Summary
Zellweger spectrum disorders (ZSD) are diagnosed by biochemical assay in blood, urine and cultured fibroblasts and PEX gene mutation identification. In most cases studies in fibroblasts corroborate results obtained in body fluids. In 1996 Clayton and colleagues described a 10-year old girl with evidence of a peroxisome disorder, based on elevated bile acid metabolites and phytanate. At the time it was not possible to distinguish whether she had a ZSD or a single peroxisomal protein defect. Studies in our laboratory showed that she also had elevated plasma pipecolate, supporting the former diagnosis. Despite the abnormal metabolites detected in blood (phytanate, bile acid intermediates and pipecolate), analysis of multiple peroxisomal pathways in fibroblasts yielded normal results. In addition, she had a milder clinical phenotype than usually associated with ZSD. Since complementation analysis to determine the gene defect was not possible, we screened this patient following the PEX Gene Screen algorithm (PGS). The PGS provides a template for sequencing PEX gene exons independent of complementation analysis. Two mutations in PEX10 were identified, a frameshift mutation inherited from her father and a de novo missense mutation in a conserved functional domain on the other allele. This case highlights that molecular analysis may be essential to the diagnosis of patients at the milder end of the ZSD spectrum. Furthermore, it supports the concept that some tissues are less affected by certain PEX gene defects than brain and liver.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Zellweger syndrome spectrum of peroxisome biogenesis disorders (PBD) comprises severe, neurodevelopmental diseases that arise from defects in at least 12 PEX genes (Steinberg et al 2006). The peroxins encoded by PEX genes are then unable to perform their normal role in peroxisome membrane formation or peroxisome matrix protein import into these organelles. Since peroxisomes fail to assemble normally, multiple biochemical pathways are affected. Patients with a classic presentation have elevations in plasma very long-chain fatty acids (VLCFA), pipecolic acid and C27-bile acid intermediates, and also have diminished erythrocyte plasmalogens. Phytanic acid and pristanic acid are normal at birth but can accumulate with dietary exposure to phytol in dairy and other dietary sources. Cultured fibroblasts have elevated VLCFA, deficient plasmalogen synthesis, deficient phytanic acid and pristanic acid oxidation, mislocalization of the peroxisomal matrix protein catalase to the cytosol, and absent or morphologically abnormal peroxisomes.
Not all PBD patients fit this classic picture. Some have normal erythrocyte plasmalogens and/or fibroblast plasmalogen synthesis. Likewise, abnormalities identified in body fluids are not always confirmed in cultured fibroblasts or the fibroblasts depict a mosaic pattern wherein some cells have normal matrix protein import but others are defective (Gootjes et al 2004a; Roels et al 2003). In some cases it is a challenge to discern whether the patient has a PBD or a single enzyme deficiency of peroxisome fatty acid β-oxidation. Recently a patient originally described as having trihydroxycholestanoic acidaemia had blood biochemistry more suggestive of a PBD; although all fibroblast parameters investigated yielded normal results, sequence analysis identified the PEX12 mutations R180X and L317F (Gootjes et al 2004b). We have reinvestigated a patient who presented as an 8-year-old girl with ataxia and had elevated plasma pristanic acid, phytanic acid, and bile acid intermediates, but normal fibroblast fatty acid oxidation (Clayton et al 1996). The determination of elevated pipecolic acid led us to investigate a PBD. We show that this now 22-year-old woman, referred to as patient PBD687, has a PEX10 deficiency.
Methods
Plasma VLCFA, erythrocyte plasmalogens, plasma and urine pipecolic acid, fibroblast VLCFA, fibroblast plasmalogen synthesis, fibroblast phytanic acid oxidation, fibroblast pristanic acid oxidation, catalase localization as assessed by the proportion of the total released to a soluble fraction (% soluble) after selective permeabilization of the plasma membrane with digitonin, and fibroblast immunocytochemical analysis were all performed as previously described (Bjorkhem et al 1986; Kelley 1991; Moser and Moser 1991; Roscher et al 1985; Wanders et al 1984; Zenger-Hain et al 1992). Immunocytochemical double labelling was performed using rabbit anti-PEX14 (1:200, gift of Dr Stephen Gould), mouse anti-catalase (1:5, gift of Dr Ronald Wanders), AlexaFluor 594 donkey anti-mouse (1:200, Molecular Probes, Eugene, OR, USA) and AlexaFluor 488 donkey anti-rabbit (1:200, Molecular Probes). Genomic DNA isolation and the PEX Gene Screen were performed as previously described (Steinberg et al 2004). Analysis of bile acids from urine, bile, and serum was performed as described previously (Setchell and Heubi 2006; Setchell et al 2003). Cloning was performed using the TOPO TA cloning kit (Invitrogen, USA) following the manufacturer’s instructions.
