Abstract
Aims
Male breast cancer incidence is 1% of all breast cancers and is increasing. We aim to present an overview of male breast cancer with particular emphasis on clinical management.
Methods
Studies were identified by an online search of literature in the MEDLINE database till June 2006 followed by an extensive review of bibliographies.
Results
Increased risk factors include genetic predisposition as in BRCA2 families; testicular dysfunction due to chromosomal abnormality such as Klinefelter’s syndrome or environmental factors such as chronic heat exposure and radiation. Clinical assessment with biopsy is the hallmark of diagnosis. Earlier presentations are becoming commoner but there are wide geographical differences. Surgical treatment involves simple or modified radical mastectomy along with surgical assessment of the axilla, either via sentinel node biopsy in clinically node-negative disease or axillary sampling/clearance in node-positive disease. Reconstructions for restoring body image have been recently reported. Indications for adjuvant therapies are similar to that in women. For metastatic disease, tamoxifen is still the mainstay for oestrogen receptor positive disease. For oestrogen receptor negative disease, doxorubicin based chemotherapy regimens are used. In addition, the oft neglected psychological aspects of men having a “cancer of women” are increasingly being recognised.
Conclusions
There is, thus, need for further increasing awareness among men to reduce stigma associated with presentation of symptoms related to breast. This should be in addition to stressing to clinicians the ways of earlier detection and tailor-made “gender oriented” treatment of breast cancer in men.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of Male Breast Cancer (MBC) is increasing along with the increasing incidence of female breast cancer. MBC comprises about 1% of all breast cancers. About 240 men are diagnosed in UK each year compared to 40,400 women (Cancer Research, UK, 2004). National Cancer Institute data on cancer survival in the US from 1973 to 1998 shows increase in the incidence of MBC from 0.86 to 1.08 per 100,000 men [1]. We, therefore, present a review of literature delving predominantly into the concepts in the clinical management of MBCs.
Aetiology
Genetic predisposing factors include abnormalities of both somatic and sex chromosomes. Linkage to both BRCA1 [2–4] and BRCA2 [5, 6] genes occur in breast cancer prone families with MBC cases. BRCA2 mutations are much commoner and the carrier frequency in UK is 8% [7]. Men with this mutation have a 6% risk of developing breast cancer by the age of 70 [8]. Furthermore, BRCA2 (but not BRCA1) gene rearrangements have been reported in MBC families [9, 10]. Androgen receptor gene mutation do not substantially predispose to MBC [11].
Klinefelter’s syndrome, a prototype XXY sex chromosome anomaly may predispose to up to 7.5% of MBCs, a higher rate than previously reported 3% with a 50-fold increased risk of developing breast cancer relative to normal men [12].
Acquired aetiological factors include those attributable to testis or certain systemic factors. Hormonal imbalance between oestrogen (excess) and testosterone (deficiency) has been suggested as a possible mechanism of MBC though male patients do not have detectable hormonal imbalances [13–15]. This imbalance may occur endogenously due to testicular maldescent, injury, mumps orchitis [16] or cirrhosis of the liver [17, 18] or by increased peripheral aromatisation of androgens. MBCs due to iatrogenic exogenous administration of oestrogen as in transsexuals [19, 20] have been reported. Similarly in prostate cancer, both iatrogenic administration of oestrogen/diethylstilbestrol [21, 22] and anti-androgen monotherapy have been incriminated [23]. Increased risk by possible increased prolactin production as in head trauma [24]; drugs such as selective serotonin re-uptake inhibitors [25], digoxin and methyldopa [26] have been reported too.
Environmental factors as in men employed in motor vehicle manufacturing and in blast furnaces, steel works, and rolling mills have increased risk of MBC probably because chronic heat exposure suppresses testicular function [27, 28]. Men who work in electromagnetic fields [29–31] are believed to have increased risk of MBC although this has been refuted lately [32, 33]. Carcinogenic effect of therapeutic or accidental radiation either in fractionated or single exposure (of the same total dose) is known in women [34] and has been reported in men [35, 36] including World War II aviators [37]. In 45,880 Japanese male atomic bomb survivors, the excess relative risk is 8 times per sievert of radiation suggesting a statistically significant dose–response relationship [38].
Other reported factors include local chest trauma [39], childless males, benign breast disease, gynaecomastia, Jewish ancestry, history of breast cancer in first-degree relatives [40], smoking, obesity, diabetes [26], and alcohol drinking [41].
Pathology
MBCs appear to be biologically similar to female breast cancers but there are some basic pathological differences. MBCs are predominantly ductal in origin as male breast normally contains ducts only and no lobules [42]. Almost all of the histological subtypes in women have been reported in men too with a relative lack of tubular and medullary carcinomas [42, 43]. About 90% of MBCs are invasive carcinomas while the remaining 10% are non-invasive in situ carcinomas; almost all again being ductal carcinoma in situs [42]. In a study of 84 male ductal carcinoma in situs, 74% of cases were of papillary subtype and almost all cases were of low to intermediate grade [44]. Lobular carcinoma in situ has only been reported in conjunction with invasive lobular carcinoma [45]. The surveillance, epidemiology, and end results (SEER) database of the National Cancer Institute showed rise in in situ carcinomas by 123% in men and 555% in women during the time period between 1973 and 2001 [46].
A review of literature comprising of 46 individual earlier series between 1942 and 2000 on pathology data in MBC by Giordano et al. [45] had revealed 81% of tumours to be oestrogen receptor (ER) positive and 74% progesterone receptor (PR) positive. However, a subsequent large retrospective study by Giordano et al. [1] of 2537 men and 383,146 women in SEER database revealed even higher rates with 90.6% ER positivity in men (with 680 known ER status) compared to 76.0% (with 119,737 known ER status) in women (P < 0.001). Similarly, 81.2% of tumours in men expressed more PR (with 660 known) compared to 66.7% (P < 0.001) in women (with 116,195 known).
As in women, ER positivity in MBCs significantly (P = 0.04) increases with patient age, from 75% in 30–34 years age group to 94% in over 85 years age group [1] though this was not the case in the earlier review [45].
In the review by Giordano et al. [45], 37% of MBCs had overexpression of HER-2, 30% with overexpression of p53, 79% with overexpression of bcl-2, 51% with overexpression of cyclin D1, and 39% with overexpression of epidermal growth factor receptor.
