Abstract
Introduction
Niemann-Pick disease (NPD) due to acid sphingomyelinase deficiency is a lipid storage disease resulting from the accumulation of sphingomyelin, predominantly within cells of the monocyte-macrophage system. In contrast to other lysosomal storage disorders, skeletal involvement in NPD has not been systematically studied.
Methods
Pediatric and adult NPD-B patients underwent medical histories and physical examinations, DEXA scans to measure bone mineral content (BMC), and bone mineral density (BMD) and computed tomography scan or MRI of the abdomen for spleen volume. Z and/or T scores were calculated for the DEXA results. For the pediatric patients adjusted mean BMC (g) and BMD (g/cm2) of the lumbar spine, hip, and femoral neck was compared to control subjects. For determination of the relationship between spleen volume and lumbar spine BMD Z score, linear correlation analyses were performed.
Results
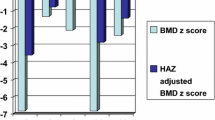
Lumbar spine Z scores for pediatric patients ranged from 0.061 to -4.879. Statistically significant decreases were observed for the adjusted mean BMC and BMD at the lumbar spine, hip, and femoral neck between the pediatric NPD-B cohort and control subjects. Most NPD-B adults were osteopenic or osteoporotic at one or more sites according the WHO classification of BMD. In NPD-B patients, the degree of splenomegaly was inversely correlated with lumbar spine BMD Z scores.
Conclusion
Skeletal involvement is a common and previously unrecognized manifestation of NPD-B. The association between splenomegaly and BMD lends further support to spleen size as an indicator of disease severity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Niemann-Pick disease (NPD) due to acid sphingomyelinase deficiency (ASM) (sphingomyelin phosphodiesterase 1; EC 3.1.4.12) (OMIM #s 607616 and 257200) is a multisystem lysosomal storage disease resulting from the accumulation of sphingomyelin predominantly within cells of the monocyte-macrophage system (Schuchman and Desnick 2001). Patients with ASM deficiency have been classified into two phenotypic subtypes, a severe neurodegenerative form leading to death by three years of age (Niemann-Pick disease type A, or NPD-A) (McGovern et al 2006), and a widely variable phenotype characterized by hepatosplenomegaly, hyperlipidemia and pulmonary involvement (Niemann-Pick disease type B, or NPD-B) (McGovern et al 2008). The diagnosis of NPD-B is usually made in childhood after organomegaly is noted. Affected patients who do not have neurologic involvement usually survive into late childhood or adulthood.
In contrast to other lipid storage disorders in which bone involvement is known to be a common and potentially debilitating clinical feature, systematic evaluation of the skeleton in affected patients with NPD have not previously been undertaken. To date, the only published documentation of skeletal disease in NPD-B is a single case report of a postmenopausal woman with vertebral fractures (Volders et al 2002). Of interest, a survey study of 59 pediatric and adult NPD-B patients revealed that 39 % complained of joint or limb pain suggesting that skeletal involvement may be a more common feature of NPD-B (McGovern et al 2008). Indeed, skeletal disease is known to be a common and potentially debilitating clinical feature of Gaucher disease, which manifests as bone pain and/or bone crises, osteopenia, pathologic fractures, and avascular necrosis (AVN) of the femoral head (Bembi et al 2002; Wenstrup et al 2002). Similarly, osteopenia and osteoporosis have been reported as manifestations in Fabry disease (Germain et al 2005; Sacre et al 2010; Mersebach et al 2007).
In this study, we obtained bone scan images in 46 affected patients with NPD-B to measure bone mineral content (BMC), and bone mineral density (BMD) and compared them to a cohort of unaffected healthy children and adult norms. We also explored the relationship between lumbar spine BMD Z score and spleen size, which has previously been shown to correlate with the severity of other disease manifestations in NPD-B (McGovern et al 2008).
Methods
Study subjects
Pediatric (n = 20; <21 yrs) and adult (n = 26) NPD-B patients participated in the study, which was carried out at the General Clinical Research Center. The study was approved by the Mount Sinai School of Medicine Institutional Review Board. Voluntary, written informed consent was obtained from each patient or guardian, and children over the age of six gave assent prior to any study procedure. The diagnosis of NPD-B was confirmed in each patient by the demonstration of reduced ASM activity in isolated leukocytes and/or cultured skin fibroblasts.
