Abstract
Pompe disease is a lysosomal storage disorder caused by acid α-glucosidase deficiency and characterized by progressive muscle weakness. Enzyme replacement therapy (ERT) has ameliorated patients’ perspectives, but reversal of skeletal muscle pathology remains a challenge. We studied pretreatment biopsies of 22 patients with different phenotypes to investigate to what extent fiber-type distribution and fiber-type-specific damage contribute to clinical diversity. Pompe patients have the same fiber-type distribution as healthy persons, but among nonclassic patients with the same GAA mutation (c.-32-13T>G), those with early onset of symptoms tend to have more type 2 muscle fibers than those with late-onset disease. Further, it seemed that the older, more severely affected classic infantile patients and the wheelchair-bound and ventilated nonclassic patients had a greater proportion of type 2x muscle fibers. However, as in other diseases, this may be caused by physical inactivity of those patients.
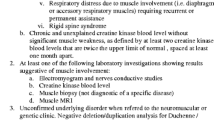
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pompe disease (glycogen storage disease type II, acid maltase deficiency) (OMIM 232300) is an inherited lysosomal storage disorder caused by the deficiency of acid α-glucosidase (EC 3.2.1.3). Deficiency of this lysosomal enzyme leads to glycogen accumulation in a variety of tissues, including skeletal muscle (Hirschorn and Reuser 2001; van der Ploeg et al. 2010). Pompe disease shows a broad clinical spectrum, ranging from the classic infantile form characterized by hypotonia, hypertrophic cardiomyopathy, and death within the first year of life (van den Hout et al. 2003; Kishnani et al. 2006), to more slowly progressive forms characterized by proximal muscle weakness and respiratory problems in children and adults (Winkel et al. 2005; Wokke et al. 2008).
Skeletal muscle weakness is attributed to the loss of mechanical force through deposition of the glycogen-loaded lysosomes between the contractile myofibrils, followed by muscle damage by lysosomal rupture and release of lysosomal enzymes into the cytoplasm (Hesselink et al. 2003; Griffin 1984; Thurberg et al. 2006). A study in infants with Pompe disease confirmed this view (Raben et al. 2010). In mice with Pompe disease and in affected adults, the accumulation of autophagic debris seems to aggravate skeletal muscle damage (Raben et al. 2010; Shea and Raben 2009; Fukuda et al. 2006). Unlike in mice, autophagic accumulation in humans is not restricted to type 2 muscle fibers but also involves type 1 fibers (Raben et al. 2010; Fukuda et al. 2006).
The introduction of enzyme replacement therapy (ERT) in 2006 changed the perspectives of patients with Pompe disease (van der Ploeg et al. 2010; Van den Hout et al. 2004; Kishnani et al. 2007, 2009; van Capelle et al. 2008; Strothotte et al. 2010); it largely solved the cardiac problem, but reversal of skeletal muscle pathology remains a challenge (Schoser et al. 2008). In a recent case report, we drew attention to the occurrence of fiber-type-specific pathology and its potential relevance for clinical presentation and responsiveness to ERT (van den Berg et al. 2011). In the study reported here, we assessed 22 patients with Pompe disease with regard to fiber-type distribution and fiber-type-specific damage in order to investigate to what extent this might contribute to clinical diversity.
Methods
This study was performed at the Erasmus MC University Medical Center in Rotterdam, The Netherlands, in collaboration with the Maastricht University, Maastricht, The Netherlands. The Ethical Committee of the Erasmus MC University Medical Center approved the research protocol. Written informed consent was obtained from all patients or their parents. Twenty-two patients were selected for this study, representing a cross-section of the Dutch Pompe patient population and divided over different groups (classic versus nonclassic Pompe disease, and the latter group subdivided in clearly distinct ages of onset: <15 years or >30 years). Diagnosis was in all cases established by clinical and biochemical assessments. Muscle biopsies, either open surgical biopsies or needle biopsies from the vastus lateralis, were taken just before the start of ERT.
