Abstract
Different studies have shown that −238 G>A polymorphism in promoter region of tumor necrosis factor alpha (TNF-α) gene is associated with increased risk of non-alcoholic fatty liver disease (NAFLD). The current study investigates the association between metabolic parameters and nutritional intakes with −238 G>A of TNF-α promoter gene polymorphism among the Iranian patients with NAFLD. In this study, 75 patients with NAFLD and 76 individuals as control were enrolled. Dietary intakes were assessed using a semi-quantitative food-frequency questionnaire. Body mass index and waist to hip ratio were calculated. Biochemical assays were measured after 12 h fasting. −238 G>A Polymorphism of TNF-α gene was determined by using sequencing method. We observed no significant difference in frequency of different genotypes of this polymorphism between NAFLD and control groups (P > 0.05). Among biochemical parameters, TAC showed significant decrease in NAFLD patients with GG genotype when compared to controls (P = 0.001). The comparison of macro and micronutrient intakes between groups according to genotypes showed no statistically significant difference (P > 0.05). Although the data were not statistically significant, further studies with larger sample size are needed to determine the effect of dietary compounds in NAFLD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-alcoholic fatty liver disease (NAFLD) is featured by abnormal accumulation of droplet of triglycerides in the absence of significant alcohol consumption (Xu et al. 2013). NAFLD encompasses a spectrum that ranges from simple steatosis to non-alcoholic steatohepatitis (NASH) (Weiß et al. 2014). It is strongly associated with Type 2 Diabetes Mellitus (T2DM), central obesity, insulin resistance (IR), and features of metabolic syndrome (Gaggini et al. 2013; Marchesini et al. 2003; Weiß et al. 2014).
The prevalence of the NAFLD in developed countries is up to 30 % among the general population, 50 % in patients with T2DM, 76 % in obese individuals, and nearly 100 % in patients with morbid obesity (Adams et al. 2005; Browning et al. 2004).
Genetic polymorphism and nutrition intake are involved in NAFLD progression as a multifactorial disease (Kalafati et al. 2014; Moore 2010). Dietary composition can be a major factor to influence by altering the relative sources of hepatic fat accumulation (Utzschneider and Kahn 2006). Therefore, knowledge on environmental factors like diet and metabolic factors should be combined to achieve new facts about genetic variety (Wang et al. 2012). Moreover, genetic variations are associated with several factors such as reactive oxygen species, cytokines, endotoxin receptors, and insulin resistance which are involved in susceptibility to NAFLD (Zhou et al. 2010).
Insulin-resistant patients with NAFLD show decreased insulin sensitivity either at the level of muscle or at the level of liver and adipose tissue (Bugianesi et al. 2005; Lomonaco et al. 2012). Insulin resistance is related to increase of free fatty acids (FFAs) flux that causes increased triglyceride (TG) production, assembly, and secretion of very low-density lipoprotein (VLDL) in hepatocytes. Fat accumulation in liver is also linked with lipid peroxidation and oxidative stress (Gaggini et al. 2013). Oxidative stress phenomenon is induced by imbalance in the pro-oxidant/antioxidant equilibrium; a condition that may influence a number of pathophysiological events in the liver (Videla et al. 2004).
Tumor necrosis factor-alpha (TNF-α) is an important pro-inflammatory cytokine and is associated with development forms of liver injury because of its possibility to induce apoptosis, IR, and oxidative stress (Oliveira and Stefano 2015; Valenti et al. 2002; Wong et al. 2008). Previous studies in other countries have reported higher prevalence of −238 TNF-α gene promoter polymorphism in NAFLD patients and its association with high risk of IR (Oliveira and Stefano 2015; Wang et al. 2012). The TNF-α gene is located on chromosome 6p21.3 in human which codes for a 157-amino acid polypeptide and processed from a 233-amino acid precursor (Beutler and Cerami 1985). Immune cells in adipose tissue are a significant source of TNF-α production (Vikram et al. 2011).
On the basis of relation between −238 G>A TNF-α polymorphisms with NAFLD reported in other countries, in the current study, we aimed to evaluate the association of −238 G>A polymorphism of TNF-α gene with NAFLD. Considering the fact that there is no report about the relationship between −238 G>A TNF-α different genotypes with insulin resistance and oxidative stress parameters in NAFLD patients, in this study we evaluated the relation between frequency of different genotypes of this polymorphism with insulin resistance, oxidative stress parameters, and nutritional intakes in NAFLD patients of North West of Iran.
Methods
The current case control study was carried out between 75 patients with NAFLD and 76 healthy subjects. Patients were selected from the gastroenterology clinics of Tabriz University of Medical Sciences, Tabriz, IRAN. Disease diagnosis was confirmed by the physician based on the findings of ultrasonography (US). The patients had simple steatosis (grades 1–2). Control group was composed of the volunteers from university staff and acquired relatives of patients. They were matched by age and gender with case group. Also US was done for healthy volunteers to confirm the lack of NAFLD. Written informed consent was obtained from all of participants.