The PEX10 gene was reported to have two transcripts based on alternative splicing of intron 3 (Warren et al 2000); the shorter transcript encoding 19 fewer amino acids is the predominant transcript. According to ENSEMBL transcript ENST00000288774 there are 20 additional amino acids in the longer isoform (see http://www.dbpex.org/refseq/PEX10.pdf; retrieved 27 October 2006). Of the two longer putative transcripts, in silico modelling indicates that the splice site adding 19 amino acids is more favourable than the site that would add 20 amino acids (Yeo and Burge 2004). This is supported by the results of Warren and colleagues (2000), who detected a second, less abundant transcript with 57 additional nucleotides. Until this is resolved we have annotated sequence changes at the cDNA level based on the longest putative transcript (i.e. transcript 1 in Fig. 1).
PEX10 Splicing of Intron 3. Three splice variants have been recognized for PEX10. The three different potential intron 3 acceptor sites are shown as individual transcripts. In silico maximum entropy modelling suggests that transcripts 2 and 3 are the most likely isoforms (Yeo and Burge 2004)
Clinical summary
Patient PBD687 has two unaffected younger sisters; her mother had a spontaneous abortion at 14 weeks prior to the birth of patient PBD687. She was originally presented in this journal by Clayton and colleagues (Clayton et al 1996). At the time of publication she was 10 years old, and biochemical investigations indicated a novel, uncharacterized disorder of peroxisomal branched-chain fatty acid oxidation. In review, she was born of a full term pregnancy, birth weight 2.9 kg, and had normal early development. Around 3–4 years, she was first noted to have an unsteady gait, and then had progressive deterioration of motor abilities, including ataxia and dysarthria. IQ testing placed her cognitive abilities in the low normal range. Her past medical history was significant for absence of liver disease, retinal disease, or cataracts. She did not have hearing impairment or evidence of peripheral neuropathy.
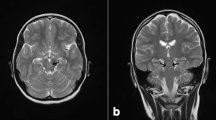
At 10 years of age she was started on bile acid supplementation with oral administration of cholic acid (10–15 mg/kg of body weight per day) with the aim of preventing onset of liver disease (Setchell et al 1992). She has continued on this regimen for the past 13 years. On examination at Kennedy Krieger Institute at age 10 years, her growth parameters were normal, and there were no dysmorphic features, ichthyosis or hepatomegaly. Her neurological examination was abnormal. She had slow speech with variation in volume, difficulty with handwriting, spelling and calculations. She did not have nystagmus, but had breakdown of pursuits and dysmetric saccades. She had marked ataxia on finger-to-nose and heel-shin testing, as well as gait ataxia. She had mild hypotonia, reflexes were 1+ knees, 0 elsewhere, downgoing toes, negative Romberg’s sign, and normal sensation. The MRI report showed moderately severe cerebellar atrophy and evidence of leukodystrophy.
At age 17 years, she was a well-developed, well-nourished young woman who was normal with the exception of having ataxia and delayed menarche that required oestrogen therapy. Pubic hair and breast development were Tanner Stage 4. She weighed 48.1 kg and was 163 cm tall with a body mass index of 18 kg/m2. Her vital signs were normal and her physical examination was unremarkable except for incoordination of gait and hand movement. Her laboratory examinations were unremarkable with normal serum alanine aminotransferase, aspartate aminotransferase, alkaline phosphatase, γ-glutamyl aminotransferase, albumin, total and conjugated bilirubin, and coagulation studies. Her serum cholesterol was 93 mg/dl. Complete blood count was normal, as were levels of vitamins 25-OH D, E and A. Liver biopsy histology revealed normal lobular architecture with no intralobular fibrosis and no cholestatic changes. Central vein and zone 3 sinusoidal architecture was normal.
