Abstract
Objective
To investigate the roles of miR-34a in progression and chemoresistance of glioma cells.
Results
Quantitative real-time PCR analysis showed that miR-34a level was lower, but PD-L1 expression level was higher in glioma tissue specimens compared with normal brain tissues and their expression levels were negatively correlated. Ectopic expression of miR-34a inhibited glioma cell proliferation, promoted cell cycle arrest in G1/S phase and cell apoptosis. Additionally, miR-34a/PD-L1 axis was again confirmed and co-expression of PD-L1 with miR-34a mimics attenuated the effects of miR-34a on cell proliferation and apoptosis in glioma cells. Importantly, PD-L1 overexpression resulted in chemoresistance in glioma cells, this effect was attenuated by miR-34a overexpression.
Conclusions
miR-34a inhibits glioma cells progression and chemoresistance via targeting PD-L1.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Malignant glioma is a highly aggressive cancer associated with low survival rate (Zhang et al. 2017). Paclitaxel is one of the most effective anticancer agents available clinically. It has a wide spectrum of activity against solid tumors, including brain glioma, which are treated with paclitaxel alone or in combination with other chemotherapeutic agents (Pessina et al. 2011). However, chemoresistance is the main obstacle for glioma treatment (Kessler et al. 2015). Therefore, there is a need to find new targets or novel therapeutic modalities for glioma patients.
One of the most inspiring recent progresses in cancer therapy is the development of immune checkpoint inhibitors, such as Ipilimumab targeting CTLA-4 (cytotoxic T-lymphocyte-associated protein 4) and Pembrolizumab targeting the Programmed Death 1 (PD-1; CD279) molecule. These two immune checkpoint blockade inhibitors are approved for the treatment of cancers, such as advanced melanoma, renal carcinoma, non-small cell lung cancer, Hodgkin’s lymphoma, and others (Sagiv-Barfi et al. 2015).
PD-L1, the ligand of PD-1, has distinct expression profiles with PD-1 in several tumor types (Bozeman et al. 2016). Importantly, the inhibitor of PD-L1 has been approved for the treatment of non-small cell lung cancer and bladder cancer by US FDA (Feld and Horn 2016; Tsao et al. 2017). PD-L1 serves as a prognostic marker in local advanced breast cancer and lung cancer after neoadjuvant chemotherapy (Chen et al. 2017; Teng et al. 2016). PD-L1 is highly expressed in human glioma and its level is positively correlated with the grade of glioma (Zhang et al. 2017). However, the relationship between PD-L1 expression and chemotherapy is poorly revealed in glioma.
Here, we report that miR-34a level is downregulated in glioma tissues compared with the normal brain tissues, and this negatively correlates with PD-L1 expression. Additionally, PD-L1 expression was significantly increased in paclitaxel-resistant glioma cells, while miR-34a level was downregulated. Furthermore, PD-L1 was identified as a potential target of miR-34a in glioma cells, and upregulation of miR-34a enhanced paclitaxel sensitivity of glioma cells. Moreover, overexpression of PD-L1 in glioma cells decreased the paclitaxel sensitivity of glioma cells, this effect was attenuated by miR-34a overexpression. Our results reveal a potential involvement of the miR-34a/PD-L1 axis in paclitaxel resistance and progression of glioma.
Materials and methods
Tissue samples and cell culture
Written informed consent was obtained from the patients for the publication of this report and any accompanying images. This study was performed with the approval of the Ethics Committee of the Cangzhou Central Hospital. Methods were performed in accordance with the approved guidelines. 21 clinical glioma samples were collected randomly from patients immediately after surgical resection at the Neurosurgery Department of the Third Hospital of Hebei Medical University from 2014 to 2017. The mean age of the patients was 48.5 years (range 5–76 years), and the patient cohort included 14 men and 7 women. Human glioma cell lines U251 and U87-MG were purchased from the cell bank of Chinese Academy of Sciences (Shanghai, China) and cultured in DMEM medium containing 10% (v/v) FBS and 1% penicillin/streptomycin at 37 °C under humidified atmosphere with 5% CO2. Paclitaxel-resistant cells (U87-P) were developed by culturing paclitaxel-sensitive U87 cells in a gradually increasing concentration of paclitaxel (The Third Affiliated Hospital of Hebei Medical University) up to 2 μM for more than 6 months. The normal concentration of paclitaxel used is 30 nM which is referred to in a previous study (Zhou et al. 2017) and is its IC50 value.