Inclusion criteria were as follows: aged between 20 and 50 years and BMI between 25 and 39.9 kg/m2. The exclusion criteria were as follows: other liver diseases such as viral hepatitis, autoimmune or endocrine disorders, hemochromatosis, Wilson’s disease, pregnancy or lactation, alcohol consumption, using hepatotoxic medications and being on weight loss diets for at least 3 months prior participation in study.
Anthropometric Assessments
Subjects’ weight was measured with a calibrated scale (SECA, Hamburg, Germany) to the nearest 0.1 kg, while they were in minimal clothing without shoes. Their height was measured by non-stretchable measurement tape with the precision of 0.1 cm. Weight (kg) divided by height squared (m2) were calculated for body mass index (BMI). Waist circumference (WC) was performed in standing position at the level of the umbilicus, and hip circumference (HC) was measured at the maximum circumference between the hip and the buttock with a non-elastic tape.
Biochemical Assessments
After an overnight fasting, 7 cc venous blood samples were obtained from subjects. Approximately, 2 cc of the blood was transferred into tubes containing ethylene diamine tetra acetic acid (EDTA) for genetic assays. Serum samples were obtained from remaining blood for biochemical assays. Measuring of fasting serum glucose (FSG), alanine aminotransferase (ALT), aspartate aminotransferase (AST), total cholesterol (TC), TG, and high-density lipoprotein cholesterol (HDL-C) were assessed by Abbott ALCYON™ 300 auto analyzer using commercial ELISA kits (Pars-Azmoon, Tehran, Iran). Serum LDL-C was calculated by Friedewald formula (Friedewald et al. 1972). Insulin resistance was estimated by the homeostasis model (HOMA-IR) by following equation: fasting serum insulin (µU/ml) × fasting glucose (mg/dl)/405 (Tokushige et al. 2007).
Measuring of serum total antioxidant capacity (TAC) was performed by colorimetric method using Randox Kit (Randox laboratories ltd., UK). Malondialdehyde (MDA) levels were measured by thiobarbituric acid reactive substances (TBARS) method. Samples were heated with 0.6 % thiobarbituric acid under acidic condition; the colored product was extracted into n-butanol after cooling. The color absorbance was measured at 530 nm. MDA standards were made with 1,1,3,3-tetraethoxypropane. All of the biochemical assays were conducted by a trained lab assistant who was blinded to group assignments.
Dietary Intakes
Dietary intakes were analyzed by semi-quantitative food-frequency questionnaire (FFQ) adapted to the Iranian society (Mirmiran et al. 2009). The FFQ contained 168 food items with specified serving sizes usually consumed by Iranians. Study subjects reported their average frequency intake of each food item in terms of the number of specified serving sizes consumed per day/week/month/year, or never. The reported frequency of food consumption and portion sizes were converted to a daily intake.
DNA Extraction and Genotyping
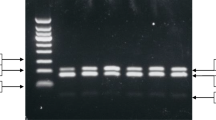
Genomic DNA was isolated from the blood cells by salting out method (Miller et al. 1988). Our designed primers for evaluation of this polymorphism were 5′-GGT CCT ACA CAC AAA TCA GTC A-3′ as forward primer and 5′-GGA CAC ACA AGC ATC AAG GA-3′ as reverse primer. For doing polymerase chain reaction (PCR), 1 µl of genomic DNA, 0.2 µl of Taq DNA polymerase, and 1 µl from each primers were added to 22 µl of 1× PCR master-mix. PCR procedure included a primary denaturation at 95 °C for 5 min followed by 35 cycles of denaturation at 95 °C for 1 min, annealing at 59 °C for 1 min, extension at 70 °C for 1 min, and a final extension at 70 °C for 5 min. Sequencing of PCR products was carried out according to Sanger method using ABI 3730XL Capillary Sequencer. Sequencing results were compared with the sequence of normal TNF-α gene obtained from NCBI website: http://www.ncbi.nlm.nih.gov; also, sequence traces were assembled using Chromas software (version 2.4). At position 238 of the TNF-α gene promotor region, guanine substitutes to adenine and three different forms of genotypes of this gene polymorphism are wild type (GG), heterozygote (GA), and homozygote (AA) (Wang et al. 2012).
Statistical Analysis
All data analysis was performed using the SPSS software (Statistical Package for the Social Sciences, SPSS Inc., Chicago, IL, USA). The normality of variables was assessed by Kolmogorov–Smirnov test. Variables are expressed as mean ± standard deviation (SD) or numbers and percentages. The comparison of continuous variables between two groups was performed by 2-tailed independent sample t test. Comparison of continuous variables between different TNF-α genotypes was performed by analysis of covariance (ANCOVA) with adjustment for the confounder effect of age and sex. Categorical variables were also compared using the χ2 test. Logistic regression analysis was used to assess the relationship between anthropometric and biochemical variables with NAFLD genotypes adjusted for the confounding role of sex and age. P value of less than 0.05 was considered to be significant.
