Abstract
Objectives
A lifelong phenylalanine-restricted diet with supplementation of a phenylalanine-free amino acid formula is recommended in patients with phenylketonuria (PKU). The effect of a long-term PKU diet on renal function and blood pressure has not been investigated yet.
Design
We analyzed renal function in 67 patients with PKU, aged 15–43 years, by measuring glomerular filtration rate (GFR) and effective renal plasma flow by isotope clearance (51Cr-EDTA, 123J-Hippuran), estimated GFR, blood retention parameters, urinary protein and electrolyte excretion. Renal ultrasound and 24 h ambulatory blood pressure monitoring were performed additionally. Patients were divided into three groups according to their: 1) current diet (CD), i.e., daily protein intake: ICD <0.8 g/kg, IICD 0.8–1.04 g/kg, IIICD >1.04 g/kg; 2) life-long diet time (LDT), i.e., cumulative years of life in which daily protein intake exceeded dietary recommendations: ILDT <15 years, IILDT 15–19 years, IIILDT >19 years.
Results
GFR was decreased in 19 % of the patients. With increasing protein intake, GFR decreased significantly (ICD 111 ml/min; IICD 105 ml/min; IIICD 99 ml/min. ILDT 112 ml/min; IILDT 103 ml/min; IIILDT 99 ml/min). Proteinuria was detected in 31 %, microalbuminuria in 7 %, and hypercalciuria in 23 % of the patients. 23 % of the patients had arterial hypertension, and 41 % revealed a nocturnal non-dipping status.
Conclusions
In patients with PKU on a lifelong diet we could detect impaired renal function in 19 %, proteinuria in 31 %, and arterial hypertension in 23 %. Thus, chronic kidney disease may develop in PKU patients, and routine renal function tests should be performed during long-term follow-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Phenylketonuria (PKU, MIM 261600) is a rare autosomal recessive inborn error of metabolism caused by phenylalanine-4-hydroxylase (PAH, EC 1.14.16.1) deficiency (Scriver and Kaufman 2001). In untreated children, PKU results in severe neurological impairment with mental retardation, seizures, and behavioral disorders. Normal mental and motor activity skills can be achieved by early institution of a phenylalanine (Phe)-restricted diet consisting of a strong restriction of natural protein intake and substitution with a Phe-free L-amino acid (AA) formula (Scriver and Kaufman 2001). The Phe-restricted diet consists of foods with low protein content, e.g., vegetables, fruits and special low-protein food products. Most of the protein supply in PKU patients, e.g., 75–95 % of the whole protein intake, derives from the prescribed Phe-free AA formula (Mönch et al 1996). The allowed amount of the daily natural protein intake is dependent on the individual residual PAH enzyme activity corresponding to the severity of the disease. At the current state of knowledge, diet is recommended to be kept life-long.
To prevent a nutritional deficiency in essential AA, patients with PKU receive high amounts of the AA formula (Krauch et al 1996). Thus, protein intake in patients with PKU almost entirely consists of the AA formula, and often exceeds the current recommended daily allowance (RDA) for the general population, especially during the first years of life (D-A-CH Empfehlung 2000; Acosta et al 1998; Arnold et al 2002; Hoeksma et al 2005). AA formulas consist of synthetic mono AA, which have a lower biological efficacy than natural protein. The intake of the synthetic AA leads to peak plasma AA concentrations shortly after ingestion resulting in a high renal acid load (Mönch et al 1996; Manz et al 1977). This is in marked contrast to the stable plasma AA concentrations after the intake of intact natural protein (Gropper et al 1993).
Dietary protein is a well known modulator of kidney function (Brenner et al 1982; King and Levey 1993). The hyperfiltration theory suggests that protein consumption acutely results in an increase of renal plasma flow and glomerular filtration rate (GFR), leading to hyperfiltration and hypertension, thus resulting in chronic glomerular injury, fibrosis and mesangial cell proliferation (Bernstein et al 2007; Brenner et al 1996). In animal experiments, a high protein diet resulted in renal and glomerular enlargement, collagen deposition and tubulointerstitial infiltration, leading to cortical fibrosis and glomerulosclerosis (Jia et al 2010). In adult patients with chronic kidney disease (CKD), a low protein diet has been recommended to delay the progression of renal failure (Brenner et al 1982; Fouque and Aparicio 2007; Schena 2011).
Patients with PKU have to keep a life-long Phe-restricted diet, but it is unknown whether the relatively high total protein intake with the high proportion of synthetic AA may have an effect on renal function. We have therefore investigated the effect of the PKU diet on renal structure, function and blood pressure (BP) in adolescent and adult patients with PAH deficiency.
