Abstract
The development of in vitro methods of engineering three-dimensional cardiac tissues can be useful for tissue replacement, diagnostics and drug discovery. Here, we introduce the use of patterned hyaluronic acid (HA) substrates generated using microfluidic patterning as a method of fabricating 3D cardiac organoids. HA micropatterns served as inductive templates for organoid assembly. Upon seeding, cardiomyocytes elongated and aligned along the pattern direction attaching preferentially to the glass substrate and the interface between HA patterns and glass substrate. After 3 days in culture, the linearly aligned myocytes detached from the surface and formed contractile cardiac organoids. The procedure can be utilized to simply, rapidly and inexpensively create in vitro cardiac tissue models.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
The inability of myocardium to regenerate after injury necessitates the need for development of alternative treatment options. Engineered three-dimensional (3D) cardiac tissues can thus serve as models to study normal and pathological tissue function in vitro, or test the effect of drugs on tissue structure and function.
Induction of cardiac tissue assembly is one of the challenges in 3D approaches. In one approach heart cells are combined with scaffolds made of natural (collagen (Li et al., 2000)) or synthetic materials (poly glycolic acid (Carrier et al., 1999)) and cultivated in bioreactors designed to provide some of the aspects of the environment found in the native myocardium (Radisic et al., 2003, 2004a,b 2005). Scaffolds serve as inductive templates for tissue assembly while bioreactors provide sufficient nutrient and oxygen supply (Radisic et al., 2004b) or physical stimuli (Radisic et al., 2004b). Hydrogels can also be utilized for induction of 3D tissue assembly. Differentiated cardiac tissue had been engineered by casting neonatal rat cardiac myocytes into collagen gels and subjecting them to cyclic mechanical stretch (Zimmermann et al., 2002).
In a scaffold-free approach, 3D tissues were created by stacking confluent cardiac monolayers. The monolayers, cultivated on a temperature responsive surface, were detached upon the change in temperature and stacked to create 25–50 μm thick cardiac tissue (Shimizu et al., 2002). Most recently, 24 mm long and 100 μm thick contractile cardiac organoids were fabricated by self-organization (Baar et al., 2005). Cardiomyocytes were cultivated on a PDMS surface coated with laminin. As laminin degraded the confluent monolayer detached from the periphery of the substrate, moving towards the center and wrapping around a string placed in the center of the plate until a cylindrical contractile organoid was formed.
Cell and protein arrays have been generated on various substrates using soft lithographic approaches such as self-assembled monolayers (SAMs) (Singhvi et al., 1994; Mrksich and Whitesides, 1996; Mrksich et al., 1996; 1997; Whitesides et al., 2001; Prime and Whitesides, 1991; Chen et al., 1997), microstamped proteins (Hyun et al., 2001), biological (Bhatia et al., 1997,1998a,b, 1999) and comb polymers (Hyun et al., 2003), microfluidic channels (Murakami et al., 1999), and elastomeric membranes (Ostuni et al., 2000; Folch et al., 2000). Since native myocardium consists of elongated cardiomyocytes arranged into aligned myofibers, significant efforts have been focused on reproducing the elongated phenotype on two-dimensional (2D) substrates. Attachment and alignment has been modulated using grooved and pegged surfaces (Deutsch et al., 2000). Micropatterning substrates and microdevices have a potential of enhancing the function of cardiomyocytes by controlling topographical features and spatial presentation of surface molecules. For instance, fibroblasts overgrowth in cultures of primary cardiomyocytes was prevented using topographical cues (Boateng et al., 2003). Spatially organized cardiomyocyte cultures were created on biodegradable, elastomeric polyurethane films patterned by microcontact printing of laminin lanes (McDevitt et al., 2002). Elongated phenotype was achieved by patterning photoresist lanes on glass substrate and growing the myocytes onto the exposed glass (Rohr et al., 1991; Thomas et al., 2000). Myocyte cultivation on patterned substrates generated important insight into the role of fibroblasts (Gaudesius et al., 2003) in electrical signal propagation as well as the effect of electrical field shocks on changes in transmembrane potential (Fast et al., 2000). However, the described methods specifically using cardiomyocytes generated only 2D structures.