However, recent-most data show lesser overexpression of HER-2 up to 15% in MBCs. In one study [47], only 1.7% (1 out of 58 cases) of MBCs overexpressed HER-2 on immunohistochemistry but no amplification on FISH (fluorescence in situ hybridisation) compared with 26% and 27% in women, respectively. Similarly, 1.1% (1 out of 91 cases) positivity on FISH was shown from Finnish Cancer Registry [48]. However, in contrast to the above two, in another study [49] HER-2 positivity was seen in 15.1% (15 out of 99 cases) by immunohistochemistry and 11.1% (11 out of 99 cases) on FISH.
Clinical features
MBCs present 10 years later than female breast cancers [29, 50–53]. The mean age of presentation is mostly in sixties but ranging from twenties to nineties. The duration of symptoms before diagnosis is declining [54] but there are major geographical differences ranging from a mean of 1–8 months [52, 55, 56] in western world to a mean of 12–15 months in the Asian–African continents and hence a later stage of presentation [57, 58].
Painless mass is the predominant presentation in 13% [59] to 90% [52, 55, 60] of patients with subareolar disposition in 68–90% [53, 59].
Changes in nipple-areola complex occur in up to one third of patients [52, 59] in the form of nipple fixation or retraction, inversion, oedema, or eczema. Bloody discharge is associated in 75% of cases with malignancies [61] including DCIS [62]. Serous discharge occurs in approximately 15% of patients [52].
Ulceration of the skin is reported in approximately 27% of patients [59]. Paget’s disease may be a form of presentation in up to 5% of cases with skin erythema, inflammatory changes, skin nodules or satellite lesions. Pigmented lesion of Paget’s disease may be confused with melanoma [55, 63, 64]. There is no evidence that Paget’s disease in males behaves differently to that in females although survival is less (20–30% in males versus 30–50% in females) [64].
Less common symptoms are breast tenderness, swelling, nipple itching, or symptoms of distant metastasis [59]. Axillary adenopathy suspicious for metastasis is clinically detected in 40–55% of patients at the time of presentation [65–67]. However, axillary metastasis as the first presentation of occult breast cancer is rare [68]. Bilateral MBCs range from 0% to 1.9% [50, 52] compared to reported incidence of 4.3% in women [69].
Rare presentations include granulomatous mastitis [70], cystosarcoma phyllodes [71], inflammatory breast cancer [72]; unusual paraneoplastic syndromes [73]. Late presentations include distant metastases including reported metastasis to brain [74].
Investigations
Mammographically detected breast cancer has been reported [75] but breast cancer screening programme in the male population is not feasible at present considering the relative low incidence as compared with females though it is technically possible in spite of the dimensions of the male breast. Therefore, clinical examination remains the key in evaluation of a palpable mass in men. If the clinical features strongly suggest gynaecomastia, further evaluation may not be necessary. Clinicians, however, should be aware that an overtly obvious gynaecomastia can partially or completely obscure underlying malignant mass [76]. Imaging in equivocal cases is often not helpful, as gynaecomastia and cancer can mimic each other on both mammography and ultrasound. Fine-needle aspiration (FNA)/core biopsy guided by palpation and/or excisional biopsy are necessary to make the diagnosis.
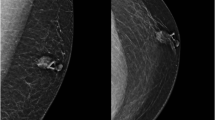
Mammography in pre-operative evaluation of the opposite breast has a limited role in MBC and often overused [77]. Primary mammographic characteristics in men include a mass, subareolar or somewhat eccentric to the nipple and mostly well-defined with speculated margins [76, 78, 79]. Micro calcifications are observed less commonly than in women, and are coarser in appearance [79]. A mammogram showing only fat can be helpful in cases of unilateral breast enlargement without mass and it is more useful in obese men with large breasts. False positives occur in inflammation, gynaecomastia, and fat necrosis.
On Ultrasound, a hypo-echoic mass with mostly irregular or less commonly circumscribed margins may be observed [76, 79]. With colour flow imaging, vascular flow within the mass may be demonstrated [79]. The appearance of a complex cystic mass in the male breast on sonography should suggest the possibility of malignancy and therefore warrants biopsy [80]. False positive cases are similar to that of mammography. In mammographically and sonographically indeterminate breast lesions, thallium scanning (Tl-201 scintigraphy) may be a third step of investigation to obviate biopsy [81]. Mammography was the most sensitive (92%) and thallium scanning was the most specific (75%) in a study, which compared mammography, ultrasound and thallium scanning [81].
Galactograms can aid in the localisation of abnormal ductal tissue in patients with nipple discharge and no mass [82]. MRI has not been studied regarding sensitivity in diagnosis, but since the lesions are always palpable and can be biopsied easily under palpation, there is no clear role for MRI [79].
The cytological features on FNA are similar to those described in women [83]. In one series, FNA was positive in 27 of 49 patients with operable breast cancer [84]. Generally, conventional cytological examination of the aspirate is adequate [85], but in some cases, monoclonal antibody analysis may be a useful adjunct [86]. In cases with inadequate FNA, core biopsy is recommended [87].
Treatment
Surveillance
Rise in MBCs as seen in SEER database including rising in situ incidence rates [46] over the past three decades suggest increasingly earlier detection over time, irrespective of mammography, because men do not participate in routine screening mammography.
However, screening in men with high risk factors may be warranted. For example, screening for large BRCA2 gene rearrangements has been suggested especially in MBC families tested negative for BRCA1 and BRCA2 mutations [9, 10]. Klinefelter’s syndrome is another condition where screening may be feasible as there is 50-fold increased risk of breast cancer in patients with this syndrome [12]. Clinicians treating patients with anti-androgens/oestrogens should be aware of the increased risk of MBC.
Early/local disease
Surgery
There is no survival difference in MBCs treated either with radical procedures or lesser radical procedures such as modified radical or simple mastectomy [50, 55, 88–91]. Compared with mastectomy, lumpectomy was associated with significantly worse local control rate in a Canadian series of 229 patients treated over 40 years, 20 (8.7%) of whom were treated with lumpectomy including eight with axillary dissection [92]. In a French study of 31 DCIS cases treated with surgery, there were three local recurrences out of six treated with lumpectomy compared to only 1 recurrence in the rest 25 treated with mastectomy [93]. In addition, adequate tumour excision by lumpectomy may not be possible due to the small volume of male breast tissue [45, 92].
Surgical treatment therefore involves simple or modified radical mastectomy along with surgical assessment of the axilla, either via sentinel node biopsy in clinically node-negative disease or axillary sampling/clearance in node-positive disease. Simple mastectomy is the preferred local surgical option and is the routine surgical procedure in Nottingham Breast Unit [55].