Study population and methods
Study population
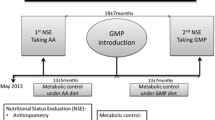
Eighty patients with PKU treated in the metabolic unit of the Department of Pediatrics at the Charité Berlin were eligible for this cross-sectional study evaluating clinical and biochemical data, ultrasound studies, renal function, 24-h ambulatory blood pressure monitoring (ABPM), and dietary history. Exclusion criteria were: age <15 years, pregnancy or breastfeeding. Of a total of these 80 patients, 13 refused participation completely and 28 patients refused participation in some parts of the study. Therefore, of the 67 patients participating in the study, ultrasound was performed in 61 patients, ABPM in 44 patients and radio-isotope clearance studies in 59 patients. Informed consent was obtained from all patients and/or their parents.
The median age of the patients was 24 years (15–43 years) with 38 females and 29 males. According to established criteria (Guldberg et al 1998; Güttler and Guldberg 1994), 60 % of the patients were classified as classic PKU (n = 40), 37 % as mild PKU (n = 25) and 3 % as hyperphenylalaninemia (n = 2). Fifty-eight patients were diagnosed by newborn screening, nine patients were diagnosed by selective screening at a median age of 42 months (3–171 months). In total, we collected data of cumulative 1600 patient-years.
Chart review showed that dietary treatment had been started in all patients immediately after diagnosis of PKU. At the time of examination, 82 % of the patients (n = 55) kept a Phe-restricted diet with supplementation of a Phe-free AA formula, 3 % (n = 2) kept a diet low in natural protein without additional AA formula, and 15 % (n = 10) had stopped adhering to the diet. Protein intake was calculated regularly by three-day-dietary-protocols. At the time of examination AA formula was applied thrice a day (AA formulas and hydrolysates supplemented in the patients are shown in Supplementary Table 1).
Methods
Clinical examination including body mass index (BMI) was performed in every patient. According to the World Health Organization “overweight” was defined as a BMI equal to or more than 25, and “obesity” as a BMI equal to or more than 30. ABPM was performed by using Model 90207(−32), Spacelabs Medical (USA). Arterial hypertension was defined according to established criteria as a daytime average above systolic 135 mmHg and/or systolic 85 mmHg (Parati and Pickering 2009; O’Brien et al 2005; Wühl et al 2002). A decrease of systolic BP during nocturnal time by ≥10 % of the diurnal BP was defined as a “dipper”, a decrease of <10 % as a “non-dipper” (Kastarinen et al 2010). In three patients without nocturnal sleeping phase during ABPM, “dipping”-/“non-dipping”-status was not discriminated. Renal ultrasound was performed with a 50/60 Hz transducer (Sonoline Antares, Siemens, Germany).
Laboratory analysis was performed in the fasting state in all patients and included the determination of serum creatinine, urea, uric acid, cystatin C, blood gases, electrolytes, total protein, albumin, vitamin D status and parathormone. Excretion of creatinine, protein, albumin, alpha-1-microglobuline, immunglobulin G, glucose, and electrolytes was analyzed in a 24-h urine collection. AA in plasma and urine were measured by cation exchange chromatography (Biotronic/Eppendorf). Plasma Phe was analyzed regularly in all study patients, according to the German recommendations for the treatment in PKU (Burgard et al 1999).
Renal function was determined by radio-isotope clearance: 80 kBq 51Cr-EDTA/kg and 15 kBq 123J-Hippuran/kg were simultaneously applied intravenously, and measured 30 min after application in a 2.0 ml plasma sample. 51Cr-EDTA clearance was used to evaluate GFR, 123J-Hippuran clearance to evaluate effective renal plasma flow (ERPF), and the ratio of 51Cr-EDTA/123J-Hippuran clearances to evaluate the filtration fraction (Hüseman et al 1999). Upper and lower cut off levels of GFR and ERPF were defined as ±2 SD. Additional informed consent for performing radio-isotope clearance was obtained from all patients and/or their parents.
The estimated GFR (eGFR) was calculated using the formula of Schwartz for adolescent patients ≤16 years (n = 6) and the “modification of diet in renal disease” (MDRD) formula for adult patients (n = 61) (Kooman 2009; Schwartz et al 2009; Staples et al 2010). Urinary creatinine clearance was not evaluated, since inaccuracy of sampling might have resulted in a falsely low estimation of GFR.
PAH genotype was determined in 60 patients, as previously described (Hennermann et al 2000). According to their genotype patients were classified into two different groups. Group 1: patients with two null mutations, corresponding to a complete loss of residual PAH activity; group 2: patients with at least one putative milder mutation, corresponding to a certain residual PAH activity. In three patients only one mutation was identified; they were not included in any group.
