Summary
Inherited disorders of amino and organic acid metabolism have a high cumulative frequency, and despite heterogeneous aetiology and varying clinical presentation, the manifestation of neurological disease is common. It has been demonstrated for some of these diseases that accumulating pathological metabolites are directly involved in the manifestation of neurological disease. Various pathomechanisms have been suggested in different in vitro and in vivo models including an impairment of brain energy metabolism, an imbalance of excitatory and inhibitory neurotransmission, altered transport across the blood–brain barrier and between glial cells and neurons, impairment of myelination and disturbed neuronal efflux of metabolic water. This review summarizes recent knowledge on pathomechanisms involved in phenylketonuria, glutaric aciduria type I, succinic semialdehyde dehydrogenase deficiency and aspartoacylase deficiency with examples, highlighting general as well as disease-specific concepts and their putative impact on treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
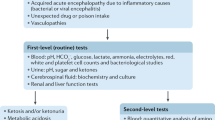
Despite heterogeneous aetiology and varying clinical presentation, the onset of neurological disease is common in inherited disorders of amino acid and organic acid metabolism. Among them, cerebral organic acidurias, such glutaric aciduria type I (GA I; OMIM #231670), d-2-hydroxyglutaric aciduria (OMIM #600721) and l-2-hydroxyglutaric aciduria (OMIM #236792; succinic semialdehyde dehydrogenase (SSADH) deficiency (OMIM #271980) and aspartoacylase deficiency (synonym, Canavan–Bogaert–Bertrand disease; OMIM #271900), and amino acid disorders such as phenylketonuria (PKU; OMIM #261600) and maple syrup urine disorder (OMIM #248600) present predominantly or even exclusively with neurological symptoms, whereas inclassical organic acidurias, such as methylmalonic (mut0, OMIM #251000) and propionic acidurias (OMIM #606054), neurological diseases usually manifest in combination with the involvement of other organs including skeletal and heart muscle, kidneys, liver and pancreas. However, children with classical organic acidurias may present exclusively with neurological symptoms.
Neurological symptoms may occur acutely, such as cytotoxic or vasogenic oedema, ‘metabolic stroke’ and acute encephalopathic crises characteristically involving the basal ganglia (Funk et al 2005; Heidenreich et al 1988; Kölker et al 2007; Strauss et al 2003; 2007). However, neurological deterioration may progress over many years, resulting in cerebral or cerebellar atrophy, basal ganglia injury, white-matter disease, and optic nerve atrophy (Huttenlocher 2000; Külkens et al 2005; Matalon et al 1988; Pearl et al 2003; Thompson et al 1993). Owing to the involvement of grey and white matter in various brain regions, the neurological presentation of affected individuals with disorders of amino and organic acid metabolism is wide, including developmental delay, motor dysfunction (e.g. muscular hypotonia, spasticity, dystonia, chorea, ataxia), cognitive dysfunction (e.g. mental retardation, delayed speech development, behavioural problems), psychiatric disease, epilepsy, and macrocephaly or microcephaly (Matalon et al 1988; Nikolaides et al 1998; Paine 1957; Strauss et al 2003; Surtees et al 1992). Despite the heterogeneous nature of these inborn errors of metabolism, recent pathophysiological concepts for some of these diseases have highlighted that frequent CNS involvement may be the consequence of impairment of brain energy metabolism and transport mechanisms including the blood–brain barrier (BBB) and the metabolic coupling between astrocytes and neurons.
An approach to neurometabolism: From evolution of man to modern neuroenergetics
The brain volume of the genus Homo has been tripled within 2.5 million years of evolution, resulting in an increase of the brain-to-body ratio compared to apes. This had significant consequences for the neurometabolism of Homo sapiens sapiens. It has been estimated that in adults glucose and oxygen consumption of the CNS accounts for approximately 20% of the total daily demand of the human body, although the brain weight makes up approximately 2% of the body weight (Sokoloff 1960). During intrauterine development as well as in young infants, the energetic costs of the CNS may increase up to 60–70% of the daily demand. The major consumers of brain energy are excitatory glutamatergic neurons, and in particular the Na+/K+-ATPases that are indispensable to restore the resting membrane potential and Na+-dependent glutamate transport (Erecinska and Dagani 1990).
Not unexpectedly, the increasing energy demand of the human brain has had tremendous phylogenetic and ontogenetic consequences: (1) requirement of food with a high biological quality which is confirmed by the observation that in primates brain volumes correlate with the quality of the diet (Leonard and Robertson 1992); (2) the involution of organs with a high energy demand, in particular the digestive system, which has been formulated along with the ‘expensive tissue hypothesis’ (Aiello and Wheeler 1995); (3) slow intrauterine growth of the body, long duration of pregnancy and single offspring (Hofman 1983); and (4) decrease in interbirth intervals compared to gorilla and chimpanzees, reducing the high energetic costs of breastfeeding (Galdikas and Wood 1990).
After Roy and Sherrington published their groundbreaking paper on the regulation of blood supply of the brain in 1890; it was confirmed in many ways that neuronal activity, brain energy metabolism and cerebral blood flow are directly coupled (Roy and Sherrington 1890). Sokoloff has demonstrated using the 2-deoxyglucose method that glucose is the primary energy substrate of the brain and that glucose is almost completely oxidized to carbon dioxide and water (Sokoloff 1991). This has been the dogma of classical neuroenergetics for many decades. However, modern neuroenergetics has highlighted that astrocytes, which make up half of the brain volume and are 10-fold higher in number than neurons, are indispensable for the understanding of brain energy metabolism. Neuroanatomically, astrocytes are suggested to function as sensors of neuronal activity since they have close connections with synapses and microvessels. The astrocyte-to-neuron ratio has increased during evolution, which may reflect increasing energy demand of the growing neocortex (Sherwood et al 2006). Three distinct biochemical pathways have been delineated that are the basis of the bioenergetic coupling between astrocytes and neurons forming a neuroenergetic unit:
-
1.
The glutamate/glutamine cycle manages glutamate uptake from the synaptic cleft and glutamate recycling following synthesis of glutamine in astrocytes (Schousboe et al 1993).
-
2.
The astrocyte-to-neuron lactate shuttle allows transport and oxidation of lactate in neurons (Magistretti et al 1999). In fact, evidence supports the notion that under certain conditions lactate is the primary energy substrate of neurons instead of glucose, challenging the dogma of classical neuroenergetics (Bouzier-Sore et al 2003).
-
3.
The dicarboxylic acid shuttle from astrocytes to neurons compensates for the constant drain of dicarboxylic acids from the tricarboxylic acid (TCA) cycle for glutamate neosynthesis (Schousboe et al 1997). This shuttle prevents decreased flux through the TCA cycle since neurons are suggested to lack an important anaplerotic mechanism, in particular pyruvate carboxylase.