Clinical assessments
Medical histories and physical examinations were obtained for all patients, including pubertal maturation by Tanner staging. Height without shoes was measured with the Seca height-Rite Stadiometer (Model 225, Culver City, Calif), and weight was measured with a digital scale (Scan-Tronix Stand on Scale, Model 5002, Carol Stream, Ill). None of the patients had been previously diagnosed with osteoporosis or osteopenia, or were taking any medications that influence bone turnover. None of the females were pregnant or lactating, and all but one adult female included in the study were premenopausal.
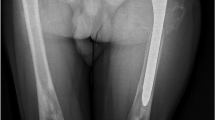
Imaging studies
Bone scan images in all patients were obtained with the same DEXA instrument (Hologic QDR-4500A, Waltham, Mass). Bone mineral content (BMC, g), and bone mineral density (BMD, g/cm2) were measured at the hip, femoral neck, and lumbar spine using a standard protocol. Bone age was determined during the same visit in 12 of the pediatric study participants. Radiographs of the left hand, wrist, and forearm were interpreted by a single pediatric radiologist to assess skeletal maturity according to the standards of Greulich and Pyle (1959). Bone age delay was expressed as bone age minus chronological age (BA–CA). Imaging studies also included computed tomography scan or MRI of the abdomen for spleen volume. Spleen volume was calculated by integrating cross-sectional images and expressed as multiples of normal (MN), assuming a normal spleen volume is 0.2 % of body weight (with 1 kg equivalent to 1 L) (McGovern et al 2008).
Statistical methods
For pediatric patients, Z score (SD compared to age and gender matched controls) was calculated at the lumbar spine using the Hologic database; normative data is not available in the Hologic system for pediatric hip or forearm. For adults, T (SD compared to gender and race matched young normals) and Z scores were calculated at the lumbar spine, hip and forearm using the Hologic database. For the pediatric subjects, BMC and BMD data as a whole cohort also were compared with DEXA data from a cohort of 293 healthy children without NPD (age 3-21 years) collected by the Center for Pediatric Nutrition Research at the University of Utah (Stevenson et al 2007). Hip, femoral neck and lumbar spine BMC and BMD were compared between the pediatric NPD cohort and control subjects. Adjusted means for the difference between patients and controls (adjusted for gender, age, and age2) and adjusted means for the difference between males and females (adjusted for case/control status, age and age2) were obtained. Statistical significance of differences observed in BMC (g) and BMD (g/cm2) of the lumbar spine, hip, and femoral neck between the pediatric NPD-B cohort and control subjects was calculated with analysis of covariance adjusting for age, weight, height, Tanner stage, and gender. A separate analysis comparing BMC (g) and BMD (g/cm2) between the pediatric NPD-B cohort and control subjects was calculated using bone age in the place of chronologic age for the 12 pediatric NPD-B subjects who also had bone age assessed at the time of the DEXA scan. For determination of whether spleen volume correlates with lumbar spine BMD Z score, linear correlation analyses were performed by using Pearson’s correlation coefficient (r). P < 0.05 was considered to be statistically significant, and r >0.4 was considered to be a high correlation.
Results
Patient characteristics
The NPD pediatric cohort included 11 boys and 9 girls from 16 different families (age range 1.6 y to 18.2 years; mean age 10.3 ± 4.1 years; mean height, 131.4 ± 23.1 cm; mean weight, 35.2 ± 19.1 kg; median Tanner stage 2, range 1 to 5). Within the NPD pediatric cohort, 5 of 20 subjects (25 %) had suffered a skeletal fracture. Notable among these was an 18 month old girl who had suffered three tibial fractures beginning at the age of 14 months when she first began to walk. Fracture sites in other pediatric patients included wrist, ankle and skull after trauma, and clavicle after trivial trauma. Twelve of the 20 (60 %) affected children also had complaints of back and leg pain. Bone age studies in 12 pediatric patients revealed an average bone age delay of 1.6 years (range: 0 to –3.2 years). The NPD adult cohort included 9 males and 17 females from 24 different families (age range 22.1 years to 54.5 years; mean age 33.7 ± 8.92 years). Among the adults, 14 (53 %) had suffered at least one fracture and 15 (58 %) had complaints of back pain. Notable among the fracture histories was a 42 year old woman who had vertebral collapse of six thoracic vertebrae requiring multiple spinal surgeries, and a 63 year old man who had a wrist fracture at age 23, rib fractures at age 43, and an ankle fracture at age 51 with no history of trauma.