Immunohistochemistry
Muscle biopsies were embedded in Tissue-Tek (Aurian, Wageningen, The Netherlands) and immediately frozen in melting isopentane. All tissue samples were stored at −80 °C until analysis. Immunostaining was performed on cryostat sections (5 μm). To identify muscle fiber types, we used two different staining procedures. The first identifies type 1 and type 2a fibers in combination with laminin. For this staining, we used the following primary monoclonal mouse antibodies: A4.840, anti-human myosin heavy-chain (MHC) type 1 [Developmental Studies Hybridoma Bank (DSHB), Iowa City, IA. USA]; N2.261, anti-human MHC type 2a (DSHB); and L-9393, anti-human laminin (Sigma, Zwijndrecht, The Netherlands). The second staining procedure identifies type 2x muscle fibers as opposed to type 1 plus type 2a fibers and laminin. The following primary antibodies were used for this staining: N2.261, anti-human MHC type 1 and type 2a (DSHB); 6H1, anti-human MHC type 2x (DSHB); and L-9393, anti-human laminin (Sigma, Zwijndrecht, The Netherlands). After incubation with the primary antibodies, sections were incubated with a mixture of appropriate conjugates, i.e., goat anti-mouse immunoglobulin G (IgM) Alexa-Fluor 555, goat anti-mouse IgG1 Alexa-Fluor 488, and goat anti-mouse IgG Alexa-Fluor 350. Images were obtained using a Nikon E800 fluorescence microscope (Nikon, Amsterdam, The Netherlands) coupled to a progressive scan color CCD camera (Basler 101C).
Analysis of stained tissue sections
To obtain a representative overview of a stained muscle section, ten images were taken at separate locations of a section using a 20× objective lens. This procedure enabled analysis of at least 25 fibers per image. The number of each of the different muscle fiber types was counted and the total number of type 2 muscle fibers was taken as the sum of type 2a and type 2x muscle fibers. The percentage surface area occupied by vacuoles was estimated with a planimetric method. The degree of muscle fiber vacuolation was scored in four categories: very severe, 100 –75 % vacuolated; severe, 74–50 % vacuolated; intermediate, 49–25 % vacuolated; mild or normal, 24–0 % vacuolated. Muscle fibers with >25 % of vacuoles were considered as damaged fibers. The total percentage of damaged muscle fibers was calculated, as was the percentage of damaged fibers per muscle fiber type.
Clinical parameters
Laboratory analysis
We analyzed nonfasting blood samples for serum concentrations of creatine kinase (CK) (normal values <295 U/L in infants; <230 U/L in young children; <270 U/L in teenage boys; <123 U/L in teenage girls; <200 U/L in men; <170 U/L in women).
Pulmonary function
Pulmonary function tests were performed in all patients >4 years. Pulmonary function was measured with spirometry in all patients while sitting, and in nonventilated patients also in supine position. Historical data were used for comparison.
Muscle strength
Muscle-strength measurements were performed in all patients >6 years, being measured in 12 muscle groups with a hand-held dynamometer (dynamometer type CT 3001- C.I.T. Technics). Maximum contraction values were assessed with the break technique in which the examiner applies adequate force to overcome the examinee, thereby producing an eccentric contraction. The values obtained for the different muscle groups were expressed as percentages of age- and sex-matched reference values. We used summed scores for total muscle force (neck flexors, neck extensors, shoulder abductors, elbow flexors, elbow extensors, wrist extensors, hip flexors, hip abductors, knee flexors, knee extensors, foot dorsiflexors, and foot plantar flexors) and proximal muscle force (shoulder abductors, elbow flexors and extensors, hip flexors and abductors, knee flexors and extensors). All muscle groups were assigned equal weight. Isometric muscle strength of the quadriceps femoris muscle was measured by quantitative muscle testing (QMT) on a Biodex ® isokinetic dynamometer (Model 2000, Multijoint System 3, Biodex Corporation, Shirley, NY, USA). Values obtained per group are expressed as percentages of age- and sex-matched reference values as provided by the manufacturer.