Lentivirus plasmids and transfection
We thanked for OBiO Inc. for constructing the PD-L1 overexpression (LV-PD-L1) and knockdown (LV-PD-L1-shRNA) lentivirus vectors, these vectors were verified by DNA sequencing. For miRNA target validation, the fragment of PD-L1 3′UTR containing the wild-type or the mutant binding sites for miRNA-34a was introduced into pMIR-Report vector and named Luc-PD-L1-WT and Luc-PD-L1-MUT, respectively.
MTT assay
MTT assay was utilized to examine whether miR-34a could ameliorate the resistance of paclitaxel in glioma cells. Cells, transfected with miR-34a mimics or inhibitor, were seeded in 96-well plates at 5000/well and grown overnight. Cells were then treated with paclitaxel. 48 h later, 20 μl MTT (5 mg/ml) was added to each well and incubated for 4 h. The medium was removed and 150 μl DMSO was added to dissolve the purple formazan crystals. The absorbance at 570 nm was measured with a microplate reader.
Quantitative real-time PCR (qRT-PCR)
Total RNA was extracted with TRIzol. The first-strand cDNA was reverse transcribed using oligo(dT) primers and M-MLV reverse transcriptase (Promega, USA). qRT-PCR was carried out with SYBR Green master mix (Biomics, China) on an StepOne Plus real-time PCR Detector (Applied Biosystems, USA). GAPDH served as an internal control. Relative quantification was conducted using the \( 2^{{ - \Delta \Delta {\text{C}}_{\text{t}} }} \) method. For miRNA qRT-PCR, cDNA was synthesized using a microRNA reverse transcription kit (GenePharma, China) with miR-34a- and U6-specific primers (GenePharma, China) according to the manufacturer’s instructions. The level of miR-34a was normalized to U6. For all cases, relative quantification was conducted using the \( 2^{{ - \Delta \Delta {\text{C}}_{\text{t}} }} \) method.
Western blotting
Cells were lysed with RIPA and quantified by a BCA protein assay kit. Equal amounts of protein were separated by 10% SDS-PAGE and electrotransferred onto PVDF membranes. The membranes were blocked with 5% (v/v) non-fat milk at room temperature for 1 h. The membranes were subsequently incubated with primary antibodies at 4 °C overnight. After washing three times in TBST, the membranes were blotted with the corresponding secondary antibodies and developed with an ECL kit (Thermo Fisher, USA). β-Actin was used as an internal control.
Luciferase report assay
For miRNA target validation, U251 and U87-MG cells were seeded in 24-well plates at 8 × 104 per well and co-transfected with Luc-PD-L1-WT or Luc-PD-L1-MUT and miR-34a mimics or NC. The cells were lysed and luciferase activity was detected with a luminometer 48 h later. β-Gal was employed to normalize the Fluc values expressed from the pMIR-Report constructs.
RNA-immunoprecipitation (RIP) analysis
Cells were lysed on ice 48 h after transfection with Luc-PD-L1-WT plasmid, and RIPs were performed as previously described (Tay et al. 2011). Briefly, cell lysates were incubated overnight at 4 °C with control rabbit IgG (Jackson ImmunoResearch) or anti-Ago2 antibody that were bound to Protein A-Sepharose beads (Sigma). Beads were then washed five times with NT2 buffer, and RNA was eluted by incubation with SDS-TE buffer by heating at 55 °C for 30 min. RNA was then precipitated using the standard Trizol protocol, reverse transcribed and analyzed via qRT-PCR.
Annexin V/PI apoptosis assay
The apoptotic cells were determined by the Annexin V-FITC Apoptosis Detection Kit (Beyotime, China) according to the manufacturer’s protocol. Cells were collected 48 h after transfection and washed twice with cold PBS. Then cells were resuspended in binding buffer containing 5 µl annexin V-FITC and 5 µl PI for 10 min in the dark at room temperature and followed by flow cytometric measurement at 488 nm excitation.