Last but not least, neurometabolism cannot be understood without consideration of the BBB. The BBB is a specialized system of brain microvascular endothelial cells rich in tight junctions that shield the brain from toxic substances in the blood; it supplies brain tissues with nutrients and filters harmful compounds from the brain back to the bloodstream. The close interaction between endothelial cells and other components of the neurovascular unit (astrocytes, pericytes and basement membrane) ensures proper function of the central nervous system (Persidsky et al 2006). This physiological barrier strongly limits the transport of hydrophilic compounds (e.g. glucose, amino acids, monocarboxylic acids) from blood to brain (influx) and from brain to blood (efflux). Many transporters for specific hydrophilic substrates with various substrate specificities, capacities and affinities have been identified that allow the BBB to function as a gatekeeper (Pardridge 1998).
The improved understanding of neurometabolism has significantly influenced the unravelling of pathomechanisms underlying neurological disease in inborn errors of metabolism (IEMs). In the following, basic pathomechanistic principles of CNS involvement in disorders of amino and organic acid metabolism (PKU, GA I, SSADH deficiency, and aspartoacylase deficiency) are discussed with examples.
Amino acid disorders
Classical phenylketonuria
PKU (OMIM #261600), which has a prevalence of approximately 1:8000 newborns in Europe, was the first neurogenetic disorder identified (Følling 1934) and the first successfully treated IEM (Bickel et al 1953). Furthermore, PKU was instrumental for the introduction of newborn mass screening by Guthrie and Susi (1963) and is now diagnosed most commonly in routine screening of newborns. PKU is caused by autosomal recessively inherited disease-causing mutations in the PAH gene on chromosome 12q24.1 resulting in deficient activity of phenylalanine hydroxylase (EC 1.14.16.1) which leads to intolerance of dietary phenylalanine and reduced tyrosine production. Before it was known that PKU was treatable and before newborn mass screening was established in many countries worldwide, affected individuals suffered severe mental retardation, microcephaly, epilepsy, spasticity and behavioural problems, and neuropathological studies have demonstrated low brain weight, white-matter lesions, decreased myelin formation and dopamine, norepinephrine and serotonin production, and less-developed dendritic trees in untreated patients (Huttenlocher 2000; Paine 1957). Despite significant progress in the management of patients with PKU, the pathogenesis is less clear.
While phenylalanine hydroxylase is expressed in liver and kidneys, the manifestation of PKU is predominantly neurological. This has led to consideration of how the disease is ‘transported’ to the CNS. The most conclusive explanation as outlined by the ‘large neutral amino acid (LNAA) hypothesis’ is that elevations of phenylalanine in plasma impair the transport of LNAA via system L (Pietz et al 1999). System L has a high affinity for LNAA, resulting in selective vulnerability to derangements of single LNAAs in plasma. As a consequence of competition at the BBB, LNAA are depleted in the CNS compartment, resulting in decreased protein synthesis and decreased production of serotonin, catecholamines, histamine, carnosine and S-adenosylmethionine (Matalon et al 2003; McKean 1972; Pardridge 1998; Pietz et al 1999; Smith et al 1988). Supplementation with LNAA can reduce brain levels of phenylalanine despite high serum levels by competition at this transporter and therefore is under investigation as a dietary therapy (Pietz et al 1999).
In addition to LNAA depletion, increased phenylalanine concentrations in the CNS mediate direct effects. These include competition of phenylalanine with glycine at the glycine-binding site of NMDA receptors and with glutamate at the glutamate binding site of AMPA receptors. This has implications for long-term changes in glutamatergic synaptic transmission, demonstrated by phenylalanine-induced increased expression of glutamate receptor subunits NR2A, GluR1 and GluR2/3 and decreased expression of NR2B (Glushakov et al 2003, 2005). The glutamatergic neurotransmission plays a key role in synaptic function and density, memory and learning, epilepsy, dendritic arborization, and the regulation of apoptosis in the immature brain (Collingridge et al 1983; Erwald et al 2008; Fox et al 1991; Ikonomidou et al 1999; Meador 2007; Pawlak et al 2005; Rowland et al 2005; Tsukada et al 2005). Given the important role of the glutamatergic system in brain development and function, these changes may, at least in part, explain the brain disorder associated with untreated PKU (Huttenlocher 2000). Furthermore, it has been suggested that phenylalanine may affect myelination in the forebrain. This is supported by the reduction of 3-hydroxy-3-methylglutaryl-CoA reductase activity and cholesterol synthesis in the forebrains of pah enu2 mice, a transgenic mouse modelfor PKU (Shefer et al 2000), the identification of phenylalanine-sensitive oligodendroglial subpopulations in the forebrain, and the observation that size and nature of white-matter lesions correlate with blood phenylalanine levels (Bick et al 1991; Dyer et al 1996; Huttenlocher 2000; Shefer et al 2000; Thompson et al 1993).
Some studies have demonstrated that brain energy metabolism is altered in PKU, which is demonstrated by impairment of glucose metabolism in PKU patients and pah enu2 mice and following phenylalanine loadingin rats, as well as by the phenylalanine-induced inhibition of pyruvate kinase (Hasselbalch et al 1996; Hörster et al 2006; Quin and Smith 2007; Weber 1969). However, it remains to be elucidated whether impaired brain energy metabolism is a primary change in PKU orwhether it reflects reduced functional activity along withsilencing of cost-extensive glutamatergic signalling.
Magnetic resonance (MR) spectroscopy studies have demonstrated that patients’ brain phenylalanine concentrations were different in spite of similar plasma levels following oral phenylalanine load. Interindividual apparent Michaelis constants, brain influx ratios and consumption rates varied significantly in clinically typical patients and untreated, normally intelligent, adult patients. Thus such variations seem to be a major causative factor for the individual vulnerability to PKU (Möller et al 1998; Weglage et al 2002). Although it is not yet identified, a second catalytic variant affecting amino acid transport at the BBB is a likely candidate for protection against high phenylalanine concentrations in the brain (Trefz et al 2000).
In conclusion, despite interindividual variations, solid evidence confirms the notion that increased plasma concentrations of phenylalanine correlate directly with the onset or deterioration of neurological disease in PKU. This has led to the successful development of phenylalanine-restricted dietary treatment, which prevents the onset of neurological disease in pre-symptomatically diagnosed individuals. Since responsiveness to tetrahydrobiopterin is more prevalent than was previously assumed, particularly in patients with mild PKU, long-term treatment with tetrahydrobiopterin could be a potential treatment option for a subgroup of patients (Burnett 2007; Fiege and Blau 2007; Muntau et al 2002; Trefz et al 2005).
Organic acidurias
General concepts
At present, there is no unifying and generally accepted concept for the neuropathogenesis of organic acidurias (OADs). A few general pathogenetic concepts have been introduced.
-
1.
‘Metabolic stroke’ and toxic metabolite hypothesis: Owing to the stroke-like onset of neurodegenerative changes in OADs that may evolve during acute encephalopathic or acute metabolic crises and that particularly affect the basal ganglia, the term ‘metabolic stroke’ has been introduced (Heidenreich et al 1988). It has been suggested that these lesions are induced by an accumulation of putatively toxic metabolites and that they cannot be explained by hypoxaemia or vascular insufficiency, nor do the lesions fit a vascular distribution when detected on neuroimaging studies. A limitation of this concept is that it is purely descriptive and lacks a conclusive pathophysiological and neuroradiological definition. However, this concept has for the first time highlighted that accumulating pathological metabolites may contribute to the manifestation of neurological disease in OADs.