Microfluidic patterning through 2D and 3D networks has been used previously to obtain complex structures of E. Coli, erythrocytes, bovine capillary endothelial cells and human bladder cancer cells (Takayama et al., 1999; Chiu et al., 2000). Microfluidic networks were utilized to pattern avidin on surfaces followed by binding of biotinylated human dermal fibroblasts (Sinclair and Salem, 2006). Geometric parameters essential for formation of functional neuronal networks were investigated via microfluidic patterning of poly-L-lysine and collagen-4 (Romanova et al., 2004). Three dimensional structures were achieved using photoreaction injection molding in microfluidic channels of cells (e.g. fibroblasts) encapsulated in the RGD modified poly(ethylene glycol) (Koh et al., 2003). In addition, microfluidic patterning allows for formation of 3D structures consisting of multiple cell types (e.g. fibroblasts, smooth muscle and endothelial cells) (Tan and Desai, 2003, 2004). In this approach a desired cell type resuspended in an appropriate extracellular matrix was applied into a microfluidic network. Following the contraction of the biopolymer matrix by cells another layer with a different cell type was applied to the microfluidic network to build a tissue with multiple cell types arranged in the z-direction.
Hyaluronic acid (HA), or hyaluronan, is a natural, linear and nonadhesive glycosaminoglycan (Morra, 2005), which is composed of repeating disaccharide units of N-acetyl-D-glucosamine and D-glucuronic acid. As a component of the ECM, HA is found in many tissues where it plays an important role in lubrication, water-sorption, water-retention, and a number of cellular functions such as attachment, migration, and proliferation (Bulpitt and Aeschlimann, 1999; Oerther et al., 1999). Thus, HA may be a suitable biomaterial for many applications relating to tissue engineering, and viscosupplementation (Abantangelo and Weigel, 2000; Balazs, 1973; Piacquadio et al., 1997; Pei et al., 2002). We have previously shown that HA can be patterned on hydrophilic surfaces using a moulding process for the fabrication of cell arrays (Suh et al., 2004) and patterned co-cultures (Khademhosseini et al., 2004). We hypothesized that the biocompatible and enzymatically degradable nature of HA may make it a useful technology for formation of cardiomyocyte organoids.
In this paper, we demonstrate the feasibility of fabricating contractile cardiac organoids via microfluidic patterning of hyaluronic acid on a glass substrate. Aqueous HA solution was forced through microchannels that were reversibly sealed on a glass substrate and allowed to physically adsorb on particular regions of the substrate. Upon removal of the microfluidic mould the patterned HA substrate was generated. HA patterns served as inductive templates for organoid assembly. Upon seeding, cardiomyocytes elongated and aligned along the pattern direction, attaching preferentially to the glass substrate and the interface between HA patterns and glass substrate. After 3 days in culture, the myocytes, detached from the surface and formed contractile cardiac organoids. The procedure can be utilized to create in vitro cardiac tissue models simply, rapidly and inexpensively.
2 Methods
2.1 Materials
All tissue culture media and serum were purchased from Gibco Invitrogen Corporation. All chemicals were purchased from Sigma, unless otherwise indicated.
2.2 PDMS fabrication
Polydimethylsiloxane (PDMS) (Essex Chemical, Sylgard 184) moulds were fabricated by mixing silicone elastomer and curing agent in a 10:1 ratio. The mixture was poured onto the silicon masters that were patterned with SU-8 in the shape of lanes of 100 μm in width and 60 μm in height and cured at 60°C for 4 hr. PDMS moulds were then peeled from the silicon surfaces and cut prior to use. For patterning, the surfaces of PDMS moulds were made hydrophilic by plasma treatment for 1min (60 W, PDC-32G, Harrick Scientific).