Sentinel lymph node biopsy
There has been tremendous interest in sentinel lymph node biopsy (SLNB) of late and if present, SLNB of the internal mammary chain. In limited number of cases, in the hands of experienced surgeons it has been equally successful as in women [94, 95]. Blue dye injection and radioisotope injection have been complementary for the identification of SLN [96, 97]. The findings in men seem to correlate with women. Therefore, SLNB should be considered for axillary staging in MBC patients with clinically negative axillae to avoid unwarranted axillary dissection and subsequent arm lymphoedema.
Reconstruction
As most of the MBCs present late, larger excisions are mostly necessitated. Reconstructions of the male breasts are thus for some resultant post-excision “chest wall defect”. Reconstructions can be done by means of fasciocutaneous or myocutaneous local or distant flaps, depending on the stage of the neoplasia [98]. Use of delto-pectoral flap [99] and transverse thoracoepigastric skin flap [100] has been reported. The TRAM flap has been recommended because not only it can replace the missing skin and fat but also because it may be a source of hair-bearing skin similar to the native breast skin [101, 102]. The external oblique musculocutaneous flap has also been considered a reliable option; with segmental blood supply from the posterior intercostal arteries. Use of a reverse-flow external-internal oblique flap supports the concept of rotating the muscles as a unit to encourage viability of the denervated and relatively devascularized component [103].
Systemic (adjuvant) therapy
Systemic adjuvant therapy improves prognosis in cases with lymph node involvement [104, 105]. In a retrospective series of 50 patients, Margaria et al. [91] reported a median survival of 33 months for patients receiving surgery alone and 86 months for those who also had adjuvant therapy (P = 0.003). No difference in survival was found among the various types of adjuvant therapy.
Endocrine therapy
As MBCs are predominantly ER positive [1], in high-risk patients, the use of adjuvant endocrine therapy and/or combined endocrine and chemotherapy should be considered. The most commonly used endocrine agent is tamoxifen. Although in some series [54, 106, 107] adjuvant tamoxifen was not associated with improved survival but in a large series of 57 men, adjuvant tamoxifen had a positive influence on disease-free survival and overall survival [92]. In another series of 39 men, there was highly significant improvement in both 5-year actuarial survival and disease-free survival compared with historical controls [108]. In a recently published data of 38 men who received adjuvant hormonal therapy (including 35 who received tamoxifen), Giordano et al. [109] reported that the recurrence rate (HR of 0.49; 95% CI, 0.27–0.90) and overall survival (HR of 0.45; 95% CI, 0.25–0.84) was significantly better for men who received adjuvant hormonal therapy compared with no adjuvant therapy.
As adjuvant hormonal therapy for 5 years, anastrozole has recently been shown to impart significantly prolonged disease-free survival and time-to-recurrence compared to tamoxifen in a large multi-centre trial [110] in 9,366 postmenopausal women with localised breast cancer. However, usage of aromatase inhibitors alone is biologically doubtful in men [111]. Twenty percent of circulating estrogens [112] in men is produced by testes and this is independent of aromatase enzyme, which is blocked by aromatase inhibitors. Hence, complete inhibition of oestrogen may not occur in the absence of orchidectomy. However, gonadal ablation by gonadotropin-releasing hormone (GnRH) analogue such as goserelin along with aromatase inhibitors may afford complete suppression of oestrogens but there is no such data in literature at present.
Radiotherapy
Since MBCs are predominantly central in location, adjuvant radiotherapy may include the internal mammary nodes in addition to the routine fields used in women [78, 113–115]. In one series, there was no loco regional relapse in five patients who received adjuvant radiotherapy in contrast to the two relapses in three patients who underwent surgery alone [113]. Considering the small volume of the male mammary gland, Gennari et al. [116] suggested post-mastectomy irradiation in case of T >1 cm and/or presence of >1 metastatic axillary lymph node. The authors also suggested radiotherapy after all cases of breast conserving surgery when performed in selected cases of MBCs.
Although postoperative radiotherapy showed benefit in reducing loco-regional recurrence but no survival benefit was achieved in some series [117, 118]. However, in a review of 42 MBCs, superior 10-year disease-free and overall survival rates (P = 0.2) was seen when both tamoxifen and radiotherapy were used as adjuvant therapy in localised MBC [118].
Chemotherapy
Patients with ER negative disease should be offered chemotherapy [105] though older presentation age of MBC patients may render them unfit for such therapy. Adjuvant combination chemotherapy has been administered to men with positive axillary nodes or stage II or greater disease in a number of series [78]. Chemotherapy regimes include cyclophosphamide-methotrexate-5-fluorouracil (CMF) or anthracycline based regimens predominantly being 5-fluorouracil-adriamycin-cyclophosphamide (FAC). Taxanes have been used along with anthracyclines [109] in adjuvant settings but data is extremely limited in MBCs to draw any conclusion [119].
In the only existing prospective series, 24 patients with stage II disease were treated with CMF. The projected 5-year actuarial survival rate was greater than 80% (95% confidence interval 74–100%) [120], a substantial improvement over survival rates than in other series. In another study of 11 patients with stage II or III disease treated with FAC, 63% disease-free survival rate and a 91% survival rate at 52 months was reported [121]. In the retrospective study by Giordano et al. [109], there was statistically non-significant improvement in time to recurrence and overall survival in comparison to patients who did not receive chemotherapy among 57 patients with node-positive disease. The authors concluded that the point estimate of a risk reduction of 22% with adjuvant chemotherapy in their study was consistent with the risk reductions in women with chemotherapy.
Trastuzumab therapy
MBC patients with overexpression of C-erb-B2 oncogene [45, 47–49] may benefit from humanised anti-HER-2 monoclonal antibody, trastuzumab especially in ER negative disease in light of its proven efficacy in women.
Therefore, although there is no prospective randomised controlled trials to confirm the value of systemic adjuvant therapies in MBC but most retrospective series and also extrapolation of beneficial results of such therapies in women demonstrate the recurrence and survival benefits especially with adjuvant hormonal therapy in predominantly ER positive disease and adjuvant chemotherapy in ER negative disease or in node-positive disease irrespective of ER status.
Late/metastatic disease
Due to late presentation, men have more advanced disease at diagnosis than women [1]. Sites of metastases are similar to those in women and include bone, lung, liver, brain and others. Median survival from the time of presentation with metastatic disease is approximately 26.5 months [56, 78].
Systemic therapy
Endocrine therapy
In patients with metastatic ER positive disease, initial treatment should be with endocrine agents [105] because significant majority of MBCs are positive for ERs [1]. Surgical ablation by way of orchidectomy, adrenalectomy or hypophysectomy is obsolete now with the advent of endocrine agents.