The contribution of putatively toxic metabolites to neurological disease is the backbone of recent pathophysiological hypotheses for OADs (Kölker et al 2004; Okun et al 2002; Sauer et al 2005, 2006; Schwab et al 2006; Ullrich et al 1999; Zinnanti et al 2006) involving excitotoxic cell damage and mitochondrial dysfunction. A limitation of this concept is that tissue-specific concentrations of accumulating metabolites are only known for a few OADs because of a lack of postmortem studies and rare animal studies. Furthermore, OADs often lack a clear-cut correlation between the biochemical and clinical phenotypes.
-
2.
Trapping hypothesis: Recently, it has been demonstrated that glutaric and 3-hydroxyglutaric acids strongly accumulate in the brain following intracerebral de novo synthesis and owing to a very limited efflux from brain to blood (Funk et al 2005; Sauer et al 2006). The physiological basis of this observation is the lack of a known high-capacity transporter system for dicarboxylic acids at the BBB, facilitating the cerebral accumulation of non-permeating compounds if these are produced within the brain compartment (Hassel et al 2002). It has been hypothesized that, as a result of the very limited efflux, in certain OADs there is pathological accumulation of dicarboxylic acids in the brain secondary to the metabolic block (Kölker et al 2006a). At high concentrations some of these compounds may become neurotoxic. This is the second identified principle in which the BBB significantly contributes to the manifestation of neurological disease in IEM. In contrast to the BBB, glutaric and 3-hydroxyglutaric acids are transported along thedicarboxylate shuttle between astrocytes and neurons, mediated by dicarboxylate transporters NaC2 and NaC3 which are expressed on neurons and astrocytes (Stellmer et al 2007; Yodoya et al 2006).
Glutaric aciduria type I
The molecular basis of GA I (OMIM #231670) relies on autosomal recessively inherited deficiency of glutaryl-CoA dehydrogenase (EC 1.3.99.7), which is encoded by the GCDH gene localized on chromosome 19p13.2. The onset of acute striatal injury, which manifests during acute encephalopathic crises mostly before the age of 3 years, is the prognostically relevant event in GA I (Kölker et al 2006b; Strauss et al 2003). Such crises are usually precipitated by conditions that are likely to induce catabolic state, e.g. infectious diseases (Hoffmann et al 1996). Striatal injury is irreversible and most characteristically results in dystonia or other extrapyramidal manifestations such as chorea (Kölker et al 2006b; Strauss et al 2007). Recent studies have highlighted that acute striatal injury may be induced by a synergistic effect of accumulating metabolites (glutaric acid, 3-hydroxyglutaric acid, glutaryl-CoA) in combination with age-dependent and area-specific changes during brain maturation. Specifically, it was shown that accumulating metabolites induce activation of NMDA receptors (Kölker et al 2004); inhibition of glutamate uptake from the synaptic cleft (Porciuncula et al 2000); depletion of the intracellular phosphate pool (Ullrich et al 1999); inhibition of the glutamate decarboxylase, the key enzyme of GABA synthesis (Stokke et al 1976); inhibition of the α-ketoglutarate dehydrogenase complex, the rate-limiting enzyme of the TCA cycle (Sauer et al 2005); disturbance of the dicarboxylate shuttle between astrocytes and neurons (Stellmer et al 2007; Yodoya et al 2006); and dysfunction and cell death of microvessel endothelial cells (Mühlhausen et al 2006) and oligodendroglial precursors (Gerstner et al 2005).
Recently, oral lysine loading in Gcdh −/− mice, a transgenic mouse model for GA I (Koeller et al 2002), produced a clinical phenotype similar to acute encephalopathic crises in affected individuals (Zinnanti et al 2006). The onset of neurological disease was accompanied by an increase of putatively toxic metabolites in the brain compartment. The manifestation of cerebral injury was prevented by treatment with homoarginine, limiting the lysine influx into the brain and, as a consequence, intracerebral production of toxic metabolites (Zinnanti et al 2007). This is in line with previous animal and postmortem studies which have highlighted that concentrations of glutaric and 3-hydroxyglutaric acids are 10- to 1000-fold higher in brain than in plasma (Funk et al 2005; Goodman et al 1977; Külkens et al 2005; Leibel et al 1980; Sauer et al 2006), reflecting the limited efflux capacity of the BBB for dicarboxylic acids. In addition, in two patients receiving lysine-restricted dietary treatment and lysine-free amino acid supplementation, the cerebral concentrations of glutaric and 3-hydroxyglutaric acids were almost normalized (Bennett et al 1986; Kölker et al 2003). Recently, a cross-sectional study on 279 patients with GA I demonstrated that oral lysine restriction (plus administration of lysine-free amino acid supplements), in combination with carnitine supplementation, and emergency treatment had a beneficial effect on the prevention of acute striatal injury in pre-symptomatically diagnosed children (Kölker et al 2006b). This has been confirmed by a prospective study including 38 children identified by newborn screening in Germany demonstrating that 89% of these children remained asymptomatic on this treatment (Kölker et al 2007).
Since pathophysiological and clinical studies have suggested that lysine influx into the brain via system y+ at the BBB and accumulation of toxic dicarboxylic acids in the brain, which are trapped owing to limited permeability of the BBB, contribute to the pathomechanism underlying neurological disease in GA I, optimization of treatment has to consider a balanced reduction of cerebral lysine influx across the BBB by dietary lysine restriction (Kölker et al 2006b, 2007) or supplementation with arginine (competing with lysine for transporter y+) or by trans-stimulation of organic acid transporters (e.g. OAT3; Sauer et al 2006) to stimulate the efflux of dicarboxylic acids.
Succinic semialdehyde dehydrogenase deficiency
Succinic semialdehyde dehydrogenase (SSADH; EC 1.2.1.16) deficiency (OMIM #271980), first described by Jakobs and co-workers (1981), is an autosomal recessively inherited neurometabolic disorder of GABA metabolism resulting in accumulation of succinic semialdehyde and, secondarily, γ-hydroxybutyric acid (GHB), 4,5-dihydroxyhexanoic acid and GABA. The CSF concentrations of GHB are massively elevated (up to 230-fold of controls), and GABA concentrations show a 3-fold increase (Gibson et al 2003). The molecular basis of this disease relies on the SSADH (ALDH5A1) gene localized on chromosome 6p22. Language and motor delay, muscular hypotonia and hyporeflexia, mental retardation, ataxia, behaviour problems and epilepsy (absence, myoclonic epilepsy or generalized tonic-clonic seizures) are frequently found in these patients. Symptoms outside of the central nervous system have not been reported. Neuroimaging reveals cerebral and cerebellar atrophy, and signal changes in the globus pallidus, subcortical white matter, the dentate nucleus and the brainstem (Pearl et al 2003).
