Abstract
The concentration of cardiac troponin I (cTnI) in blood is an important marker for heart muscle cell damage. A surface plasmon resonance (SPR)-based immunosensor was devised for the rapid and specific detection of cTnI. It was constructed by crosslinking a monoclonal antibody P-II-13, which was generated against a loop region (aa 84–94) of cTnI protein as an epitope peptide, onto a chemically modified thin gold film. The performance of the sensor was examined with respect to the SPR signal intensity versus cTnI concentration. The signal intensity was directly correlated with the cTnI concentration in the range of 0–160 μg/l. The sensor signal was saturated when the concentration of cTnI approached 660 μg/l with the SPR intensity of 172 RU. The lower detection limit of the sensor was 68 ng/l cTnI, which was comparable to ELISA-based commercial cTnI detection systems.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myocardial infarctions, also known as heart attacks, are caused by the blockage of blood flow to the heart, which results in damage of the heart muscle cells. Biochemical diagnosis of heart muscle damage, an indication of myocardial infarction, has been facilitated by measuring the blood levels of cardiac markers such as cardiac troponin I or T (cTnI or cTnT), creatine kinase-MB, lactate dehydrogenase, and myoglobin (Akhar 2003; Alpert et al. 2000). cTnI, a component of troponin involved in the regulation of cardiac muscle contraction (Zot and Potter 1987), is of particular interest because of its near-absolute myocardial tissue specificity (Alpert et al. 2000). cTnI, together with the troponin components cTnT and cTnC, is released into the bloodstream upon degradation of the contractile apparatus to which it is attached (Jaffe et al. 2000; Katrukha et al. 1997). Therefore, the plasma level of cTnI is one of the most specific and sensitive markers of acute myocardial infarction (AMI) and perioperative myocardial infarction (Adams et al. 1993, 1994).
Assays of cTnI have been facilitated by various forms of enzyme-linked immunosorbent assay (ELISA) systems, detection limits range 6–40 ng/l, depending on detection method and antibody performance (Tate 2008). Although ELISA-based assays can detect cTnI, they are time-consuming and laborious. They involve multiple laboratory processes with adequate instrumentations. As a result, they cannot be performed near the site of patient care (i.e., point-of care test), or in situations when a prompt diagnosis is required. Biosensors with microfabrication technology have been sought to overcome such limitations (Christenson and Azzazy 2009; McDonnell et al. 2009). The biosensors developed thus far have consisted essentially of the binding antibody and the labeled-capture antibody with different detection methodologies, including electrochemistry (Abbott i-Stat), fluorescence (Biosite Triage), or Ab-labeled gold nanoparticle (Roche cardiac reader) (Christenson and Azzazy 2009). Their detection limits range from 20 to 190 ng/l.
Surface plasmon resonance (SPR) has emerged as a new optical detection component of biosensors (Baac et al. 2006; Boltovets et al. 2004; Kim et al. 2008a). SPR detects the binding of protein molecules on to a metal surface by measuring changes in the index of refraction upon adsorption (Karlsen et al. 1995; Liedberg et al. 1993). It enables rapid detection of unlabeled proteins with a simple optical apparatus (Homola 2003), making SPR an ideal detection system for POCT devices. Accordingly, this study focused on the development of an immunobiosensor for rapid detection of cTnI using the SPR technique.
Materials and methods
Design of peptide antigen for anti-cTnI monoclonal antibody generation
Two immunogenic regions of cTnI are frequently utilized epitopes in cTnI (James et al. 2006; Takeda et al. 2003; Tate 2008): aa 41–49, which is located at the N-terminal part of the first α-helix, and aa 87–91, which is the loop region between the first and the second α-helices. The former is located in the vicinity of the cTnI–cTnC interaction site and the latter is located on the side opposite the first α-helix and is close to the cTnI–cTnT interaction site. To generate monoclonal antibodies (MAbs) against cTnI, the following two peptides were designed. Peptide I spans residues 41–50 and has the amino acid sequence of CSASRKLQLK-NH2. Peptide II spans residues 84–94, extends over the end of the second loop and the start of the second helix, and has the amino acid sequence of CELTGLGFAELQ-NH2. The N-terminal Cys was included for cross-linking the peptide onto a carrier protein.