The preferred endocrine agent is tamoxifen. It has a response rate of up to 80% in ER positive tumours [88, 122]. In one study, objective response was noted in soft-tissue disease, bone and lung metastases in 38% of patients with the duration of response ranging from 8 months to 60 months with a mean of 21 months [122]. Another study of 41 MBCs revealed the response to additive hormonal therapy as 31% and was not affected by prior ochidectomy (33% vs. 30%) [123].
Use of selective aromatase inhibitors has been widely reported in females but as mentioned earlier in the adjuvant section, use of aromatase inhibitors is biologically doubtful in men. However, there are individual case-reports of its efficacy in locally advanced and metastatic MBC without hormonal or surgical ablation of testes. Treatment of metastatic MBC with anastrozole has been reported from one centre where three out of five patients treated with it had stable disease [124]. Two case reports have suggested the benefit of letrozole in recurrent metastatic breast cancer [125] and in locally advanced breast cancer [126]. In an attempt to clarify the role of aromatase inhibitors vis-à-vis GnRH agonists, the Southwest Oncology Group of National Cancer Institute in US is currently recruiting 56 MBC patients to a phase II study to evaluate the efficacy of anastrozole in combination with goserelin acetate (GnRH analogue) in hormone-receptor (ER or progesterone receptor) positive recurrent or metastatic breast cancer [127].
There is lack of data on activity of new pure anti-oestrogen, fulvestrant, in men. However, Agrawal et al. [128] have recently reported clinical benefit in two ER positive cases treated with 250 mg of fulvestrant as 1st line endocrine therapy. One of these patients had locally advanced breast cancer and had partial response while the other patient with metastatic disease in bone and pleura had stable disease.
Other hormonal agents that have been used include ketoconazole, oestrogen, cyproterone acetate, corticosteroids, androgens, progestins, aminoglutethimide and buserelin with or without the anti-androgen flutamide [78, 129–134]. The duration of response to these agents varies from 3 months to 12.5 months [133].
Therefore, tamoxifen remains as first line hormone therapy till further large-scale data are available. As a second-line hormonal therapy for men, orchidectomy or luteinizing hormone-releasing hormone agonists with or without antiandrogens are reasonable present alternatives [135].
Radiotherapy
Radiotherapy for control of locally advanced fungating/bleeding tumour may be necessitated as in females. It may be also be necessary for palliation of pain or soft tissue pressure symptoms in metastatic disease.
Chemotherapy
Systemic chemotherapy should be used in patients who are either hormone-receptor negative or resistant to available endocrine therapies [105, 135] or in patients with disease-free interval of less than 1 year as they often fail to respond to hormonal therapy [123]. About 35% of patients respond to combination chemotherapy, with doxorubicin-based regimens proving more effective, as in female breast cancer [136]. Although men appear to respond faster to chemotherapy, their duration of response may be shorter [129].
Trastuzumab therapy
Pending larger series, one case report does exist of the use of trastuzumab with paclitaxel where the patient with HER2 positive metastatic disease had complete response in the lung and stable disease in bones [137].
Psychological support
There is relative paucity of evidence in literature about the psychological consequences following diagnosis of breast cancer in men as compared with women. In a questionnaire based cross-sectional study of emotional expression of 41 men with prostate cancer and 41 women with gynaecological cancers, the authors reported that the more important cause of distress resulting from cancer is not due to men being less emotionally expressive but because they are more vulnerable to perceptions of social constraints from spouse/partner or others [138]. This distress could be even worse in men with breast cancer seeing themselves, albeit incorrectly, as having a cancer in a sexual organ associated with females.
In a cross-sectional questionnaire of 161 MBC patients that included measures of anxiety and depressive symptoms, cancer-specific distress, body image, coping, information and support needs, and clinical and demographic variables; low clinical levels of anxiety (6%) and depressive (1%) symptoms were reported but high levels of traumatic stress symptoms specific to breast cancer (23%) were reported [139]. France et al. [140] conducted six in-depth interviews regarding seven major issues: delay in diagnosis, shock, stigma, body image, causal factors, the provision of information and emotional support. Authors opined that men tended to develop denial defence mechanism which may be beneficial in short-term but it delayed their seeking professional help. Authors, therefore, recommended development of a structured education programme aimed at all primary health-care professionals and supported by media for increasing awareness along with availability of pre and postoperative gender-specific information to alleviate the potential psychological problems associated with the diagnosis. In addition to men with breast cancer, appropriate support/counselling services for partners of patients were recommended. Peate [141] suggested that as nurses often act as advocates for women with breast cancer, they are in an ideal position to do the same for men with breast cancer. However, although men acknowledged support of breast care nurses but they appreciated the need for one-to-one discussion with another MBC patient [142].
Risk of second primary
The risk of subsequent cancers among 1788 men diagnosed with a 1st primary breast cancer between 1973 and 1996 in SEER program [143] showed that the relative risk of 2nd breast cancer among men was 30-fold increased compared with two to fourfold risk among women with breast cancer though the absolute risk was much lower (0.1% per year) than among women (0.6% per year). The risk was higher for men with 1st breast cancer before the age of 50 years than for older men. The authors did not report major differences in the risk of contralateral breast cancer associated with different treatments received for the 1st breast cancer.
Prognostic features and survival
There are some racial/ethnic differences as seen by O’Malley et al. Overall, 5-year survival rates were 66% for whites, 57% for blacks, and 75% for men of other race/ethnicity. Blacks presented with more advanced disease. By stage, whites and blacks had worse survival rates compared with men of other race/ethnicity [144].
The most important independent prognostic factors appear to be tumour size [1, 107, 145, 146], grade [1, 107], lymphatic invasion, axillary node status [1, 146] and stage [146].
MBC patients have previously been reported to have significantly better 5-year survivals than females [147] partly due to increased use of modified radical mastectomy and systemic adjuvant therapy [54] but in a review of 229 patients during the same time period, no difference in outcome was observed despite a change in standard primary surgical treatment and an increased use of chemotherapy and hormone therapy [109]. Furthermore, in the review of 2537 men and 383,146 women in SEER program, Giordano et al. [1] reported lower stage-by-stage overall 5-year survival for men than women. However, the relative survival rate (Stage I = 96%, II = 84%, III = 52%, IV = 24%) was not much different from women (Stage I = 99%, II = 84%, III = 55%, IV = 18%) when adjusted for the expected survival rate of the US population for race, gender and age. Similarly in another comparative large study with demographically identical pairs of 4755 men and 624,174 women, although the relative 5-year survival rate for Stage I and II was almost the same for both men and women but for Stage III and IV, survival was non-significantly worse in men [148].