Major pathomechanisms involved in this disease were elucidated by studying Aldh5a1 −/− mice, a transgenic mouse model for SSADH deficiency generated by Hogema and co-workers (Hogema et al 2001), and by clinical experience with increasing illicit use of GHB as a recreational club drug (‘liquid XTC’) or for drug-facilitated sexual assault (‘date rape’) because of its rapid sedative effect (Drasbek et al 2006; Snead and Gibson 2005). Recent pathophysiological concepts have highlighted that neurological disease is induced by cerebral increase of GHB and GABA (reviewed by Knerr et al 2007). At physiologically low concentrations, GHB primarily acts via GHB receptors, which are presynaptically located G-protein-coupled receptors. GABAB receptors are the major target at high pharmacological GHB concentrations (Lingenhoehl etal 1999). GHB-induced stimulation of GABAB receptors activates various pre- and postsynaptic mechanisms, inducing alterations in the release of dopamine, GABA and glutamate (Berton et al 1999). Changes in the expression of age-dependent AMPA receptor subunits during brain development in Aldh5a1 −/− mice have been described (Wu et al 2004). In addition, GHB inhibits the mitogen-activated protein kinase (MAPK) pathway, which may have numerous consequences including long-term neuroadaptive changes (Ren and Mody 2003) and impaired myelination (Donarum et al 2006).
Chronic increases in GABA, the major inhibitory neurotransmitter in the CNS, primarily involves signalling via GABAA receptors. Prolonged occupancy of GABAA receptors results in use-dependent downregulation of this receptor. Recently, it was shown in Aldh5a1 −/− mice that progressive downregulation of GABAA receptor subunit β2 from postnatal day 7 to day 19 was paralleled by progressive GABAA receptor dysfunction, hyperexcitability of neurons and, as a consequence, the manifestation of seizures (Wu et al 2006). These observations may explain why the irreversible GABA transaminase inhibitor vigabatrin, which is most widely used for treatment of SSADH deficiency and rescues Aldh5a1 −/− mice from lethal seizures (Gibson et al 1989; Hogema et al 2001), is inconsistent in treatment of seizures associated with SSADH deficiency. This drug decreases the cerebral concentrations of GHB but exacerbates hyperGABAergic status (Gropman 2003). In addition, GABA elevations may also affect myelination via GABAA and GABAB receptors involving the MAPK pathway and the production of neurosteroids such as progesterone and allopregnanolone (Gupta et al 2003; Donarum et al 2006).
These studies may have consequences for optimization of treatment involving drugs or dietary strategies that specifically inhibit or modulate GHB and GABAB receptors without exacerbating the hyperGABAergic state (reviewed by Knerr et al 2007).
Aspartoacylase deficiency (Canavan–van Bogaert–Bertrand disease)
Canavan–van Bogaert–Bertrand disease (CD; OMIM #271900; Canavan 1931; Van Bogaert and Bertrand 1949) is a rare autosomal recessive cerebral OAD caused by disease-causing mutations in the ASPA gene localized on chromosome 17pter-p13. Aspartoacylase (EC 3.5.1.15) is localized in oligodendrocytes (Baslow et al 1999) and catalyses the hydrolysis of N-acetyl-l-aspartate (NAA) to form aspartate and acetate (Matalon et al 1988). NAA is synthesized primarily in neurons and its production is directly coupled to glucose metabolism, i.e. 1 mol NAA is produced for every 40 mol glucose or glucose equivalent oxidized (Moreno et al 2001). The neuronal NAA concentration is up to 20 mmol/L, representing about 7% of neuron osmolarity and 3–4% of total brain osmolarity (Baslow 2000a). Biochemically, aspartoacylase deficiency results in significant increase of cerebral NAA concentrations.
Clinically, CD mostly manifests at age 2–4 months with delayed development. Muscular hypotonia with prominent head lag, epilepsy, loss of previously acquired skills and progressive megalencephaly are regularly found. Seizures and optic nerve atrophy develop during the second year of life. As the diseaseprogresses, affected children develop pyramidal signs, and finally decerebration (Matalon et al 1988). CD demonstrates bilateral symmetric T2-weighted white-matter hyperintensity, including involvement of the subcortical arcuate fibres. This disease appears diffusely throughout the cerebral white matter, and demonstrates variable involvement of the basal ganglia and cerebellar white matter (McAdams et al 1990). Histology demonstrates spongiform degeneration, in particular of the cortex and subcortical white matter, with less involvement in the cerebellum and brainstem which is caused by excessive fluid accumulation within oligodendrocyte myelin lamellae, in swollen astrocytes and in extracellular fluid vacuoles (Matalon et al 1988). Electron microscopy reveals swollen astrocytes and distorted mitochondria (Adornato et al 1972).
The pathophysiology of CD is still unclear, but a recent hypothesis has suggested that spongiform degeneration might be induced by impaired efflux transport of neuronal metabolic water. The average utilization of glucose in cortical grey matter is approximately 37 μmol/100 g per min (De Volder et al 1997) which, following complete oxidation, results in the production of 133 μmol/g per h of metabolic water (Baslow 2002c). The metabolic water production in the brain is 12 times higher than in other tissues (Raichle et al 2001). A large proportion of the neuronal surface is separated from the extracellular space following myelination, impeding efflux of metabolic water. It has been hypothesized by Baslow (the ‘molecular water pump hypothesis’) that NAA may act as a molecular water pump between neurons and oligodendrocytes, promoting the efflux of neuronal metabolic water (Baslow 2002c). In fact, it has been estimated that NAA has a high turnover rate in brain and that 1 mol NAA transports 110–130 mol of metabolic water (Baslow 2002c). As the NAA level in the brain is constant in healthy individuals, the rate of NAA synthesis from glucose in neurons must equal the rate of NAA hydrolysis by aspartoacylase in oligodendrocytes. As a consequence of aspartoacylase deficiency resulting in disruption of the catabolic part of the NAA cycle, i.e. hydrolysis of NAA to acetate and aspartate, CD can be understood as an osmotic disease resulting in osmotic imbalance and, subsequently, spongy demyelination. In contrast, complete disruption of the NAA cycle due to impairment of NAA synthesis, as described in hypoacetylaspartic children, does not exhibit megaloencephalopathy and demyelination (Martin et al 2001). Despite these considerations, there is not yet any direct evidence that supports the notion that excess NAA in the brain causes dysmyelination through osmotic damage. Furthermore, it remains unclear why disruption of the catabolic pathway of the NAA cycle causes spongy demyelination prior to brain oedema.
A major disadvantage of this hypothesis is that to date no protein has been characterized that acts to co-transport NAA and water out of neurons. However, ithas been shown that the sodium-dependent transporter NaC3 moves extracellular NAA into glial cells (George et al 2004). Furthermore, there is strong evidence against the suggestion that NAA is involved in axon–glial signalling in analogy to the glutamate/glutamine cycle (Baslow 2000b). In fact, Miller and co-workers (1996) found no evidence that following hydrolysis of NAA the breakdown products acetate and aspartate are passed from glia back to neurons, and then are re-utilized for re-synthesis of NAA. Interestingly, recent studies have proposed that reduced supply of NAA-derived acetate is the primary aetiological mechanism in the pathogenesis of CD, resulting in reduced lipid synthesis in myelinating cells of the brain, in particular when axonal myelination is maximal during early infancy (reviewed by Moffett et al 2007). Therefore, dietary acetate supplementation therapy using glyceryl triacetate has been considered a possible treatment for Canavan disease and was recently studied in ASPA −/− mice (Madhavarao et al 2005).