Statistics
For statistic analyses PASW Statistics, Version 18.0, was used. Differences between patients groups were analyzed by non-parametric tests, the Mann-Whitney-test, and the Jonckheere-Terpstra test. Significance of correlations of variables was tested with the Spearman-Rho-correlation coefficient. Multiple forward stepwise regression analysis was performed to analyze the significance of effects of several variables on the outcome variable, GFR measured by isotope clearance.
Results
Protein intake
Median current total protein intake in all 67 PKU patients was 0.96 ± 0.23 g/kg/day. Current total protein intake was 1.01 ± 0.23 g/kg/day in patients on a Phe-restricted diet with AA formula (n = 55), 0.57 ± 0.01 g/kg/day in patients on a low protein diet without AA formula (n = 2), and 0.75 ± 0.00 g/kg/day in patients off PKU diet (n = 10).
According to their dietary protein intake, patients were divided into three groups: according to the amount of their current diet (CD), and according to their life-long diet time (LDT). CD was determined by the amount of total daily protein intake and daily AA intake (Table 1). LDT was determined by the number of cumulative years of life in which the daily protein intake has exceeded German RDA of 1985 (DGE Empfehlung 1985) (Table 2).
Clinical examination
Clinical examinations revealed no significant abnormalities in any patient. Median BMI was 23.9 ± 4.8 kg/m2 and was increased in 25/67 patients (37.3 %). Sixteen patients (23.9 %) were overweight, nine patients were obese (13.4 %). There was an inverse correlation between BMI and actual total and synthetic protein intake (p = 0.000; r = −0.470, r = −0.421, respectively). None of the patients was suffering from any other inborn error of metabolism or from insulin dependent or non-insulin dependent diabetes.
Renal ultrasound
Renal ultrasound revealed bilateral nephrocalcinosis in 1/61 patient, associated with increased calcium excretion. Increased renal echogenity was found in 4/61 patients (6.6 %), associated with arterial hypertension and increased calcium excretion in 3/4. None of these patients received calcium supplementation. One patient showed unilateral polycystic changes, one patient a renal position abnormality. The size of both kidneys was within normal range with a mean size of 10.7 ± 0.75 cm (left), and 10.4 ± 0.78 cm (right), respectively, and correlated significantly with serum creatinine (p = 0.041).
Hypertension
Mean 24-h systolic BP was 127.0 ± 14.1 mmHg (105–182 mmHg), diastolic BP 77.6 ± 9.6 mmHg (58–118 mmHg), and MAD 93.4 ± 10.4 mmHg (73–138 mmHg). Arterial hypertension was diagnosed in 22.7 % of the patients (10/44). 41 % of the patients (17/41) revealed a nocturnal non-dipping status. Neither arterial pressure nor dipping status were correlated with GFR, eGFR, protein intake (CD, LDT), or proteinuria. There was a significant correlation of all BP parameters with BMI (p = 0.000; r = 0.510).
GFR
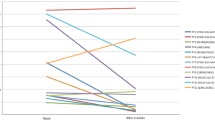
GFR measured by 51Cr-EDTA was 107 ± 15.5 ml/min/1.73 m2 (range 64–149; norm 95–161). GFR was decreased in 18.6 % of the patients (n = 11) and normal in 81.4 % of the patients (n = 48). ERPF measured by 123J-Hippuran was 707 ± 159 ml/min/1.73 m2 (range 426–1197; norm 515–916), and revealed an increase corresponding to hyperfiltration in four patients (6.8 %), a decrease in five patients (8.5 %), and normal values in 50 patients (84.7 %). ERPF correlated significantly with GFR (p = 0.000; r = 0.512). Filtration fraction was increased in five patients (8.5 %) and normal in 54 patients (91.5 %). GFR decreased significantly with increasing protein intake, both was correlated with CD and LDT (Figs. 1, 2, and 3). GFR was associated with BMI (p = 0.025; r = 0.295); in contrast, there was no correlation of GFR with the patient’s age. Neither ERPF nor filtration fraction were correlated with CD or LDT. Data of patients with diminished GFR are included in Supplementary Table 2.
