Abstract
Cervical degenerative disease is a common and frequently occurring disease, which seriously affects the health and quality of the life of patients worldwide. Anterior cervical decompression and interbody fusion is currently recognized as the gold standard for the treatment of degenerative cervical spondylosis. Polyetheretherketone (PEEK) has become the prevailing material for cervical fusion surgery. Although PEEK has excellent biocompatibility, it is difficult to form bone connection at its bone-implant interface due to its low surface hydrophilicity and conductivity. It is widely accepted that Ti has excellent osteogenic activity and biocompatibility. In this study, a Ti-PEEK composite cage was prepared by coating Ti on the surface of a PEEK cage using a vacuum plasma spraying technique to enhance the osteogenic property of PEEK. The Ti-PEEK samples were evaluated in terms of their in vitro cellular behaviors and in vivo osteointegration, and the results were compared to a pure PEEK substrate. The skeleton staining and MTS assay indicated that the MC3T3-E1 cells spread and grew well on the surface of Ti-PEEK cages. The osteogenic gene expression and western blot analysis of osteogenic protein showed upregulated bone-forming activity of MC3T3-E1 cells in Ti-PEEK cages. Furthermore, a significant increase in new bone formation was demonstrated on Ti-PEEK implants in comparison with PEEK implants at 12 weeks in a sheep cervical spine fusion test. These results proved that the Ti-PEEK cage exhibited enhanced osseointegrative properties compared to the PEEK cage both in vitro and in vivo.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Cervical degenerative diseases are common, including cervical spondylosis and cervical spinal stenosis, which seriously affects the health and quality of life of patients worldwide (Schoenfeld et al. (2000). According to literature, the incidence of cervical spondylotic myelopathy–related hospitalizations has been estimated at 4.04/100,000 people a year in North America (Nouri et al. 2015). Another report showed an increase of more than 28% in spinal interventions from 288,178 to 369,339 cases per year between 2007 and 2010 in Germany alone (Wiedenhöfer et al. 2017). According to a study by Hansson, the total annual costs for back and neck problems are approximately 1% of the gross national product (Hansson and Hansson 2005). Therefore, research on the prevention and treatment of cervical degenerative diseases are of vital importance to reduce personal and social burdens.
Anterior cervical decompression and interbody fusion (ACDF) with trilateral cortical iliac bone is recognized as the gold standard for the treatment of degenerative cervical disease (Buttermann 2018). However, graft resorption, collapse, loosening, displacement and other complications may occur that result in failure of fusion or pseudoarthrosis. In addition, autologous iliac bone extraction can increase blood loss, hematoma, and pain at the donor site (Korovessis et al. 2013; Ha et al. 2007). In recent years, various kinds of cervical intervertebral fusion cages have been developed including stainless cages (Kuslich et al. 1998), carbon fiber cages (Hermansen et al. 2011), and degradable polylactides (Dijk et al. 2002). Among available cages, polyetheretherketone (PEEK) has been widely applied in clinical trials because of its similar elastic modulus to that of cortical bone and its relatively stable chemical properties in vivo (Kurtz and Devine, 2007). However, its implantation in vivo may lead to fibrous tissue encapsulation, isolating the implant from surrounding bone tissue, which will affect the bone contact between the vertebral endplate and fusion cage, leading to the failure of direct bone apposition due to its relatively low biocompatibility (Walsh et al. 2015; Devine et al. 2013). In addition, there is a risk of loosening or even detachment in the long-term (Yang et al. 2011; Toth et al. 2006).
The surface properties of the implant material are regarded as key factors for rapid and stable bone tissue integration. Some studies have shown that the application of different surface topography or coatings with metal substrates could improve the biological implant fixation (Wennerberg and Albrektsson, 2009; Bertollo et al. 2012). Therefore, there has been research for a process and method for enhancing the attachment of bone to the surface of the PEEK cage. Bioceramics, such as hydroxyapatite (HA), are a representative coating material for enhancing the biocompatibility of polymeric implants. HA coatings have improved osseointegration between the implant and bone, and have already been used in clinical application (Bodén et al. 2006). However, the coating could lead to degradation and fatigue-induced failure under tensile loading because of the low bonding strength and rapid dissolution of the HA coating (Tan et al. 2012), which has limited the clinical applications. Titanium (Ti) is a widely used material for orthopedic and dental applications owing to its excellent mechanical properties, biocompatibility and chemical stability (Duraccio et al. 2015). Several physical and chemical surface treatments have already been proposed to improve reliable osseointegration of titanium implants to enhance clinical performances. For example, Toth (Toth et al. 2006) demonstrated that in vivo studies, direct contact between PEEK implants and bone was less than that with titanium cages. Shin (Shin et al. 2019) produced nanopattern Ti surfaces by electrochemical nanopattern formation (ENF) and found that human mesenchymal stem cells on the surfaces exhibit enhanced osteogenic differentiation compared to ordered TiO2 nanotubular and compact TiO2 surfaces. Therefore, a potential solution is to add a hydrophilic, rough and microporous layer of titanium onto the surface of a PEEK matrix for enhancing the bioactivity and osseointegration of the implant.