In addition to the link between NAA catabolism and myelination, there is growing evidence that NAA and brain energy metabolism are directly coupled (reviewed by Clark 1998). In glial cells, unlike in neurons, acetate is preferentially utilized for energy production through the TCA cycle, suggesting that oligodendrocytes could use NAA-derived acetate for energy production, in particular after myelination is complete (Bluml et al 2002).
Furthermore, acetylation of aspartate may facilitate its removal from neuronal mitochondria, thus favouring conversion of glutamate to α-ketoglutarate which then enters the TCA cycle for energy production (Madhavarao et al 2005).
The prognosis of infantile Canavan disease is rapidly fatal, whereas milder disease courses have been described in some patients. Unfortunately, therapeutic strategies do not yet significantly influence the cause of disease. However, improved understanding of the physiological functions NAA in the brain may elucidate novel therapeutic options: Lithium chloride, decreasing abnormally elevated NAA levels in one affected individual, has recently been considered as supportive therapy but warrants further investigation (Janson et al 2005). Gene therapy using neurosurgical application of recombinant adeno-associated virus containing the recombinant aspartoacylase gene has been studied recently (Janson et al 2002; McPhee et al 2006).
Conclusions
Pathomechanisms underlying CNS involvement in inherited disorders of amino acid and organic acid metabolism are coming to be elucidated and are seemingly complex. As far as is understood, synergistic effects of accumulating putatively toxic metabolites are more likely to contribute to the manifestation of neurological disease than are single major effects. This reflects the complexity of regulatory mechanisms underlying the balance of excitatory and inhibitory transmission and the short-term coupling of brain energy metabolism to local changes in neuronal activity and energy demand. Not unexpectedly, putative pathomechanisms identified for amino acid disorders and organic acidurias interfere with some of the key mechanisms of neurometabolism, including the regulation of glutamatergic and GABAergic neurotransmission, neuroenergetics and the handling of metabolic water, regulation of influx and efflux of hydrophilic compounds from and to the brain compartment via the BBB, and the process of myelination. Although only some of these IEMs are considered as treatable and the burden of neurological complications is still high in affected individuals, it is hoped that novel or optimized therapeutic strategies derive from systematic pathophysiological studies. Such studies may stimulate a refinement of current dietary treatment strategies by systematic exploitation of the physiological function of the BBB, restoration of brain energy metabolism by implementation of anaplerotic therapies, or development of novel detoxification strategies. Enzyme replacement or gene therapy, however, are not yet available or reliably established for these disorders. Liver transplantation is an alternative approach allowing long-lasting correction of the hepatic phenotype. However, although liver transplantation is a therapeutic option for some of these IEMs, such as maple syrup urine disorder (Strauss et al 2006), it may not reliably protect against long-term complications in other IEMs, such as in methylmalonic aciduria (Leonard et al 2001).
Abbreviations
- CD:
-
Canavan–van Bogaert–Bertrand disease
- CNS:
-
central nervous system
- GA I:
-
glutaric aciduria type I
- IEM:
-
inborn error of metabolism
- LNAA:
-
large neutral amino acid
- NAA:
-
N-acetyl-l-aspartate
- OAD:
-
organic aciduria
- PKU:
-
phenylketonuria
- SSADH:
-
succinic semialdehyde dehydrogenase
- TCA cycle:
-
tricarboxylic acid cycle
References
Adornato BT, O’Brien JS, Lampert PW, Roe TF, Neustein HB (1972) Cerebral spongy degeneration of infancy: a biochemical and ultrastructural study of affected twins. Neurology 22: 202–210.
Aiello LC, Wheeler P (1995) The expensive tissue hypothesis: the brain and digestive system in human and primate evolution. Curr Anthropol 36: 199–221.
Baslow MH (2000a) Canavan’s spongiform leukodystrophy: a clinical anatomy of a genetic metabolic CNS disease. J Mol Neurosci 15: 61–69.
Baslow MH (2000b) Functions of N-acetyl-l-aspartate and N-acetyl-l-aspartylglutamate in the vertebrate brain: role in glial cell-specific sigaling. J Neurochem 75: 453–459.
Baslow MH (2002c) Evidence supporting a role for N-acetyl-l-aspartate as a molecular water pump in myelinated neurons in the central nervous system. An analytic review. Neurochem Int 40: 295–300.
Baslow MH, Suckow R, Sapirstein V, Hungrund BL (1999) Expression of aspartoacylase activity in cultured rat macroglial cells is limited to oligodendrocytes. J Mol Neurosci 13: 47–53.
Bennett MJ, Marlow N, Pollitt RJ, Wales JK (1986) Glutaric aciduria type 1: biochemical investigations and post mortem findings. Eur J Pediatr 145: 403–405.
Berton F, Brancucci A, Beghe F, et al (1999) Gamma-hydroxybutyrate inhibits excitatory postsynaptic potentials in rat hippocampal slices. Eur J Pharmacol 380: 109–116.
Bick U, Fahrendorf G, Ludolph AC, Vassallo P, Weglage J, Ullrich K (1991) Disturbed myelination in patients with untreated hyperphenylalaninemia: evaluation with magnetic resonance imaging. Eur J Pediatr 150: 185–189.
Bickel H, Gerrard J, Hickmans EM (1953) Influence of phenylalanine intake on phenylketonuria. Lancet 265: 812–813.
Bluml S, Moreno-Torres A, Shic F, Nguy CH, Ross BD (2002) Tricarboxylic acid cycle of glia in the in vivo human brain. NMR Biomed 15: 1–5.
Bouzier-Sore AK, Voisin P, Canioni P, Magistretti P, Pellerin L (2003) Lactate is a preferential oxidative energy substrate over glucose for neurons in culture. J Cereb Blood Flow Metab 23: 1298–1306.
Burnett JR (2007) Sapropterin dihydrochloride (Kuvan/phenoptin), an orally active synthetic form of BH4 for the treatment of phenylketonuria. IDrugs 10: 805–813.
Canavan MM (1931) Schilder’s encephalitis perioxialis diffusa. Neurology 15: 299–308.
Clark JB (1998) N-Acetyl aspartate: a marker for neuronal loss or mitochondrial dysfunction. Dev Neurosci 20: 271–276.
Collingridge GL, Kehl SJ, McLennan H (1983) Excitatory amino acids in synaptic transmission in the Schaffer collateral-commissural pathway of the rat hippocampus. J Physiol 334: 33–46.
De Volder AG, Bol A, Blin J, et al (1997) Brain energy metabolism in early blind subjects: neural activity in the visual cortex. Brain Res 750: 235–244.
Donarum EA, Stephan DA, Larkin K, et al (2006) Expression profiling reveals multiple myelin alterations in murine succinate semialdehyde dehydrogenase deficiency. J Inherit Metab Dis 29: 143–156.
Drasbek KR, Christensen J, Jensen K (2006) Gamma-hydroxybutyrate – a drug of abuse. Acta Neurol Scand 114: 145–156.
Dyer CA, Kendler A, Philibotte T, et al (1996) Evidence for central nervous system glial cell plasticity in phenylketonuria. J Neuropath Exp Neurol 55: 795–814.