There has been no neurological deterioration over the past decade, but she has not had a repeat brain scan. She has persistent nystagmus and ataxia, but there has been no cognitive decline and she completed a college programme.
Results
We measured blood metabolites when this patient was 10 years old (Table 1). Her plasma VLCFA had normal C26:0, but a slight increase in C26:0/C22:0 and borderline normal C24:0/C22:0. Her phytanic acid level was normal, but she was following a special low-phytol diet. When she was younger and on an unrestricted diet, her branched-chain fatty acids levels were elevated (Clayton et al 1996). Erythrocyte plasmalogens and urine pipecolic acid were normal, but plasma pipecolic acid was significantly elevated. Further studies in cultured fibroblasts did not identify any defects in peroxisome metabolism or assembly (Table 2). In addition, we cultured the cells at 40°C (Gootjes et al 2004a) but were unable to elicit any biochemical phenotype in the cultured cells at this higher temperature (Fig. 2). Neither was catalase import perturbed at 40°C. Figure 3 shows catalase immunocytochemical analysis in patient PBD687 and in PBD052, another Zellweger spectrum disorder (ZSD) patient with a PEX10 defect whose cultured cells had normal VLCFA at 37°C, but was responsive to the stress of 40°C (Fig. 2).
Biochemical Analyses in Fibroblasts Cultured at 37°C and 40°C. Biochemical assays were performed using cultured fibroblasts from patient PBD687, a normal control, and two other patients with PEX10 mutations. PBD052 had the genotype PEX10-R125X/H310E (Warren et al 1998) and had a mild biochemical defect, exhibiting normal very long-chain fatty acid (VLCFA) content (A) and plasmalogen synthesis (B) when cultured at 37°C. PBD100 was homozygous for c.600+1G>A (Warren et al 1998) and had a severe biochemical defect, with elevated VLCFA content (A) and deficient plasmalogen synthesis (B) at 37°C. However, PBD052 had mislocalized catalase (C), as determined by catalase solubility, and when cultured at 40°C elevated VLCFA (A). In contrast, patient PBD687 had normal results for all three parameters when cultured at 37°C and 40°C. The catalase solubility for patient PBD687 at 40°C is in the range (37.8% ± 13.6, n = 32) we observe for patients with the peroxisomal single enzyme disorder D-bifunctional protein deficiency
Immunostaining of fibroblasts cultured at 37° and 40°C. Fibroblasts from patient PBD687 and from PBD052, another PEX10-deficient cell line, were double-labelled with antibodies to the peroxisomal membrane protein PEX14 and the peroxisomal matrix protein catalase. For PBD052, peroxisome structures are detectable (A), but catalase is distributed throughout the cytoplasm (B). In contrast, fibroblasts from PBD687 show normal catalase import when cultured at 37°C (D) and 40°C (F). The approximate number and size of the peroxisome structures appear within normal limits at both temperatures (C, E)
Urinary fast-atom bombardment–mass spectrometry (FAB-MS) analysis revealed normal levels of bile acids (18.9 μmol/L; normal <20 μmol/L), but detected C27-cholestanoic acids (15% of the total). Gas chromatography–MS documented the presence of both dihydroxycholestanoic acid (DHCA) and trihydroxycholestanoic acid (THCA) along with a number of more polar hydroxylated cholestanoic acids (data not shown). FAB-MS analysis of the bile was also abnormal, detecting the taurine conjugate of DHCA (m/z 556) and THCA (m/z 572) (Fig. 4A). These ions are diagnostically definitive for a peroxisomal disorder involving the β-oxidation of bile acid intermediates. The lower intensity ions at m/z 448, 464, and 480 and m/z 498 and 514 reflect the synthesis of the usual glycine- and taurine-conjugated primary bile acids; the concentrations were relatively low, but consistent with impaired peroxisomal β-oxidation.