Fatigue assessment
This assessment was obtained in all adult patients. The severity and impact of fatigue was assessed using the Fatigue Severity Scale (FSS) (Krupp et al. 1989). The total FSS score is the average of the nine-item scores and ranges from 1 (no signs of fatigue) to 7 (most disabling fatigue).
Statistical analysis
Descriptive statistics are presented as mean ± standard deviation (SD). Student’s t test was used for comparison of means after validating normality assumptions. Nonparametric tests for independent samples (Mann–Whitney and Kruskal–Wallis tests) were used for the other variables. Pearson’s correlation coefficients were calculated to ascertain relationships between the percentage of damaged muscle fibers and age, disease duration at time of the biopsy, and clinical parameters. All analyses were performed using SPSS for Windows (version 15.0, SPSS Inc. Chicago, IL, USA). Two-sided P values <0.05 were considered significant.
Results
Patients
Muscle biopsies of 22 patients were selected for this study. Nine patients had the classic infantile form of Pompe disease (group 1), and 13 were nonclassic patients. Four of the latter 13 had their first symptoms before the age of 15 years (group 2). The other nine had their first symptoms after the age of 30 years; four of them were severely affected (group 3) and five were mildly affected (group 4) at the time the biopsy was taken. No patient had ever received ERT. Supplementary Table 1 summarizes patient characteristics.
Muscle-fiber typing
Classic infantile patients compared with nonclassic patients had a lower percentage of type 1 fibers (p 0.04) and a significantly higher percentage of type 2a muscle fibers (p < 0.01) (Supplementary Fig. 1). The latter difference was mainly due to the difference between infants (group 1), and adults >30 years (groups 3 and 4) (Fig. 1).
a Percentage of type 1 and type 2 muscle fibers and b type 2a and type 2x muscle fibers in classic infantile patients (group 1), patients with the IVS1 mutation and symptom onset before the age of 15 years (group 2), and mildly and severely affected patients with the IVS1 mutation and symptom onset after the age of 30 years (groups 3 and 4, respectively). b Group 1: 55.8 % ± 9.8 (37–73 %), group 3: 29.0 % ± 20.2 (10–47 %); group 4: 26.6 % ± 13.7 (3–39 %). Significance between the different groups of patients is shown by * (P < 0.05)
Figure 2 shows correlations between patients’ ages and muscle-fiber types. For the total group, a significant decrease of type 2a muscle fibers was found with increasing age (Fig. 2c, d; Spearman Rho −0.703, P < 0.001). In classic infantile Pompe patients, the decrease in the percentage of type 2a muscle fibers (Spearman Rho −0.773, P = 0.015) coincided with a significant increase in type 2x muscle fibers (Fig. 2c, e; Spearman Rho 0.950, P < 0.001).
a, b Type 1 muscle fibers, c, d type 2a, and e, f type 2x versus age in classic infantile patients and patients with the IVS1 mutation. Correlations are significant (P < 0.05) for age and type 2a muscle fibers in classic infantile patients (c Pearson’s r = −0.773) and for age and type 2x muscle fibers in classic infantile patients (e Pearson’s r = 0.950)
No significant differences in muscle-fiber-type distribution were found between ambulant and wheelchair-bound patients (Fig. 3a) or between ventilated and nonventilated patients (Fig. 3b). However, wheelchair-bound patients seemed to have a slightly higher percentage of type 2x muscle fibers than did ambulant patients. Also, ventilated patients seemed to have a slightly higher percentage of type 2x muscle fibers than did nonventilated patients.
Muscle-fiber damage
The left column of Table 1 shows that the percentage of muscle fibers with >25 % vacuolation (damaged fibers) did not differ between the four subgroups. The three columns at the right illustrate the percentage of damaged muscle fibers per muscle-fiber type. Damage of type 1 muscle fibers was more prominent in classic infantile Pompe disease than in nonclassic disease (P = 0.04). With regard to the degree of vacuolation, there were no significant differences between the four subgroups (Supplementary data, Table 2).
