Abstract
There is no evidence that high phenylalanine (Phe) levels have irreversible effects on the adult brain. Many adults with phenylketonuria (PKU) no longer follow a protein-restricted diet. Neuropsychological studies have shown that reaction time in adults with PKU is slower than controls. There are no data to show that this is directly related to Phe levels. Another way to assess reaction time is to measure saccadic latency. We have used a portable, head-mounted saccadometer to measure latency in the outpatient setting. Patients with PKU were split into three groups: off-diet (Phe>1,200 μmol/l), on-diet (Phe <800 μmol/l) and maternal diet (Phe 100–400 μmol/l ). Reciprocal median latency (RML) was compared between groups. Latency was significantly slower in patients who were off-diet than in patients on-diet, on a maternal diet or in normal controls. Reaction times in both diet-treated groups were not significantly different from normal controls. In 16 women planning pregnancy we obtained values before and after they commenced the maternal diet. Stricter control of Phe levels resulted in a significant improvement in reaction times. We conclude that saccadometry is useful in monitoring PKU patients. Adult patients with PKU not on a protein-restricted diet have significantly slower reaction times than controls. In addition, off-diet patients have significantly slower reaction times than on-diet. Paired data show that effects of Phe levels on reaction time are reversible.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Phenylketonuria (PKU, OMIM #261600) is one of the most common inherited metabolic disorders with an incidence of about 1 in 10,000 (Scriver et al. 2008). The majority of cases result from deficiency of phenylalanine hydroxylase (PAH) which converts phenylalanine into tyrosine. In PKU, phenylalanine (Phe) accumulates, with high levels in the blood and brain and a relative deficiency of tyrosine.
The infant brain is sensitive to high Phe levels and, if left untreated, PKU gives rise to severe mental retardation. Microcephaly is common and about 25% of patients have epilepsy. Many older patients have behavioural problems and some suffer from psychiatric illnesses. A few patients develop movement disorders with pyramidal and extrapyramidal signs (Brenton and Pietz 2000). The precise mechanism of neurotoxicity is not fully understood (de Groot et al. 2010), but neurological, neurocognitive and neuropsychological outcomes in children are correlated with blood Phe levels (Scriver et al. 2008).
The aim of dietary management in PKU is to reduce the flux through the affected metabolic pathway and thus reduce the accumulation of Phe. Strict control of Phe levels in infancy and early childhood allows normal intellectual development (Burgard 2000). Newborn screening for PKU was introduced in the UK in 1969. Diagnosis is now made in the first week of life and it is possible to institute dietary therapy before the infant sustains any irreversible brain damage. This has completely transformed the prognosis of this disorder, and patients with PKU now lead normal lives with intellectual and physical achievements similar to their peers.
Their diet is, however, quite demanding and, although compliance is normally good in infants and young children, it is not uncommon for older children and young adults to want to be able to eat the same things as their friends and family (Walter et al. 2002). Although there was initially much concern about possible cognitive decline in adolescent patients who stopped their low-protein diets, experience has on the whole been good, and it now seems that, after the age of 10, IQ is fixed, and the brain is no longer susceptible to the sort of irreversible injury seen in infants exposed to high Phe levels (Brenton and Pietz 2000; Burgard 2000).
The only group of adult patients for whom it is essential to obtain strict dietary control of Phe levels is women who are pregnant or considering pregnancy. Exposure of the foetus to high maternal Phe levels results in the maternal PKU syndrome, which consists of a combination of cardiac and skeletal defects, microcephaly, developmental delay and low birth weight (Levy and Ghavami 1996). The syndrome can be entirely prevented if mothers maintain low Phe levels throughout their pregnancies (Maillot et al. 2008).
In our centre we care for about 400 adults with PKU. Of these, only around 150 are following a protein-restricted diet at any time, about 30 of whom are on a pre-conception or maternal diet. Most of the adults who no longer follow a protein-restricted diet do not themselves notice any ill effects associated with having high blood Phe levels. Some, however, do find that their concentration, mood and temper are better when their levels are lower and choose to return to a low protein diet, as has been reported by others (Gassió et al. 2003)
Neuropsychological studies in adults with PKU have shown that performance on certain tests of executive function can be related to Phe levels, but these effects are not consistent, and their significance to everyday life is unclear (Christ et al. 2010). Nonetheless, there is concern that an accumulation of subtle neuropsychological deficits may lead to significant psychosocial morbidity in adults with PKU which is not always recognised and which might be improved by stricter control of Phe levels (Gentile et al. 2010).