Preparation of peptide antigen
The epitope peptides were chemically synthesized and cross-linked to the keyhole limpet hemocyanin protein (KLH), a widely employed carrier protein for the generation of antibodies (Lateef et al. 2007). Briefly, 10 mg KLH (Pierce, USA) were dissolved in 1 ml 10 mM potassium phosphate buffer (pH 7.0). KLH was activated by adding 100 μl of m-maleimidobenzoic acid N-hydroxysuccinimide ester (MBS, 15 mg/ml in DMF). The mixture was incubated for 1 h at 25°C with stirring and the free MBS was removed by PD-10 column (Pierce). The activated KLH was diluted to 1 mg/ml with deionized water. To cross-link the peptide, 1 ml activated KLH was mixed with 100 μl peptide solution (50 mg/ml DMF, pH 7.0). The mixture was incubated overnight at 4°C and the reaction was stopped by the addition of 3 ml of 0.1 M (NH4)HCO3.
Generation of hybridoma cells and the production of monoclonal antibody
To generate hybridoma cells producing anti-cTnI MAb, 0.2 mg of the peptide-KHL was injected into a female Balb/c mouse. An equal quantity of the peptide-KHL was injected with Freund’s incomplete adjuvant (Sigma) after 3 weeks. Immunization was confirmed by ELISA test with 50 μl of blood taken from the mouse. Finally, the peptide-KHL in phosphate-buffered saline (PBS: 8 g NaCl/l, 0.2 g KCl/l, 1.44 g Na2HPO4/l, and 0.24 g KH2PO4) was injected after an additional 3 weeks. When the production of antibody was confirmed, spleen cells from the immunized mouse were collected and fused with myeloma cells to generate the hybridoma cells. The hybridoma cells (384 cell lines) were distributed in four 96-well culture plates and cultured for 10 days.
For the production of MAb, 1 ml pristane was injected into a 5-week-old Balb/c mouse. Hybridoma cells (107 cells) were injected 1 week later. Ascites of the mouse were collected 2 weeks after the cell injection and centrifuged at 3,000×g for 30 min. The MAb in the supernatant was precipitated with 50% (NH4)2SD4. The resulting precipitate was dissolved in PBS and the solution was dialyzed against PBS overnight.
Protein chip fabrication and screening of MAb
A protein chip technique was employed for the final screening of the MAbs as previously described (Kim et al. 2008b). To generate the protein chip surface, ovalbumin (OVA, 1 mg/ml) was layered on to an aldehyde-modified slide glass (NuriCell, Korea). Subsequently, the bound OVA was activated with MBS as described above. Epitope peptides were coupled by layering 100 μl peptide solution (1 mg/ml) onto the activated OVA surface for 4 h at room temperature. To screen the MAb specific for cTnI, the ELISA-screened culture supernatants of hybridoma cells were mixed with PBS containing 20% (v/v) glycerol at 1:1 and 4 nl was spotted on to the epitope-OVA coupled slide using a protein arrayer (Proteogen, Korea). Each spot was 0.3 mm wide. The slide was incubated for 1 h at 25°C at 80% humidity and then washed with PBS containing 0.1% Tween 80. Detection of the bound MAb was facilitated using Alexa 488-goat anti-mouse IgG (5 μg/ml, Invitrogen). The fluorescence intensity of each spot was analyzed with a microarray scanner.
Surface plasmon resonance (SPR) analysis
Performance of the generated MAb was analyzed using a surface plasmon resonance (SPR) system (K-MAC micro SPR model, Korea). The selected MAb (P-II-13) solution (1 mg/ml) in PBS buffer (pH 7.0) was introduced onto a NHS gold chip (K-MAC), which can couple with free amine groups in a target protein, at 40 μl/min. The unreacted chip surface was blocked with bovine serum albumin (1 mg/ml). When the chip was ready, 100 μl cTnI of varying concentrations was introduced and the SPR signal intensity was determined. cTnI in human serum was analyzed using the same procedure. Human sera subjected to the SPR analysis were acquired from the National Biobank of Korea in Gyeongsang National University Hospital.