51Cr-EDTA related to current total protein intake 51Cr-EDTA was measured in 59 patients. Median 51Cr-EDTA was 111 ml/min in the group with the lowest total protein intake (I-CD), 105 ml/min in the group with the medium total protein intake (II-CD), and 99 ml/min in the group with the highest total protein intake (III-CD). The correlation of 51Cr-EDTA with current total protein intake was significant (p = 0.008; r = 0.341)
51Cr-EDTA related to current AA intake (synthetic protein intake) 51Cr-EDTA was measured in 59 patients. Median 51Cr-EDTA was 111 ml/min in the group with the lowest AA intake (I-CD), 105 ml/min in the group with the medium AA intake (II-CD), and 100 ml/min in the group with the highest AA intake (III-CD). The correlation of 51Cr-EDTA with current AA intake was significant (p = 0.011; r = −0.331)
51Cr-EDTA related to life-long-diet 51Cr-EDTA was measured in 59 patients. Median 51Cr-EDTA was 112 ml/min in the group with the lowest life-long protein intake (I-LDT), 103 ml/min in the group with the medium life-long protein intake (II-LDT), and 99 ml/min in the group with the highest life-long protein intake (III-LDT). The correlation of 51Cr-EDTA with life-long-diet was significant (p = 0.003; r = −0.410)
The eGFR correlated significantly with 51Cr-EDTA (Fig. 4). eGFR was 108 ± 18.1 ml/min/1.73 m2 (range 74–157; norm 90–160). eGFR was decreased in 10.4 % of the patients (n = 7) and normal in 89.6 % of the patients (n = 60). The eGFR did not correlate with CD, LDT or BMI.
By multiple forward stepwise regression analysis, only proteinuria and the current total protein intake were independent predictors of the GFR estimated by isotope clearance (p < 0.005; r 2 = 0.201).
Creatinine and cystatin C serum concentrations were within normal ranges in all patients. There was a significant correlation between serum creatinine and 51Cr-EDTA (p = 0.000; r = 0.519). Both, creatinine and cystatin C, increased non-significantly with increasing protein consumption.
Proteinuria and Phe excretion
Mean serum levels of protein and albumin were within normal ranges. Proteinuria, defined as a protein excretion of >150 mg/24 h (Guy et al 2009), was found in 19/62 patients (30.6 %). Microalbuminuria, defined as an albumin excretion of 30–300 mg/g creatinine (Blecker et al 2011), was detected in 4/62 patients (6.5 %). Proteinuria was not correlated to BMI. The excretion of alpha-1-microglobulin was increased in one patient (18.3 mg/g creatinine), the excretion of immunglobulin G in two patients (maximum 25.1 mg/g creatinine).
Urinary AA analysis revealed no hyperaminoaciduria in any patient. Urinary Phe concentrations were increased to 0.713 ± 0.375 mmol/g creatinine (range 0.087–2.429; norm <0.19) and correlated significantly with actual and life-long Phe plasma concentrations (p = 0.000, p = 0.001; r = 0.727, r = 0.488, respectively). Urinary Phe excretion correlated significantly with GFR (p = 0.011; r = 0.332), proteinuria (p = 0.007; r = 0.338), and systolic BP (p = 0.040; r = 0.311). Actual Phe plasma levels were 796 ± 317 μmol/L (range 169–2,143; recommendations for PKU patients >15 years 40–1,200) and exceeded actual German recommendations in only 4/67 patients. However, actual or life-long plasma Phe concentrations did not correlate with GFR, eGFR, proteinuria, or BP.
Calcium, phosphate, hypercalciuria and vitamin D
Serum calcium was slightly increased in 3/61 patients (4.9 %), and serum phosphate was decreased in 3/59 patients (5.1 %). Calcium excretion was 0.17 ± 0.09 g/g creatinine (range 0.04–0.54; norm <0.2) and was increased in 22.7 % of the patients (15/66). Renal tubular reabsorption of phosphate (TmP/GFR) was within the normal range (0.96 ± 0.27 mmol/L; norm 0.6–1.7 mmol/L). In only two patients, both, calcium and phosphate excretion were increased. The serum calcium phosphate product was normal in all patients. An increase in calcium excretion was significantly associated with CD, mainly with actual synthetic AA intake (Fig. 5), but there was no correlation to LDT. Phosphate reabsorption was not correlated to CD or LDT. Venous blood gas analysis revealed no abnormalities in any patient.
Calcium excretion related to current synthetic protein intake calcium excretion was measured in 66 patients. Median urinary calcium concentration was 0.15 g/g creatinine in the group with the lowest AA intake (I-CD), 0.12 g/g creatinine in the group with the medium AA intake (II-CD), and 0.21 g/g in the group with the highest AA intake (III-CD). The correlation of calcium excretion and current synthetic protein intake (AA intake) was significant (p = 0.008)
Mean parathormone concentrations were 2.89 ± 1.11 pmol/L (norm 1.6–6.9 pmol/L) and revealed no signs of hyperparathyreoidism. The 25-hydroxy-vitamin D(3) serum levels were within the normal range (24.3 ± 8.8 ng/ml; norm 9.2–45.2 ng/ml). Mean 1,25-dihydroxy-vitamin D(3) serum levels were 50.4 ± 17.7 ng/L (norm 17–53 ng/L) and were increased in 24/64 patients (median: 69.6 ng/L, range: 56–113 ng/L), 21 of them on synthetic AA substitution (which contained 0.13–0.2 μg vitamin D3/gram protein). However, there was no correlation between nutritional supply with D3 and either 25-hydroxy-vitamin D(3) or 1,25-dihydroxy-vitamin D(3) levels. Vitamin D deficiency was not diagnosed in any of the patients. There was no correlation between vitamin D3 intake and hypercalciuria.