In this study, we created a composite Ti-PEEK material for ACDF surgery with a pure titanium coating on a PEEK substrate using vacuum plasma spraying technology. The physical properties of the Ti coating layer were evaluated in terms of the characterization of the topography, microstructure and mechanical performances. The effects of the Ti coating layer on the osteoblastic properties of PEEK were assessed through in vitro and in vivo tests. More specifically, the in vitro cellular responses of the Ti-PEEK samples were evaluated in terms of the cell attachment, proliferation, and osteoblastic differentiation. The in vivo bone conductivity was examined by measuring the BV/TV ratio using a sheep cervical spine fusion model for a period of 12 weeks. We hypothesized that the application of the titanium layer to the PEEK cage with vacuum plasma-sprayed technology could encourage early bony fixation and the Ti-PEEK cage could be used in cervical ACDF surgery.
2 Materials and methods
2.1 The fabrication and characterization of Ti-PEEK
The manufacturing process of the HeniaPoreTM-K pure Titanium coating is based on two distinct steps: surface preparation and the effective micro porous titanium plasma spraying process. The surface preparation is subdivided in two phases. The first one consists of grit blasting of corundum (Al2O3) to the PEEK surface to increase the surface roughness. The second phase uses a proprietary process of plasma surface activation on the PEEK substrate after grit blasting. The aim of this process is to create the conditions for strong adhesion of the titanium VPS coating. Finally, the second step of the manufacturing process is the effective deposition of a micro porous titanium VPS coating on the plasma activated PEEK surface. An optical profilometer, Altisurf 500, was used to characterize the roughness of the sample. Using the software, Phenix V2, cartographies of the disc surfaces were created with 5x5 mm dimensions. An acquisition with steps of 2 microns, a speed of 400 micron/sec and a double frequency of 400/800 Hz. Roughness profiles of a 7-mm length were extracted from the diagonal of the cartographies and their parameter (Ra, Rz, etc.) were calculated with Altimap topography XT software. Ten Ti-PEEK samples were used to measure the coating thickness. Five pictures were taken for each sample (Leica DMRX at a magnification of 50:1), and the picture was divided using a superimposed grid with 20 crossing lines so that 20 measurements of the coating thickness were made at random points. The same images were also used to determine the coating porosity. The measurement method was a data-processing-assisted technique that identified the percentage of different levels of gray in the imaged titanium-coated PEEK bone–implant interface (software: Dietermann and Heuser Solution, Greifenstein-Beilstein, version 13, Masterstand 5). An evaluation of the coating porosity was performed in the field of the average coating thickness determined in each image. A static four point bend test was performed as previously reported Belouettar et al. 2009. The corresponding element was analyzed by energy disperse spectroscopy (EDS, JSM-7500F, JEOL, Japan) .
2.2 Contact angle test
The contact angle of Ti-PEEK cages and PEEK cages was measured by the deionized water bubble method using a SDC-100S contact angle tester (Dingsheng Precision Instrument Company, China). Five samples of each kind of cages were taken for the test, and the average was considered as the contact angle of the samples.
2.3 Cell proliferation test
Mouse pre-osteoblast cells (MC3T3-E1) (Cell Bank, Shanghai Institutes for Biological Sciences, CAS, Shanghai, China) were purchased and stored in liquid nitrogen before performed the cell seeding experiments. The cytotoxicity tests were performed according to the instructions of the international standard procedure (ISO 10,993). Briefly, the Ti-PEEK cages and PEEK cages were separately soaked in alpha-minimum essential medium (α-MEM) solutions (Hyclone, Novato, CA, USA) (3cm2 /mL) at 37 °C for 24 h, then the cages were collected and sterilized before the following experiments. The MC3T3-E1 cells were seeded at a density of 2,000 cells/well in a 96-well plate. After 4 h of incubation, the medium was changed to media containing 10% FBS (Gibco, Grand Island, NY, USA) and 1% penicillin–streptomycin (Gibco, USA). α-MEM medium containing 10% FBS and 1% penicillin–streptomycin with no Ti-PEEK or PEEK cages were used as a control group. The medium was refreshed every 3 days. Cell proliferation was measured by a MTS assay on day 1, 3, 5 and 7. The specific method was to remove the culture medium of each well, and to wash each well twice with the PBS solution. 200 μL of the PBS solution and 20 μL of the MTS reagent (CellTiter 96® AQueous, Promega) were then added to each well and incubated at 37 °C for 4 h. 150 μL of the supernatant was removed to another 96-well plate and the absorbance measured at 490 nm using a microplate reader (BioTek Instruments, USA).
