
(a)
180 g of the raw herb is ground to a fine powder,
-
(b)
the powder is mixed with 1800 ml of distilled water,
-
(c)
it is simmered at 70-72°C for 60 min,
-
(d)
the extract is decanted and filtered through 22 μ filter,
-
(e)
the supernatant weight after extraction is 168 gm,
-
(f)
the volume of the filtered solution is 1750 ml,
-
(g)
the extract is concentrated with a vacuum evaporator to reduce the volume of water to 350 ml which constitutes a 5:1 concentration of the original solution (dry weight 12 g),
-
(h)
it is packaged in a sterile, vacuum sealed aluminum can, and
-
(i)
the final extract is tested for bacteria, yeast and heavy metals by an accredited laboratory.
Results
Analysis of the effects of BZL101 on tumor cells
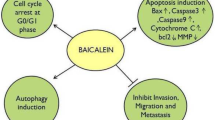
Treatment of breast cancer cell lines with BZL101 leads to dramatic growth inhibition [6, 7]. Preliminary results indicated that this inhibition results from induction of cell death. We have analyzed several parameters of cell death induced by BZL101 in order to understand if this death is apoptotic in character.
One of the hallmarks of apoptosis is the fragmentation of chromosomal DNA which can be detected by analysis of DNA content in ethanol fixed cells that lose small DNA fragments and are, therefore, seen as cells with reduced (<2n) amount of DNA. DNA fragmentation after BZL101 treatment was observed in seven out of nine breast cancer cell lines analyzed, though the percentage of cells with fragmented DNA varied between the cell lines (Table 1 and Fig. 1A). No correlation was observed between the degree of DNA fragmentation and the amplification status of HER2 receptor (Table 1). We have also noticed that BZL101 induces a G2/M delay or arrest in two of the breast cancer lines analyzed, MDA MB 468 cells (Fig. 1B) and BT474 cells (not shown), but not in other cell lines examined. Significantly, BZL101 did not induce DNA fragmentation in normal human fibroblasts IMR90 (Fig. 1A and B).
Induction of DNA fragmentation and G2/M arrest in breast cancer cells by BZL101. (A) Cells were treated with BZL101 at 1:100 dilution with indicated number of days. Percentage of cells with DNA content less than 2n was analyzed by flow cytometry of ethanol fixed, PI-stained cells. (B) DNA content histograms of cells treated as in A. Numbers in the histograms show percentage of cells in G1 and G2/M phases of cell cycle, respectively
To ascertain that at least some of the cell death induced by BZL101 could be attributed to an apoptotic process, we examined if treatment with BZL101 induces translocation of phosphatidylserine to the outer membranes of cells, a process known to occur specifically in early apoptotic cells. Staining of cells treated with BZL101 revealed an accumulation of Annexin V positive cell populations among both live and dead cells. Figure 2A and B show percentage of Annexin V positive cells that do not uptake propidium iodide, consistent with early apoptotic cells. Binding of Annexin V to the cell surface increased with the time of incubation with BZL101 (Fig. 2B). Percentage of Annexin binding cells did not exceed 5% in IMR90 cells after treatment with BZL101 even after 3 days with the extract (data not shown).
Induction of apoptosis and caspase activation in breast cancer cells by BZL101. (A) Flow cytometric analysis of MDA MD 468 cells treated with BZL101 for Annexin V binding. (B) Cells were treated with BZL101 for times indicated. Percentage of cells binding Annexin V was analyzed by flow cytometry as shown in A. Only cells negative for propidium iodide staining (i. e., live cells) were gated for analysis. (C) Percentages of cells with activated caspases as quantified by specific binding of fluorescent caspase inhibitor VAD-FMK
We also evaluated if BZL101 treated cells exhibit yet another hallmark of apoptosis, activation of caspases. Figure 2C shows that a small percentage of cells from treated cell lines contained activated caspases as detected by staining with VAD-FMK. Caspase activation was not seen in the normal IMR90 cells treated with BZL101 (data not shown). The low number of cells with evidence of caspase activation correlates with the observation of minimal cleavage of the caspase substrate PARP-1 in BZL101-treated cells (not shown) even though there was a significant cell death at the time of analysis.