PAH genotype
34/57 patients carried two null mutations (genotype group 1), 23/57 patients carried at least one putative milder PAH mutation (genotype group 2). No significant differences between both groups were found for CD, LTD, GFR, eGFR, and proteinuria (Table 3).
Discussion
Dietary protein is a well known modulator of kidney function (Brenner et al 1982; King and Levey 1993). The effect of the PKU diet, which is characterized by a relative high protein content with a high proportion of synthetic AA, on renal function has not been previously examined. We show that adolescent and adult PKU patients may develop CKD (impaired renal function, proteinuria) and arterial hypertension. In contrast, CKD in the general population is mainly prevalent at older ages (Zhang and Rothenbacher 2008).
The RDA for the daily protein intake has changed within the last decades, and a lower nutritional protein intake is currently recommended (D-A-CH Empfehlung 2000; DGE Empfehlung 1985; DGE Empfehlung 1991). Although median total protein intake in PKU patients exceeded these RDA, the amount of total protein intake was still within the range of a typical Western diet and, thus, may not account for the development of CKD in our patients (Fouque and Aparicio 2007; Halbesma et al 2009). However, we could demonstrate that GFR decreased significantly with increasing total protein and increasing AA intake, both related to CD as well to LDT. Overall, we found hyperfiltration in only 7 % of the patients, but a decrease of GFR in 19 % of the patients. Although Phe might interfere with renal clearance of hippurate due to the competition for renal anion transporters (Enomoto and Niwa 2007), there were no correlations with plasma or urine Phe values and ERPF measured by 123J-Hippuran.
Importantly, protein composition in PKU diet differs from that of healthy population and mainly derives from the synthetic AA formula. Ingestion of AA formula results in plasma peak AA concentrations (Mönch et al 1996; Gropper et al 1993), and high plasma AA concentrations have been shown to be nephrotoxic in animals, resulting in a significant decrease of GFR, an increase in albuminuria and histological changes consistent with tubular damage (Zager et al 1983). A similar pathomechanism may account for the renal damage in PKU patients.
An increase in renal protein excretion was detected in more than 30 % of the PKU patients, and microalbuminuria in 7 % of the patients. Multivariant linear regression analysis revealed a significant association of GFR measured by 51Cr-EDTA with both, current total protein intake and proteinuria, indicating that protein intake and proteinuria are involved independently in the pathomechanism of renal injury in phenylketonuric patients.
Arterial hypertension was found in one fourth of the PKU patients, reflecting an important secondary health problem in PKU patients. Furthermore, 40 % of the patients revealed a nocturnal non-dipping status, which is known to be associated with CKD (Kastarinen et al 2010). Arterial BP was significantly associated with BMI, but not with actual or lifelong protein intake, GFR or proteinuria. More than one third of the examined patients revealed an increase in BMI. It has been reported before that obesity is a common problem in PKU patients (MacDonald et al 2011). Though, it is our experience and that of others that caloric intake in PKU patients is within normal limits (Acosta 1996). An increase in BMI in PKU patients may be due to inadequate energy expenditure (Acosta et al 2003; White et al 1982). Furthermore, our data reveal that BMI is inversely correlated with the actual total and synthetic protein intake. Obesity is a known risk factor for glomerulosclerosis (Kambham et al 2001), which is reflected by our data, revealing an association of BMI and GFR. Though, BMI was not associated proteinuria in our study. Hence, obesity is a further risk factor for CKD in PKU patients.
Calcium excretion significantly increased with increasing protein intake, mainly with increasing synthetic AA intake, whereas the time of the lifelong diet (LDT) seemed not to influence calcium excretion. A high protein intake is associated with an increase in calcium excretion (Itoh et al 1998). An increase in calcium excretion (found in 23 % of patients) could imply an additional long-term risk for PKU patients on the current diet. However nephrocalcinosis was rarely observed and the presence of hypercalciuria was not associated with diminished GFR, proteinuria or hypertension. 1,25-dihydroxy-vitamin D(3) serum concentrations were increased in 38 % of the PKU patients, but there was no correlation between the nutritional vitamin D3 supply with either 25-hydroxy-vitamin D(3) or 1,25-dihydroxy-vitamin D(3) levels. However, 1,25-dihydroxy-vitamin D(3) levels are tightly regulated on the level of synthesis, independent of nutritional supply (Anderson et al 2004). Furthermore, an increase in vitamin D(3) serum concentrations was not associated with hypercalciuria. Although actual recommendations indicate a higher vitamin D intake in adolescents and adults (German Nutrition Society 2012), none of our patients had vitamin D deficiency.