Bone density studies
Among the 20 pediatric patients, 29 DEXA observations were made, with nine of the subjects having had two DEXA scans at different ages. Anthropometric data for the pediatric control subjects (healthy individuals without NPD) included: 132 boys and 161 girls; mean age, 11.8 ± 4.3 years; mean height 145.8 ± 22.5 cm; mean weight, 43.1 ± 19.7 kg; median Tanner stage 2, range 1 to 5. The lumbar spine BMD Z scores for the pediatric patients ranged from 0.061 to -4.879 (mean = -2.3135). Ten (50 %) had Z scores that were <-2.5 SD. Statistically significant differences (p < 0.001) were observed for the adjusted mean BMC and BMD of the lumbar spine, hip, and femoral neck between the pediatric NPD-B cohort and control subjects by analysis of covariance adjusting for age, weight, height, Tanner stage, and sex (Table 1). Statistically significant differences in BMD and BMC also were observed when the chronologic age was replaced with bone age for the 12 pediatric patients who had this assessment performed at the same time as the DEXA (p < 0.001).
Among the adult subjects, most were osteopenic or osteoporotic at one or more sites according the WHO classification of BMD (normal, T Score > -1 SD; osteopenia, -2.5 < T score < -1 SD; osteoporosis, T score ≤ -2.5 SD; and severe osteoporosis, T score ≤ -2.5 with spontaneous fracture (Table 2). Only two adults had a normal T score for lumbar spine BMD, and two had T scores ≤ -2.5 with evidence of vertebral fractures, which placed them in the severe osteoporosis category. The two adults with a normal lumbar spine BMD T score also had normal scores at the hip and forearm and overall had a mild disease phenotype.
Relationship between bone density and spleen size
All subjects had intact spleens that ranged from 4.5 to 27.3 MN in volume. The lumbar spine BMD Z score for all subjects showed a strong inverse correlation with spleen size (r = 0.7311, p = 0.001), such that patients with larger spleens had lower BMD (Fig 1).
Discussion
The results reported here demonstrate that skeletal involvement occurs commonly in patients with NPD-B, as has been noted for other lipid storage disorders. Both pediatric and adult patients with NPD-B had decreased BMD compared to controls, and the majority of adults had lumbar spine, hip and femur T scores in the osteopenic or osteoporotic range. Therefore patients with NPD-B may be at increased risk for the development of clinical complications related to osteoporosis. In this series, 43 % of all patients had a history of one or more skeletal fractures, some of which by history were pathologic. These findings suggest that examination of the skeleton including DEXA scan, with the frequency of this study guided by the findings and the clinical status of the patient, should be part of the clinical evaluation of patients with NPD.
The finding that BMD is decreased from the earliest age studied suggests the need for early intervention since accrual of bone mass during childhood is an important factor in determining final adult bone mass. Such interventions can include load-bearing activities and muscle strengthening (NIH Consensus Statement 2001; de Kam et al 2009). However, many pediatric patients with NPD-B suffer from chronic fatigue and pulmonary disease which may make such activities difficult. In addition, due to the presence of splenomegaly NPD-B patients are usually encouraged to participate in aerobic activities that have a low risk of abdominal trauma (e.g., swimming). Therefore, a program designed to increase load bearing would have to be carefully developed.