Conclusion
There is lack of prospective randomised studies due to the lower incidence as compared to that in women. However, recent most articles report clinical management procedures specific to men and not as earlier reported extrapolations from female breast cancers. Breast cancer in men has aetio-pathological differences from that of women but present treatment regimes are comparative. Men with any breast symptom should essentially be investigated in the same manner and degree of urgency as in women.
Clinical examination remains the modality of diagnosis though biopsy is confirmatory. Simple mastectomy is the treatment of choice for early disease with choices of reconstruction for resultant chest wall defects, which can be more extensive than in women. Adjuvant radiotherapy decreases local recurrence especially in selective cases with conservative surgery. Adjuvant systemic endocrine therapy in ER positive disease and chemotherapy in ER negative disease and node-positive disease have shown local and survival benefits over no adjuvant therapy.
For metastatic disease, tamoxifen (this is where the bulk of data is) remains the gold standard for ER positive disease. Orchidectomy, luteinizing hormone-releasing hormone agonists are subsequent alternatives. For ER negative disease, doxorubicin based chemotherapeutic regimens are standard.
Despite a wealth of small retrospective studies on MBC, its relative low incidence contributes to the lack of prospective randomised controlled treatment trials with resultant relative lack of tailor-made “gender oriented” management of breast cancer in males. This needs to be addressed in light of the fact that the incidence is increasing if significant advances are to be made in the treatment of this unusual challenging disease. These should delve into the psychological and social factors too.
References
Giordano SH, Cohen DS, Buzdar AU, Perkins G, Hortobagyi GH (2004) Breast carcinoma in men: a population based study. Cancer 101(1):51–57
Pich A, Margaria E, Chiusa L (2000) Oncogenes and male breast carcinoma: c-erbB-2 and p53 coexpression predicts a poor survival. J Clin Oncol 18(16):2948–2956
Bernard-Gallon DJ, Dechelotte PJ, Le Corre L et al (2003) Expression of BRCA1 and BRCA2 in male breast cancers and gynecomastias. Anticancer Res 23(1B):661–667
Struewing JP, Brody LC, Erdos MR et al (1995) Detection of eight BRCA1 mutations in 10 breast/ovarian cancer families, including 1 family with male breast cancer. Am J Hum Genet 57:1–7
Wooster R, Neuhausen SL, Mangion J et al (1994) Localization of a breast cancer susceptibility gene, BRCA2, to chromosome 13q 12–13. Science 265:2088–2090
Thorlacius S, Tryggvadottir L, Olafsdottir GH et al (1995) Linkage to BRCA2 region in hereditary male breast cancer. Lancet 346:544–545
Basham VM, Lipscombe JM, Ward JM et al (2002) BRCA1 and BRCA2 mutations in a population-based study of male breast cancer. Breast Cancer Res 4(1):R2. Epub 2001 Nov 21
Wolpert N, Warner E, Seminsky MF, Futreal A, Narod SA (2000) Prevalence of BRCA1 and BRCA2 mutations in male breast cancer patients in Canada. Clin Breast Cancer 1(1):57–63 discussion 64-5
Woodward AM, Davis TA, Silva AG, Kirk JA, Leary JA (2005) kConFab investigators. Large genomic rearrangements of both BRCA2 and BRCA1 are a feature of the inherited breast/ovarian cancer phenotype in selected families. J Med Genet 42(5):e31
Tournier I, Paillerets BB, Sobol H et al (2004) Significant contribution of germline BRCA2 rearrangements in male breast cancer families. Cancer Res 64(22):8143–8147
Syrjakoski K, Hyytinen ER, Kuukasjarvi T et al (2003) Androgen receptor gene alterations in Finnish male breast cancer. Breast Cancer Res Treat 77(2):167–170
Hultborn R, Hanson C, Kopf I et al (1997) Prevalence of Klinefelter’s syndrome in male breast cancer patients. Anticancer Res 17(6D):4293–4297
Ballerini P, Recchione C, Cavalleri A et al (1990) Hormones in male breast cancer. Tumori 76:26–28
Casagrande JT, Hanisch R, Pike MC et al (1988) A case–control study of male breast cancer. Cancer Res 48:1326–1330
Kessler LRS II (1980) Selected aspects of breast cancer etiology and epidemiology. Proc Am Assoc Cancer Res 21:72
Thomas DB, Jimenez LM, McTiernan A et al (1992) Breast cancer in men: risk factors with hormonal implications. Am J Epidemiol 135:734–748
Sorensen HT, Friis S, Olsen JH et al (1998) Risk of breast cancer in men with liver cirrhosis. Am J Gastroenterol 93(2):231–233
Misra SP, Misra V, Dwivedi M (1996) Cancer of the breast in a male cirrhotic: is there an association between the two? Am J Gastroenterol 91(2):380–382
Symmers WS (1968) Carcinoma of the breast in transsexual individuals after surgical and hormonal interference with the primary and secondary sexual characteristics. Br Med J 2:83–87
Pritchard TJ, Pankowsky DA, Crowe JP et al (1988) Breast cancer in male-to-female transsexual: a case report. J Am Med Assoc 259:2278–2280
O’Grady WP, McPivin RW (1969) Breast cancer in a man treated with diethylstilbestrol. Arch Path 88:162–165
Schlappack OK, Braun O, Maier U (1986) Report of 2 cases of male breast cancer after prolonged estrogen treatment for prostatic carcinoma. Cancer Detect Prev 9:319–322
Karamanakos P, Mitsiades CS, Lembessis P et al (2004) Male breast adenocarcinoma in a prostate cancer patient following prolonged anti-androgen monotherapy. Anticancer Res 24(2C):1077–1081
Olsson H, Ranstam J (1988) Head trauma and exposure to prolactin elevating drugs as risk factors for male breast cancer. J Natl Cancer Inst 80:679–683
Wallace WA, Balsitis M, Harrison BJ (2001) Male breast neoplasia in association with selective serotonin reuptake inhibitor therapy: a report of three cases. Eur J Surg Oncol 27(4):429–431
Ewertz M, Holmberg L, Tretli S, Pedersen BV, Kristensen A (2001) Risk factors for male breast cancer—a case–control study from Scandinavia. Acta Oncol 40(4):467–471