Bile acids in bile and serum DHCA enantiomers from PBD687. Negative ion FAB-MS spectra comparing the bile acid composition of bile from patient PBD687 before (A) and 7 years after treatment (B) with oral cholic acid (10 mg/kg body weight per day) are shown. Suppression of endogenous bile acid synthesis by cholic acid administration is confirmed by the disappearance of the highlighted ions m/z 540, 556 and 572 that represent dihydroxy-, trihydroxy- and tetrahydroxy-cholestanoic (C27) acids characteristic of the peroxisomal β-oxidation defect. The bile became enriched with conjugated cholic acid (m/z 514) and its metabolites derived from the therapy. Electrospray LC-MS analysis of bile from patient PBD687 identified the presence of both 25R and 25S diastereoisomers of THCA and DHCA, thus ruling out 2-methylacyl-CoA racemase deficiency. The ion current plot for tauro-THCA is shown (C)
The patient has been undergoing bile acid therapy with oral cholic acid since 10 years of age and routine annual monitoring of her urinary bile acid excretion has confirmed compliance with therapy and an essentially normal bile acid profile (results not shown). Downregulation in bile acid synthesis led to a marked decline in the proportions of C27 bile acids, particularly DHCA and THCA. FAB-MS analysis of bile showed a virtual disappearance of the C27 ions m/z 556 and m/z 572, concomitant with a predominance of the ions m/z 514 and m/z 464, representing the taurine and glycine conjugates, respectively, derived from cholic acid (Fig. 4B). Using electrospray liquid chromatography–MS we analysed the serum of this patient to ascertain the enantiomeric nature of the C27-cholestanoic acids. This ion current chromatogram revealed the presence in serum of both 25(R)- and 25(S)-DHCA in the typical normal ratio of 3:1 (Fig. 4C).
Based on the significant elevation in plasma pipecolic acid and the bile acid intermediates THCA and DHCA, we suspected that she had a peroxisome assembly defect. Since her cultured fibroblasts did not have a phenotype that could be used for complementation studies, we followed the PEX gene screen algorithm (Steinberg et al 2004) to search for PEX gene mutations. Sequence analysis of PEX10 exons 3–5 identified three heterozygous sequence variations: c.337delC, c.880A>G and c.890T>C. The mutation c.337delC causes a frameshift (L113fs) that would introduce a termination codon 39 amino acids downstream. Most likely this transcript is subject to nonsense-mediated decay (Frischmeyer and Dietz 1999). The variants c.880 A>G and c.890T>C cause the amino acid substitutions T294A and L297P, respectively. Other polymorphisms identified after sequencing the remaining three PEX10 exons are indicated in Fig. 5. We isolated DNA from the parents and found that the L113fs and T294A were both on the paternal allele (Fig. 5). L297P, however, appears to be a de novo mutation as this was not detected in either parent. Patient PBD687’s amplicons for exons 4 and 5 (derived from genomic DNA) were T/A cloned and then sequenced. Three of seven subclones had the genotypes c.880A and c.890C in cis, consistent with L297P arising on the maternal allele (Fig. 5); the remaining four clones had the genotypes c.880G and c.890T in cis. L297 is highly conserved evolutionarily (Fig. 6A). In addition, the majority of reported missense mutations of the PEX10 and PEX12 genes occur in the C3HC4 domain where L297 is located (Fig. 6B).
Pedigree for PBD687 showing PEX10 sequence variations. Haplotypes for PBD687 and her parents were determined based upon six PEX10 nucleotides sequenced from either purified PCR products or T/A clones derived from those products. The de novo PEX10 mutation at position c.890 (boxed) arose on one of the maternal chromosomes
PEX10 multiple sequence alignment. (a) A multiple sequence alignment shows that PEX10-L297 is highly conserved evolutionarily. (b) Alignment of PEX10 and PEX12 in mouse, rat and human in the region of the C3HC4 domain shows that PEX10-L297 resides next to a highly conserved cysteine residue. Furthermore, many other pathogenic amino acid substitutions have been reported within this domain for both proteins
Discussion
Zellweger spectrum disorder (ZSD) includes the neurodevelopmental syndromes Zellweger syndrome (OMIM 214100), neonatal adrenoleukodystrophy (OMIM 202370), and infantile Refsum disease (IRD; OMIM 266510) (Steinberg et al 2006). Patients with IRD have the mildest clinical and biochemical features. Cases have been reported of patients with biochemical or clinical features that are milder than the phenotype associated with IRD. For example, patients with PEX1 or PEX6 defects have been reported who had sensory defects but not the severe mental retardation associated with ZSD disorders (Moser et al 1995; Raas-Rothschild et al 2002). However, in both instances these patients had biochemical phenotypes in blood and cultured fibroblasts characteristic of ZSD. In contrast, Gootjes and colleagues showed that a patient with apparently normal peroxisome function in cultured fibroblasts had a PEX12 defect (Gootjes et al 2004b). In general it is rare for a patient in the ZSD not to have abnormalities in blood and cultured fibroblasts that demonstrate characteristic defects in peroxisome assembly and metabolism.