Patients with Gaucher disease often have low BMD, which has been reported to respond to both enzyme replacement therapy and substrate reduction therapy (Deegan et al 2011, Goker-Alpan 2011). Other treatments for osteoporosis include pharmacologic therapy with antiresorptive agents such as the bisphosphonates. In Gaucher disease, one study found that alendronate adjunctive therapy in combination with enzyme replacement therapy (ERT) incrementally improved osteopenia in affected adults (Wenstrup et al 2004). To date, no clinical trials to assess the use of bisphosphonates have been carried out in children with Gaucher disease. However, this approach in NPD-B may be precluded by the finding that biphosphonates are inhibitors of ASM activity (Arenz 2010, Roth et al 2009) and have a prolonged half-life in bone (Lin 1996) which could potentially worsen the disease. Newer treatments for osteoporosis, such as monoclonal antibodies (e.g., Denosumab) that inhibit the receptor activation of nuclear factor kappa-B ligand (RANKL) thus reducing osteoclast function may be worth consideration (Russell et al 2011).
Previously, spleen volume has been shown to correlate with several aspects of disease severity in patients with NPD-B, including liver volume, triglyceride and high-density lipoprotein levels, height Z score, hemoglobin concentration, white blood cell count, and percent predicted forced vital capacity (McGovern et al 2008). The relationship between spleen size and decreased bone density in both pediatric and adult patients reported here provides further evidence that spleen volume may be a useful surrogate marker of disease burden. This finding is similar to the correlation of skeletal involvement and spleen size reported for Gaucher disease, where the degree of splenomegaly has been shown to correlate with higher bone marrow burden scores (DeMayo et al 2008).
The pathophysiologic basis for skeletal findings in the lipid storage disorders is not completely understood. In Gaucher disease, substantial infiltration of the bone marrow with Gaucher cells, osteonecrosis and osteosclerosis all contribute to the skeletal findings. In addition, it has been hypothesized that activated macrophages in affected Gaucher patients produce cytokines, including IL-1, IL-6 and tumor necrosis factor (TNF), that interfere with normal osteoclast and osteoblast function (van Breemen et al 2007; Makoto et al 2008). More recent studies conducted in Gaucher patients ( Mistry et al, 2011) and in a Gaucher mouse model (Mistry et al 2010) suggest that low BMD in Gaucher disease is due to inhibition of bone formation rather than stimulation of bone resorption. In future studies, it will be of interest to determine the role of macrophage activation and substrate accumulation in NPD-B patients, to characterize bone biomarkers in plasma, and to see how they compare to findings in Gaucher disease.
The finding that patients with NPD-B have clinically significant skeletal involvement has implications both for the clinical evaluation of patients as well as the future development of therapy for this disorder. Although there is currently no definitive treatment for NPD-B, a recent phase 1 trial of enzyme replacement therapy (ERT) has been undertaken. The experience with ERT for Gaucher disease has documented that although ERT improves bone density over time, certain skeletal complications are difficult to treat and may continue to progress or display lack of improvement (Mistry et al 2011; Deegan et al 2011). Therefore, future monitoring of NPD-B patients enrolled in clinical trials should include the evaluation of the impact of new therapies on bone involvement.
References
Arenz C (2010) Small molecule inhibitors of acid sphingomyelinase. Cell Physiol Biochem 26(1):1–8
Bembi B, Ciana G, Mengel E, Terk MR, Martini C, Wenstrup RJ (2002) Bone complications in children with Gaucher disease. Br J Radiol 75:A37–A44
de Kam D, Smulders E, Weerdesteyn V, Smits-Engelsman BCM (2009) Exercise interventions to reduce fall-related fractures and their risk factors in individuals with low bone density: a systematic review of randomized controlled trials. Osteoporos Int 20(12):2111-25 print
Deegan PB, Pavlova E, Tindall J et al (2011) Osseous manifestations of adult Gaucher disease in the era of enzyme replacement therapy. Med Jan 90(1):52–60