Erecinska M, Dagani F (1990) Relationships between the neuronal sodium/potassium pump and energy metabolism. Effects of K+, Na+, and adenosine triphosphate in isolated brain synaptosomes. J Gen Physiol 95: 591–616.
Erwald RC, van Keuren-Jensen KR, Aizenman CD, Cline HT (2008) Roles of NR2A and NR2B in the development of dendritic arbor morphology in vivo. J Neurosci 28: 850–861.
Fiege B, Blau N (2007) Assessment of tetrahydrobiopterin (BH4) responsiveness in phenylketonuria. J Pediatr 15: 627–630.
Følling A (1934) Über Ausscheidung von Phenylbrenztraubensäure in den Harn als Stoffwechselanomalie in Verbindung mit Imbezillität. Z Physiol Chem 227: 169–176.
Fox K, Daw N, Sato H, Czepita D (1991) Dark-rearing delays the loss of NMDA-receptor function in kitten visual cortex. Nature 350: 342–344.
Funk CB, Prasad AN, Frosk P, et al (2005) Neuropathological, biochemical, and molecular findings in a glutaric acidemia type I cohort. Brain 128: 711–722.
Galdikas BMF, Wood JW (1990) Birth sparing patterns in humans and apes. Am J Phys Anthropol 83: 185–191.
George RL, Huang W, Naggar HA, Smith SB, Ganapathy V (2004) Transport of N-acetylasparate via murine sodium/dicarboxylate cotransporter NaDC3 and expression of this transporter and aspartoacylase II in ocular tissues in mouse. Biochim Biophys Acta 1690: 63–69.
Gerstner B, Gratopp A, Marcinkowski M, Sifringer M, Obladen M, Bührer C (2005) Glutaric acid and its metabolites cause apoptosis in immature oligodendrocytes: a novel mechanism of white matter degeneration in glutaryl-CoA dehydrogenase deficiency. Pediatr Res 57: 771–776.
Gibson KM, DeVivo DC, Jakobs C (1989) Vigabatrin therapy in patient with succinic semialdehyde dehydrogenase deficiency. Lancet 8671: 1105–1106.
Gibson KM, Gupta M, Pearl PL, et al (2003) Significant behavioural disturbances in succinic semialdehyde dehydrogense (SSADH) deficiency (gamma-hydroxybutyric aciduria). Biol Psychiatry 54: 763–768.
Glushakov AV, Dennis DM, Sumners C, Seubert CN, Martynyuk AE (2003) l-Phenylalanine selectively depresses currents atglutamatergic excitatory synapses. J Neurosci Res 72: 116–124.
Glushakov AV, Glushakova O, Varshney M, et al (2005) Long-term changes in glutamatergic synaptic transmission in phenylketonuria. Brain 128: 300–307.
Goodman SI, Norenberg MD, Shikes RH, Breslich DJ, Moe PG (1977) Glutaric aciduria: biochemical and morphological considerations. J Pediatr 90: 746–750.
Gropman A (2003) Vigabatrin and newer interventions in succinic semialdehyde dehydrogenase (SSADH) deficiency (4-hydroxybutyric aciduria, gamma-hydroxybutyric aciduria). Eur J Paediatr Neurol 8: 261–265.
Gupta M, Hogema BM, Grompe M, et al (2003) Murine succinate semialdehyde dehydrogenase deficiency. Ann Neurol 54(Supplement 6): S81–90.
Guthrie R, Susi A (1963) A simple phenylalanine method for detecting phenylketonuria in large populations of newborn infants. Pediatrics 32: 338–343.
Hassel B, Brathe A, Petersen D (2002) Cerebral dicarboxylate transport and metabolism studied with isotopically labelled fumarate, malate and malonate. J Neurochem 82: 410–419.
Hasselbalch S, Knudsen GM, Toft PB, et al (1996) Cerebral glucose metabolism is decreased in white matter changes in patients with phenylketonuria. Pediatr Res 40: 21–24.
Heidenreich R, Natowicz M, Hainline BE, et al (1988) Acute extrapyramidal syndrome in methylmalonic acidemia: ‘Metabolic’ stroke involving the globus pallidus. J Pediatr 113: 1022–1027.
Hofman MA (1983) Evolution of brain size in neonatal and adult placental mammals: a theoretical approach. J Theoret Biol 105: 317–322.
Hoffmann GF, Athanassopoulos S, Burlina AB, et al (1996) Clinical course, early diagnosis, treatment, and prevention of disease in glutaryl-CoA dehydrogenase deficiency. Neuropediatrics 27: 115–123.
Hogema BM, Gupta M, Senephansiri H, et al (2001) Pharmacologic rescue of lethal seizures in mice deficient in succinate semialdehyde dehydrogenase deficiency. Nat Genet 29: 212–216.
Hörster F, Schwab MA, Sauer SW, et al (2006) Phenylalanine reduces synaptic density in mixed cortical cultures from mice. Pediatr Res 59: 544–548.
Huttenlocher PR (2000) The neuropathology of phenylketonuria: human and animal studies. Eur J Pediatr 159: S102–S106.
Ikonomidou C, Bosch F, Miksa M, et al (1999) Blockade of NMDA receptors and apoptotic neurodegeneration in the developing brain. Science 283: 70–74.
Jakobs C, Bojasch M, Mönch E, Rating D, Siemes H, Hanefeld F (1981) Urinary excretion of gamma-hydroxybutyric acid in a patient with neurological abnormalities. The probability of a new inborn error of metabolism. Clin Chim Acta 111: 169–178.
Janson C, McPhee S, Bilaniuk L, et al (2002) Clinical protocol. Gene therapy of Canavan disease: AAV-2 vector for neurosurgical delivery of aspartoacylase gene (ASPA) to the human brain. Hum Gene Ther 13: 1391–1412.
Janson CG, Assadi M, Francis J, Bilaniuk L, Shera D, Leone P (2005) Lithium citrate for Canavan disease. Pediatr Neurol 33: 235–244.
Knerr I, Pearl PL, Bottiglieri T, Snead OC, Jakobs C, Gibson KM (2007) Therapeutic concepts in succinate semialdehyde dehydrogenase (SSADH; ALDH5a1) deficiency (γ-hydroxybutyric aciduria). Hypotheses evolved from 25 years of patient evaluation, studies in Aldh5a1 −/− mice and characterization of γ-hydroxybutyric acid pharmacology. J Inherit Metab Dis 30: 279–294.
Koeller DM, Woontner M, Crnic LS, et al (2002) Biochemical, pathological and behavorial analysis of a mouse model of glutaric acidemia type I. Hum Mol Genet 11: 347–357.
Kölker S, Hoffmann GF, Schor DS, et al (2003) Glutaryl-CoA dehydrogenase deficiency: regional-specific analysis of organic acids and acylcarnitines in post mortem brain predicts vulnerability of the putamen. Neuropediatrics 34: 253–260.
Kölker S, Koeller DM, Okun JG, Hoffmann GF (2004) Pathomechanisms of neurodegeneration in glutaryl-CoA dehydrogenase deficiency. Ann Neurol 55: 7–12.
Kölker S, Sauer SW, Surtees RA, Leonard JV (2006a) The aetiology of neurological complications of organic acidemias – a role for the blood–brain barrier. J Inherit Metab Dis 29: 701–704.