2.3 Microfluidic patterning and analysis
Solutions containing 5 mg/ml HA (Genzyme) or FITC-HA (Sigma) in distilled water solution were made and vortexed overnight. To pattern the substrates, PDMS microfluidic moulds were cleaned using soap, water and ethanol and then plasma cleaned for 1 min. The mould was then placed on a glass slide to form a reversibly sealed array of microchannels on the substrate. To pattern the HA, a few drops of the HA was placed on one side of the mould. The HA solution filled the channels through capillary action. The HA was left undisturbed to dry for 12 hr at room temperature. Subsequently, the PDMS mould was removed and the substrate was rinsed with water, which resulted in the formation of HA patterns.
Texas Red-BSA and FN (Sigma) were dissolved in PBS at a concentration of 250 μg/mL, and 50 μg/mL, respectively. A few drops of the protein solution was then evenly distributed onto the substrates and stored at room temperature for 30 min, and subsequently rinsed with PBS solution and water and blown dry in a stream of nitrogen. To measure fibronectin adhesion, the surfaces were stained with anti-fibronectin antibody (Sigma) for 45 min, followed by 1 hr incubation with the FITC-labelled anti-rabbit secondary antibody (Sigma). The surfaces were then imaged using an inverted microscope (Axiovert 200, Zeiss).
2.4 Scanning electron microscopy
To perform scanning electron microscopy (JEOL 6320FV), samples were mounted onto aluminium stages, sputter coated with gold to a thickness of 200 Å and analyzed at a working distance of 20 mm.
2.5 Cells
Cardiomyocytes were obtained from 1 to 2 day old neonatal Sprague Dawley rats using a protocol approved by the Institute’s Committee on Animal Care. In brief, ventricles were quartered, incubated overnight at 4°C in a 0.06% (w/v) solution of trypsin in Hank’s Balanced Salt Solution (HBSS), washed in culture medium, and subjected to a series of digestions (3 min, 37°C, 150 rpm) in 0.1% (w/v) solution of collagenase type II in HBSS. The first digestate was discarded, and the cell suspensions from the subsequent 4–6 digestions were centrifuged (750 rpm, 4 min), resuspended in HBSS, pooled, and resuspended in DMEM containing 4.5 g/L glucose supplemented with 10% FBS, 10 mM HEPES, 2 mM L-glutamine and 100 units/ml penicillin. Cells were pre-plated for one 60 min period to enrich for cardiomyocytes (i.e. cells that remained unattached were used for seeding).
NIH-3T3 fibroblasts were purchased from American Type Culture Collection and maintained in 10% fetal bovine serum (FBS) in Dulbecco’s modified eagle medium (DMEM). They were cultured at 37°C, 5% CO2 in humidified incubator and passaged every 3 days. To analyze cell adhesion, NIH-3T3 cells at a concentration of 1×106 cells/mL were seeded on HA or glass surfaces, the attached cells were counted after six-hour incubation.
2.6 Cardiomoycte seeding and culture
The glass substrates with patterned HA were placed into 6 well plates (one substrate/well) and rinsed briefly with 2 ml of PBS and UV sterilized for 10 min (UV-B, EFOS Ultracure 100ss Plus, UV spot lamp). Each well was inoculated with 1.5×106 cells using 2 ml of culture medium. The medium was completely replaced 5 hr later and every 2 days thereafter. Images were taken at 100 × and 200 × (Nikon Diaphot microscope) to assess cell attachment. Contractions were video recorded using a CCD camera attached to the microscope.
2.7 Immunostaining
After 6 days in culture, the organoids were fixed in paraformaledehyde (4%, 30 min) and incubated with polyclonal rabbit anti-cardiac troponin I for 30 minutes at room temperature (1:50, Chemicon) followed by incubation with fluorescein conjugated goat anti-rabbit IgG (1:100, Vector Laboratories) for 30 min at room temperature. The glass slides with organoids were coverslipped using mounting medium with DAPI (Vector Laboratories) and imaged using Zeiss Axioplan.