DeMayo RF, Haims AH, McRae MC, Yang R, Mistry PK (2008) Correlation of MRI-based bone marrow burden score with genotype and spleen status in Gaucher’s disease. Am J Rheum 191:115-123
Germain DP, Benistan K, Boutouyrie P (2005) Mutschler C (2005) Osteopenia and osteoporosis: previously unrecognized manifestations of Fabry disease. Clin Genet 68(1):93–5
Goker-Alpan O (2011) Therapeutic approaches to bone pathology in Gaucher disease: past, present and future. Molec Genet Metab 104(4):438–447
Greulich WW, Pyle SI (1959) Radiographic atlas of skeletal development of the hand and wrist, 2nd edn. Stanford University Press, Stanford
Lin JH (1996) Biphosphonates: a review of their pharmacologic properties. Bone 18(2):72–85
Makoto Y, Watanabe Y, Tokunaga Y et al (2008) Roles of specific cytokines in bone remodeling and hematopoiesis in Gaucher disease. Ped Int 49:959–965
McGovern MM, Aron A, Brodie S, Desnick RJ, Wasserstein MP (2006) The natural history of Niemann Pick disease type A. Neurology 66(2):228–232
McGovern MM, Wasserstein MP, Bembi B et al (2008) A cross sectional study of disease manifestations in Niemann Pick disease yype B. Pediatrics 122(2):e341–349
Mersebach H, Johansson JO, Rasmussen AK et al (2007) Osteopenia: a common aspect of Fabry disease. Predictors of bone mineral density. Genet Med 12:812–8
Mistry PK, Liu J, Yang M et al (2010) Glucocerebrosidase gene-deficient mouse recapitulates Gaucher disease displaying cellular and molecular dysregulation beyond the macrophage
Mistry PK, Weinreb NJ, Kaplan P et al (2011) Osteopenia in Gaucher disease develops early in life: response to imiglucerase enzyme therapy in children, adolescents and adults. Blood Cells Mol Dis 46(1):66–72
NIH Consensus Development Panel (2001) Osteoporosis prevention, diagnosis, and therapy. JAMA 285:785–795
Roth AG, Drescher D, Yang Y et al (2009) Potent and selective inhibition of acid sphingomyelinase by bisphosphonates. Angewandte Chemie 48:7560–7568
Russell S, Crawford B, Morgane C, Diven D, Yarbor L (2011) Denosumab: a review of its pharmacology and clinical implications. Contemp Oncol 3(1)
Sacre K, Lidove O, Giroux B et al (2010) Bone and joint involvement in Fabry disease. Scand J Rheum 39:171–174
Schuchman EH, Desnick RJ (2001) Niemann Pick disease types A and B: acid sphingomyelinase deficiencies. In: Scriver CR, Beaudet AL, Sly WS, Valle D (eds) The metabolic & molecular bases of inherited disease, 8th edn. McGraw Hill, New York, pp 3589–3610
Stevenson DA, Moyer-Mileur LJ, Murray M et al (2007) Bone mineral density in children and adolescents with neurofibromatosis type 1. J Ped 150(1):83–88
van Breemen MJ, de Fost M, Voerman JS et al (2007) Increased plasma macrophage inflammatory protein (MIP)-1alpha and MIP-1beta levels in type 1 Gaucher disease. Biochim Biophys Acta 1772(7):788–796
Volders P, Van Hove J, Lories RJU et al (2002) Niemann-Pick disease type B: an unusual clinical presentation with multiple vertebral fractures. Am J Med Genet 109(1):42–51
Wenstrup RJ, Roca-Espiau M, Weinreb NJ, Bembi B (2002) Skeletal aspects of Gaucher disease: a review. Br J Rad 75:A2–A12
Wenstrup RJ, Bailey L, Grabowski GA et al (2004) Gaucher disease: alendronate disodium improves bone mineral density in adults receiving enzyme therapy. Blood 104:1253–1257
Acknowledgments
The authors wish to thank the Center for Pediatric Nutrition Research at the University of Utah for sharing their normative pediatric DEXA data. Dr. McGovern is the recipient of Mid Career Patient-Oriented Research Career Development Award K24 RR021991 from the National Institutes of Health. These studies were supported by grant 5 MO1 RR00071 for the Mount Sinai General Clinical Research Center from the National Center for Research Resources, National Institutes of Health as well as a research grant from Genzyme, a Sanofi Company, Cambridge, MA.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by: Olaf Bodamer
Rights and permissions
About this article
Cite this article
Wasserstein, M., Godbold, J. & McGovern, M.M. Skeletal manifestations in pediatric and adult patients with Niemann Pick disease type B. J Inherit Metab Dis 36, 123–127 (2013). https://doi.org/10.1007/s10545-012-9503-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10545-012-9503-0