Results and discussion
Primary screening of monoclonal antibody
Culture supernatants from 384 hybridoma cell cultures for each epitope were subjected to ELISA assay using the epitope peptide-KLH-coated 96-well plates. Sixteen supernatants from the peptide II-immunized hybridoma cell lines showed strong anti-cTnI MAb positive wells. Cells from the positive wells were cloned. Finally, 17 positive hybridoma cell lines, which produced MAbs against the cTnI epitope peptide II, were obtained (Fig. 1). Cell lines generated by the peptide I-immunized hybridoma cell lines bound the carrier KLH protein not the epitope peptide I (Fig. 1).
Primary screening of hybridoma cell lines producing MAb against the epitope peptides. The hybridoma cell lines P-I-1–P1-6 and P-II-1–P-II-17 were generated by the immunization of mice with the epitope peptide P-I-KLH and the epitope peptide P-II-KLH, respectively. The culture supernatants of the hybridoma cells were subjected to ELISA analysis against KLH (grey bar), Peptide I-KLH (white bar), and Peptide II-KLH (black bar). PBS was used as a control
Protein array screening of anti-cTnI MAb
To screen the MAbs further, the supernatants from each hybridoma cell line were spotted onto the peptide I- and peptide II-OVA-layered slides. The peptides were cross-linked to ovalbumin (OVA) and not to KLH so that MAb binding to the carrier protein KLH could be eliminated. Bound MAb was detected with Alexa 488-linked anti-mouse IgG. The MAbs generated by peptide I were not able to bind to the chip surface coated with either peptide I or peptide II (Fig. 2a and the spots from P-I-1 to P-I-6 in Fig. 2b), confirming that the high ELISA readings of the MAbs P-I-1–P-I-6 (Fig. 1) were from the KLH binding. The MAbs generated by peptide II (MAb P-II-1–P-II-17) were mostly specific to the epitope peptide II. They did not show any significant fluorescence intensity on the peptide I-layered chip surface but showed intense fluorescence from the spots on the peptide II-layered chip surface (Fig. 2b). The digitized fluorescence intensity data indicated that the MAb P-II-13 were most specific (Fig. 2c). Immunoblot analysis of cTnI, peptide I, and peptide II with the MAb P-II-13 containing culture supernatant demonstrated that the MAb was specific for cTnI and peptide II but not for the peptide I (Fig. 2d).
Protein chip-based screening of MAb-producing hybridoma cell lines. The epitope peptides were cross-linked to ovalbumin (OVA). The peptide I-OVA and peptide II-OVA were chemically coupled to an aldehyde-coated glass chip. The culture supernatants of the hybridoma cell lines (shown in the Fig. 1) were spotted onto the peptide I-OVA-layered chip (a) or the peptide II-OVA-layered chip (b). The bound MAb was detected with Alexa 488-linked anti mouse IgG. The fluorescence intensity of each spot was digitized (c). The specificity of the selected MAb (the culture supernatant of hybridoma cell P-II-13) was confirmed by immunoblot analysis against KLH, Peptide I-KLH (P-I-KLH), Peptide II-KLH (P-II-KLH), and troponin I (cTnI). Each lane contained 5 μg corresponding protein (see ponceau stain)
Preparation of MAb P-II-13 and the construction of SPR biosensor
MAb P-II-13 was produced in mouse ascites by injecting the corresponding hybridoma cells. The ascites were concentrated by (NH4)2SO4 precipitation. The major protein component of the precipitates was MAb P-II-13 (lane 2, Fig. 3a). Subsequent densitometer analysis revealed that 60% of the protein was MAb. The final yield of MAb production was approx. 1 mg per mouse. To construct an SPR biosensor, the MAb was adsorbed on to the surface of the NHS gold chip by injecting 100 μl of the MAb solution at a flow rate of 40 μl/min. The SPR angle shift was then monitored for 8 min (Fig. 3b). The MAb binding resulted in a SPR angle shift of 1,680 RU, which corresponds to the binding of 1,680 pg protein per 1 mm2 chip surface. Because 60% of the protein in the solution was MAb P-II-13, the final amount of bound MAb P-II-13 was 1,008 pg/mm2 or 6.72 × 10−3 pmol/mm2.