2.4 Cell morphology
Ti-PEEK and PEEK cages were placed in a 24 well plate and MC3T3-E1 cells were seeded at a density of 5 × 103 cells per well at 37 °C in a humidified 5% CO2. The media was α-MEM with high glucose supplemented with 10% fetal bovine serum and 1% penicillin/streptomycin incubated. The cell morphology was stained by Cy3-Phalloidin for the skeleton and DAPI for the nucleus on the third day of culture with the Ti-PEEK cages and PEEK cages. Cells were rinsed with PBS twice, fixed in 4% paraformaldehyde for 15 min and permeabilized with 0.1% Triton X-100 for 5 min followed by staining with Cy3-phalloidin and DAPI for the F-actin and nuclei, respectively. After washing with PBS, the morphology of the cells from different scaffolds was visualized under a fluorescence microscope (Zeiss Axiovert 200, Carl Zeiss Inc, Thornwood, NY). At the same time, the morphology of the MC3T3-E1 cells on the Ti-PEEK cages and PEEK cages were observed by scanning electron microscope (SEM) three days after culturing. The specific method is as follows: each group of the cell-cage complex was washed twice with PBS solution, fixed with 2.5% glutaraldehyde for 30 min, and rinsed with deionized water three times. Samples were then dehydrated using gradient concentrations of ethanol from 50 to 100% for 10 min each. The dried samples were sputter coated with gold and visualized under the SEM at an accelerating voltage of 3 kV.
2.5 Osteogenic gene expression
Ti-PEEK and PEEK cages were placed in a 24 well plate and MC3T3-E1 cells were seeded at a density of 5 × 103 cells per well. After culturing for 2 weeks, reverse transcriptase-mediated quantitative polymerase chain reaction (RT-qPCR) was performed to analyze the gene expression of osteoblastic genes of collagen-I (Col-I), alkaline phosphatase (ALP), Runt-related transcription factor 2 (Runx-2) and osteocalcin (OCN). Total RNA from cells cultured on Ti-PEEK and PEEK cages after two weeks were extracted using the TRIZOL isolation system (Invitrogen). RT-qPCR was performed with a Bio-Rad CFX96TM Real-Time System using the SsoFast™ EvaGreen Supermix Kit (Bio-Rad). The primer sequences of Col-I, Runx-2, OCN and ALP and glyceraldehyde-3-phosphate dehydrogenase (GAPDH) are listed in Table 1. The relative gene expression level of Col-I, ALP, Runx-2 and OCN were analyzed using the 2−∆∆Ct method. The gene expression level was normalized to the housekeeping gene GAPDH, which acted as an internal control.
2.6 Western-blot of osteogenic protein
For Western blot analysis, MC3T3-E1 cells on the Ti-PEEK and PEEK cages after culturing for 2 weeks were lysed in ice-cold lysis buffer with protease inhibitors (Millipore). Lysates were centrifuged at 12,000 rpm for 15 min and supernatants were collected. The total protein extracts (20 mg) were fractionated by 10% sodium dodecylsulfate-polyacrylamide gel electrophoresis and then electroblotted onto nitrocellulose membranes (Millipore). The membranes were blocked in 5% bovine serum albumin and then incubated overnight at 4℃ with primary antibodies against Col-I (1:1,000), ALP (1:1,000), Runx-2 (1:1,000), OCN (1:1,000), and GAPDH (1:3,000) all purchased from Abclonal, Wuhan, China. After washing with Tris-buffered saline containing 0.1% Tween-20 three times for 10 min, horseradish peroxidase-conjugated secondary antibodies were applied at a 1:5,000 dilution. The antibody-bound complexes were detected using an enhanced chemiluminescence detection system (Millipore).
2.7 In vivo test
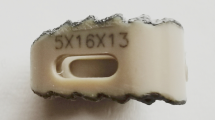
The Institutional Review Board of Wannan Medical College (Wuhu, China) approved all animal procedures. Fifteen, 2-year-old male sheep with a body weight of 28.50 ± 2.35 kg were randomly divided into three groups of five: Ti-PEEK cage, PEEK cage and three-sided cortical tibia. The cage dimensions were designed as 5*12*14 mm based on the anatomical parameters design of an adult sheep. The C3-4 intervertebral disc of the goat was prepared and a Ti-PEEK cage, PEEK cage or three-sided cortical tibia graft were implanted.
The surgical technique is as follows. Using a right anterior lateral longitudinal incision of the neck, separate the shallow and deep fascia, and expose it between the long neck muscles. Distract the intervertebral space with a Caspar opener and remove the C3-4 intervertebral disc. Scrape the cartilage endplate with a curette until the bone surface has uniform bleeding. The posterior longitudinal ligament was not removed, and the spinal canal was not exposed. The sheep were then treated with their respective group and suitable plates were fixed with two screws over the segment. The autogenous iliac bone was used as bone graft material in the operation. The area was rinsed with saline and the tissue layers sutured. The fascia and skin were reapproximated and closed using 2–0 Vicryl sutures. The animals were allowed unrestricted movement after surgery without any additional fixation. All animals recovered well after surgery with no adverse events. Penicillin, 800,000 units, was administered two times per day by intravenous drip for 3 days. Twelve weeks after the operation, potassium chloride was injected intravenously under pentobarbital sodium anesthesia for termination. The C3/C4 segments were removed and the surrounding muscle tissues were removed. The specimens were stored in 40 g/L polyformaldehyde for the next experiment.
2.8 Micro-CT analysis
After 12 weeks, micro-CT (XTH 225–320 LC, Nikon Corporation, Japan) was used to obtain high-resolution radiographic images of the implantation sites. The slice thickness was set to approximately 50 μm. Images were examined in the axial, sagittal and coronal planes to analyze the bone formation in the region of interveterbral fusion. Data were processed by micro-CT software (Dragonfly 4.0, Object Research Systems, Canada) and three-dimensional images were reconstructed. The bone volume (BV), tissue volume (TV) and BV/TV were quantified.