Cell cycle assay
The cells were stained by a cell cycle detection kit (KeyGen BioTech, Nanjing, China) following the manufacturer’s protocols. Briefly, cells (5 × 105/well) were seeded in six-well plates and serum-starved for 24 h to synchronize into the G0 phase of cell cycle. Cells were then transfected with miR-34a mimics for 48 h, washed twice with ice-cold PBS, centrifuged and fixed in ice-cold 75% (v/v) ethanol for 1 h at 4 °C. After that, cells were suspended in PI (50 µg/ml) with ribonuclease A (RNase A) (0.1 mg/ml) for 30 min in the dark. Cell cycle distribution was assessed using a flow cytometer.
Statistical analysis
Data were presented as the mean ± SD. Statistical comparisons of multiple groups were performed with a one-way ANOVA and p value of less than 0.05 was considered as significant.
Results
Overexpression of PD-L1 induces paclitaxel resistance in glioma cells
The sensitivity of paclitaxel in U87-P and U87 cells, was determined; paclitaxel significantly decreased the cell viability of U87 cells but had little effect on U87-P cells (Fig. 1a). Then the expression level of PD-L1 was examined in U87-P and U87 cells. As shown in Fig. 1b, PD-L1 expression was increased in U87-P cells. Thus we speculate that PD-L1 overexpression could induce paclitaxel resistance in glioma cells. As expected, U87 cells infected with LV-PD-L1 showed lower sensitivity of paclitaxel characterized as increased cell proliferation, decreased cell apoptosis with paclitaxel treatment (Fig. 1c, d). Knockdown of PD-L1 in U87-P cells, however, increased paclitaxel sensitivity (Fig. 1e, f). Therefore, our results demonstrate that PD-L1 overexpression induces paclitaxel resistance in glioma cells.
Overexpression of PD-L1 induced paclitaxel resistance in glioma cells. a The cell viability of U87 and U87-P cells was assessed after paclitaxel treatment. b The mRNA and protein levels of PD-L1 were examined in U87 and U87-P cells via qRT-PCR and western blot analyses. c Overexpression of PD-L1 conferred paclitaxel resistance in U87 cells. d U87 cells were infected with LV-PD-L or not and followed by paclitaxel treatment, then the cell apoptosis was examined. e, f U87-P cells were infected with LV-PD-L1-shRNA and followed by paclitaxel treatment, then the cell viability and apoptosis were examined. Data were presented as the mean ± SD; **P < 0.01 versus control
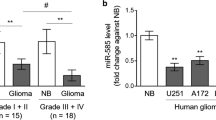
miR-34a is downregulated and negatively correlates with PD-L1 expression in glioma samples
qRT-PCR was performed to examine the levels of miR-34a and PD-L1 in glioma tumor and adjacent normal brain tissues. miR-34a was downregulated in glioma tumors compared with the normal adjacent tissues (Fig. 2a). In contrast, PD-L1 expression level was higher in glioma tumors (Fig. 2b). In addition, miR-34a level was negatively correlated with PD-L1 expression in glioma tissues (Fig. 2c). Moreover, miR-34a level was downregulated in U87-P cells (Fig. 2d) and transfection with miR-34a mimics attenuated the paclitaxel resistance in U87-P cells, characterized as decreased cell proliferation (Fig. 2e) and increased cell apoptosis (Fig. 2f). The transfection efficiency of miR-34a mimics in U87-P cells was denoted in Fig. 2g. These results indicate that miR-34a might hold a suppressive role in cell progression and chemoresistance in glioma tumors, which is correlated with PD-L1 expression.
miR-34a is downregulated and negatively correlated with PD-L1 expression in glioma samples. a, b The expression levels of miR-34a and PD-L1 were detected in normal brain and glioma tissues via qRT-PCR assay. c Correlation between the levels of miR-34a and PD-L1 in glioma tissues. d, e U87-P cells were transfected with miR-34a mimics or not and followed by paclitaxel treatment, cell viability (d) and cell apoptosis (e) were determined. f The transfection efficiency of miR-34a in U87-P cells was evaluated by qRT-PCR analysis. Data were presented as the mean ± SD; **P < 0.01 versus control
Effects of miR-34a on glioma cell proliferation, cell cycle and apoptosis
We continue investigating whether miR-34a holds a suppressive role in glioma cell progression. Transfection with miR-34a mimics significantly upregulated miR-34a level in U87 and U251 cells (Fig. 3a). Cell viability assay showed that upregulation of miR-34a level blocked cell proliferation in glioma cells (Fig. 3b, c). Additionally, the cell cycle assay indicated that ectopic expression of miR-34a promoted cell cycle arrest in G1/S phase (Fig. 3d). And miR-34a overexpression enhanced cell apoptosis in U87 and U251 cells (Fig. 3e).