Our patient, PBD687, initially appeared to have an isolated defect in fatty acid metabolism. However, she also had a persistent significant elevation in plasma pipecolic acid. Although nonspecific liver disease and diet may be associated with pipecolic acidaemia (Baas et al 2002), its coexistence with DHCA and THCA acidaemia indicated that two separate peroxisomal pathways were defective, suggesting a generalized defect in peroxisome assembly. We were not able to demonstrate any defects in peroxisome metabolism or assembly in cultured fibroblasts of patient PBD687. This may be due to the artificial growth conditions of the cultured cells and/or tissue specificity of the defect. The abnormal metabolites detected in the blood of PBD687 are the result of defective liver metabolism. Stressing the cultured cells by growth at 40°C did not elicit any observable perturbations of peroxisome metabolism or assembly. Perhaps studies in liver tissue would demonstrate perturbations of peroxisome assembly not detectable in the cultured fibroblasts.
We previously reported that sequence analysis of 12 exons across the six PEX genes most commonly defective in ZSD, the PEX Gene Screen algorithm, identified at least one pathogenic mutation in 79% of ZSD patients (Steinberg et al 2004). In the absence of a marker for complementation studies of patient PBD687, this patient was an ideal candidate for the PEX Gene Screen algorithm. This analysis identified one clearly pathogenic PEX10 mutation (c.337delC) that was paternally inherited and one PEX10 missense mutation (L297P) that was de novo. L297 is highly conserved evolutionarily and resides in the C3HC4 domain, a functionally important part of zinc-RING finger proteins. Interestingly, other missense mutations have been reported in this domain in PEX10 and PEX12 and have on the whole been associated with milder biochemical and clinical phenotypes. The PEX12 mutation S320F has been reported multiple times, often in the homozygous state. Gootjes and colleagues reported eight S320F homozygotes (Gootjes et al 2004a) that all had abnormalities of blood metabolites including VLCFA and bile acid intermediates, but in cultured fibroblasts the results were mostly normal. However, their cultured fibroblasts had a mosaic pattern of catalase immunofluorescence, meaning that some cells had diffuse, cytosolic catalase and some cells had particulate, peroxisome-localized catalase. Furthermore, culturing the cells at 40°C exacerbated the defect and made the catalase import defect apparent in all of the cells. In contrast, we were not able to demonstrate any evidence of impaired peroxisome import or assembly in fibroblasts of patient PBD687, whether cultured at 37°C or 40°C. This is significant because catalase is recognized as one of the peroxisome matrix proteins most susceptible to perturbations of the import machinery. Our inability to elicit a defect in peroxisome assembly at 40°C in fibroblasts of patient PBD687 suggests that PEX10-L297P, in contrast to PEX12-S320F, is not temperature sensitive.
C27 bile acids are not normally present in the urine of healthy children and adults. The profiles for patient PBD687’s urine and bile were consistent with a defect in peroxisomal β-oxidation. Given the unusual biochemical presentation, we explored the possibility of a defect involving a deficiency in the 2-methylacyl-CoA racemase, an enzyme responsible for conversion of 25(S)- to 25(R)- diastereoisomers of DHCA and THCA (Ferdinandusse et al 2001; Setchell et al 2003). However, the presence of both (R)-and (S)- diastereoisomers of DHCA and THCA in serum and bile ruled out the possibility of a deficiency in 2-methylacyl-CoA racemase. Although the molecular basis of the error in bile acid metabolism for this patient was not known, early recognition of DHCA and THCA uraemia and acidaemia permitted the start of bile acid supplementation before severe liver disease developed.