2.9 Histology
Histological samples were obtained from Ti-PEEK and PEEK dowels at 12 weeks to evaluate bone formation and apposition. The samples were placed into appropriately labeled containers flled with a tenfold volume of 10% neutral buffered formalin and were shipped to anoutside laboratory for undecalcifed processing and analysis. The samples from each group were stained with toluidine blue ranse, H&E ranse and Goldener trichrome ranse. And then they were evaluated by histomorphometry for new bone formation and bony apposition.
2.10 Statistical analysis
All data were expressed as mean ± standard deviation (SD). The statistical analyses were performed by SPSS 19.0 software. Statistical analysis was performed using non-parametric analysis of variance (ANOVA) testing (Kruskal–Wallis) and p < 0.05 was considered statistically significant.
3 Results
3.1 Characterization of the Ti-PEEK
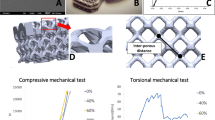
The surface characterization of the Ti-PEEK cages and PEEK cages were analyzed by SEM. We observed very thin grooves and ligaments due to the machining process as shown in Fig. 1a-b. However, numerous spherical titanium particles with a diameter between 0.5 μm and 5 μm were partially melted on the surface of the Ti-PEEK cages (Fig. 1c-d). Some titanium particles of the coating were slightly flattened because of the post coating blasting process, which is needed to reduce loose particles. The coating thickness of Ti was 124.2 ± 11.3 μm, the porosity of the Ti was 44.1% ± 1.5%, and the roughness after coating was 115.1 ± 6.7 μm (Table 2). The failure modes of the products in the Ti-PEEK cage group were plastic deformation in the direction of force, and the coating did not fall off. The failure modes of the products in the control group were plastic deformation in the direction of the force. The failure pictures of the products in the Ti-PEEK cage group are shown in Fig. 2a, and the failure pictures of the products in the PEEK cage group are shown in Fig. 2b. The yield loads of the static four-point bending test of the Ti-PEEK and PEEK cage were 1166.2 ± 48.4 N and 1118.2 ± 26.6 N. There was no difference between the two groups. The yield displacement of the Ti-PEEK cages and PEEK cages were 3.56 ± 0.05 mm and 3.48 ± 0.12 mm. There was also no difference between the two groups (Fig. 2c-d). Therefore, the static four-point bending performance of the Ti-PEEK cages was not inferior to that of the PEEK cages. The contact angles of PEEK cages and Ti-PEEK cages were 76.0° ± 8.0° and 41.0° ± 10.0° respectively (Fig. 2e). The contact angles of Ti-PEEK cages were lower than that of PEEK cages and the difference was significant (P < 0.05). In addition, the pictures of Ti -PEEK cage was shown as Fig. S1, and the EDS analysis (Fig. S2) indicated that the Ti element was included in the compositions. Besides, the element analysis was provided in Table S1.
The results of static four point bend test showed that the failure modes of the products in the Ti-PEEK group a were plastic deformation in the direction of force, and the coating did not fall off. The failure modes of the products in the PEEK group b were plastic deformation in the direction of force. There was no difference between the Ti-PEEK group and PEEK group in terms of yield load c and yield displacement d. The contact angle test of Ti-PEEK cage group and PEEK cage group. The result showed that the average contact angle of Ti-PEEK cage group was much higher than those of PEEK cage group e
3.2 Cell morphology and proliferation analysis
The cell morphology was observed using the skeleton staining (Fig. 3a-f) of Cy3-phalloidine (Red) and DAPI (Blue) and SEM after 3 days of culture of the Ti-PEEK and PEEK cages. Both cytoskeleton staining and SEM images indicated the MC3T3-E1 cells spread and grew well on the two cages (Fig. 3g-h). The cell proliferation on both cages was determined by the MTS assay at 1, 3, 5 and 7 days. The results showed that the MC3T3-E1 cells proliferated well on both the Ti-PEEK cage and PEEK cage, and there was no significant difference compared to a TCP surface (Fig. 3i).
Cytoskeleton staining images of MC3T3-E1 cells for Cy3-phalloidin (red) and DAPI (blue) on the surface of PEEK cages a-c and Ti-PEEK cages d-e. SEM images of MC3T3-E1 on the surface of PEEK cages g and Ti-PEEK cages i. The scale bars, 200 μm a-e and 20 μm g-h. Cell proliferation i tested by MTS assay of MC3T3-E1 cells on PEEK cages and Ti-PEEK cages, cells growing on the TCPS as for control
3.3 Detection of osteogenic capacity in vitro
The osteogenic gene expression of Col-I, ALP, Runx-2 and OCN were tested by RT-qPCR. After two weeks culture, the gene expression of Collagen-I from MC3T3-E1 cells cultured on Ti-PEEK cages was 1.6 times higher than those on the PEEK cages (Fig. 4a). However, MC3T3-E1 cells on Ti-PEEK cages was approximately 1.7 times greater than those on the PEEK cages in terms of ALP (Fig. 4b). As to the gene expression of Runx-2, the expression of Runx-2 from the MC3T3-E1 cells grown on the Ti-PEEK cages was nearly 1.3 times greater than those on PEEK cages (Fig. 4c). In addition, the gene expression of OCN from the MC3T3-E1 cells cultured on Ti-PEEK cages was 1.4 times greater than those on PEEK cages (Fig. 4d). Additionally, the osteogenic related protein of Col-I, ALP, Runx-2 and OCN was tested by Western blot analysis. The result shows that levels of these osteogenic related proteins secreted from MC3T3-E1 cells on Ti-PEEK were also significantly greater than that observed from cells on PEEK cages (Fig. 4e).