2.8 Image analysis
To assess contractile properties, the video-recorded sequences were digitized at the rate of 25 frames per second. The contraction frequency was assessed by counting. To assess the amplitude and the duration of contraction, the digitized sequences were imported as a stack into ImageJ. For each beating strand a landmark was determined. The position of the landmark in the first frame was identified as a reference point. As the contraction occurred the landmark moved away from the reference point (Fig. 4). The distance between the landmark and the reference point was determined for each frame using Image J, and plotted to determine amplitude and duration of contraction (Fig. 5).
2.9 Statistical analysis
Statistical analysis was performed using one-way ANOVA in conjunction with Tukey’s test or Dunn’s test using SigmaStat 3.0. Normality and equality of variance was tested for each data set. P<0.05 was considered significant.
3 Results and discussion
3.1 Approach to organoid formation
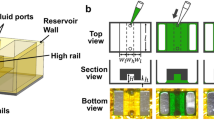
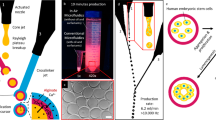
Figure 1 illustrates the procedure for fabricating cardiomyocyte organoids using a microfluidic patterning method. In this approach, a PDMS microfluidic mould was placed on a glass substrate, and HA solution was injected into the microchannels (100 μm in width and 60 μm in height) and allowed to physisorb onto the substrate after 12 hr of incubation at room temperature. Once the cell-repulsive HA regions were formed, the PDMS mould was removed, and the resulting substrate was rinsed with PBS and treated with fibronectin to generate cell-adhesive regions. Primary cardiomyocytes were then seeded onto the microlanes and allowed to elongate and attach, forming long strands. The organiods spontaneously lifted off from the surface and started beating. Presence of residual PDMS (from the stamp) on the glass substrate was crucial for the lift-off of cardiac organoids. The patterns that were dried for a time period lesser then 12 hr did not have residual PDMS in between HA lanes and although patterned lanes of cardiomyocytes were formed, they could not lift off the surface to form 3D organoid.
Characterization of microfluidic patterned HA surfaces. (A, B) Representative SEM and (C, D) light microscope (A, C) images of the unwashed and (B, D) washed HA-patterned substrates. (E) represents FITC-HA patterned regions, while (F) represents subsequent TR-BSA adsorption on HA micropatterned surface. (G, H) represent fibroblast cell adhesion 6 h after seeding on (G) HA-coated and (H) glass surfaces that were treated with fibronectin
3.2 Patterned HA substrates
To generate HA micropatterns, microfluidic channels were used to deliver the HA solution to specific regions of a substrate. The microfluidic patterning is applicable for this application, since the desired features are in the shape of long lanes. PDMS microfluidic moulds were placed on glass substrates and reversibly sealed. In this process, the reversible sealing of elastomeric microchannels, fabricated from PDMS was used to generate channels in which the HA solution could be deposited. The 0.5% w/v solution of HA was then added to one end of the channel and was pulled through the microchannel using capillary action. Figure 2 demonstrates the HA patterning process and characterization.
We have previously characterized this process using capillary moulding and microcontact printing approaches (Suh et al., 2004). Here, we demonstrate that microfluidic patterning can also be used to pattern HA on glass substrates. Scanning electron microscopy (SEM) images (Fig. 2(A)) show that HA deposition is regulated by the drying process as well as the geometry of the microchannels. As the HA is dried within the channels, it accumulates at the walls and edges of the microchannels which is clearly visible using SEM and light microscopy images (Fig. 2(A) and (C)). After washing, the HA microstructures which formed the visible features dissolved, leaving a thin layer of a physisorbed HA (Fig. 2(B)). Previously, we have demonstrated that the thickness of this physisorbed HA layer should be as small as 3 nm (Suh et al., 2004). This is confirmed in light microscopy images (Fig. 2(C) and (D)), in which visible patterns were no longer visible after rinsing.
To directly demonstrate HA patterning on the glass surface, FITC-conjugated HA was immobilized on the surface using microfluidic patterning and visualized under a fluorescent microscope. As shown by the green lanes in Fig. 2(E), HA could be directly patterned on a substrate using physisorption and remained stable after washing.