Rat studies have shown that administration of tauro-THCA causes a hepatic lesion with mitochondrial membrane disruption similar to that observed in patients with Zellweger syndrome (Hanson et al 1977; Mathis et al 1980). Beneficial effects of cholic acid therapy on liver function were first reported in a Zellweger syndrome patient and have subsequently been found to be clinically helpful in a number of patients with single enzyme defects in peroxisomal function (Setchell and Heubi 2006; Setchell et al 1992). The low risk of serious side-effects from cholic acid therapy and its clinical efficacy in other bile acid synthetic defects made this an obvious approach to managing a patient in this situation. Therapy in patient PBD687 was associated with maintenance of normal liver function tests and a significant suppression in endogenous bile acid synthesis as seen from the virtual disappearance of C27 bile acids.
This patient received bile acid therapy, phytanic acid restriction, fat-soluble vitamin supplementation, and DHA supplementation. We do not know whether any of these therapies alone or in combination improved her clinical outcome, contributed to arresting neurological deterioration, or protected her liver from toxic damage. Biochemistry and histology indicate that her liver is functioning well and remains healthy. There are additional long-term consequences of ZSD, including urolithiasis associated with deficient alanine glyoxylate aminotransferase, adrenal dysfunction, and the development of leukodystrophy (Gould et al 2001). The pathogenesis of leukodystrophy is poorly understood in peroxisomal disorders associated with elevated VLCFA content. There are, however, therapeutic options to prevent or minimize the onset of leukodystrophy. The rationale for treatment with Lorenzo’s oil would be questionable in a patient who has relatively normal plasma VLCFA levels (Moser et al 2005), although we cannot rule out the possibility of accumulations arising in nervous system and hepatic tissues. Bone marrow transplantation has been established as an approach to halting demyelination in boys with X-linked adrenoleukodystrophy who have not been functionally impacted (Mahmood et al 2007). Annual brain MRI and neuropsychological testing would be an approach to monitoring a patient such as this, so that treatment modalities could be implemented at an early stage and have a better chance of preserving cognitive function.
This case highlights several important points regarding the diagnosis of patients suspected to have a defect in peroxisome metabolism. The elevation in pipecolic acid was critical to determining that this patient had an assembly defect rather than an isolated defect in peroxisomal β-oxidation. Thus, although pipecolic acidaemia can be associated with nonspecific liver disease, diet, or the isolated defect of alpha-aminoadipic semialdehyde dehydrogenase deficiency, it is a very useful marker when measured in conjunction with other peroxisomal biomarkers (Baas et al 2002; Mills et al 2006; Peduto et al 2004). Rarely, elevations in plasma pipecolic acid have been reported in patients with the peroxisomal disorders rhizomelic chondrodysplasia punctata and adult Refsum disease, although the basis of this is not understood (Peduto et al 2004). In addition, this case provides another example of a patient with a clinical phenotype outside of the classic spectrum associated with assembly defects. Thus, it highlights the importance of comprehensive blood and urine analyses in patients outside of the classic ZSD to rule out a diagnosis. Furthermore, it shows the utility of direct DNA analysis in patients suspected to have a PEX gene defect without first performing complementation studies. Finally, we suggest that missense alleles in the zinc finger region of PEX10 and PEX12 are associated with milder phenotypes as shown here for PEX10-L297P, and PEX10-H310D (PBD723, http://www.dbpex.org), PEX10-H310Q (Warren et al 2000), PEX12-S320F (Gootjes et al 2004a), and PEX12-L317F (Gootjes et al 2004b).
Abbreviations
- DHCA:
-
3α,7α-dihydroxy-5β-cholestanoic acid
- DMA:
-
dimethylacetal
- FAB-MS:
-
fast-atom bombardment–mass spectrometry
- IQ:
-
intelligence quotient
- IRD:
-
infantile Refsum disease
- MRI:
-
magnetic resonance imaging
- MS:
-
mass spectrometry
- PBD:
-
peroxisome biogenesis disorder
- THCA:
-
3α,7α,12α-trihydroxy-5β-cholestanoic acid
- VLCFA:
-
very long-chain fatty acids
- ZSD:
-
Zellweger spectrum disorder
References
Baas JC, van de Laar R, Baas JCM, et al (2002) Plasma pipecolic acid is frequently elevated in non-peroxisomal disease. J Inherit Metab Dis 25(8): 699-701. doi:10.1023/A:1022889400302.
Bjorkhem I, Sisfontes L, Bostrom B, Kase BF, Blomstrand R (1986) Simple diagnosis of the Zellweger syndrome by gas–liquid chromatography of dimethylacetals. J Lipid Res 27(7): 786–791.