3.4 Surgery and postoperative period
There were no deaths or spinal cord injuries in the sheep during the surgery. After the surgery, the sheep were fed normally, and the wounds healed normally. Additionally, no delamination of the Ti coating was visible during the surgery. The operation pictures and X-ray immediately after operation were shown in Fig. S3 and Fig. S4. The light press fit of the implants resulted in primary stability of all implants and prevented clinical mobility.
3.5 Histology
The result of histological examination of the Ti-PEEK cages showed bony apposition immediately on the surface of the Ti-PEEK cage at the 12-week time point. (Fig. 5). However, the PEEK dowels did not demonstrate the same extent of bony apposition. On the contrary, the fibrous connective tissue could be observed in the histological specimen taken from the PEEK cage group just as Fig. 5 showed.

taken from the PEEK group as the red allow showed. Scale bars: Scale bars: a-b,e–f,i-j 2 mm; c-d,g-h,k-l 1 mm
The toluidine blue ranse a at 12 weeks for Ti-PEEK cage and PEEK cage. The Ti-PEEK cage had direct bone ongrowth at 12 weeks, whereas the PEEK samples presented a fibrous tissue interface with limited direct bone contact as the red allow showed. The typical HE ranse result b at 12 weeks for Ti-PEEK cage compared to PEEK cage. The Ti-PEEK cage had direct bone ongrowth at 12 weeks. In the PEEK group, the fibrous connective tissue resulted in a smaller percentage of the circumference of the dowel being directly opposed to bone as the red allow showed. Goldener trichrome stain result c at 12 weeks for Ti-PEEK cage and PEEK cage. The histological examination of the Ti-PEEK group shows bony apposition adjacent to the Ti-PEEK cage surface. Fibrous connective tissue is the only evident in the histological specimen
3.6 Micro-CT analysis
Micro-CT analysis showed that Ti-PEEK cages supported rapid bone formation within 12 weeks. In contrast, PEEK cages achieved only partial unbridged intervertebral fusion (Fig. 6a-h). The new bone formation was greater with the Ti-PEEK cages than the PEEK cages at 12 weeks. At the 12th week, the bone formation of BV/TV (Bone Volume/Tissue Volume) levels in the Ti-PEEK cages was 77.12% ± 10.80%, which was greater than 56.72% ± 7.84% in the PEEK cages (Fig. 6i). The quantitative results of the micro-CT are similar to those of three-dimensional bone reconstruction.
Micro-CT analysis of bone formation in vertebral fusion area were observed at 12 weeks. 3D bone reconstruction and two-dimensional images of PEEK cage a-b, e–f and Ti-PEEK cage c-d, g-h were exhibited. Quantitative analysis of Bone Volume/Tissue Volume (BV/TV) of PEEK cages and Ti-PEEK cages in vertebral fusion region by Micro-CT i
4 Discussion
Anterior cervical intervertebral decompression and fusion with autologous iliac bone graft often results in collapse of the graft and loss of intervertebral space height. PEEK has clear benefits in the application of spinal fusion surgery in terms of reduced elastic modulus and good chemical resistance, whereas the lack of direct bone apposition that results in a nonreactive fibrous layer post-operatively remains a potential concern (Pelletier et al. 2016). Many studies have been reported to overcome the shortcomings of PEEK. An effective option is to coat the surface of PEEK with a bioactive substance for not only enhancing the biocompatibility of the PEEK but also maintaining its other advantages. In this study, we coated a thin Ti layer on the surface of a PEEK cage with vacuum plasma spraying technique to further develop the Ti-PEEK composites as cervical spinal fusion cages, and the osteoblastic performance of the Ti layer coating on the PEEK cage was evaluated through in vitro and in vivo tests. Sheep were chosen as the animal model to evaluate the effectiveness of Ti-PEEK cages because they are similar to humans in spine anatomy and kinematics. It is well known that the surface characteristics, including the surface roughness, topography and chemical composition, can directly affect the biocompatibility and osteoconductive activity of progenitor and mature osteoblast cells (Schwarz et al. 2010; Anselme and B. Noe¨l, Hardouin P. 1999). Various methods have been introduced to form Ti layers on PEEK cages, including electron beam deposition (Han et al. 2010), ionic plasma deposition (Yao et al. 2007) and plasma spray deposition (Wu et al. 2009). We used a vacuum plasma spraying method to coat Ti on PEEK cages. The optimized dynamic of the coating process helps to keep the implant below 200 °C to avoid alterations of the PEEK substrate. The atmosphere and pressure level are important variables for plasma spraying and various process can be obtained by the interactions between the melted powder and surrounding atmosphere are strongly reduced. This is indispensable for coating titanium materials, which are materials sensitive to oxidation and nitrogen absorption. During vacuum plasma spraying, the melting grade of particles can be easily managed by changing the chamber pressure, which allows tailoring of the coating porosity while maintaining very good cohesion and adhesion. In fact, the surface characteristics in our case achieved satisfactory results. The high porosity structure promotes osteoblasts and bone grew into the cage. Cells cultured on rougher surfaces tend to exhibit attributes of more differentiated osteoblasts (Boyan et al. 2015). Besides, the contact angle of Ti-PEEK cage was much lower than that of PEEK cage, which proved that the the Ti layer improved hydrophilicity of PEEK