Micropatterned HA substrates were tested for their ability to resist proteins using Texas Red-conjugated BSA as well as fibronectin . As shown by the alternating red lanes in Fig. 2(F), HA was bioresistant and caused preferential adsorption of BSA to the glass substrate. Quantification of the level of protein adsorption on the surface indicated that HA-coated surfaces resisted >98% of BSA and fibronectin adsorption relative to the glass substrate.
To test the ability of the HA-coated surfaces to resist cell adhesion, cell adhesion to HA-coated surfaces was measured in the presence of serum containing medium (Figs. 2(G) and 1(H)). HA-coated surfaces and glass substrates, both of which were treated with fibronectin for 15 min were incubated with cells and analyzed after 6 hr. As can be seen in Fig. 2(G), cell adhesion on HA coated surfaces was poor as less than 1% of cells attach to these surfaces and exhibit rounded morphologies. Alternatively, cells completely coated the surface of a FN-treated glass substrate as 90% of the original cells attached with morphologies typical of fibroblasts in culture. Similar results were observed for HA and glass surfaces that were not treated with fibronectin, although the differences were less noticeable.
Spontateneous contraction of an organoid after 6 days in culture. The white line indicates a position of the landmark at the beginning of contraction. The landmark shifts downward as the organoid contracts. (A) Frame taken at t=0 (B) Frame taken at t=800 ms, when the landmark has shifted by 38 μm. Scale bar 100 μm
3.3 Cardiac organoid formation
Upon seeding of primary cardiac myocytes, cells attached preferentially to the FN-coated microlanes and the interface between the HA pattern and the FN coated glass microlanes. The cells exhibited the rounded morphology immediately after enzymatic isolation and upon seeding. Within the first 24 hr in culture, the cells present at the adhesive regions started changing their shape and elongating. The cells at the interface between the HA and FN lanes elongated significantly more than those on the FN coated glass microlanes reaching the length on the order of ∼100 μm. Thus, the HA patterns served as inductive templates for formation of cardiac organoids. Individual contractile cells were observed after 2 days in culture.
By day 3 it was obvious that the cells were exerting force as pattern narrowing was observed in some regions (Fig. 3). Elongated cardiomyocytes present at the opposing sides of the lane came in proximity to one another as a result of the microlane compression process. In addition, 67% of the pattern strands were beating, although most cardiomyocytes were attached at the surface of the substrate. The organoid formation progressed by further pattern compression and slow detachment of the 2D cardiomyocyte structures. As such, the process was similar to the recently described cardiac self-organization by spontaneous monolayer detachment (Baar et al., 2005).
By day 4, 3D cardiac organoids formed on all patterned substrates. The organoids detached and 100% of them exhibited contractile activity (Fig. 4). At day 4 in culture the average organoid diameter was 16±4 μm. The compression of the structures continued in 3D as well, as evidenced by the progressively decreasing organoid diameter. At day 6 in culture final diameter of the organoids was 10±5 μm, with the length corresponding to the length of the patterned HA lanes (∼10 mm). This cross-sectional dimension is well below oxygen diffusional limitation of ∼100 μm (Radisic et al., 2006) for the engineered cardiac tissue, indicating the organoids had sufficient oxygen and nutrient supply at all times. The cross-sectional diameter thus corresponds to the width of 2–3 individual elongated cardiac myocytes. This is a physiological situation since in the native heart elongated myofibers are supported by a dense network of capillaries, with the average inter-capillary spacing of ∼20 μm (Rakusan and Korecky, 1982).
3.4 Contractile properties
The organoids exhibited spontaneous contractility in a range of frequencies. Initially, (day 2) spontaneous contractions were present only in the individual cells. As the HA lanes compressed and cells started to contact one another, the contractions became stronger and more synchronized (day 3). In general the contractile properties improved with time of culture. The contractile activity was maintained for up to 10 days in culture at which point the experiment was terminated.