Preparation of MAb P-II-13 and its binding to a surface plasmon resonance (SPR) biosensor chip. a Preparation of MAb P-II-13. MAb P-II-13 was produced from mouse ascites after injection of the corresponding hybridoma cells. The MAb was concentrated by the ammonium sulfate precipitation of the ascites solution. Lane M; size marker, lane 1; mouse ascites with hybridoma cells, lane 2; prepared MAb. H and L indicate heavy and light chains of MAb, respectively. b Binding of MAb P-II-13 on the surface of the modified gold thin film. The MAb (1 mg/ml PBS) was injected on to the gold thin film with a flow rate of 40 μl/min
SPR biosensor analysis
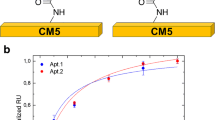
We then investigated the detection of cTnI by the MAb P-II-13-layered SPR biosensor. cTnI solutions, ranging from 150 ng/l to 660 μg/l, were introduced and the SPR angle shift was monitored at least for 5 min. As shown in Fig. 4, the SPR angle shift was directly correlated with cTnI up to 160 μg/l. The statistically significant detection limit of the SPR biosensor was 68 ng/l cTnI. The SPR angle shift approached the saturation value of 171.8 RU, which corresponded to 171.8 pg cTnI/mm2 or 6.87 × 10−3 pmol cTnI/mm2 of the MAb P-II-13 surface layer, at a cTnI concentration above 660 μg/l (Fig. 4a). The dissociation constant, Kd, derived from Fig. 4b was 13.4 μg/l, indicating high binding affinity of MAb P-II-13 to cTnI.
Finally, we tested the performance of MAb P-II-13 SPR biosensor with human sera. Human sera (100 μl) from a patient with cardiac problems and a healthy volunteer were applied to the SPR biosensor. As shown in Fig. 5a, the SPR sensor detected the serum cTnI. The final SPR angle shift values for serum samples were 125RU for the cardiac patient and 85RU for the healthy volunteer, which corresponded to 65 and 15 μg/l of serum cTnI concentration, respectively. This was further confirmed with an immunoblot analysis of the samples with MAb P-II-13 (Fig. 5b).
Detection of troponin I (cTnI) in human serum samples. a Detection of cTnI by the MAb P-II-13-layered SPR sensor chip. Human serum (100 μl) was applied onto the MAb P-II-13-layered SPR sensor chip. b Immunoblot analysis of human sera with MAb P-II-13. Lane 1; patient serum, lane 2; control serum. Albumin was used as a loading control
Conclusion
we developed an SPR biosensor for detection of cTnI, a cardiac marker. For sensitive detection, we generated a highly specific anti-cTnI MAb P-II-13 using a peptide epitope with a protein chip-based screening method. The sensor was constructed on a modified gold thin film with MAb P-II-13 as a receptor for cTnI. The detection limit of the sensor was 68 ng/l, which was slightly higher than some commercial POCT devices (20–50 ng/l, Christenson and Azzazy 2009). With the merits of rapidity and simplicity, the SPR biosensor is a new way to diagnose heart muscle cell damage in point-of-care assays.