Several putative pathomechanism could explain the association of (synthetic) protein intake and a decrease in renal function. First, Phe excretion was significantly correlated with GFR and proteinuria. Although a nephrotoxic effect of Phe has not been described yet, renal damage by high urinary Phe concentrations may contribute to the development of CKD in PKU. Second, increased oxidative stress has been demonstrated in PKU patients and attributed to an increased free radical generation, a deprivation of micronutrients or an increase of phenylalanine and its metabolites (Sirtori et al 2005; Sitta et al 2009; Ribas et al 2011). Therefore, oxidative stress could be involved in the pathophysiology of the tissue damage and chronic renal injury found in PKU. Third, it has been postulated that human kidney PAH may play a significant role in phenylalanine homeostasis. PAH has been shown to be expressed in human kidneys (Lichter-Konecki et al 1999), and impaired phenylalanine hydroxylation has been observed in renal failure (Zhao et al 2012). Thus, renal PAH expression could influence renal function in PKU patients, although in our study an association with the PAH genotype could not be found. In contrast, hyperfiltration, a well-known mediator of renal injury associated with a high protein intake (Bernstein et al 2007; Brenner et al 1996), was not observed in our patient’s cohort.
CKD in patients with PKU may benefit from an early start of treatment. Although the effects of a low-protein diet on the progression of CKD has been the subject of controversy, a protein restriction of 0.6–0.8 g/kg/day is recommended in adult patients with end-stage CKD (Fouque and Aparicio 2007). In contrast, a protein-restricted diet seems to have no significant impact on the progression of CKD in children (Wingen et al 1997; Chaturvedi and Jones 2007). Thus, at the current state of knowledge, recommendations for protein intake in PKU patients with CKD are difficult to establish. However, given the potential nephrotoxicity of AA, we recommended substitution of the AA formula in at least three daily doses (Mönch et al 1996). In addition to dietary protein restriction, ACE inhibitors or angiotensin-receptor blockers were shown to have a beneficial effect on progression of CKD (Kriz 2004). Therapy with these drugs could be beneficial in view of the high incidence of arterial hypertension in patients with PKU; however, efficacy of such treatment remains to be established in this patient population.
Conclusions
In conclusion, we found a high prevalence of proteinuria, decreased GFR, hypercalciuria, and arterial hypertension in adolescent and adult PKU patients. An increased intake of protein with a high content of synthetic AA due to lifelong prescription of a PKU diet and the presence of proteinuria were independently associated with the decrease in GFR. Although GFR was within the normal range in the whole group of patients, there was a continuous and graded relationship of both, CD and LTD, with decreasing GFR. The intake of high amounts of synthetic AA, increased oxidative stress, and local damage through high Phe excretion may contribute to renal damage in PKU. Arterial hypertension was mainly explained by increased BMI and unrelated to protein intake or proteinuria. Altogether, PKU patients constitute a high risk group for the development of CKD.
Abbreviations
- AA:
-
Amino acids
- ABPM:
-
Ambulatory blood pressure monitoring
- BMI:
-
Body mass index
- BP:
-
Blood pressure
- CD:
-
Current diet
- CKD:
-
Chronic kidney disease
- eGFR:
-
Estimated glomerular filtration rate
- ERPF:
-
Effective renal plasma flow
- GFR:
-
Glomerular filtration rate
- LDT:
-
Life-long diet time
- PAH:
-
Phenylalanine hydroxylase
- Phe:
-
Phenylalanine
- PKU:
-
Phenylketonuria
- RDA:
-
Recommended daily allowance
References
Acosta PB (1996) Recommendations for protein and energy intakes by patients with phenylketonuria. Eur J Pediatr 155(Suppl 1):S121–S124
Acosta PB, Yannicelli S, Marriage B et al (1998) Nutrient intake and growth of infants with phenylketonuria undergoing therapy. J Pediatr Gastroenterol Nutr 27:287–291
Acosta PB, Yanicelli S, Singh R et al (2003) Nutrient intakes and physical growth of children with phenylketonuria undergoing nutrition therapy. J Am Diet Assoc 103:1167–1173