Mabuchi K, Bross DS, Kessler II (1985) Risk factors in male breast cancer. J Natl Cancer Inst 74:371–375
Cocco P, Figgs L, Dosemeci M et al (1998) Case–control study of occupational exposures and male breast cancer. Occup Environ Med 55(9):599–604
Koc M, Polat P (2001) Epidemiology and aetiological factors of male breast cancer: a ten years retrospective study in eastern Turkey. Eur J Cancer Prev 10(6):531–534
Demers PA, Thomas DB, Rosenblatt KA et al (1991) Occupational exposure to electromagnetic fields and breast cancer in men. Am J Epidemiol 134:340–347
Matanoski GM, Breysse PN, Elliot EA (1991) Electromagnetic field exposure and breast cancer. Lancet 337(8743):737
Stenlund C, Floderus B (1997) Occupational exposure to magnetic fields in relation to male breast cancer and testicular cancer: a Swedish case–control study. Cancer Causes Control 8(2):184–191
Rosenbaum PF, Vena JE, Zielezny MA, Michalek AM (1994) Occupational exposures associated with male breast cancer. Am J Epidemiol 139(1):30–36
Carmichael A, Sami AS, Dixon JM (2003) Breast cancer risk among the survivors of atomic bomb and patients exposed to therapeutic ionising radiation. Eur J Surg Oncol 29(5):475–479
Crichlow RW (1972) Carcinoma of the male breast. Surg Gynecol Obstet 13:1011–1019
Cohen R, Schauer PK (1984) Male breast cancer following repeated fluoroscopy. Am J Med 76:929–930
Gordon DJ, Chin KH, Budny PG, Taylor AR (2003) Male breast cancer in World War II aviation: a case report and review. Breast 12(2):156–157
Ron E, Ikeda T, Preston DL, Tokuaka S (2005) Male breast cancer incidence among atomic bomb survivors. J Natl Cancer Inst 97:603–605
Raviglione MC, Graham PE (1987) Breast carcinoma in a man following local trauma. NY State J Med 87:186–187
Sasco AJ, Lowenfels AB, Pasker-De Jonc P (1993) Epidemiology of male breast cancer. A meta-analysis of published case–control studies and discussion of selected etiologic factors. Int J Cancer 53:538–549
Guenel P, Cyr D, Sabroe S et al (2004) Alcohol drinking may increase risk of breast cancer in men: a European population-based case–control study. Cancer Causes Control 15(6):571–580
Stalsberg H, Thomas DB, Rosenblatt KA et al (1993) Histologic types and hormone receptors in breast cancer in men: a population-based study in 282 United States men. Cancer Causes Control 4:143–151
Hultborn R, Friberg S, Hultborn KA (1987) Male breast carcinoma. A study of the total material reported to the Swedish Cancer Registry 1958–1967 with respect to clinical and histopathologic parameters. Acta Oncol 26:241–256
Hittmair AP, Lininger RA, Tavassoli FA (1998) Ductal carcinoma in situ (DCIS) in the male breast: a morphologic study of 84 cases of pure DCIS and 30 cases of DCIS associated with invasive carcinoma—a preliminary report. Cancer 83:2139–2149
Giordano SH, Buzdar AU, Hortobagyi GN (2002) Breast cancer in men. Ann Intern Med 37(8):678–687
Anderson WF, Devesa SS (2005) In situ male breast carcinoma in the surveillance, epidemiology, and end results database of the National Cancer Institute. Cancer 104(8):1733–1741
Bloom KJ, Govil H, Gattuso P, Reddy V, Francescatti D (2001) Status of HER-2 in male and female breast carcinomas. Am J Surg 82: 389–392
Barlund M, Kuukasjarvi T, Syrjakoski K, Auvinen A, Kallioniemi A (2004) Frequent amplification and overexpression of CCNDI in male breast cancer. Int J Cancer 111:968–971
Rudlowski C, Friedrichs N, Faridi A et al (2004) Her-2/neu gene amplification and protein expression in primary male breast cancer. Breast Cancer Res Treat 84(3):215–223
Ribeiro G (1985) Male breast carcinoma. A review of 301 cases from the Christie Hospital and Holt Radium Institute, Manchester. Br J Cancer 51:115–119
Horm JW, Asire AJ, Young JL et al (eds) (1984) SEER Program: Cancer incidence and mortality in the United States 1973–1981. NIH Publication No. 85-1837. Bethesda, Maryland, U.S. Department of Health and Human Services pp 54–55
Borgen PI, Wong GY, Vlamis V et al (1992) Current management of male breast cancer: a review of 104 cases. Ann Surg 215:451–459
de Perrot M, Deleaval J, Robert J, Spiliopoulos A (2000) Thirty-year experience of surgery for breast carcinoma in men. Eur J Surg 166(12):929–931
Donegan WL, Redlich PN, Lang PJ, Gall MT (1998) Carcinoma of the breast in males: a multiinstitutional survey. Cancer 83(3):498–509
Willsher PC, Leach IH, Ellis IO et al (1997) Male breast cancer: pathological and immunohistochemical features. A comparison outcome of male breast cancer with female breast cancer. Am J Surg 173(3):185–188
Sandler B, Carman C, Perry RR (1994) Cancer of the male breast. Am Surg 60: 816–820
Hassan I, Mabogunje O (1995) Cancer of the male breast in Zaria, Nigeria. East Afr Med J 72(7):457–458
Shukla NK, Seenu V, Goel AK et al (1996) Male breast cancer: a retrospective study from a regional cancer center in northern India. J Surg Oncol 61(2):143–148
Scheike O (1975) Male breast cancer. Acta Pathol Microbiol Scand [A](Suppl 251):3–35
Erlichman C, Murphy KC, Elhakim T (1984) Male breast cancer: a 13-year review of 89 patients. J Clin Oncol 2:903–909
Treves N, Robbins FG, Amorosos WL (1956) Serous and serosanguineous discharge from the male nipple. Arch Surg 73:310
Simmons RM (2002) Male ductal carcinoma in situ presenting as bloody nipple discharge: a case report and literature review. Breast J 8(2):112–114
Perez A, Sanchez JL, Colon AL (2003) Pigmented mammary Paget’s disease in a man. Bol Asoc Med P R 95(4):36–39
Desai DC, Brennan EJ Jr, Carp NZ (1996) Paget’s disease of the male breast. Am Surg 62(12):1068–1072
Crichlow RW, Kaplan EL, Kearney WH (1972) Male mammary cancer. An analysis of 32 cases. Ann Surg 175:489–494
Guinee VF, Olsson H, Moller T et al (1993) The prognosis of breast cancer in males: a report of 335 cases. Cancer 71:154–161