Potential effects of BZL101 on mitochondrial transmembrane potential (MTP) were examined using cationic dye JC-1. JC-1 exhibits potential-dependent accumulation in mitochondria, where it forms red fluorescent J-aggregates. In cells where mitochondria are depolarized, as often occurs during apoptosis, a shift from red (FL2) to green (FL1) fluorescence of JC-1 takes place. This is indicated by a reduction in the FL2/FL1 ratio.
We examined the effect of BZL101 on MTP. As shown in Fig. 3A, BZL101 induced strong, dose-dependent depolarization of mitochondria in SKBr3 cells as well as in all four other breast cancer cell lines tested (BT474, Du4475, MDA MB 231 and MDA MB 468) in a dose-dependent manner (not shown). Loss of MTP occurred within 1 h of addition of BZL101 to the culture medium; if BZL101 was washed away after several hours of incubation, the low MTP persisted for up to 6 h (data not shown).
Disruption of mitochondrial transmembrane potential (MTP) and induction of reactive oxygen species by BZL101. (A) SKBr3 cells on a 96 well plate were treated with indicated dilutions of BZL101 for three hours. JC-1 was added to the media for the last 20 min of incubation. Cells were washed; retained red (FL2) and green (FL1) fluorescence were analyzed on fluorescence plate reader. Data are represented as ratios of FL2 to FL1 where the ratio in untreated (UT) cells is assigned a value of 1. CCCP is a known disruptor of MTP and was used as a positive control for shift in JC1 emission. It was added to untreated cells simultaneously with JC-1. Results are representative of two experiments performed in triplicate. (B) SKBr3 cells on a 96 well plate were treated with indicated dilutions of BZL101 for three hours. 10 μM dihydroethidium was added to wells for the last 20 min of incubation. Wells were washed and analyzed for fluorescence at the wavelength of 610 nM
Levels of reactive oxygen species (ROS) in cells treated with BZL101 were analyzed using staining with dihydroethidium, a cell permeable dye that has weak blue fluorescence. Intracellular ROS, if present, convert dihydroethidium to ethidine, a compound that emits red fluorescence and can bind DNA. Staining was performed on several cell lines, and the representative results for SKBr3 are shown in Fig. 3B. There was a dose-dependent induction of ROS in cells treated with BZL101.
Patient characteristics
A total of 22 patients with advanced breast cancer signed informed consent and enrolled to the study; 21 were treated with at least one dose of oral BZL101 and are evaluable for safety analysis. The last patient accrued to the study was not treated with BZL101 as funding for the study from the California Breast Cancer Research Program had ended and the expiration date for the study medication was too close to allow adequate duration of therapy. Sixteen of the patients were treated for at least 28 days and are evaluable for response. Nine subjects discontinued study medication due to patient preference (primarily grade I/II gastrointestinal toxicity) and 12 patients discontinued BZL101 due to progression based on RECIST criteria. No patients stopped therapy due to either grade III or IV adverse events categorized according to the National Cancer Institute (NCI) Common Toxicity Criteria (CTC) Version 2. Table 2 provides a summary of study patients and Table 3 shows a summary of selected patient characteristics.
Safety data
There were no deaths on study and no serious adverse events or hematological adverse effects attributed to the study medication. There were no grade III or IV toxicities that were classified as possibly, probably or definitely related to BZL101. A total of 22 grade I and 18 grade II toxicities were reported as possibly, probably or definitely related to BZL101 (Table 4). The majority of the AEs, including 31 incidents, were categorized as grade I or II gastrointestinal side effects that were expected as a potential toxicity of BZL101 (Table 5). All four AEs categorized as pain were due to headaches.
Feasibility
Feasibility of the study was measured by compliance with the study medication as reported on a patient self-reported questionnaire. Data were available for 15 of the 21 study patients who took at least one dose of BZL101 and completed the questionnaire. Six patients did not complete the questionnaire. On average, compliance with study medication was 84.5% of prescribed doses taken (range 20%–100%, median was 92.2%). There were nine patients who went off of the trial due to patient preference; eight of whom discontinued treatment due to grade I/II gastrointestinal side effects or an inability to tolerate the taste of the extract. The last patient discontinued study medication because she wanted to start a new therapy.