Effects of miR-34a on glioma cell proliferation, cell cycle and apoptosis. a The transfection efficiency of miR-34a was determined in U87 and U251 cells via qRT-PCR assay. b–e U87 and U251 cells transfected with miR-34a mimics were applied to analyze cell viability (b and c), cell cycle (d) and cell apoptosis (e). Data were presented as the mean ± SD; **P < 0.01 versus control
PD-L1 is a target of miR-34a in glioma cells
PD-L1 was identified as a potential target of miR-34a in acute myeloid leukemia (Wang et al. 2015). We investigated whether miR-34a/PD-L1 regulatory route did exist in glioma cells. Luciferase reporter analysis showed that co-transfection of U87 and U251 cells with miR-34a mimics and the Luc-PD-L1-WT construct led to a significant reduction in luciferase activity compared with NC (Fig. 4a). Conversely, the activity in Luc-PD-L1-MUT was unaffected by miR-34a upregulation, suggesting that PD-L1 is a direct target of miR-34a in glioma cells. qRT-PCR and western blot experiments further confirmed that upregulation of miR-34a level significantly decreased PD-L1 expression in glioma cells (Fig. 4b, c). Additionally, we performed RIP to confirm the physical association between miR-34a and PD-L1 3′UTR. RIP for PD-L1 3′UTR in U87 and U251 cells significantly enriched for miR-34a compared to empty vector and IgG controls (Fig. 4d). In summary, we confirm that PD-L1 is a direct target of miR-34a in glioma cells.
PD-L1 is a target of miR-34a in glioma cells. a U87 and U251 cells were co-transfected with Luc-PD-L1-WT or Luc-PD-L1-MUT, miR-34a mimics and β-gal control plasmid for 48 h, then luciferase activity was measured and normalized to β-gal activity. b, c qRT-PCR and western blot results of PD-L1 in U87 and U251 cells after transfection of miR-34a mimics for 48 h. d qRT-PCR was used to measure the level of enrichment of miR-34a in the anti-Ago2-immunoprecipitated complexes in U87 and U251 cells with Luc-PD-L1-WT transfection. Data were presented as the mean ± SD; **P < 0.01 versus control
miR-34a counteracts the effects of PD-L1 overexpression in glioma cells
We investigated whether miR-34a exerted its functional effects dependent on PD-L1 expression and attenuated the effects of PD-L1 overexpression. Firstly, as we have indicated the inhibitory roles of miR-34a in progression of glioma cells, we needed to confirm whether PD-L1 holds an opposite effect. As expected, knockdown of PD-L1 inhibited cell proliferation (Fig. 5a, b) and promoted cell apoptosis (Fig. 5c) in glioma cells. LV-PD-L1 was then co-infected with miR-34 mimics transfection in U87 and U251 cells. As shown in Fig. 5d–f, overexpression of PD-L1 counteracted the inhibitory effects of miR-34 on cell proliferation and the promotive effects on cell apoptosis. Furthermore, co-transfection of miR-34a mimics with LV-PD-L1 infection attenuated the inductive effects of PD-L1 overexpression on paclitaxel resistance in U87 cells (Fig. 5g, h). Therefore, these results demonstrate that miR-34a exerts its inhibitory effects on glioma cell progression partly dependent on PD-L1 expression.
miR-34a counteracted the effects of PD-L1 overexpression in glioma cells. a, b U87 and U251 cells were infected with LV-PD-L1-shRNA or not, then the cell viability was examined by MTT assays. c The crucial executioner of cell apoptosis (cleaved caspase-3) protein level was evaluated in cells depicted in (a, b). d, e U87 and U251 cells were transfected with miR-34a mimics plus LV-PD-L1 infection, then the cell viability was examined by MTT assays. f The crucial executioner of cell apoptosis (cleaved caspase-3) protein level was evaluated in cells depicted in (d, e). g U87 and U2511 cells were infected with LV-PD-L1 plus miR-34a mimics or not and followed by the treatment of paclitaxel, then the cell viability was examined by MTT assay. h The crucial executioner of cell apoptosis (cleaved caspase-3) protein level was evaluated in cells depicted in (g). Data were presented as the mean ± SD; **P < 0.01 versus control
Discussion
miR-34a plays an inhibitory role in glioma stem cells (Sun et al. 2012). Its level correlates with glioma grade and prognosis (Gao et al. 2013). In this study, we demonstrate that the functional roles of miR-34a are correlated with PD-L1 expression in glioma cells, characterized as decreased cell proliferation and increased cell apoptosis, and even the chemoresistance.