A more quantitative assessment of the effects of high Phe levels on the adult brain may be possible by measuring reaction time. A meta-analysis of neuropsychological studies comparing reaction times in patients with and without PKU has shown that there is a relationship between high Phe levels and slower reaction times for children and adolescents with PKU (Albrecht et al. 2009). In adults, however, although reaction times for all people with PKU were slightly slower than for people who don’t have PKU, this was independent of whether they were on dietary treatment or not, and there was no direct relationship between Phe levels and reaction time. It is important to note, however, that all groups of adult PKU patients studied had relatively high Phe levels (above 700 μmol/l), and it was therefore not possible to investigate whether reaction times would return to ‘normal’ at levels closer to the normal reference range (33–81 μmol/l).
If we are going to advise our adult patients to continue on or return to a protein-restricted diet, we need to be able to demonstrate that they will gain real benefit from doing so. The literature demonstrates that it is often difficult for professionals to interpret the results of neurocognitive tests, and it may therefore be hard for patients to make decisions which will have a profound effect on their everyday life based on the results of neuropsychological assessments. A simple test of reaction time, which can be expressed numerically, might be easier for patients and their carers to interpret.
In the current study we have used saccadic latency as a measure of reaction time in adult PKU patients. Saccades are rapid, conjugate eye movements elicited in response to a stimulus. Saccadic latency or reaction time is determined by mostly cortical decision-making processes, and prolonged saccadic latency can be a sign of subtle cortical dysfunction, even in the absence of symptoms (Ali et al. 2006; Pearson et al. 2007). We used a portable, head-mounted saccadometer which allowed us to gather data simply and quickly in the outpatient clinic.
We compare saccadic reaction times in adult PKU patients off-diet, on-diet and on a highly restrictive pre-conception/maternal (PC/M) diet. Saccade data for each group of patients were also compared with data from adults without PKU.
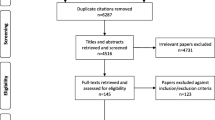
Materials and methods
Subjects
Subjects were adult PKU patients over the age of 18 years attending the Metabolic Clinic at the National Hospital for Neurology and Neurosurgery, London, UK. All participants had been diagnosed by newborn screening and started dietary treatment early in life. They had remained on a low protein diet and amino acid supplements at least until adolescence. Patients with late diagnosed PKU or other serious neurological or psychiatric disorder were excluded.
Patients were split into three groups (Table 1). The off-diet group were those who, at the time of saccadometry, had an unrestricted dietary protein intake and were not taking any amino acid supplements. In practice, people who follow a protein-restricted diet during childhood often never acquire a taste for meat, and PKU adults who are ‘off-diet’ commonly have a lower meat, fish and dairy intake than average. Only data from patients whose Phe level was greater than 1,200 μmol/L, suggesting adequate natural dietary protein, were included in the analysis. The on-diet group were subjects following a protein-restricted diet and taking amino acid supplements. The current recommended treatment target in the UK is to obtain blood Phe levels less than 700 μmol/L. In fact, few patients are able to consistently achieve this, and all patients achieving a Phe level <800 μmol/L at the time of saccadometry measurement were included. The pre-conception/maternal group (PC/M) were female patients who were either trying to conceive or actually pregnant at the time of saccadometry measurement. To prevent maternal PKU syndrome, we advise women to maintain Phe levels between 100 and 300 μmol/L before conception and throughout pregnancy.
A sub-group of 16 of these patients on a PC/M diet also had saccadometry performed when they were on a less restricted diet, with higher Phe levels [mean off-diet Phe 1,223 (±330) μmol/L; mean PC/M diet Phe 277 (±108) μmol/L). For this group, a further paired analysis was performed comparing the two data sets.
Saccade data was also collected from healthy age-matched volunteers without PKU. Control groups were constructed which were age- and sex-matched to the experimental groups (n = 56 for off-diet group, n = 21 for on-diet, n = 33 for PC/M group).
Following an explanation of the procedure, consent was obtained from each subject and saccadometry performed during a routine outpatient appointment. This study was approved by the local research ethics committee.