Clayton PT, Johnson AW, Mills KA, et al (1996) Ataxia associated with increased plasma concentrations of pristanic acid, phytanic acid and C27 bile acids but normal fibroblast branched-chain fatty acid oxidation. J Inherit Metab Dis 19(6): 761–768. doi:10.1007/BF01799170.
Ferdinandusse S, Overmars SH, Denis S, Waterham HR, Wanders RJ, Vreken P (2001) Plasma analysis of di- and trihydroxycholestanoic acid diastereoisomers in peroxisomal alpha-methylacyl-CoA racemase deficiency. J Lipid Res 42(1): 137–141.
Frischmeyer PA, Dietz HC (1999) Nonsense-mediated mRNA decay in health and disease. Hum Mol Genet 8(10): 1893–1900. doi:10.1093/hmg/8.10.1893.
Gootjes J, Schmohl F, Mooijer PAW, et al (2004a) Identification of the molecular defect in patients with peroxisomal mosaicism using a novel method involving culturing of cells at 40 degrees C: implications for other inborn errors of metabolism. Hum Mutat 24(2): 130–139. doi:10.1002/humu.20062.
Gootjes J, Skovby F, Christensen E, Wanders RJA, Ferdinandusse S (2004b) Reinvestigation of trihydroxycholestanoic acidemia reveals a peroxisome biogenesis disorder. Neurology 62(11): 2077–2081.
Gould SJ, Raymond GV, Valle D (2001) The peroxisome biogenesis disorders. In: Scriver CR, Beaudet AL, Sly WS, Valle D, eds; Childs B, Kinzler KW, Vogelstein B, assoc. eds. The Metabolic and Molecular Bases of Inherited Disease, 8th edn. New York: McGraw-Hill, 3181–3217.
Hanson RF, Williams GC, Hachey D, Sharp HL (1977) Hepatic lesions and hemolysis following administration of 3alpha, 7alpha, 12alpha-trihydroxy-5beta-cholestan-26-oyl taurine to rats. J Lab Clin Med 90(3): 536–548.
Kelley R (1991) Quantification of pipecolic acid in plasma and urine by isotope-dilution gas chromatography/mass spectrometry. In: Hommes F, ed. Techniques in Diagnostic Human Biochemical Genetics. New York: Wiley-Liss, 205–218.
Mahmood A, Raymond GV, Dubey P, Peters C, Moser HW (2007) Survival analysis of haematopoietic cell transplantation for childhood cerebral X-linked adrenoleukodystrophy: a comparison study. Lancet Neurol 6(8): 687–692. doi:10.1016/S1474-4422(07)70177-1.
Mathis RK, Watkins JB, Szczepanik-Van Leeuwen P, Lott IT (1980) Liver in the cerebro-hepato-renal syndrome: defective bile acid synthesis and abnormal mitochondria. Gastroenterology 79(6): 1311–1317.
Mills PB, Struys E, Jakobs C, et al (2006) Mutations in antiquitin in individuals with pyridoxine-dependent seizures. Nat Med 12(3): 307–309. doi:10.1038/nm1366.
Moser AB, Rasmussen M, Naidu S, et al (1995) Phenotype of patients with peroxisomal disorders subdivided into sixteen complementation groups. J Pediatr 127(1): 13–22. doi:10.1016/S0022-3476(95)70250-4.
Moser HW, Moser AB (1991) Measurement of saturated very long chain fatty acids in plasma. In: Hommes F, ed. Techniques in Diagnostic Human Biochemical Genetics. New York: Wiley-Liss, 177–191.
Moser HW, Raymond GV, Lu SE, et al (2005) Follow-up of 89 asymptomatic patients with adrenoleukodystrophy treated with Lorenzo’s oil. Arch Neurol 62(7): 1073–1080. doi:10.1001/archneur.62.7.1073.
Peduto A, Baumgartner MR, Verhoeven NM, et al (2004) Hyperpipecolic acidaemia: a diagnostic tool for peroxisomal disorders. Mol Genet Metab 82(3): 224–230. doi:10.1016/j.ymgme.2004.04.010.