PD-L1 is involved in tumor immune therapy; however, it is still unclear whether PD-L1 expression is associated with chemoresistance in glioma cells. Here, we found that PD-L1 expression level was upregulated in U87-P cells and overexpression of PD-L1 conferred paclitaxel resistance in U87 cells, while knockdown of PD-L1 attenuated the chemoresistance in U87-P cells. These results indicate that PD-L1, except for modulating the immune therapy via PD-1/PD-L1 pathway, could still contribute to drug resistance in glioma cells. As miR-34a can target PD-L1 in acute myeloid leukemia (Chen et al. 2016; Wang et al. 2015) and non-small cell lung cancer (Cortez et al. 2016), we speculate that the miR-34a/PD-L1 regulatory route might be a universal phenomenon in tumors, which should be confirmed with further experiments.
Although immune therapy has not been used to treat glioma, combined therapeutic methods with PD-L1 antibody have given encouraging results. For example, immunovirotherapy with measles virus strains in combination with anti-PD-1 antibody blockade enhanced antitumor activity in glioblastoma treatment (Hardcastle et al. 2016), and non-tumor cell IDO1 predominantly contributes to enzyme activity and response to CTLA-4/PD-L1 inhibition in mouse glioblastoma (Zhai et al. 2017). Individual immune response to cancer immunotherapy often rely on tumor immunogenicity that varies extensively between different cancer types and different individuals; therefore, immune checkpoint inhibitors may not work in cases where tumor immunogenicity is intrinsically limited (Moroishi et al. 2016; Ock et al. 2016).
Based on our results, we strongly believe that a combination of miR-34a and immune checkpoint inhibitors would be a novel and exciting therapeutic approach for glioma. As the miR-34a/PD-L1 pathway is universal, miR-34a may enhance tumor immunity in most cancer types. However, the caveat remains that our results have been acquired by in vitro experiments, which is different from the in vivo environment. Whether our in vitro findings can directly be translated to in vivo remains to be determined. Moreover, the effect of miR-34a inhibition as an intervention for established tumors needs to be explored. Nevertheless, future studies expanding the therapeutic potentials of miR-34a/PD-L1 pathway will have important clinical implications.
Change history
10 January 2023
This article has been retracted. Please see the Retraction Notice for more detail: https://doi.org/10.1007/s10529-023-03344-4
References
Bozeman EN, He S, Shafizadeh Y, Selvaraj P (2016) Therapeutic efficacy of PD-L1 blockade in a breast cancer model is enhanced by cellular vaccines expressing B7-1 and glycolipid-anchored IL-12. Hum Vaccin Immunother 12:421–430
Chen J, Jiang CC, Jin L, Zhang XD (2016) Regulation of PD-L1: a novel role of pro-survival signalling in cancer. Ann Oncol 27:409–416
Chen S, Wang RX, Liu Y, Yang WT, Shao ZM (2017) PD-L1 expression of the residual tumor serves as a prognostic marker in local advanced breast cancer after neoadjuvant chemotherapy. Int J Cancer 140:1384–1395
Cortez MA, Ivan C, Valdecanas D, Wang X, Peltier HJ, Ye Y, Araujo L, Carbone DP, Shilo K, Giri DK et al (2016) PDL1 regulation by p53 via miR-34. J Natl Cancer Inst. doi:10.1093/jnci/djv303
Feld E, Horn L (2016) Targeting PD-L1 for non-small-cell lung cancer. Immunotherapy 8:747–758
Gao H, Zhao H, Xiang W (2013) Expression level of human miR-34a correlates with glioma grade and prognosis. J Neurooncol 113:221–228