Procedure
A head-mounted saccadometer (Ober Consulting, Poland) was used. This projects red 0.1° 13 cd m-2 target dots onto a blank wall approximately 1.5 m in front of the seated subject at three different horizontal positions (10° left, 0° or 10° right of centre); because the stimuli move exactly with the head, it is not necessary to stabilise the head with a bite-bar. Subjects were seated comfortably and were asked to follow the target dot with their eyes keeping their head as still as possible. Eye movements were recorded by binocular infra-red scleral reflectance (Ober et al. 2003) with a band-width of 1 kHz.
The saccadometer is fitted to the head with elastic straps, is comfortable to wear and requires no specific skill or training for use either by the examiner or the subject. Saccadometry was performed in the outpatient clinic. Each subject performed a single run of 80–100 saccades on each occasion, taking less than 5 min.
Data analysis
Data for each patient were downloaded onto a computer running LatencyMeter version 4.4 (Ober Consulting, Poland) which automatically rejects invalid data caused by, for example, blinks, saccades in the wrong direction, or saccades falling outside the amplitude range 5–15° or latency range 50–600 ms. Reciprobit plots were generated using SPIC software (Advanced Clinical Instrumentation, Cambridge), which combines data from subjects’ leftwards and rightwards saccadic latencies and automatically generates best-fit values of the underlying LATER parameters by minimisation of the Kolmogorov-Smirnov one-sample statistic (Carpenter and Williams 1995).
Reciprocal median latency follows a Gaussian distribution, and unpaired two-tailed t tests were therefore used to compare the mean reciprocal median latency between each subject group. A paired two-tailed t test was used to compare data from patients in the PC/M group for whom there were on-diet and off-diet saccade recordings.
Results
It has been previously reported that age increases saccadic latency by about 1 ms/year but the sex of the patient does not influence saccades (Klein et al. 2005). There was no significant difference in age between groups (Table 1). Approximately half of the off-diet group were female, whereas the on-diet groups were predominantly female (Table 1).
Our results show that there is a significant (p = 0.02) difference in reciprocal median latency between patients with PKU who are off-diet and controls (Table 2). Median latency for the PKU subjects was 12 ms longer than the controls. In contrast, both for PKU subjects on standard and PC/M diets, median latency was not significantly different from control groups. PKU subjects who were on a normal unrestricted diet had longer median latencies than those on a low protein diet (+13 ms, p = 0.04) or those on PC/M diet (+14 ms, p = 0.01).
For 16 women with PKU we recorded latency data before and after they commenced PC/M diet. Paired t test showed that median latency improved from 171 ms before PC/M diet to 160 ms on diet (p = 0.04) (Table 2 and Fig. 1).
Overall, there was a negative correlation between reciprocal median latency and Phe level (r 2 = 0.05, p = 0.02) (Fig. 2). This relationship persisted following adjustment for age.
Discussion
These data show that adults with PKU who are following an unrestricted diet have significantly slower reaction times than a control population who don’t have PKU. This finding supports previous neuropsychological studies (Albrecht et al. 2009). However, our data also show that in individuals with PKU on a protein-restricted diet, reaction times are related to the blood Phe level. In the diet-treated population with a Phe level of 800 μmol/l or less, reaction times did not differ significantly from people who don’t have PKU.
These differences in reaction time do not represent a fixed deficit. In a group of women with PKU returning to a protein-restricted diet in order to become pregnant, reaction times improve as their blood Phe levels come down, returning to the normal range once the diet is established.
The magnitude of the increase in latency seen in subjects with PKU on unrestricted diets as compared to those on low protein diets (13 ms) is similar to that which has previously been measured in control subjects breathing sub-anaesthetic doses of sevofluorane but less than those seen in boxers suffering from head trauma and concussion after a bout (Pearson et al. 2007).
Decision processes determining reaction time and saccade latency are controlled by a widely distributed network of high level cortical neurones (Carpenter 2000, 2005). Adult patients with PKU can have white matter changes on MRI (Pietz et al. 1996) which may represent oedema of myelin tracts (Vermathen et al. 2007). It is possible that these ‘lesions’ might affect cortical function and be related to the prolonged saccadic latency we have documented in adult PKU patients with high Phe levels. We do not routinely request MRI brain scans for patients with PKU so were unable to test this hypothesis in our patients. Interestingly, it has been shown that these white matter changes resolve if patients return to diet and their blood Phe levels come down (Cleary et al. 1995).