Lartigua E, El-jabbour JV, Dubray B et al (1994) Male breast carcinoma: a single center report of clinical parameters. Clin Oncol 6:162–166
Namba N, Hiraki A, Tabata M et al (2002) Axillary metastasis as the first manifestation of occult breast cancer in a man: a case report. Anticancer Res 22(6B):3611–3613
Maculotti L, Gandini F, Pradella P (1996) Bilateral breast carcinoma. 12 years’ experience. Minerva Chir 51(1–2):33–37(Abstract)
Heer R, Shrimankar J, Griffith CD (2003) Granulomatous mastitis can mimic breast cancer on clinical, radiological or cytological examination: a cautionary tale. Breast 12(4):283–286
Campagnaro EL, Woodside KJ, Xiao SY, Daller JA, Evers BM (2003) Cystosarcoma phyllodes (phyllodes tumor) of the male breast. Surgery 133(6):689–691
Spigel JJ, Evans WP, Grant MD et al (2001) Male inflammatory breast cancer. Clin Breast Cancer 2(2):153–155
Agrawal RS, Agrawal JR, Agrawal BL et al (2003) Some unusual paraneoplastic syndromes. Case 3. Metastatic pulmonary calcification causing hypoxemia in male breast cancer. J Clin Oncol 21(13):2622–2624
Nieder C, Jost PJ, Grosu AL, Peschel C, Molls M (2003) Report of a male patient with brain metastases from breast cancer. Breast 12(5):345–347
Brenner RJ, Weitzel JN, Hansen N, Boasberg P (2004) Screening-detected breast cancer in a man with BRCA2 mutation: case report. Radiology 230(2):553–555
Gunhan-Bilgen I, Bozkaya H, Ustun EE, Memis A (2002) Male breast disease: clinical, mammographic, and ultrasonographic features. Eur J Radiol 43(3):246–255
Hanavadi S, Monypenny IJ, Mansel RE (2006) Is mammography overused in male patients? The Breast 15:123–126
Ravandi-Kashani F, Hayes TG (1998) Male breast cancer: a review of the literature. Eur J Cancer 34(9):1341–1347
Roubidoux MA, Patterson SK (2005) Breast cancer, male. eMedicine. Last Updated: February 2
Yang WT, Whitman GJ, Yuen EH, Tse GM, Stelling CB (2001) Sonographic features of primary breast cancer in men. Am J Roentgenol 176(2):413–416
Ozdemir A, Oznur II, Vural G et al (1997) Tl-201 scintigraphy, mammography and ultrasonography in the evaluation of palpable and nonpalpable breast lesions: a correlative study. Eur J Radiol 24(2):145–154
Detraux P, Benmussa M, Tristant H et al (1983) Breast disease in the male: galactographic evaluation. Radiology 154:605–606
Sneige N, Holder PD, Katz RL et al (1993) Fine needle aspiration cytology of the male breast in a cancer center. Diag Cytopathol 9:691–697
Salvadori B, Saccozzi R, Manzari A et al (1994) Prognosis of breast cancer in males: an analysis of 170 cases. Eur J Cancer 30A: 930–935
Joshi A, Kapila K, Verma K (1999) Fine needle aspiration cytology in the management of male breast masses. Nineteen years of experience. Acta Cytol 43:334–338
Mottolese M, Bigotti G, Coli A et al (1991) Potential use of monoclonal antibodies in the diagnostic distinction of gynecomastia from breast carcinoma in men. Am J Clin Pathol 96:233–237
Westenend PJ (2003) Core needle biopsy in male breast lesions. J Clin Pathol 56(11):863–865
Jaiyesimi IA, Buzdar AU, Sahin AA et al (1992) Carcinoma of the male breast. Ann Intern Med 117:771–777
Scheike O (1974) Male breast cancer. Factors influencing prognosis. Br J Cancer 30:261–271
Spence RAJ, MacKenzie G, Anderson JR et al (1985) Long-term survival following cancer of the male breast in Northern Ireland. Cancer 55:648–652
Margaria E, Chiusa L, Ferrari L, Dal Canton O, Pich A (2000) Therapy and survival in male breast carcinoma: a retrospective analysis of 50 cases. Oncol Rep 7(5):1035–1039
Goss PE, Reid C, Pintilie M, Lim R, Miller N (1999) Male breast carcinoma: a review of 229 patients who presented to the Princess Margaret Hospital during 40 years: 1955–1996. Cancer 85(3):629–639
Cutuli B, Dilhuydy JM, De Lafontan B et al (1997) Ductal carcinoma in situ of the male breast. Analysis of 31 cases. Eur J Cancer 33(1):35–38
Port ER, Fey JV, Cody HS 3rd, Borgen PI (2001) Sentinel lymph node biopsy in patients with male breast carcinoma. Cancer 91(2):319–323
Cimmino VM, Degnim AC, Sabel MS et al (2004) Efficacy of sentinel lymph node biopsy in male breast cancer. J Surg Oncol 86(2):74–77
Albo D, Ames FC, Hunt KK et al (2003) Evaluation of lymph node status in male breast cancer patients: a role for sentinel lymph node biopsy. Breast Cancer Res Treat 77(1):9–14
Goyal A, Horgan K, Kissin M et al (2004) ALMANAC Trialists Group. Sentinel lymph node biopsy in male breast cancer patients. Eur J Surg Oncol 30(5):480–483
Di Benedetto G, Pierangeli M, Bertani A (1998) Carcinoma of the male breast: an underestimated killer. Plast Reconstr Surg 102(3):696–700
Nakao A, Saito S, Naomoto Y, Matsuoka J, Tanaka N (2002) Deltopectoral flap for reconstruction of male breast after radical mastectomy for cancer in a patient on hemodialysis. Anticancer Res 22(4):2477–2479
Caglia P, Veroux PF, Cardillo P et al (1998) Carcinoma of the male breast: reconstructive technique. G Chir 19(8–9):358–362(Abstract)
Spear SL, Bowen DG (1998) Breast reconstruction in a male with a transverse rectus abdominis flap. Plast Reconstr Surg 102(5):1615–1617
Igun GO (2000) Rectus abdominis myocutaneous flap in reconstruction for advanced male breast cancer: case report. Cent Afr J Med 46(5):130–132
Danino A, Ichinose M, Yoshimoto S, Kuroki T, Servant JM (1998) External-internal oblique reverse blood supply musculocutaneous flap for chest wall reconstruction. Ann Plast Surg 41(4):430–433
Donegan WL, Redlich PN (1996) Breast cancer in men. Surg Clin North Am 76(2):343–363
Buzdar AU (2003) Breast cancer in men. Oncology (Huntingt) 17(10):1361–1364, , 1369–1372 (discussion)
La Vecchia C, Levi F, Lucchini F (1992) Descriptive epidemiology of male breast cancer in Europe. Int J Cancer 51:62–66