Kölker S, Garbade SF, Greenberg CR, et al (2006b) Natural history, outcome, and treatment efficacy in children and adults with glutaryl-CoA dehydrogenase deficiency. Pediatr Res 59: 840–847.
Kölker S, Garbade SF, Boy N, et al (2007) Decline of acute encephalopathic crises in children with glutaryl-CoA dehydrogenase deficiency identified by neonatal screening in Germany. Pediatr Res 62: 357–362.
Külkens S, Harting, Sauer S, et al (2005) Late-onset neurologic disease in glutaryl-CoA dehydrogenase deficiency. Neurology 64: 2142–2144.
Leibel RL, Shih VE, Goodman SI, et al (1980) Glutaric aciduria type I: a metabolic disorder causing progressive choreoathetosis. Neurology 30: 1163–1168.
Leonard JV, Walter JH, McKiernan PJ (2001) The management of organic acidaemias: the role of transplantation. J Inherit Metab Dis 24: 309–311.
Leonard WR, Robertson ML (1992) Nutritional requirements and human evolution: a bioenergetics model. Am J Hum Biol 4: 179–195.
Lingenhoehl K, Brom R, Heid J, et al (1999) Gamma-hydroxybutyrate is a weak agonist at recombinant GABA(B) receptors. Neuropharmacology 38: 1667–1673.
Madhavarao CN, Arun P, Moffett JR, et al (2005) Defective N-acetylaspartate catabolism reduces brain acetate levels and myelin lipid synthesis in Canavan’s disease. Proc Natl Acad Sci U S A 102: 5221–5226.
Magistretti PJ, Pellerin L, Rothman DL, Shulman RG (1999) Energy on demand. Science 283: 496–497.
Martin E, Capone A, Schneider J, Hennig J, Thiel T (2001) Absence of N-acetylaspartate in the human brain: impact on neurospectroscopy. Ann Neurol 49: 518–521.
Matalon R, Michals K, Sebesta D, Deanching M, Gashkoff P, Casanova J (1988) Aspartoacylase deficiency and N-acetylaspartic aciduria in patients with Canavan disease. Am J Med Genet 29: 463–471.
Matalon R, Surendran S, Michals Matalon K, et al (2003) Future role of large neutral amino acids in transport of phenylalanine into the brain. Pediatrics 112: 1570–1574.
McAdams HP, Geyer CA, Done SL, Deigh D, Mitchell M, Ghaed VN (1990) CT and MR imaging of Canavan disease. Am J Neuroradiol 11: 397–399.
McKean CM (1972) The effects of high phenylalanine concentrations on serotonin and catecholamine metabolism in the human brain. Brain Res 47: 469–476.
McPhee SW, Janson CG, Li C, et al (2006) Immune responses to AAV in a phase I study for Canavan disease. J Gene Med 8: 577–588.
Meador KJ (2007) The basic science of memory as it applies to epilepsy. Epilepsia 48(Supplement 9): 23–25.
Miller SL, Daikhin Y, Yudkoff M (1996) Metabolism of N-acetyl-l-aspartate in rat brain. Neurochem Res 21: 615–618.
Moffett JR, Ross B, Arun P, Madhavarao CN, Namboodiri AA (2007) N-Acetylaspartate in the CNS: from neurodiagnostics to neurobiology. Prog Neurobiol 81: 89–131.
Möller HE, Weglage J, Wiedermann D, Ullrich K (1998) Blood-brain barrier phenylalanine transport and individual vulnerability in phenylketonuria. J Cereb Blood Flow Metab 18: 1184–1191.
Moreno A, Ross BD, Bluml S (2001) Direct determination of the N-acetyl-l-aspartate synthesis rate in the human brain by 13C MRS and [1-13C]glucose infusion. J Neurochem 77: 347–350.
Mühlhausen C, Ott N, Chalajour F, et al (2006) Endothelial effects of 3-hydroxyglutaric acid: implications for glutaric aciduria type I. Pediatr Res 59: 196–202.
Muntau AC, Röschinger W, Habich M, et al (2002) Tetrahydrobiopterin as an alternative treatment for mild phenylketonuria. N Engl J Med 347: 2122–2132.
Nikolaides P, Leonard J, Surtees R (1998) Neurological outcome of methylmalonic acidemia. Arch Dis Child 78: 508–512.
Okun JG, Hörster F, Farkas LM, et al (2002) Neurodegeneration in methylmalonic aciduria involves inhibition of complex II and the tricarboxylic acid cycle, and synergistically acting excitotoxicity. J Biol Chem 277: 14674–14680.
Paine RS (1957) The variability in manifestations of untreated patients with phenylketonuria (phenylpyruvic aciduria). Pediatrics 20: 290–302.
Pardridge WM (1998) Blood-brain barrier carrier-mediated transport and brain metabolism of amino acids. Neurochem Res 23: 635–644.
Pawlak V, Schupp BJ, Single FN, Seeburg PH, Köhr G (2005) Impaired synaptic scaling in mouse hippocampal neurones expressing NMDA receptors with reduced calcium permeability. J Physiol 562: 771–783.
Pearl PL, Gibson KM, Acosta MT, et al (2003) Clinical spectrum of succinic semialdehyde dehydrogenase deficiency. Neurology 60: 1413–1417.
Persidsky Y, Ramirez SH, Haorah J, Kanmogne GD (2006) Blood-brain barrier: structural components and function under physiologic and pathophysiologic conditions. J Neuroimmune Pharmacol 1: 223–236.
Pietz J, Kreis R, Rupp A, et al (1999) Large neutral amino acids block phenylalanine transport into brain tissue in patients with phenylketonuria. J Clin Invest 103: 1169–1178.
Porciuncula LO, Dal-Pizzol A Jr, Coitinho AS, Emanuelli T, Souza DO, Wajner M (2000) Inhibition of synaptosomal [3H]glutamate uptake and [3H]glutamate binding to plasma membranes from brain of young rats by glutaric acid in vitro. J Neurol Sci 73: 93–96.
Quin M, Smith CB (2007) Regionally selective decreases in cerebral glucose metabolism in a mouse model of phenylketonuria. J Inherit Metab Dis 30: 318–325.
Raichle ME, MacLeod AM, Snyder AZ, Powers WJ, Gusnard DA, Shulman GL (2001) A default mode in brain function. Proc Natl Acad Sci U S A 98: 676–682.
Ren X, Mody I (2003) Gamma-hydroxybutyrate reduces mitogen-activated protein kinase phosphorylation via GABA B receptor activation in mouse frontal cortex and hippocampus. J Biol Chem 278: 42006–42011.
Rowland LM, Astur RS, Jung RE, et al (2005) Selective cognitive impairments associated with NMDA receptor blockade in humans. Neuropsychopharmacology 30: 633–639.
Roy CS, Sherrington CS (1890) On the regulation of the blood supply of the brain. J Physiol (London) 11: 85–108.
Sauer SW, Okun, Schwab MA, et al (2005) Bioenergetics in glutaryl-coenzyme A dehydrogenase deficiency, a role for glutaryl-coenzyme A. J Biol Chem 280: 21830–21836.