Another mechanism by which high blood Phe levels might affect brain function is by competition with other large neutral amino acids (LNAAs) for transport across the blood brain barrier (van Spronsen et al. 2009). All these amino acids share a single transporter, SCL7A5, and high levels of Phe will prevent amino acids such as tyrosine and tryptophan from entering the brain. The resulting intracerebral deficiency could lead to reduced neurotransmitter levels: tyrosine is the precursor of dopamine and noradrenaline, and tryptophan is the precursor of serotonin. Oral supplementation with LNAAs has been shown to reduce brain Phe levels and increase brain tyrosine and tryptophan levels in PKU patients (Pietz et al. 1999), and it would be interesting to see what effect such supplementation would have on saccadic latency.
Standard dietary treatment of PKU would also be expected to improve brain levels of tyrosine and tryptophan by reducing competition for transport across the blood brain barrier. The low protein diet lowers Phe levels in the blood and the amino acid supplements contain the other LNAAs.
In summary, this study shows that the portable saccadometer is a useful tool in monitoring patients with PKU. Saccadometry can be easily performed in the routine outpatient setting and may provide a useful surrogate measurement of cognitive function in PKU patients, having the advantage that it is relatively objective, less prone to practice effects than conventional cognitive tests, and capable of providing standardised information that can be related to studies in other clinics and laboratories, as well as to the growing literature examining the neural mechanisms underlying the brain’s decision processes. Because we make two or three saccades every second of our waking life, these tests do not fatigue the subject in the way that manual tasks can, so that a great deal of data can be collected in a short period of time—typically some 100 trials in 3–4 min.
Our data suggest that improved reaction time, as measured by saccadic latency, is apparent in patients treated to the current UK recommended target Phe level for adults of <700 μmol/L. Although there was no significant difference in saccadic latency between PKU patients with Phe levels <800 μmol/l and controls in our study, the data from patients on PC/M diets, with Phe levels <300 μmol/l, suggest that further lowering of Phe levels may lead to incremental improvements in reaction time. These paired data imply that any effects which high Phe levels have on reaction time are reversible if patients return to a protein-restricted diet. In practice, for individual patients on a low protein diet, serial saccadometry in the outpatient clinic should allow us to define the Phe level at which they gain maximum benefit in terms of reaction time and attention.
A meta-analysis of previous studies involving neuropsychological testing has not been able to demonstrate that the reductions in reaction time seen in adult patients with PKU have been related to their blood Phe levels (Albrecht et al. 2009). In contrast, this study shows a clear relationship between lowering Phe levels and an improvement in cortical function. As such, our data would appear to provide a strong argument in favour of ‘diet for life’ for patients with PKU. However, it is not clear how improvements in surrogate markers of cognitive function such as these saccadic parameters translate into quality of life for the patient. It is, for example, instructive to note that the vast majority of young women who return to diet for pregnancy choose to revert to a normal, unrestricted diet as soon as their baby is born. For these women the effects of improvements in cognitive function may be too subtle to compensate for the major practical and social inconveniences of being on-diet. These individual decisions are likely to be finely balanced, and it will be interesting to see what effect the ability to give patients with PKU routine feedback about cognitive parameters, by performing saccadometry regularly in the outpatient clinic, will have on their decisions about dietary management.