Efficacy
Of the 21 patients who were treated with study medication, 16 remained on study for 28 days or more and were evaluable according to RECIST criteria. The average number of prior therapies for metastatic disease for patients who took at least one dose of BZL101 was 3.9. Four of 16 (25%) had stable disease for >90 days and 3/16 (19%) had stable disease for >180 days. Five patients had some degree of objective tumor regression, one of which was 1 mm short of a partial remission based on RECIST criteria (See Table 6). The last column of Table 6 shows tumor response based on RECIST criteria and the month on study that the response was noted. The range for minimal response was 8%–29%.
Using a modified RECIST evaluation, where all measurable lesions including those under 1 cm were included as evaluable, one participant had a partial response or a reduction of 31% in the sum of the longest tumor diameter of all measurable lesions after 7 weeks of treatment and a reduction of 33% after 11 weeks of treatment (Table 7).
Survival calculation
Follow-up survival information was available for 12 patients enrolled on this trial (Table 8). The mean survival from study initiation for these 12 patients was 327.5 ± 184.6 days (range = 82–757 days), while the mean survival after study end was 243.6 ± 193.9 days (range = 45–713 days). There was a trend for better survival among the patients who had received 2–3 prior treatments for metastatic disease compared to the patients who had received >3 prior treatments (p = 0.67; Table 8 and Fig. 4A). Of the 12 patients with survival information, six discontinued therapy due to progression of disease, while six discontinued while on therapy due to preference. The mean survival time for the patients who progressed on therapy was 379 ± 218.0 days (205–553 days) compared to 276 ± 144.5 days (161–391 days) for patients who discontinued therapy due to preference (p = 0.35) (Fig. 4B).
Discussion
BZL101 is an aqueous extract of Scutellaria barbata with cytotoxic activity demonstrating unique pro-apoptotic properties that are cancer cell-specific. BZL101 appears to induce a pathway in which tumor cells but not normal cells undergo apoptosis. Our results indicate that BZL101 extract might have mitochondriotoxic activity as evidenced by the fast dissipation of the mitochondrial transmembrane potential and induction of reactive oxygen species. Overexpression of the anti-apoptotic mitochondrial membrane protein Bcl-2 in ovarian cancer cells has been shown to lead to only partial protection from BZL101 induced cell death in one of four cell lines (A2780) but not in others (SKOV3, Hey and HA8), suggesting that Bcl-2 expression does not have much effect on BZL101 induced cytotoxicity [11]. Our data show that caspases are involved in the BZL101 induced cell death, but it remains to be elucidated if caspase activation is a causative event in this process or is secondary to the other death signaling pathways.
In a phase I clinical trial, we have shown that treatment with BZL101 is feasible and safe. Unlike most phase I trials, we chose to conduct this study in women with advanced breast cancer rather than a cohort of patients with many different types of tumors due to the strength of our preclinical data in breast cancer cell lines. Our cohort was heavily pre-treated for their advanced disease with an average of 3.9 (0–10) prior treatments since metastatic diagnosis.
The phase I of BZL 101 was conducted with a grant from the State of California Breast Cancer Research Program. Due to the limited budget, issues related to the optimization of the method of administration were delayed. The extract was concentrated but the bitter taste was not modified. This taste was likely responsible for some of the recorded side effects such as the transient nausea, vomiting and gagging. Although a relatively large proportion of subjects on this trial encountered these symptoms, 48%, 10% and 5%, respectively, none of the symptoms required medical attention or pharmacological intervention.
Another contributing factor for gastrointestinal toxicities could be that the manufacturing of the extract was not refined, and insoluble plant roughage was ingested in high doses (approximately 12 g/day). The transient symptoms of diarrhea, constipation, bloating, gas and abdominal cramping were most likely caused by the significant increased intake of insoluble fiber. None of these gastrointestinal side effects were severe enough to require medical attention or pharmacological intervention.
Other grade I/II side effects of BZL101 were likely due to underlying disease or prior therapy including headache, numbness and tingling, chills and fatigue. There were no grade III or IV toxicities attributed to BZL101. There were no deaths reported during or shortly after the trial. Most of the patients who discontinued study medication due to personal preference (8/9), did so due to minor and transient gastrointestinal side effects or due to the taste of the drug. Even with the bitter taste of the extract, patients who remained on study were willing to take the drug with a high compliance (84.5%).