Although we did not find statistical differences in the percentage of damaged fibers or in the degree of vacuolation between subgroups, muscle biopsies of mildly (Fig. 4, left panels) and severely (Fig. 4, right panels) affected patients had a quite different appearance. Biopsies of the mildly affected patients showed normally shaped and neatly organized muscle fibers, whereas biopsies of the severely affected patients showed irregularly shaped and loosely organized muscle fibers.
Differences in appearance of muscle fibers in a classic infantile patient with an early diagnosis and b classic infantile patient with a late diagnosis; in a c mildly and d severely affected patient with the IVS1 mutation and symptom onset before 15 years of age; e mildly and f severely affected patient with the IVS1 mutation and symptom onset after 30 years of age. Fiber typing was performed with antibodies against myosin heavy-chain (MHC) type 1 (red) and MHC type 2a (green) fibers. MHC-negative regions within muscle fibers indicate the presence of vacuoles. Anti-laminin staining (blue) was used to mark fiber boundaries
Muscle-fiber damage and clinical parameters
Figure 5 shows correlations between percentage of damaged muscle fibers and the different clinical parameters. We found significant correlations between the percentage of damaged muscle fibers and (1) forced vital capacity (FVC) in the supine position (r = −0.862, P = 0.027), (2) proximal muscle strength tested by hand-held dynamometry (r = −0.762, P = 0.046), and (3) quadriceps femoris muscle strength by QMT (r = −0.744, P = 0.022). The correlation between the percentage of damaged muscle fibers and the total muscle strength by hand-held dynamometry was close to significant (r = −0.748, P = 0.053). Four patients were excluded from the analysis for muscle strength by hand-held dynamometry and two from the analysis for muscle strength of the quadriceps femoris muscle by QMT because data could not be obtained for some muscle groups.
a Forced vital capacity (FVC) in the supine position, b muscle strength of the quadriceps femoris, c muscle strength of the proximal muscles, and d total muscle strength versus percentage of damaged muscle fibers. Correlations are significant (P < 0.05) for FVC in supine position (a Pearson’s r = −0.862), muscle strength of the quadriceps femoris (b Pearson’s r = −0.744), and muscle strength of the proximal muscles (c Pearson’s r = −0.862). Total muscle strength showed a trend (d Pearson’s r = −0.748)
Severely affected nonclassic patients seemed to have lower levels of serum CK than patients in the other groups of (279.8 ± 125.5 U/L in severely affected patients with onset >30 years vs 894.4 ± 641.3 U/L in classic infantile patients, 720.0 ± 456.8 U/L in patients with symptom onset <15 years of age, and 948.8 ± 530.1 U/L in mildly affected patients with symptom onset >30 years). There were no significant correlations between the percentage of damaged muscle fibers and FVC in sitting position and FSS.
Discussion
ERT has ameliorated the perspectives of patients with Pompe disease. Knowledge of prognostic factors as well as factors predicting the response to ERT has become increasingly important. The aims of our study were to investigate to what extent skeletal-muscle fiber-type distribution and fiber-type-specific damage contribute to the clinical course of Pompe disease.
Skeletal-muscle fiber-type distribution
Compared with patients with nonclassic forms of Pompe disease, classic infantile patients had a lower percentage of type 1 and a higher percentage of type 2a muscle fibers. As little is known about muscle-fiber-type distribution in healthy infants, it is hard to say whether this finding is physiological or related to Pompe disease pathophysiology. Healthy 6- to 50-year-old humans have an equal distribution of types 1 and 2 fibers in the vastus lateralis, although the range is very wide (from 20–75 % type 1 fibers) (Bell et al. 1980; Lexell et al. 1988). Skeletal-muscle fiber-type distribution in nonclassic patients appeared to be no different among the selected subgroups.