References
Albrecht J, Garbade SF, Burgard P (2009) Neuropsychological speed tests and blood phenylalanine levels in patients with phenylketonuria: a meta-analysis. Neurosci Biobehav Rev 33:414–421
Ali FR, Michell AW, Barker RA, Carpenter RHS (2006) The use of quantitative oculometry in the assessment of Huntington's disease. Exp Brain Res 169:237–245
Brenton DP, Pietz J (2000) Adult care in phenylketonuria and hyperphenylalaninaemia: the relevance of neurological abnormalities. Eur J Pediatr 159(Suppl 2):S114–120
Burgard P (2000) Development of intelligence in early treated phenylketonuria. Eur J Pediatr 159(Suppl 2):S74–79
Carpenter RH (2000) The neural control of looking. Curr Biol 10:R291–293
Carpenter RHS (2005) Visual pursuit: an instructive area of cortex. Curr Biol 15:R638–640
Carpenter RH, Williams ML (1995) Neural computation of log likelihood in control of saccadic eye movements. Nature 377:59–62
Christ SE, Huijbregts SC, de Sonneville LM, White DA (2010) Executive function in early-treated phenylketonuria: profile and underlying mechanisms. Mol Genet Metab 99:S22–S32
Cleary MA, Walter JH, Wraith JE, White F, Tyler K, Jenkins JP (1995) Magnetic resonance imaging in phenylketonuria: reversal of cerebral white matter change. J Pediatr 127:251–255
de Groot MJ, Hoeksma M, Blau N, Reijngoud DJ, van Spronsen FJ (2010) Pathogenesis of cognitive dysfunction in phenylketonuria: review of hypotheses. Mol Genet Metab 99(Suppl 1):S86–89
Gassió R, Campistol J, Vilaseca MA, Lambruschini N, Cambra FJ, Fusté E (2003) Do adult patients with phenylketonuria improve their quality of life after introduction/resumption of a phenylalanine-restricted diet? Acta Paediatr 92:1474–1478
Gentile JK, Ten Hoedt AE, Bosch AM (2010) Psychosocial aspects of PKU: hidden disabilities—a review. Mol Genet Metab 99(Suppl 1):S64–67
Klein C, Foerster F, Hartnegg K, Fischer B (2005) Lifespan development of pro- and anti-saccades: multiple regression models for point estimates. Brain Res Dev Brain Res 160:113–123
Levy HL, Ghavami M (1996) Maternal phenylketonuria: a metabolic teratogen. Teratology 53:176–184
Maillot F, Lilburn M, Baudin J, Morley DW, Lee PJ (2008) Factors influencing outcomes in the offspring of mothers with phenylketonuria during pregnancy: the importance of variation in maternal blood phenylalanine. Am J Clin Nutr 88:700–705
Ober JK, Przedpelska-Ober E, Gryncewicz W et al (2003) Hand-held system for ambulatory measurement of saccadic durations of neurological patients. In: Gajda J (ed) Modelling and measurement in medicine. Komitet Biocybernityki i Inzyneierii Biomedycznej PAN, Warsaw, pp 187–198
Pearson BC, Armitage KR, Horner CWM, Carpenter RHS (2007) Saccadometry: the possible application of latency distribution measurement for monitoring concussion. Br J Sports Med 41:610–612
Pietz J, Kreis R, Schmidt H, Meyding-Lamadé UK, Rupp A, Boesch C (1996) Phenylketonuria: findings at MR imaging and localized in vivo H-1 MR spectroscopy of the brain in patients with early treatment. Radiology 201:413–420
Pietz J, Kreis R, Rupp A, Mayatepek E, Rating D, Boesch C, Bremer HJ (1999) Large neutral amino acids block phenylalanine transport into brain tissue in patients with phenylketonuria. J Clin Invest 103:1169–1178
Donlon J, Levy H, Scriver CR (2008) Hyperphenylalaninemia: phenylalanine hydroxylase deficiency. In: Valle D, Beaudet AL, Vogelstein B (eds) The metabolic and molecular bases of inherited disease, online. McGraw-Hill, New York
van Spronsen FJ, Hoeksma M, Reijngoud D (2009) Brain dysfunction in phenylketonuria: is phenylalanine toxicity the only possible cause? J Inherit Metab Dis 32:46–51
Vermathen P, Robert-Tissot L, Pietz J, Lutz T, Boesch C, Kreis R (2007) Characterization of white matter alterations in phenylketonuria by magnetic resonance relaxometry and diffusion tensor imaging. Magn Reson Med 58:1145–1156
Walter JH, White FJ, Hall SK, MacDonald A, Rylance G, Boneh A, Francis DE, Shortland GJ, Schmidt M, Vail A (2002) How practical are recommendations for dietary control in phenylketonuria? Lancet 360:55–57
Acknowledgements
This work was undertaken at UCLH, which received a proportion of funding from the Department of Health’s NIHR Biomedical Research Centre funding scheme.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by: Bruce A. Barshop
Competing interest: None declared.
Rights and permissions
About this article
Cite this article
Dawson, C., Murphy, E., Maritz, C. et al. Dietary treatment of phenylketonuria: the effect of phenylalanine on reaction time. J Inherit Metab Dis 34, 449–454 (2011). https://doi.org/10.1007/s10545-010-9276-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10545-010-9276-2