Contractile properties of cardiac muscle organoids. By Day 3 in culture most (67%) of organoids exhibited spontaneous contractile activity. At 4 Days in culture the frequency of contraction increased significantly and all observed organoids were contracting. The contractile activity was maintained throughout the period of cultivation (10 days), with reduced frequency but increased amplitude (by 7-fold) as time increased. (A) Contraction profile for a strand at Day 6 of culture. (B) Frequency of contraction (Day 3 n=4; Day 4 n=13; Day 6 n=34); (C) Contraction amplitude (n=3) (D) Duration of contraction (n=3). Statistical significance determined by One Way ANOVA in conjunction with Dunn’s test (B) and Tukey’s test (C,D), with p<0.05 considered significant
Figure 4 illustrates a contraction of an organoid after 6 days in culture. The white line indicates a position of the landmark at the beginning of contraction. As the organoid contracted the landmark moved downwards, in this case by 38 μm. Using a similar tracking procedure it was possible to determine the position of landmark for a beating sequence digitized at 25 frames per second. The amplitude of contraction was then determined as a change of landmark position in a given frame and plotted vs time. Figure 5(A) illustrates a typical contraction profile obtained by the described method for a cardiac organoid after 6 days of culture. The contraction profile was qualitatively and quantitavely (duration) comparable to those obtained previously for electrically stimulated cardiomyocyte constructs based on collagen sponges (Radisic et al., 2004a).
The contraction frequency increased significantly from day 3 to day 4 of culture, followed by the slight but significant decrease at Day 6 (Fig. 5(B)). This phenomenon was observed previously (Radisic et al., 2004b) for cardiac constructs contracting spontaneously early in culture and may be governed by the same mechanisms that governs the development of contractile properties in the fetal heart, where the frequency of contraction decreases from the fetal to neonatal stage.
The amplitude of contraction was relatively small at day 3 and day 4 of culture followed by nearly 7-fold increase at Day 6 (Fig. 5(C)). In a previous study (Radisic et al., 2004a) the progressive increase in the amplitude of contraction was correlated to the development of a functional contractile apparatus and a differentiated cardiac phenotype. The duration of contraction decreased although not significantly during the time of culture. The shortening of action potential duration is generally accepted as indication of progression towards differentiated phenotype (Bursac et al., 2003). At day 6 the duration of contraction was comparable to that measured previously for cardiac constructs cultivated in the presence of electrical stimulation (Radisic et al., 2004a).
Immunostaining demonstrated the presence of a phenotypic marker of cardiac differentiation, cardiac troponin I. The organoids consisted of elongated cells expressing cardiac troponin I (Fig. 6). Cross-striations were identified in the higher magnification images (Fig. 6, inset) indicating that the cardiomyocytes had well developed contractile apparatus.
Two advantages of the system we developed over other forms of topographical patterning are that it organizes the cells using highly biocompatible materials, and enables to readily reclaim the strands of beating cells by a natural release from the aligning substrate. Thereby, the strands are easily harvestable without the use of enzymes. This system is therefore protective for the cells and convenient for a variety of molecular and cellular studies. Moreover, the system can be scaled up to enable the formation of larger organoids.
The patterning technology presented here can be potentially applied to biodegradable tissue engineering scaffolds. To organize the cardiomyocytes within 3D scaffolds, it may be possible to incorporate patterning techniques presented here directly into the scaffold in order to align cardiomyocytes and organize the beating of the tissue. We have previously shown that HA can be patterned on a variety of hydrophilic polymers such as PLGA and poly(hydroxyethyl methacrylate) (pHEMA) (Suh et al., 2004). Therefore, it may be possible to pattern HA on these scaffolds to direct the initial organ formation within the scaffolds.
Potentially, the patterned organoids can be used as models for in vitro drug testing. The change in contractile properties with respect to the introduced drug can be studied in conjunction with the image acquisition/analysis system. The tools described here can easily be incorporated within high-throughput technologies such as microfluidics to simultaneously test many conditions. In a MEMS approach the cardiac organoids could potentially be integrated with force transducers or electrodes (Whittington et al., 2005) and serve as biosensors for compounds that affect myocardial function.