Raas-Rothschild A, Wanders RJ, Mooijer PA, et al (2002) A PEX6-defective peroxisomal biogenesis disorder with severe phenotype in an infant, versus mild phenotype resembling Usher syndrome in the affected parents. Am J Hum Genet 70(4): 1062–1068. doi:10.1086/339766.
Roels F, Saudubray JM, Giros M, et al (2003) Peroxisome mosaics. Adv Exp Med Biol 544: 97–106.
Roscher A, Molzer B, Bernheimer H, Stockler S, Mutz I, Paltauf F (1985) The cerebrohepatorenal (Zellweger) syndrome: an improved method for the biochemical diagnosis and its potential value for prenatal detection. Pediatr Res 19(9): 930–933. doi:10.1203/00006450-198509000-00013.
Setchell KD, Bragetti P, Zimmer-Nechemias L, et al (1992) Oral bile acid treatment and the patient with Zellweger syndrome. Hepatology 15(2): 198–207. doi:10.1002/hep.1840150206.
Setchell KD, Heubi JE, Bove KE, et al (2003) Liver disease caused by failure to racemize trihydroxycholestanoic acid: gene mutation and effect of bile acid therapy. Gastroenterology 124(1): 217–232. doi:10.1053/gast.2003.50017.
Setchell KD, Heubi JE (2006) Defects in bile acid biosynthesis–diagnosis and treatment. J Pediatr Gastroenterol Nutr 43(Supplement 1): S17–S22. doi:10.1097/01.mpg.0000226386.79483.7b.
Steinberg S, Chen L, Wei L, et al (2004) The PEX Gene Screen: molecular diagnosis of peroxisome biogenesis disorders in the Zellweger syndrome spectrum. Mol Genet Metab 83(3): 252–263. doi:10.1016/j.ymgme.2004.08.008.
Steinberg SJ, Dodt G, Raymond GV, Braverman NE, Moser AB, Moser HW (2006) Peroxisome biogenesis disorders. Biochim Biophys Acta 1763(12): 1733–1748. doi:10.1016/j.bbamcr.2006.09.010.
Wanders RJ, Kos M, Roest B, et al (1984) Activity of peroxisomal enzymes and intracellular distribution of catalase in Zellweger syndrome. Biochem Biophys Res Commun 123(3): 1054–1061. doi:10.1016/S0006-291X(84)80240-5.
Warren DS, Morrell JC, Moser HW, Valle D, Gould SJ (1998) Identification of PEX10, the gene defective in complementation group 7 of the peroxisome-biogenesis disorders. Am J Hum Genet 63(2): 347–359. doi:10.1086/301963.
Warren DS, Wolfe BD, Gould SJ (2000) Phenotype-genotype relationships in PEX10-deficient peroxisome biogenesis disorder patients. Hum Mutat 15(6): 509–521. doi:10.1002/1098-1004(200006)15:6<509::AID-HUMU3>3.0.CO;2-#.
Yeo G, Burge CB (2004) Maximum entropy modeling of short sequence motifs with applications to RNA splicing signals. JComput Biol 11(2–3): 377–394. doi:10.1089/1066527041410418.
Zenger-Hain J, Craft DA, Rizzo WB (1992) Diagnosis of inborn errors of phytanic acid oxidation using tritiated phytanic acid. In: Coates PM, Tanaka K, eds. New Developments in Fatty Acid Oxidation. New York: Wiley-Liss, 399–407.
Acknowledgements
Thank you to Cicely Toomer for her technical guidance in performing immunocytochemical analysis in cultured fibroblasts. This work would not have been possible without the fortitude and commitment of Dr Hugo W. Moser. This study was funded by NIH grant HD010981-29 sponsored by NICHD. Grant RR08084 from the NIH National Center for Research Resources sponsored K.D.R.S. and J.E.H.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicating editor: Ronald Wanders
Competing interests: None declared
References to electronic databases: PEX Gene Database (dbpex) http://www.dbpex.org. Ensembl: ENST00000288774.
Rights and permissions
About this article
Cite this article
Steinberg, S.J., Snowden, A., Braverman, N.E. et al. A PEX10 defect in a patient with no detectable defect in peroxisome assembly or metabolism in cultured fibroblasts. J Inherit Metab Dis 32, 109–119 (2009). https://doi.org/10.1007/s10545-008-0969-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10545-008-0969-8