Skeletal-muscle fiber-type distribution: effect of aging
In healthy humans, skeletal muscle aging atrophy starts at the age of 25 years and accelerates thereafter (Lexell et al. 1988). Aging atrophy is due to a reduction in both the number and the size of mainly type 2 muscle fibers (Scelsi et al. 1980; Grimby et al. 1984; Lexell 1995). In patients with Pompe disease, we observed the same age-related effect. Interestingly, in classic infantile Pompe disease, a loss of type 2a muscle fibers was observed with increasing age, coinciding with a gain of type 2x muscle fibers. Though this could be a physiological phenomenon (Gojo et al. 2002), it could also be due to immobility of the older, more severely affected infants in our study group. Also, the nonambulant adults had a relatively high percentage of type 2x muscle fibers. As known from other diseases, reduced physical activity can alter fiber-type composition toward a greater proportion of type 2x fibers (Kriketos et al. 1997).
Skeletal-muscle-fiber damage
In classic infantile Pompe patients, muscle pathology closely parallels clinical findings and clinical response to ERT (Thurberg et al. 2006; Winkel et al. 2003). In nonclassic patients, the diagnostic value of muscle biopsies is rather limited, and some biopsies may not even show a sign of glycogen storage (Schoser et al. 2007, 2008; Muller-Felber et al. 2007; Straub 2008). In our study, we did see skeletal-muscle damage in all muscle biopsies. We quantified the muscle damage by using the percentage of damaged muscle fibers and the degree of muscle-fiber vacuolation but found no significant differences between the four subgroups, which confirms earlier findings (Schoser et al. 2007). Nevertheless, muscle biopsies of mildly and severely affected patients in our study had a quite different appearance. Shoser et al. also observed more pronounced secondary alterations in severely affected patients (Schoser et al. 2007). This may stress the importance of a more descriptive qualification, instead of quantification, of muscle damage.
Skeletal-muscle-fiber damage and the clinical picture
CK is a widely used marker in muscle disease, and the degree of CK elevation reflects the underlying disease process. In chronic myopathies, the CK level can drop back to normal due to loss of muscle mass (Turner and Eppenberger 1973; Giesker and Bowers 1979). Similarly, we found in this study that severely affected adult Pompe patients had near-normal CK levels, whereas less affected adults had higher levels. With respect to other clinical parameters, we found a clear correlation between the percentage of damaged muscle fibers and the loss of proximal muscle strength, as well as a concordant loss of pulmonary function in supine position.
Potential relevance of our findings for therapeutic outcome
Based on what is known from the literature, the greater proportion of type 2x muscle fibers in severely affected infants and adults in our study, together with the more severe vacuolation of these fibers, may hamper the effectiveness of ERT, as type 1 fibers were reported to respond better to ERT than were types 2 2b fibers, in particular (Raben et al. 2003, 2005; Drost et al. 2008). This also supports the notion that early treatment leads to better outcome (Kishnani et al. 2009).
In summary, our study demonstrate that muscle-fiber-type distribution in Pompe patients does not differ from that in healthy persons. Furthermore, it seemed that the older, more severely, affected classic infantile patients and the wheelchair-bound and ventilated nonclassic patients had a greater proportion of type 2x muscle fibers. However, this may be caused by physical inactivity in those patients, which is also seen in other diseases.