Tumor response was assessed with RECIST criteria and there was an early indication of biological antitumor activity; one woman was 1 mm in tumor reduction short of a partial remission (PR), 29% reduction vs. 30% required for a PR. If one of the patient’s non-evaluable palpable lesions (originally measured at 0.8 cm) was included for RECIST analysis, this would have been coded as a PR. Four other women had minimal responses.
In this heavily pre-treated population, four of the 16 evaluable patients (25%) had stable disease for >90 days and 3/16 (19%) had stable disease for >180 days, a possible sign of clinical activity. Early survival calculations using Kaplan–Meier and Cox Regression analyses suggest that patients who used BZL101 with >3 prior treatments for their metastatic disease had poorer survival than patients who used only 2–3 prior treatments. Also, survival appeared better for patients who progressed on BZL101 therapy versus patients who discontinued treatment due to personal preference. However, neither of these benefits were statistically significant, p = 0.67 and p = 0.35, respectively.
Even though BZL101 was administered as a crude, unrefined, bitter tasting extract, it did show early indications of biological antitumor activity and a potential to delay disease progression. Once the extract is modified with an improved taste and with less insoluble plant fiber, it is possible that a higher dose of BZL101 will be tolerated and that many of the gastrointestinal side effects can be significantly reduced.
In summary, this phase I clinical trial of an herbal extract was feasible and safe. BZL101, and possibly other extracts with encouraging preclinical activity, merit further investigation in the treatment of cancer. With an improved extract of BZL101, a phase 2 clinical trial for women with advanced breast cancer is planned to commence this year.
Reference
Cragg GM, Newman DJ (2005) Plants as a source of anti-cancer agents. J Ethnopharmacol 100:72–79
Bulletin of the World Health Organization (2002) 80:610
Boon H, Wong J (2004) Botanical medicine and cancer: a review of the safety and efficacy. Expert Opin Pharmacother 5:2485–2501
Vickers AJ, Kuo J, Cassileth BR (2006) Unconventional anticancer agents: a systematic review of clinical trials. J Clin Oncol 24:136–140
Zhu YP (1998) Chinese materia medica: chemistry, pharmacology and applications. Harwood Academic Publishers; Amsterdam p 210
Campbell MJ, Hamilton B, Shoemaker M, Tagliaferri M, Cohen I, Tripathy D (2002) Antiproliferative activity of Chinese medicinal herbs on breast cancer cells in vitro. Anticancer Res 22:3843–3852
Shoemaker M, Hamilton B, Dairkee SH, Cohen I, Campbell MJ (2005) In vitro anticancer activity of twelve Chinese medicinal herbs. Phytother Res 19:549–551
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS et al (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92:205–216
Diggle PJ, Heagerty PJ, Liang K-Y, Zeger SL (2002) Analysis of longitudinal data, 2nd edn. Oxford University Press New York (NY)
Lee ET, Wang JW (2003) Statistical methods for survival data analysis, 3rd edn. John Wiley & Sons; Hoboken (NJ)
Powell BC, Fung P, Jackson J, Dall’Era J, Lewkowicz D, Cohen I, Smith-McCune K (2003) Aqueous extract of herba Scutellaria Barbatae, a Chinese herb used for ovarian cancer, induces apoptosis of ovarian cancer cell lines. Gynecol Oncol 91:332–340
Author information
Authors and Affiliations
Corresponding author
Additional information
This clinical trial was supported by the California Breast Cancer Research Program IDEA Award CA-BCRP 7WB-0055. We thank Dr. Laura Esserman for encouraging rigorous scientific research in the area of botanical medicine at the University of California, San Francisco Carol Franc Buck Breast Care Center.
Rights and permissions
About this article
Cite this article
Rugo, H., Shtivelman, E., Perez, A. et al. Phase I trial and antitumor effects of BZL101 for patients with advanced breast cancer. Breast Cancer Res Treat 105, 17–28 (2007). https://doi.org/10.1007/s10549-006-9430-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-006-9430-6