Since HA micropatterns have been used to generate patterned co-cultures using layer-by-layer deposition of ionic biopolymers (Khademhosseini et al., 2004), it is possible to study the effects of secondary cell types on cardiac muscle function. In future studies, we will further characterize the presence of cardiac markers (contractile and conductive proteins) in the cardiac organoids determine, the effect of pattern size and geometry on the organoid assembly and test contractile properties including force of contraction in response to electrical stimulation.
In conclusion, we demonstrate that 3D cardiac tissues can be formed on micropatterned substrates consisting of fibronectin and HA. Upon seeding, cardiomyocytes elongated and aligned along the interface between HA patterns and glass substrate. The organoids, detached from the glass substrate and became synchronously contractile after 3 days in culture. The approach presented here may be applicable to tissue engineering and drug discovery, where proper differentiated phenotypes of cardiac tissues are desired.
References
G. Abantangelo and P. Weigel, New frontiers in medical science: redefining hyaluronan (Elsevier, Amsterdam, 2000).
K. Baar, R. Birla, M.O. Boluyt, et al., Faseb J. 19, 275 (2005).
E.A. Balazs, Int. Ophthalmology Clinics 13, 169 (1973).
S.N. Bhatia, M.L. Yarmush, and M. Toner, J. Biomed. Mater. Res. 34, 189 (1997).
S.N. Bhatia, U.J. Balis, M.L. Yarmush, et al., Biotechnol. Prog. 14, 378 (1998a).
S.N. Bhatia, U.J. Balis, M.L. Yarmush, et al., J. Biomater. Sci. Polym. Ed. 9, 1137 (1998b).
S.N. Bhatia, U.J. Balis, M.L. Yarmush, et al., Faseb J. 13, 1883 (1999).
S.Y. Boateng, T.J. Hartman, N. Ahluwalia, et al., Am. J. Physiol. Cell Physiol. 285, C171 (2003).
P. Bulpitt and D. Aeschlimann, J. Biomed. Mater. Res. 47, 152 (1999).
N. Bursac, M. Papadaki, J.A. White, et al., Tissue Eng. 9, 1243 (2003).
R.L. Carrier, M. Papadaki, M. Rupnick, et al., Biotechnol. Bioeng. 64, 580 (1999).
C.S. Chen, M. Mrksich, S. Huang, et al., Science 276, 1425 (1997).
D.T. Chiu, N.L. Jeon, S. Huang, et al., Proc. Natl. Acad. Sci. USA 97, 2408 (2000).
J. Deutsch, D. Motlagh, B. Russell, et al., J. Biomed. Mater. Res. 53, 267 (2000).
V.G. Fast, S. Rohr, and R.E. Ideker, Am. J. Physiol. Heart Circ. Physiol. 278, H688 (2000).
A. Folch, B.H. Jo, O. Hurtado, et al., J. Biomed. Mater. Res. 52, 346 (2000).
G. Gaudesius, M. Miragoli, S.P. Thomas, et al., Circulation Res. 93, 421 (2003).
J. Hyun, H. Ma, Z. Zhang, et al., Adv. Mat. 15, 576 (2003).
J. Hyun, Y.J. Zhu, A. Liebmann-Vinson, et al., Langmuir 17, 6358 (2001).
A. Khademhosseini, K.Y. Suh, J.M. Yang, et al., Biomaterials 25, 3583 (2004).
W.G. Koh, L.J. Itle, and M.V. Pishko, Anal. Chem. 75, 5783 (2003).
R.-K. Li, T.M. Yau, R.D. Weisel, et al., J. Thoracic Cardiovasc. Surg. 119, 368 (2000).
T.C. McDevitt, J.C. Angello, M.L. Whitney, et al., J. Biomed. Mater. Res. 60, 472 (2002).