References
Bell RD, MacDougall JD, Billeter R, Howald H (1980) Muscle fiber types and morphometric analysis of skeletal msucle in six-year-old children. Med Sci Sports Exerc 12:28–31
Drost MR, Schaart G, van Dijk P et al (2008) Both type 1 and type 2a muscle fibers can respond to enzyme therapy in Pompe disease. Muscle Nerve 37:251–255
Fukuda T, Roberts A, Ahearn M, Zaal K, Ralston E, Plotz PH, Raben N (2006) Autophagy and lysosomes in Pompe disease. Autophagy 2:318–320
Giesker D, Bowers GN Jr (1979) The comparative utility of serum creatine kinase versus serum aldolase in the evaluation of muscle disorders. Conn Med 43:699–704
Gojo K, Abe S, Ide Y (2002) Characteristics of myofibres in the masseter muscle of mice during postnatal growth period. Anat Histol Embryol 31:105–112
Griffin JL (1984) Infantile acid maltase deficiency. I. Muscle fiber destruction after lysosomal rupture. Virchows Arch B Cell Pathol Incl Mol Pathol 45:23–36
Grimby G, Aniansson A, Zetterberg C, Saltin B (1984) Is there a change in relative muscle fibre composition with age? Clin Physiol 4:189–194
Hesselink RP, Wagenmakers AJ, Drost MR, Van der Vusse GJ (2003) Lysosomal dysfunction in muscle with special reference to glycogen storage disease type II. Biochim Biophys Acta 1637:164–170
Hirschorn R, Reuser A (2001) Glycogen storage disease type II: acid alpha-glucosidase (Acid Maltase) deficiency. In: Scriver CR, Beaudet AL, Sly WS, Valle MD (eds) The metabolic and molecular bases of inherited disease. Mc Graw-Hill, pp 3389–3420
Kishnani PS, Corzo D, Leslie ND et al (2009) Early treatment with alglucosidase alpha prolongs long-term survival of infants with Pompe disease. Pediatr Res 66:329–335
Kishnani PS, Corzo D, Nicolino M et al (2007) Recombinant human acid [alpha]-glucosidase: major clinical benefits in infantile-onset Pompe disease. Neurology 68:99–109
Kishnani PS, Hwu WL, Mandel H, Nicolino M, Yong F, Corzo D, Infantile-Onset Pompe Disease Natural History Study Group (2006) A retrospective, multinational, multicenter study on the natural history of infantile-onset Pompe disease. J Pediatr 148:671–676
Kriketos AD, Baur LA, O’Connor J, Carey D, King S, Caterson ID, Storlien LH (1997) Muscle fibre type composition in infant and adult populations and relationships with obesity. Int J Obes Relat Metab Disord 21:796–801
Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD (1989) The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol 46:1121–1123
Lexell J (1995) Human aging, muscle mass, and fiber type composition. J Gerontol A Biol Sci Med Sci 50 Spec No: 11–16
Lexell J, Taylor CC, Sjostrom M (1988) What is the cause of the ageing atrophy? Total number, size and proportion of different fiber types studied in whole vastus lateralis muscle from 15- to 83-year-old men. J Neurol Sci 84:275–294
Muller-Felber W, Horvath R, Gempel K et al (2007) Late onset Pompe disease: clinical and neurophysiological spectrum of 38 patients including long-term follow-up in 18 patients. Neuromuscul Disord 17:698–706
Raben N, Danon M, Gilbert AL et al (2003) Enzyme replacement therapy in the mouse model of Pompe disease. Mol Genet Metab 80:159–169
Raben N, Fukuda T, Gilbert AL et al (2005) Replacing acid alpha-glucosidase in Pompe disease: recombinant and transgenic enzymes are equipotent, but neither completely clears glycogen from type II muscle fibers. Mol Ther 11:48–56
Raben N, Ralston E, Chien YH et al (2010) Differences in the predominance of lysosomal and autophagic pathologies between infants and adults with Pompe disease: implications for therapy. Mol Genet Metab 101:324–331
Scelsi R, Marchetti C, Poggi P (1980) Histochemical and ultrastructural aspects of m. vastus lateralis in sedentary old people (age 65–89 years). Acta Neuropathol 51:99–105
Schoser B, Hill V, Raben N (2008) Therapeutic approaches in glycogen storage disease type II/Pompe Disease. Neurotherapeutics 5:569–578
Schoser BG, Muller-Hocker J, Horvath R, Gempel K, Pongratz D, Lochmuller H, Muller-Felber W (2007) Adult-onset glycogen storage disease type 2: clinico-pathological phenotype revisited. Neuropathol Appl Neurobiol 33:544–559
Shea L, Raben N (2009) Autophagy in skeletal muscle: implications for Pompe disease. Int J Clin Pharmacol Ther 47(Suppl 1):S42–S47