References
Adams JE, Bodor GS, Davila-Roman VG, Delmez JA, Apple FS, Ladenson JH, Jaffe AS (1993) Cardiac troponin I. A marker with high specificity for cardiac injury. Circulation 88:101–106
Adams JE, Sicard GA, Bridwell KH, Lenke LG, Davila-Roman VG, Bodor GS, Ladenson JH, Jaffe AS (1994) Diagnosis of perioperative myocardial infarction with measurement of cardiac troponin I. N Engl J Med 330:670–674
Akhtar S (2003) Biomarkers and perioperative myocardial infarction. Semin Anesth Perioper Med Pain 22:50–61
Alpert JS, Thygesen K, Antman E, Bassand JP (2000) Myocardial infarction redefined—a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol 36:959–969
Baac H, Hajos JP, Lee J, Kim D, Kim SJ, Shuler M (2006) Antibody based surface plasmon resonance detection of intact viral pathogen. Biotechnol Bioeng 94:815–819
Boltovets PM, Snopok BA, Boyko VR, Shevchenko TP, Dyachenko NS, Shirshov YM (2004) Detection of plant viruses using a surface Plasmon resonance via complexing with specific antibodies. J Virol Methods 121:101–106
Christenson RH, Azzazy HME (2009) Cardiac point of care testing: a focused review of current National Academy of Clinical Biochemistry guidelines and measurement platforms. Clin Biochem 42:150–157
Homola J (2003) Present and future of surface plasmon resonance biosensors. Anal Bioanal Chem 377:528–539
Jaffe AS, Ravkilde J, Roberts R, Naslund U, Apple FS, Galvani M, Katus H (2000) It’s time for a change to a troponin standard. Circulation 102:1216–1220
James S, Flodin M, Johnson N, Lindahl B, Venge P (2006) The antibody configurations of cardiac troponin I assays may determine their clinical performance. Clin Chem 52:832–837
Karlsen SR, Johnston KS, Jorgenson RC, Yee SS (1995) Simultaneous determination of refractive index and absorbance spectra of chemical samples using surface plasmon resonance. Sens Actuators B 25:747–749
Katrukha AG, Bereznikova AV, Esakova TV, Pettersson K, Lovgren T, Severina ME, Pulkki K, Vuopio-Pulkki LM, Gusev NB (1997) Troponin I is released in bloodstream of patients with acute myocardial infarction not in free form but as complex. Clin Chem 43:1379–1385
Kim SW, Kim MG, Kim J, Lee HS, Ro HS (2008a) Detection of the mycovirus OMSV in the edible mushroom Pleurotus ostreatus using an SPR biosensor chip. J Virol Methods 148:120–124
Kim SW, Kim MG, Jung HA, Lee KH, Lee HS, Ro HS (2008b) An application of protein microarray in the screening of monoclonal antibodies against the oyster mushroom spherical virus. Anal Biochem 374:313–317
Ko S, Kim B, Jo SS, Oh SY, Park JK (2007) Electrochemical detection of cardiac troponin I using a microchip with the surface-functionalized poly(dimethylsiloxane) channel. Biosens Bioelectron 23:51–59
Lateef SS, Gupta S, Jayathilaka LP, Krishnanchettiar S, Huang JS, Lee BS (2007) An improved protocol for coupling synthetic peptides to carrier proteins for antibody production using DMF to solubilize peptides. J Biomol Tech 18:173–176
Liedberg B, Lundstrom I, Stenberg E (1993) Principles of biosensing with an extended coupling matrix and surface plasmon resonance. Sens Actuators B 11:63–72
McDonnell B, Hearty S, Leonard P, O’Kennedy R (2009) Cardiac biomarkers and the case of point-of-care testing. Clin Biochem 42:549–561
Takeda S, Yamashita A, Maeda K, Maeda Y (2003) Structure of the core domain of human cardiac troponin in the Ca(2+)-saturated form. Nature 424:35–41
Tate JR (2008) Troponin revisited 2008: assay performance. Clin Chem Lab Med 46:1489–1500
Zot AS, Potter JD (1987) Structural aspects of troponin–tropomyosin regulation of skeletal muscle contraction. Annu Rev Biophys Biophys Chem 16:535–559
Acknowledgment
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology.
Author information
Authors and Affiliations
Corresponding author
Additional information
Young-Chul Kwon and Min-Gon Kim are equally contributed to this article.
Rights and permissions
About this article
Cite this article
Kwon, YC., Kim, MG., Kim, EM. et al. Development of a surface plasmon resonance-based immunosensor for the rapid detection of cardiac troponin I. Biotechnol Lett 33, 921–927 (2011). https://doi.org/10.1007/s10529-010-0509-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10529-010-0509-0