Sauer SW, Okun JG, Fricker G, et al. (2006) Intracerebral accumulation of glutaric and 3-hydroxyglutaric acids secondary to limited flux across the blood–brain barrier constitute a biochemical risk factor for neurodegeneration in glutaryl-CoA dehydrogenase deficiency. J Neurochem 97: 899–910.
Schousboe A, Westergaard N, Sonnewald U, et al (1993) Glutamate and glutamine metabolism and compartmentation in astrocytes. Dev Neurosci 15: 359–366.
Schousboe A, Westergaard N, Waagepetersen HS, Larsson OM, Barken IJ, Sonnewald U (1997) Trafficking between glia and neurons of TCA cycle intermediates and related metabolites. Glia 21: 99–105.
Schwab MA, Sauer SW, Okun JG, et al (2006) Secondary mitochondrial dysfunction in propionic aciduria: a pathogenic role for endogenous mitochondrial toxins. Biochem J 398: 107–112.
Shefer S, Tint GS, Jean-Guillaume D, et al (2000) Is there a relationship between 3-hydroxy-3-methylglutaryl coenzyme A reductase activity and forebrain pathology in the PKU mouse? J Neurosci Res 61: 549–563.
Sherwood CC, Stimpson CD, Raghanti MA, et al (2006) From the cover: evolution of increased glia-neuron ratios in the human frontal cortex. Proc Natl Acad Sci USA 103: 13606–13611.
Smith CB, Deibler GE, Eng N, Schmidt K, Sokoloff L (1988) Measurement of local cerebral protein synthesis in vivo: influence of amino acids derived from protein degradation. Proc Natl Acad Sci U S A 85: 9341–9345.
Snead OC, Gibson KM (2005) γ-Hydroxybutyric acid. N Engl J Med 352: 2721–2732.
Sokoloff L (1960) The metabolism of the central nervous system in vivo. In: Field J, Magoun HW, Hall VE, eds. Handbook of Physiology, Sect 1, Vol II. New York: Raven Press, 161–168.
Sokoloff L (1991) Measurement of local cerebral glucose utilization and its relation to local functional activity in the brain. Adv Exp Med Biol 291: 21–42.
Stellmer F, Keyser B, Burckardt BC, et al (2007) 3-Hydroxyglutaric acid is transported via the sodium-dependent dicarboxylate transporter NaDC3. J Mol Med 85: 763–770.
Stokke O, Goodman SI, Moe PG (1976) Inhibiton of brain glutamate decarboxylase by glutarate, glutaconate, and beta-hydroxyglutarate: explanation of the symptoms in glutaric aciduria? Clin Chim Acta 66: 411–415.
Strauss KA, Puffenberger EG, Robinson DL, Morton DH (2003) Type I glutaric aciduria, part 1: natural history of 77 patients. Am J Med Genet C Semin Med Genet 121: 38–52.
Strauss KA, Mazariegos GV, Sindhi R, et al (2006) Elective liver transplantation of classical maple syrup urine disease. Am J Transplant 6: 557–564.
Strauss KA, Lazovic J, Wintermark M, Morton DH (2007) Multimodal imaging of striatal degeneration in Amish patients with glutaryl-CoA dehydrogenase deficiency. Brain 130: 1905–1920.
Surtees RA, Matthews EE, Leonard JV (1992) Neurologic outcome of propionic acidemia. Pediatr Neurol 8: 333–337.
Thompson AJ, Tillotson S, Smith I, Kendall B, Moore SG, Brenton DP (1993) Brain MRI changes in phenylketonuria. Associations with the dietary status. Brain 116: 811–821.
Trefz FK, Cipcic-Schmidt K, Koch R (2000) Final intelligence in late treated patients with phenylketonuria. Eur J Pediatr 159(Supplement 2): S145–S148.
Trefz FK, Scheible D, Frauendienst-Egger G, Korall H, Blau N (2005) Long-term treatment of patients with mild and classical phenylketonuria by tetrahydrobiopterin. Mol Genet Metab 86(Supplement 1): S75–S80.
Tsukada H, Nishiyama S, Fukumoto D, Sato K, Kakiuchi T, Domino EF (2005) Chronic NMDA antagonism impairs working memory, decreases extracellular dopamine, and increases D1 receptor binding in prefrontal cortex of conscious monkeys. Neuropsychopharmacology 30: 1861–1869.
Ullrich K, Flott-Rahmel B, Schluff P, et al (1999) Glutaric aciduria type I: pathomechanisms of neurodegeneration. J Inherit Metab Dis 22: 392–403.
Van Bogaert L, Bertrand I (1949) Sur une idiotie familiale avec degerescence sponglieuse de neuraxe (note preliminaire). Acta Neurol 49: 572–587.
Weber G (1969) Inhibition of human brain pyruvate kinase and hexokinase by phenylalanine and phenylpyruvate: possible relevance to phenylketonuric brain damage. Proc Natl Acad Sci U S A 63: 1365–1369.
Weglage J, Wiedermann D, Denecke J, et al (2002) Individual blood brain–barrier phenylalanine transport in siblings with classical phenylketonuria. J Inherit Metab Dis 25: 431–436.
Wu Y, Buzzi A, Shen L, et al (2004) Differential expression of AMPA-type glutamate receptors in the brain of mice deficient for succinate semialdehyde dehydrogenase. 34th Meeting of the Society for Neuroscience, San Diego, CA. Online (http://sfn.scholarone.com/itin2004).
Wu Y, Buzzi A, Frantseva M, et al (2006) Status epilepticus in mice deficient for succinate semialdehyde dehydrogenase: GABAA receptor-mediated mechanisms. Ann Neurol 59: 42–52.
Yodoya E, Wada M, Shimada A, et al (2006) Functional and molecular identification of sodium-coupled dicarboxylate transporters in rat primary rat cultured cerebrocortical astrocytes and neurons. J Neurochem 97: 162–173.
Zinnanti WJ, Lazovic J, Wolpert EB, et al (2006) A diet-induced mouse model for glutaric aciduria type I. Brain 129: 899–910.
Zinnanti WJ, Lazovic J, Housman C, et al (2007) Mechanism of age-dependent susceptibility and novel treatment strategies in glutaric acidemia type I. J Clin Invest 117: 3258–3270.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicating editor: Michael Gibson
Competing interests: None declared
References to electronic databases: Phenylketonuria: OMIM #261600. Glutaric aciduria type I: OMIM #231670. Succinic semialdehyde dehydrogenase deficiency: OMIM #271980. Aspartoacylase disease (Canavan–van Bogaert–Bertrand disease): OMIM #271900. Phenylalanine hydroxylase: EC 1.14.16.1. Glutaryl-CoA dehydrogenase: EC 1.3.99.7. Succinic semialdehyde dehydrogenase: EC 1.2.1.16. Aspartoacylase: EC 3.5.1.15.
Rights and permissions
About this article
Cite this article
Kölker, S., Sauer, S.W., Hoffmann, G.F. et al. Pathogenesis of CNS involvement in disorders of amino and organic acid metabolism. J Inherit Metab Dis 31, 194–204 (2008). https://doi.org/10.1007/s10545-008-0823-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10545-008-0823-z