cage. Regarding the mechanical characteristics, the static state four-point bending test proved that the Ti layer did not alter the mechanical strength. The morphology of the MC3T3-E1 cells grown on the cage surface was observed by skeleton staining and SEM. The skeleton staining result showed that the MC3T3-E1 cells adhered well on the surface of both Ti-PEEK and PEEK cages after culturing for three days, which was similar to the MTS analysis that demonstrated that cells on either cage proliferated well. In addition, SEM images indicated that the cells cultured on the Ti-PEEK cages more widely spread in comparison to the PEEK cage surface cultured for 3 days. In our opinion, the stretched morphology could be attributed to the microporous titanium implant surface structure, which promoted cell attachment at the surface of the implants. The result was also in line with a previous study. For example, Ma found that the Ti/PEEK combination stimulated the osteoblast adhesion and cell spreading (Ma and Tang 2014). The same result was observed by Han who found the MC3T3-E1 cells spread more widely on Ti-coated PEEK prepared by electron beam (e-beam) deposition technique than PEEK (Han et al. 2010). In addition to the cell proliferation, the osteogenic differentiation characteristics of MC3T3-E1 cells on the surface of Ti-PEEK cages and PEEK cages were also investigated. The osteogenic related gene expression of Col-I, ALP, Runx-2 and OCN were evaluated. The result revealed that these gene expressions were up-regulated from MC3T3-E1 cells on the surface of Ti-PEEK cages after culturing for two weeks. The western-blot analysis also proved that the MC3T3-E1 cells on the surface of the Ti-PEEK cages generated more Col-I, ALP, Runx-2 and OCN protein. As Col-I, ALP, Runx-2 and OCN were traditionally regarded as osteogenic differentiation-specific markers, the experiments indicated that the Ti-PEEK cage surface may be more suitable for cell osteogenic differentiation. These findings are to some extent in accordance with previous studies. Cheng (Cheng et al. 2018) cultured MG63 cells on Ti-PEEK and PEEK implants, observing a significant increase in bone cell differentiation as measured by ALP levels. Rosa (Rosa and Beloti 2003) found that the proliferation of human bone marrow cells was reduced while total protein content, and ALP activity were increased when cultured on Ti with roughnesses ranging from 0.80 µm to 1.90 µm. In another study, Han coated a pure titanium layer on PEEK to manufacture a Ti-PEEK implant using an e-beam deposition method. After culturing MC3T3-E1 cells, the Ti-coated PEEK substrate showed a significantly higher ALP level than the PEEK substrate (Han et al. 2010). It should be noted that as an early bone cell differentiation marker (Stein et al. 1990), up-regulated ALP could prevent early stage implant loosening, which is mostly caused by insufficient osseointegration on the implant surface (Castellani et al. 2011). The in vitro results indicated that Ti-PEEK promotes early osteogenesis. The ultimate goal of a fusion cage is to achieve osseous fusion in the intervertebral space. The micro-CT results of the in vivo sheep cervical spine fusion tests showed that the Ti-PEEK cages demonstrate a significantly greater amount of bone ingrowth at 12 weeks compared to the PEEK cages. The results were also observed as the translation of the enhanced osseointegration activity of Ti-PEEK cages in vitro. What’s more, the histology result also indicated good evidence of bone ingrowth and little evidence of fibrous connective tissue for the Ti-PEEK implant at the 12-week time point. The area surrounding the Ti-PEEK cages quickly filled up with new bone. On the other hand, the PEEK samples presented a fibrous tissue interface with limited direct bone contact. The similar result was found in the previous study. Walsh (Walsh et al. 2015) placed PEEK and plasma-sprayed titanium coated PEEK implants (Ti-bond implants) in a line-to-line manner in cortical bone and in a press-fit manner in cancellous bone of adult sheep. At 4 and 12 weeks, the histologic result showed that the Ti-bond implants had achieved direct bone-to-implant bonding, whereas the PEEK samples were around fibrous connective tissue with little new bone formation. The same results were observed in clinical studies. For example, (Zhu et al. 2021) evaluated t the PEEK cages coated with Ti and HA and uncoated PEEK cages in patients who received single level ACDF operation. After 3 months of operation, the fusion rate of PEEK/Ti/HA group was signifcantly higher than PEEK group (87.5% vs. 62.5%). It is widely accepted that implant loosening from the bone is one of the main factors leading to the failure of a biological implant. Early stage implant loosening is mostly caused by the failure of new bone formation due to insufficient osseo-integration growth on the implant surface. Therefore, Ti is a strong candidate as the coating material for PEEK implants. Especially, Ti is only surpassed by bioactive ceramics, such as hydroxyapatite or bioglass, and natural biopolymers in terms of biocompatibility. In fact, Ti is a “gold standard” material in orthopedics subsequent to the discovery of its osseointegration capacity (Fujibayashi et al. 2011). Additionally, Cheng(Cheng et al. 2018) compared the osseointegration ability between plasma-sprayed titanium-coated PEEK (Ti-PEEK) substrate and uncoated PEEK implants, indicating indicated that the Ti-PEEK surface demonstrated enhanced osseointegrative properties compared to the PEEK both in vitro and in vivo.