M. Morra, Biomacromolecules 6, 1205 (2005).
M. Mrksich and G.M. Whitesides, Annu. Rev. Biophys. Biomol. Struct. 25, 55 (1996).
M. Mrksich, C.S. Chen, Y. Xia, et al., Proc. Natl. Acad. Sci. USA 93, 10775 (1996).
M. Mrksich, L.E. Dike, J. Tien, et al., Exp. Cell. Res. 235, 305 (1997).
S. Murakami, S. Takayama, K. Ikezawa, et al., J. Periodontal Res. 425 (1999).
S. Oerther, H. Le Gall, E. Payan, et al., Biotechnol. Bioeng. 63, 206 (1999).
E. Ostuni, R. Kane, C.S. Chen, et al., Langmuir 16, 7811 (2000).
M. Pei, L.A. Solchaga, J. Seidel, et al., Faseb J. 16, 1691 (2002).
D. Piacquadio, M. Jarcho, and R. Goltz, J. Am. Acad. Dermatol. 36, 544 (1997).
K.L. Prime and G.M. Whitesides, Science 252, 1164 (1991).
M. Radisic, J. Malda, E. Epping, et al., Biotechnol. Bioeng. 93, 323 (2006).
M. Radisic, W. Deen, R. Langer, et al., Am. J. Physiol-Heart Circulatory Physiol. 288, H1278 (2005).
M. Radisic, M. Euloth, L. Yang, et al., Biotechnol. Bioeng. 82, 403 (2003).
M. Radisic, H. Park, H. Shing, et al., Proc. Natl. Acad. Sci. USA 101, 18129 (2004a).
M. Radisic, L. Yang, J. Boublik, et al., Am. J. Physiol.: Heart Circulatory Physiol. 286, H507 (2004b).
K. Rakusan and B. Korecky, Growth 46, 275 (1982).
S. Rohr, D.M. Scholly, and A.G. Kleber, Circ. Res. 68, 114 (1991).
E.V. Romanova, K.A. Fosser, S.S. Rubakhin, et al., Faseb J 18, 1267 (2004).
T. Shimizu, M. Yamato, Y. Isoi, et al., Circ. Res. 90, e40 (2002).
J. Sinclair and A.K. Salem, Biomaterials 27, 2090 (2006).
R. Singhvi, A. Kumar, G.P. Lopez, et al., Science 264, 696 (1994).
K.Y. Suh, A. Khademhosseini, J.M. Yang, et al., Adv. Mater. 16, 584 (2004).
S. Takayama, J.C. McDonald, E. Ostuni, et al., Proc. Natl. Acad. Sci. USA 96, 5545 (1999).
W. Tan and T.A. Desai, Tissue Eng. 9, 255 (2003).
W. Tan and T.A. Desai, Biomaterials 25, 1355 (2004).
S.P. Thomas, L. Bircher-Lehmann, S.A. Thomas, et al., Circ. Res. 87, 467 (2000).
G.M. Whitesides, E. Ostuni, S. Takayama, et al., Annu. Rev. Biomed. Eng. 3, 335 (2001).
R.H. Whittington, L. Giovangrandi, and G.T. Kovacs, IEEE Trans. Biomed. Eng. 52, 1261 (2005).
W.H. Zimmermann, K. Schneiderbanger, P. Schubert, et al., Circ. Res. 90, 223 (2002).
Acknowledgments
The authors would like to thank Lorain Chiu for immunostaining and Draper Laboratories for microfabrication. This work was supported by grants from Ontario Research and Development Challenge Fund (ORDCF), National Science and Engineering Research Council (NSERC) and Canada Foundation for Innivation (CF)) (MR) National Institutes of Health (NIH) Grant No P41 EB002520–01A1 (Tissue Engineering Resource Center, GV) R01HL076485 (GV) and NIH grants No HL060435, DE13023 and DE16516 (RL).
Author information
Authors and Affiliations
Corresponding author
Additional information
Author’s contributions: AK, RL, GV and MR designed experiments and conceived the ideas. AK, MR, GE, JY performed experiments. AK, GE and JY fabricated and analyzed the patterned substrates. SK and MR analyzed the cardiomyocyte data. All authors read and approved the final manuscript.
Rights and permissions
About this article
Cite this article
Khademhosseini, A., Eng, G., Yeh, J. et al. Microfluidic patterning for fabrication of contractile cardiac organoids. Biomed Microdevices 9, 149–157 (2007). https://doi.org/10.1007/s10544-006-9013-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10544-006-9013-7