Anderson PH, O’Loughlin PD, May BK, Morris HA (2004) Determinants of circulating 1,25-dihydroxyvitamin D3 levels: the role of renal synthesis and catabolism of vitamin D. J Steroid Biochem Mol Biol 89–90:111–113
Arnold GL, Vladutiu CJ, Kirby RS, Blakely EM, Deluca JM (2002) Protein insufficiency and linear growth restriction in phenylketonuria. J Pediatr 141:243–246
Bernstein AM, Treyzon L, Li Z (2007) Are high-protein, vegetable based diets safe for kidney function? A review of the literature. J Am Diet Assoc 107:644–650
Blecker S, Matsushita K, Köttgen A et al (2011) High-normal albuminuria and risk of heart failure in the community. Am J Kidney Dis 58:47–55
Brenner BM, Meyer TW, Hostetter TH (1982) Dietary protein intake and the progressive nature of kidney disease. N Engl J Med 307:652–659
Brenner BM, Lawler EV, Mackenzie HS (1996) The hyperfiltration theory: a paradigm shift in nephrology. Kidney Int 49:1774–1777
Burgard P, Bremer HJ, Bührdel P et al (1999) Rationale for the German recommendations for phenylalanine level control in phenylketonuria 1997. Eur J Pediatr 158:46–54
Chaturvedi S, Jones C (2007) Protein restriction for children with chronic renal failure. Cochrane Database Syst Rev 17(4):CD006863
DGE Empfehlung: Deutsche Gesellschaft für Ernährung (1985) Empfehlungen für die Nährstoffzufuhr: Umschau Verlag
DGE Empfehlung: Deutsche Gesellschaft für Ernährung (1991) Empfehlungen für die Nährstoffzufuhr: Umschau/Braus
D-A-CH Empfehlung: Deutsche Gesellschaft für Ernährung, Österreichische Gesellschaft für Ernährung, Schweizerische Gesellschaft für Ernährungsforschung, Schweizerische Vereinigung für Ernährung (2000) Referenzwerte für die Nährstoffzufuhr: Umschau/Braus
Enomoto A, Niwa T (2007) Roles of organic anion transporters in the progression of chronic renal failure. Ther Apher Dial 11(Suppl 1):S27–S31
Fouque D, Aparicio M (2007) Eleven reasons to control the protein intake of patients with chronic kidney disease. Nat Clin Pract Nephrol 3:383–392
German Nutrition Society (2012) New reference values for vitamin D. Ann Nutr Metab 60:241–246
Gropper SS, Gropper DM, Acosta PB (1993) Plasma amino acid response to ingestion of L-amino acids and whole protein. J Pediatr Gastroenterol Nutr 16:143–150
Guldberg P, Rey F, Zschocke J et al (1998) A European multicenter study of phenylalanine hydroxylase deficiency: classification of 105 mutations and a general system for genotype-based prediction of metabolic phenotype. Am J Hum Genet 63:71–79
Güttler F, Guldberg KF (1994) Mutations in the phenylalanine hydroxylase gene: genetic determinants for the phenotypic variability of hyperphenylalaninemia. Acta Paediatr 407(Suppl):46–56
Guy M, Borzomato JK, Newall RG, Kalra PA, Price CP (2009) Protein and albumin-to-creatinine ratios in random urines accurately predict 24 h protein and albumin loss in patients with kidney disease. Ann Clin Biochem 46:468–476
Halbesma N, Bakker SJ, Jansen DF et al (2009) High protein intake associates with cardiovascular events but not with loss of renal function. J Am Soc Nephrol 20:1797–1804
Hennermann JB, Vetter B, Wolf C et al (2000) Phenylketonuria and hyperphenylalaninemia in Eastern Germany: a characteristic molecular profile and 15 novel mutations. Hum Mut 15:254–260
Hoeksma M, Van Rijn M, Verkerk PH et al (2005) The intake of total protein, natural protein and protein substitute and growth of height and head circumference in Dutch infants with phenylketonuria. J Inherit Metab Dis 28:845–854
Hüseman D, Gellermann J, Vollmer I et al (1999) Long-term prognosis of hemolytic uremic syndrome and effective renal plasma flow. Pediatr Nephrol 13:672–677
Itoh R, Nishiyama N, Suyama Y (1998) Dietary protein intake and urinary excretion of calcium: a cross-sectional study in a healthy Japanese population. Am J Clin Nutr 67:438–444
Jia Y, Hwang SY, House JD, Ogborn MR, Weiler HA, Karmin O, Aukema HM (2010) Long-term high intake of whole proteins results in renal damage in pigs. J Nutr 140: 1646–1652
Kambham N, Markowitz GS, Valeri AM (2001) Obesity-related glomerulopathy: an emerging epidemic. Kidney Int 59:1498–1509
Kastarinen H, Vasunta RL, Ukkola O, Kesäniemi YA (2010) Glomerular filtration rate is related to dipping pattern in ambulatory blood pressure monitoring—a cross-sectional population-based study. J Hum Hypertens 24:247–253