5 Conclusions
In the present study, the Ti-PEEK cage was successfully manufactured by coating Ti on the surface of the PEEK cage using a vacuum plasma spraying technology. The cell skeleton staining and cell proliferation test indicated that MC3T3-E1 cells grew well on the Ti-PEEK cages. The osteogenic gene expression and western blot analysis of osteogenic protein showed that the Ti-PEEK cage had better osteo-conductivity compared to PEEK cages. The in vivo sheep tests also indicated that the Ti coating enhanced bone formation activity of PEEK. These in vitro and in vivo results demonstrated that the Ti layer on the surface of PEEK cages supported bone apposition by providing an osteo-conductive surface, which may have good application prospects in ACDF surgery.
References
K. Anselme, B. Noe¨l, P. Hardouin, Human osteoblast adhesion on titanium alloy, stainless steel, glass and plastic substrates with same surface topography. J. Mater. Sci. Mater. Med. 10(12), 815–819 (1999)
S. Belouettar, A. Abbadi, Z. Azari et al., Experimental investigation of static and fatigue behaviour of composites honeycomb materials using four point bending tests. Compos. Struct. 87(3), 265–273 (2009)
N. Bertollo, R. Da Assuncao, N.J. Hancock et al., Influence of electron beam melting manufactured implants on ingrowth and shear strength in an ovine model. J. Arthroplasty 27(8), 1429–1436 (2012)
H. Bodén, M. Salemyr, O. Sköldenberg et al., Total hip arthroplasty with an uncemented hydroxyapatite-coated tapered titanium stem: results at a minimum of 10 years’ follow-up in 104 hips. J. Orthop. Sci. 11(2), 175–179 (2006)
B.D. Boyan, R. Batzer, K. Kieswetter et al., Titanium surface roughness alters responsiveness of MG63 osteoblast-like cells to 1α,25-(OH)2D3. J. Biomed. Mater. Res., Part A 39(1), 77–85 (2015)
G.R. Buttermann, Anterior cervical discectomy and fusion outcomes over 10 years. Spine 43(3), 207–214 (2018)
C. Castellani, R.A. Lindtner, P. Hausbrandt et al., Bone–implant interface strength and osseointegration: Biodegradable magnesium alloy versus standard titanium control. Acta Biomater. 7(1), 432–440 (2011)
B.C. Cheng, S. Koduri, C.A. Wing et al., Porous titanium-coated polyetheretherketone implants exhibit an improved bone–implant interface: an in vitro and in vivo biochemical, biomechanical, and histological study. Medical Devices (Auckland, NZ) 11, 391 (2018)
D.M. Devine, J. Hahn, R.G. Richards et al., Coating of carbon fiber-reinforced polyetheretherketone implants with titanium to improve bone apposition. J. Biomed. Mater. Res. B Appl. Biomater. 101(4), 591–598 (2013)
M. van Dijk, T.H. Smit, S. Sugihara et al., The effect of cage stiffness on the rate of lumbar interbody fusion: an in vivo model using poly (l-lactic Acid) and titanium cages. Spine 27(7), 682–688 (2002)
D. Duraccio, F. Mussano, M.G. Faga, Biomaterials for dental implants: current and future trends. J. Mater. Sci. 50(14), 4779–4812 (2015)
S. Fujibayashi, M. Takemoto, M. Neo et al., A novel synthetic material for spinal fusion: a prospective clinical trial of porous bioactive titanium metal for lumbar interbody fusion. Eur. Spine J. 20(9), 1486–1495 (2011)
K.Y. Ha, J.H. Shin, K.W. Kim et al., The fate of anterior autogenous bone graft after anterior radical surgery with or without posterior instrumentation in the treatment of pyogenic lumbar spondylodiscitis. Spine 32(17), 1856–1864 (2007)
C.M. Han, E.J. Lee, H.E. Kim et al., The electron beam deposition of titanium on polyetheretherketone (PEEK) and the resulting enhanced biological properties. Biomaterials 31(13), 3465–3470 (2010)
E.K. Hansson, T.H. Hansson, The costs for persons sick-listed more than one month because of low back or neck problems. A two-year prospective study of Swedish patients. Eur. Spine J. 14(4), 337–345 (2005)
A. Hermansen, R. Hedlund, L. Vavruch et al., A comparison between the carbon fiber cage and the cloward procedure in cervical spine surgery: a ten-to thirteen-year follow-up of a prospective randomized study. Spine 36(12), 919–925 (2011)
P. Korovessis, T. Repantis, V. Vitsas et al., Cervical spondylodiscitis associated with oesophageal perforation: a rare complication after anterior cervical fusion. Eur. J. Orthop. Surg. Traumatol. 23(2), 159–163 (2013)