Hardcastle J, Mills L, Malo CS, Jin F, Kurokawa C, Geekiyanage H, Schroeder M, Sarkaria J, Johnson AJ, Galanis E (2016) Immunovirotherapy with measles virus strains in combination with anti-PD-1 antibody blockade enhances antitumor activity in glioblastoma treatment. Neuro Oncol 19:493–502
Kessler T, Sahm F, Blaes J, Osswald M, Rubmann P, Milford D, Urban S, Jestaedt L, Heiland S, Bendszus M et al (2015) Glioma cell VEGFR-2 confers resistance to chemotherapeutic and antiangiogenic treatments in PTEN-deficient glioblastoma. Oncotarget 6:31050–31068
Moroishi T, Hayashi T, Pan WW, Fujita Y, Holt MV, Qin J, Carson DA, Guan KL (2016) The hippo pathway kinases LATS1/2 suppress cancer immunity. Cell 167(1525–1539):e1517
Ock CY, Kim S, Keam B, Kim M, Kim TM, Kim JH, Jeon YK, Lee JS, Kwon SK, Hah JH et al (2016) PD-L1 expression is associated with epithelial-mesenchymal transition in head and neck squamous cell carcinoma. Oncotarget 7:15901–15914
Pessina A, Bonomi A, Cocce V, Invernici G, Navone S, Cavicchini L, Sisto F, Ferrari M, Vigano L, Locatelli A et al (2011) Mesenchymal stromal cells primed with paclitaxel provide a new approach for cancer therapy. PLoS ONE 6:e28321
Sagiv-Barfi I, Kohrt HE, Czerwinski DK, Ng PP, Chang BY, Levy R (2015) Therapeutic antitumor immunity by checkpoint blockade is enhanced by ibrutinib, an inhibitor of both BTK and ITK. Proc Natl Acad Sci USA 112:E966–E972
Sun L, Wu Z, Shao Y, Pu Y, Miu W, Yao J, Wu Y, Yang Z (2012) MicroRNA-34a suppresses cell proliferation and induces apoptosis in U87 glioma stem cells. Technol Cancer Res Treat 11:483–490
Tay Y, Kats L, Salmena L, Weiss D, Tan SM, Ala U, Karreth F, Poliseno L, Provero P, Di Cunto F et al (2011) Coding-independent regulation of the tumor suppressor PTEN by competing endogenous mRNAs. Cell 147:344–357
Teng F, Meng X, Wang X, Yuan J, Liu S, Mu D, Zhu H, Kong L, Yu J (2016) Expressions of CD8 + TILs, PD-L1 and Foxp3 + TILs in stage I NSCLC guiding adjuvant chemotherapy decisions. Oncotarget 7:64318–64329
Tsao MS, Le Teuff G, Shepherd FA, Landais C, Hainaut P, Filipits M, Pirker R, Le Chevalier T, Graziano S, Kratze R et al (2017) PD-L1 protein expression assessed by immunohistochemistry is neither prognostic nor predictive of benefit from adjuvant chemotherapy in resected non-small cell lung cancer. Ann Oncol 28:882–889
Wang X, Li J, Dong K, Lin F, Long M, Ouyang Y, Wei J, Chen X, Weng Y, He T et al (2015) Tumor suppressor miR-34a targets PD-L1 and functions as a potential immunotherapeutic target in acute myeloid leukemia. Cell Signal 27:443–452
Zhai L, Ladomersky E, Dostal CR, Lauing KL, Swoap K, Billingham LK, Gritsina G, Wu M, McCusker RH, Binder DC et al (2017) Non-tumor cell IDO1 predominantly contributes to enzyme activity and response to CTLA-4/PD-L1 inhibition in mouse glioblastoma. Brain Behav Immun 62:24–29
Zhang X, Zhu S, Li T, Liu YJ, Chen W, Chen J (2017) Targeting immune checkpoints in malignant glioma. Oncotarget 8:7157–7174
Zhou C, Cheng H, Qin W, Zhang Y, Xiong H, Yang J, Huang H, Wang Y, Chen XZ, Tang J (2017) Pygopus2 inhibits the efficacy of paclitaxel-induced apoptosis and induces multidrug resistance in human glioma cells. Oncotarget 8:27915–27928
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Wang, Y., Wang, L. RETRACTED ARTICLE: miR-34a attenuates glioma cells progression and chemoresistance via targeting PD-L1. Biotechnol Lett 39, 1485–1492 (2017). https://doi.org/10.1007/s10529-017-2397-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10529-017-2397-z