King AJ, Levey AS (1993) Dietary protein and renal function. J Am Soc Nephrol 3:1723–1737
Kooman JP (2009) Estimation of renal function in patients with chronic kidney disease. J Magn Reson Imaging 30:1341–1346
Krauch G, Müller E, Anninos A, Bremer HJ (1996) Comparison of the protein quality of dietetically treated phenylketonuria patients with the recommendations of the WHO expert consultation. Eur J Pediatr 155(Suppl 1):S153–S157
Kriz W (2004) Podocytes as a target for treatment with ACE inihibitors and/or angiotensin-receptor blockers. Kidney Int 65:333–334
Lichter-Konecki U, Hipke CM, Konecki DS (1999) Human phenylalanine hydroxylase gene expression in kidney and other nonhepatic tissues. Mol Genet Metab 67:308–316
MacDonald A, Rocha JC, van Rijn M, Feillet F (2011) Nutrition in phenylketonuria. Mol Genet Metab 104(Suppl):S10–S18
Manz F, Schmidt H, Schärer K, Bickel H (1977) Acid-base status in dietary treatment of phenylketonuria. Pediatr Res 11:1084–1087
Mönch E, Herrmann ME, Brösicke H, Schöffer A, Keller M (1996) Utilisation of amino acid mixtures in adolescents with phenylketonuria. Eur J Pediatr 155(Suppl 1):S115–S120
O’Brien E, Asmar R, Beilin L et al (2005) Practice guidelines of the European Society of Hypertension for clinic, ambulatory and self blood pressure measurement. J Hypertens 23:697–701
Parati G, Pickering TG (2009) Home blood-pressure monitoring: US and European consensus. Lancet 373:876–878
Ribas GS, Sitta A, Wajner M, Vargas CR (2011) Oxidative stress in phenylketonuria: what is the evidence? Cell Mol Neurobiol 31:653–662
Schena FP (2011) Management of patients with chronic kidney disease. Intern Emerg Med 6(Suppl 1):77–83
Schwartz GJ, Muñoz A, Schneider MF et al (2009) New equations to estimate GFR in children with CKAD. J Am Soc Nephrol 20:629–637
Scriver CR, Kaufman S (2001) Phenylalanine hydroxylase deficiency. In Scriver CR, Beaudet AL, Sly W, Valle D, Childs B, Vogelstein B (eds). The metabolic and molecular basis of inherited disease. McGraw-Hill, 1667–1724
Sirtori LR, Dutra-Filho CS, Fitarelli D et al (2005) Oxidative stress in patients with phenylketonuria. Biochim Biophys Acta 1740:68–73
Sitta A, Barschak AG, Deon M et al (2009) L-Carnitine blood levels and oxidative stress in treated phenylketonuric patients. Cell Mol Neurobiol 29:211–218
Staples A, LeBlond R, Watkins S, Wong C, Brandt J (2010) Validation of the revised Schwartz estimating equation in a predominantly non-CKD population. Pediatr Nephrol 25:2321–2326
White JE, Kronmal RA, Acosta PB (1982) Excess weight among children with phenylketonuria. J Am Coll Nutr 1:293–303
Wingen AM, Fabian-Bach C, Mehls O (1997) Randomised multicentre study of a low-protein diet on the progression of chronic renal failure in children. European study group of nutritional treatment of chronic renal failure in childhood. Lancet 349:1117–1123
Wühl E, Witte K, Soergel M, Mehls O, Schaefer F (2002) German working group on pediatric hypertension: distribution of 24-h ambulatory blood pressure in children: normalized reference values and role of body dimensions. J Hypertens 20:1995–2007
Zager RA, Johannes G, Tuttle SE, Sharma HM (1983) Acute amino acid nephrotoxicity. J Lab Clin Med 101:130–140
Zhang QL, Rothenbacher D (2008) Prevalence of chronic kidney disease in population-based studies: systematic review. BMC Publ Health 8:117
Zhao YY, Liu J, Cheng XL, Bai X, Lin RC (2012) Urinary metabonomics study on biochemical changes in an experimental model of chronic renal failure by adenine based on UPLC Q-TOF/MS. Clin Chim Acta 413:642–649
Acknowledgement
We thank all patients and their parents for the participation and for their cooperation. We are grateful to Christine Gebauer and Gudrun Heide who calculated dietary protocols and dietary protein intake of all patients included in the study.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by: Eva Morava
Eberhard Mönch and Uwe Querfeld both authors contributed equally to the study.
Rights and permissions
About this article
Cite this article
Hennermann, J.B., Roloff, S., Gellermann, J. et al. Chronic kidney disease in adolescent and adult patients with phenylketonuria. J Inherit Metab Dis 36, 747–756 (2013). https://doi.org/10.1007/s10545-012-9548-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10545-012-9548-0