S.M. Kurtz, J.N. Devine, PEEK biomaterials in trauma, orthopedic, and spinal implants. Biomaterials 28(32), 4845–4869 (2007)
S.D. Kuslich, C.L. Ulstrom, S.L. Griffith et al., The Bagby and Kuslich method of lumbar interbody fusion: history, techniques, and 2-year follow-up results of a United States prospective, multicenter trial. Spine 23(11), 1267–1278 (1998)
R. Ma, T. Tang, Current Strategies to Improve the Bioactivity of PEEK. Int. J. Mol. Sci. 15(4), 5426–5445 (2014)
A. Nouri, L. Tetreault, A. Singh et al., Degenerative cervical myelopathy: epidemiology, genetics, and pathogenesis. Spine 40(12), E675–E693 (2015)
M.H. Pelletier, N. Cordaro, V.M. Punjabi et al., PEEK Versus Ti Interbody Fusion Devices: Resultant Fusion, Bone Apposition, Initial and 26-Week Biomechanics. Clinic. Spine. Surg. 29(4), E208 (2016)
A.L. Rosa, M.M. Beloti, Effect of cpTi surface roughness on human bone marrow cell attachment, proliferation, and differentiation. Braz. Dent. J. 14(1), 16–21 (2003)
A.J. Schoenfeld, A.A. George, J.O. Bader et al., Incidence and epidemiology of cervical radiculopathy in the United States military: 2000 to 2009. J. Spinal. Disord. Tech. 25(1), 17 (2012)
M.L.R. Schwarz, M. Kowarsch, S. Rose et al., Effect of surface roughness, porosity, and a resorbable calcium phosphate coating on osseointegration of titanium in a minipig model. J. Biomed. Mater. Res., Part A 89A(3), 667–678 (2010)
Y.C. Shin, K.M. Pang, D.W. Han et al., Enhanced osteogenic differentiation of human mesenchymal stem cells on Ti surfaces with electrochemical nanopattern formation. Mater. Sci. Eng., C 99, 1174–1181 (2019)
G.S. Stein, J.B. Lian, T.A. Owen, Relationship of cell growth to the regulation of tissue-specific gene expression during osteoblast differentiation. FASEB J. 4(13), 3111–3123 (1990)
F. Tan, M. Naciri, D. Dowling et al., In vitro and in vivo bioactivity of CoBlast hydroxyapatite coating and the effect of impaction on its osteoconductivity. Biotechnol. Adv. 30(1), 352–362 (2012)
J.M. Toth, M. Wang, B.T. Estes et al., Polyetheretherketone as a biomaterial for spinal applications. Biomaterials 27(3), 324–334 (2006)
W.R. Walsh, N. Bertollo, C. Christou et al., Plasma-sprayed titanium coating to polyetheretherketone improves the bone-implant interface. The Spine Journal 15(5), 1041–1049 (2015)
A. Wennerberg, T. Albrektsson, Effects of titanium surface topography on bone integration: a systematic review. Clin. Oral Implant Res. 20, 172–184 (2009)
B. Wiedenhöfer, J. Nacke, M. Stephan et al., Is Total Disk Replacement a Cost-effective Treatment for Cervical Degenerative Disk Disease? Clin. Spine Surg. 30(5), E530–E534 (2017)
G.M. Wu, W.D. Hsiao, S.F. Kung, Investigation of hydroxyapatite coated polyether ether ketone composites by gas plasma sprays. Surf. Coat. Technol. 203(17), 2755–2758 (2009)
J.J. Yang, C.H. Yu, B.S. Chang et al., Subsidence and nonunion after anterior cervical interbody fusion using a stand-alone polyetheretherketone (PEEK) cage. Clin. Orthop. Surg. 3(1), 16–23 (2011)
C. Yao, D. Storey, T.J. Webster, Nanostructured metal coatings on polymers increase osteoblast attachment. Int. J. Nanomed. 2(3), 487–492 (2007)
C. Zhu, M. He, L. Mao et al., Titanium-interlayer mediated hydroxyapatite coating on polyetheretherketone: a prospective study in patients with single-level cervical degenerative disc disease. J. Transl. Med. 19(1), (2021)
Acknowledgment
The study was supported by the National Nature Science Foundation of China (81572185, 81702158); National Nature Science Foundation of Anhui Province (1708085MH185, 1708085QH205, 1808185QH275); Foreign Science and Technology Cooperation of Anhui Province (1704e1002229, 202004b11020027); Funding of “Peak” Training Program for Scientific Research of Yijishan Hospital, Wannan Medical College (GF2019T02, GF2019G07, GF2019G12).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liu, C., Zhang, Y., Xiao, L. et al. Vacuum plasma sprayed porous titanium coating on polyetheretherketone for ACDF improves the osteogenic ability: An in vitro and in vivo study. Biomed Microdevices 23, 21 (2021). https://doi.org/10.1007/s10544-021-00559-y
Accepted:
Published:
DOI: https://doi.org/10.1007/s10544-021-00559-y