Pich A, Margaria E, Chiusa L, Candelaresi G, Dal Canton O (1999) Androgen receptor expression in male breast carcinoma: lack of clinicopathological association. Br J Cancer 79:959–964
Ribeiro G, Swindell R (1992) Adjuvant tamoxifen for male breast cancer. Br J Cancer 65:252–254
Giordano SH, Perkins GH, Broglio K et al (2005) Adjuvant systemic therapy for male breast carcinoma. Cancer 104(11):2359–2364
Howell A, Cuzick J, Baum M, Buzdar A, Dowsett M, Forbes JF, Hoctin-Boes G, Houghton J, Locker GY, Tobias JS, ATAC Trialists’ Group (2005) Results of the ATAC (Arimidex, Tamoxifen, alone or in combination) trial after completion of 5 years’ adjuvant treatment for breast cancer. Lancet 365(9453):60–62
Nahleh ZA (2006) Hormonal therapy for male breast cancer: a different approach for a different disease. Cancer Treat Rev 32(2):101–105
Handesman (2001) Androgen actions and pharmacologic uses. In: Detroit IJ (ed) Endocrinology. WB Saunders, Philadelphia, pp 2232–2242
Chung HC, Koh EH, Roh JK et al (1990) Male breast cancer—a 20 year review of 16 cases at Yonsei University. Yonsei Med 31:242–249
Kinne DW (1991) Management of male breast cancer. Oncology 5:5–47
Robinson R, Montague ED (1982) Treatment results in males with breast cancer. Cancer 49:403–406
Gennari R, Curigliano G, Jereczek-Fossa BA et al (2004) Male breast cancer: a special therapeutic problem. Anything new? (Review). Int J Oncol 24(3):663–670
Meguerditchian AN, Falardeau M, Martin G (2002) Male breast carcinoma. Can J Surg 45(4):296–302
Fogh S, Hirsch A, Goldberg S, Powell S, Kachnic L (2005) Male breast cancer: combined modality therapy improves survival. Proc ASCO. Abstract No. 873
Fentiman IS, Fourquet A, Hortobagyi GN (2006) Male breast cancer. Lancet 367:595–604
Bagley CS, Wesley MN, Young RC et al (1987) Adjuvant chemotherapy in males with cancer of the breast. Am J Clin Oncol 10:55–60
Patel HZ, Buzdar AU, Hortobagyi GN (1989) Role of adjuvant chemotherapy in male breast cancer. Cancer 64:1583–1585
Ribeiro GG (1983) Tamoxifen in the treatment of male breast carcinoma. Clin Radiol 34(6):625–628
Kantarjian H, Yap HY, Hortobagyi G, Buzdar A, Blumenschein G (1983) Hormonal therapy for metastatic male breast cancer. Arch Intern Med 143(2):237–240
Giordano SH, Valero V, Buzdar AU, Hortobagyi GN (2002) Efficacy of anastrozole in male breast cancer. Am J Clin Oncol 25(3):235–237
Italiano A, Largillier R, Marcy PY et al (2004) Complete remission obtained with letrozole in a man treated with metastatic breast cancer. Rev Med Int 25:323–324
Zabolotny BP, Zalal CV, Meterissian SH (2004) Successful use of letrozole in male breast cancer: a case report and review of hormonal therapy for male breast cancer. J Surg Oncol 90:26–30
http://www.cancer.gov/clinicaltrials/SWOG-S0511
Agrawal A, Cheung KL, Robertson JFR (2006) Fulvestrant in advanced male breast cancer. Breast Cancer Res Treat [Epub ahead of print]
Griffith H, Muggia FM (1989) Male breast cancer: update on systemic therapy. Rev Endocrine-Related Cancer 31:5–11
Feldman LD (1986) Ketoconazole for metastatic male breast cancer. Ann Intern Med 104:123–124
Lopez M, Di Lauro L, Lazzaro B et al (1985) Hormonal treatment of disseminated male breast cancer. Oncology 42:345–349
Lopez M (1985) Cyproterone acetate in the treatment of metastatic cancer of the male breast. Cancer 55:2334–2336
Vorobiof DA, Falkson G (1987) Nasally administered buserelin inducing complete remission of lung metastases in male breast cancer. Cancer 59:688–689
Doberauer C, Niederle N, Schmidt CG (1988) Advanced male breast cancer treatment with LHRH analogue buserelin alone or in combination with the anti-androgen flutamide. Cancer 62:474–478
Volm MD (2003) Male breast cancer. Curr Treat Options Oncol 4(2):159–164
Lopez M, Di Lauro L, Papaldo P et al (1985) Chemotherapy in metastatic male breast cancer. Oncology 42:205–209
Rudlowski C, Werner R, Becker AJ et al (2001) Correspondence. N Engl J Med 345:997–998
Zakowski SG, Harris C, Krueger N et al (2003) Social barriers to emotional expression and their relations to distress in male and female breast cancer patients. Br J Health Psychol 8(Pt3):271–286
Brain K, Williams B, Iredale R, France L, Gray J (2006) Psychological distress in men with breast cancer. J Clin Oncol 24(1):95–101
France L, Michie S, Barrett-Lee P et al (2000) Male cancer: a qualitative study of male breast cancer. The Breast 9:343-348
Peate I (2001) Caring for men with breast cancer: causes, symptoms and treatment. Br J Nursing 10(15):975–981
Williams BG, Iredale R, Brain K et al (2003) The experiences of men with breast cancer: an exploratory focus group study. Br J Cancer 89:1834–1836
Auvinen A, Curtis RE, Ron E (2002) Risk of subsequent cancer following breast cancer in men. J Natl Cancer Inst 94(17):1330–1332
O’Malley CD, Prehn AW, Shema SJ, Glaser SL (2002) Racial/ethnic differences in survival rates in a population-based series of men with breast carcinoma. Cancer 94(11):2836–2843
Yildirim E, Berberoglu U (1998) Male breast cancer: a 22-year experience. Eur J Surg Oncol 24(6):548–552
Salvadori B, Saccozzi R, Manzari A et al (1994) Prognosis of breast cancer in males: an analysis of 170 cases. Eur J Cancer 30A(7):930–935
El-Tamer MB, Komenaka IK, Troxel A et al (2004) Men with breast cancer have better disease-specific survival than women. Arch Surg 139(10):1079–1082
Scott-Conner CEH, Jochimsen PR, Menck HR, Winchester DJ (1999) An analysis of male and female breast cancer treatment and survival among demographically identical pairs of patients. Surgery 126(4):775–781
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Agrawal, A., Ayantunde, A.A., Rampaul, R. et al. Male breast cancer: a review of clinical management. Breast Cancer Res Treat 103, 11–21 (2007). https://doi.org/10.1007/s10549-006-9356-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-006-9356-z