Straub V (2008) Diagnosis. In: Baethmann M, Straub V, Reuser AJJ (eds) Pompe disease. Bremen, UNI-MED, pp 51–54
Strothotte S, Strigl-Pill N, Grunert B et al (2010) Enzyme replacement therapy with alglucosidase alfa in 44 patients with late-onset glycogen storage disease type 2: 12-month results of an observational clinical trial. J Neurol 257:91–97
Thurberg BL, Lynch Maloney C, Vaccaro C et al (2006) Characterization of pre- and post-treatment pathology after enzyme replacement therapy for Pompe disease. Lab Invest 86:1208–1220
Turner DC, Eppenberger HM (1973) Developmental changes in creatine kinase and aldolase isoenzymes and their possible function in association with contractile elements. Enzyme 15:224–238
van Capelle CI, Winkel LP, Hagemans ML et al (2008) Eight years experience with enzyme replacement therapy in two children and one adult with Pompe disease. Neuromuscul Disord 18:447–452
van den Berg LE, de Vries JM, Verdijk RM, van der Ploeg AT, Reuser AJ, van Doorn PA (2011) A case of adult Pompe disease presenting with severe fatigue and selective involvement of type 1 muscle fibers. Neuromuscul Disord 21:232–234
van den Hout HM, Hop W, van Diggelen OP et al (2003) The natural course of infantile Pompe’s disease: 20 original cases compared with 133 cases from the literature. Pediatrics 112:332–340
Van den Hout JM, Kamphoven JH, Winkel LP et al (2004) Long-term intravenous treatment of Pompe disease with recombinant human alpha-glucosidase from milk. Pediatrics 113:e448–e457
van der Ploeg AT, Clemens PR, Corzo D et al (2010) A randomized study of alglucosidase alfa in late-onset Pompe’s disease. N Engl J Med 362:1396–1406
Winkel LP, Hagemans ML, van Doorn PA, Loonen MC, Hop WJ, Reuser AJ, van der Ploeg AT (2005) The natural course of non-classic Pompe’s disease; a review of 225 published cases. J Neurol 252:875–884
Winkel LP, Kamphoven JH, van den Hout HJ, Severijnen LA, van Doorn PA, Reuser AJ, van der Ploeg AT (2003) Morphological changes in muscle tissue of patients with infantile Pompe’s disease receiving enzyme replacement therapy. Muscle Nerve 27:743–751
Wokke JH, Escolar DM, Pestronk A et al (2008) Clinical features of late-onset Pompe disease: a prospective cohort study. Muscle Nerve 38:1236–1245
Acknowledgements
We thank patients and parents for participating in the study; and J. Hardon, H. Nelisse, and T. Oskam for their contribution to the study as research nurses.
The research on Pompe disease at Erasmus MC was financially supported by the Erasmus MC Revolving Fund (NAMEvdB, project no 1054), ZonMw-Dutch organization for healthcare research and innovation of care [Grant 152001005], The ‘Prinses Beatrix Fonds’ (project number OP07-08) and the European Union, 7th Framework Program “EUCLYD-a European Consortium for Lysosomal Storage Diseases” of the European Union (health F2/2008 grant agreement 201678).
Competing interest
As of August 2004, ATvdP and AJR provide consulting services for Genzyme Corp, Cambridge, MA, USA, under an agreement between Genzyme Corp and Erasmus MC, Rotterdam, the Netherlands. This agreement also caters to financial support for Erasmus MC for research in Pompe disease. Erasmus MC and inventors for the method of treatment of Pompe’s disease by ERT receive royalty payments pursuant to Erasmus MC policy on inventions, patents and technology transfer.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by: Ed Wraith
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Figure 1
The percentage of a types 1 and 2 muscle fibers, and b percentage of type 2a and type 2x muscle fibers in classic infantile patients and nonclassic patients. Significance between the different groups of patients is shown by * (P < 0.05). (JPEG 22 kb)
Supplementary Table 1
Patient characteristics (DOC 61 kb)
Supplementary Table 2
Degree of vacuolation per muscle-fiber type (percentage of fibers) (DOC 26 kb)
Rights and permissions
About this article
Cite this article
van den Berg, L.E.M., Drost, M.R., Schaart, G. et al. Muscle fiber-type distribution, fiber-type-specific damage, and the Pompe disease phenotype. J Inherit Metab Dis 36, 787–794 (2013). https://doi.org/10.1007/s10545-012-9541-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10545-012-9541-7