Results
The demographic features of the studied population are shown in Table 1. No significant difference was observed in mean age and BMI between NAFLD and healthy control groups. However, WC and waist to hip ratio (WHR) in NAFLD patients were significantly higher when compared with control group (P < 0.05). Among biochemical variables in Table 2, serum HDL-C and LDL-C concentrations were significantly lower and serum AST, ALT and triglyceride concentrations were significantly higher in NAFLD patients compared to control group (P < 0.05 and P < 0.01, respectively). HOMA-IR and MDA levels in patients with NAFLD and control subjects did not have significant difference (P > 0.05). Mean value of TAC was significantly low in NAFLD patients compared to control group (P = 0.001).
The frequency distribution of different genotypes of −238 TNF-α polymorphism in the study groups is presented in Table 3. We observed no significant difference in GG and AG genotype between NAFLD and control groups (P > 0.05). There was no AA genotype in two studied groups.
The comparison of studied parameters according to different genotypes of −238 G/A polymorphism in TNF-α gene between NAFLD and control group is presented in Tables 4 and 5. Waist circumference in NAFLD group was not significant in comparison to control individuals according to genotypes (P > 0,05); among the biochemical parameters, TAC levels were significantly lower in NAFLD patients with GG genotype in comparison to control subjects (P = 0.001). HOMA-IR and MDA have shown no significant change in NAFLD patients with AG and GG genotypes when compared with control group (P > 0.05).
Statistical significant differences were not observed in dietary intakes between patients and control subjects (P > 0.05) (Table 6). The comparison of dietary intakes between case and control groups according to different genotypes of −238 G/A TNF-α gene polymorphism is shown in Table 7. No statistical significant difference was observed for nutrient intakes in studied groups with AG and GG genotypes (P > 0.05).
Discussion
In the current case–control study, we evaluated different genotypes frequency of −238 G/A polymorphism in TNF-α gene among the NAFLD patients. Generally speaking, differences in genotype distribution in various population can be explained by racial/ethnic differences (Mcgraw and Waller 2012).
Distribution of different genotypes and allele frequency of our studied polymorphism among the Iranian population had complete concordance with Japanese population. In this regard, Tokushige et al. (2007) reported no significant difference in genotypes and allele frequency of this polymorphism among 102 Japanese patients with fatty liver in comparison to healthy group. In their study, the same as our research, there were no AA genotypes among the studied samples, and they also showed no significant difference in GG and AG genotype frequency between NAFLD and control subjects. However, in other populations, some studies have been reported higher frequency of AG genotype in case group compared to control ones (Valenti et al. 2002; Wong et al. 2008).
Central obesity and insulin resistance are well characterized to be associated with intra-abdominal fat accumulation which has been positively correlated with liver fat (Utzschneider and Kahn 2006). Waist circumference as a marker of central obesity has shown higher significant difference in NAFLD patients than healthy subjects. However, WC and WHR did not associate with different genotypes of TNF-α gene in patients compared to control. In agreement with our study, Hedayati et al. (2012) have reported no association between obesity and different genotypes of the mentioned polymorphism.
About the serum insulin and HOMA-IR, we did not observe significant association with different genotypes in our studied groups; in the line of our results, Tokushige et al. (2007) have reported no association between HOMA-IR with AG and GG genotypes in NAFLD patients; however, their control study group was not obese. On the other hand, Day et al. (1998) reported high A allele frequency in 123 non-diabetes relatives with lower HOMA-IR compared to control group. The possible explanation is that −238 TNF-α gene promoter polymorphism may be affected by population stratification and other relevant genetic variants (Day et al. 1998).
Concentration of Malondialdehyde (MDA), one of the most frequently used biomarker to indicate lipid peroxidation, was not associated with different genotypes of this polymorphism in our studied groups. On the other hand, among our samples, NAFLD patients with GG or normal genotype showed low TAC in comparison to control. These findings were in agreement with a study by Ostad Rahimi et al. (2011), where they showed significant low-serum TAC level in NAFLD patients. Other studies by Videla et al. (2004) and Yesilova et al. (2005) have reported similar results; however unlike our study, no association between biomarkers of oxidative stress and gene polymorphisms has been evaluated in their studies. The possible mechanism of the development of higher oxidative stress status in patients with NAFLD can be related to serum levels of the Kupffer cell and stellate cell-derived cytokines such as TNF-α (Videla et al. 2004).
In our study, the comparison of macro and micronutrient intake did not show any statistically significant differences between subjects. Similar to our findings, Zelber-Sagi et al. (2007) study showed no statistically significant differences in nutrients intake between NAFLD and normal liver groups.
In our study, we did not achieve significant differences in nutrients intake according to genotypes of this polymorphism. These associations are needed to be conducted in larger and best possible prospective studies designed for confirming the obvious dietary intake recommendations to prevent of NAFLD progression.
Conclusion
In conclusion, TNF-α promoter gene polymorphism at position −238 did not show to be associated with NAFLD among the North West Iranian population. Our results showed that among the metabolic parameters, TAC was significantly low in patients with GG genotype. Also, not achieving significant results in some findings might be attributed to relatively small sample size. Further studies with larger sample size and interventional designs are needed to determine the effect of dietary compounds in non-alcoholic fatty liver disease.
References
Adams LA, Lymp JF, Sauver JS, Sanderson SO, Lindor KD, Feldstein A et al (2005) The natural history of non-alcoholic fatty liver disease: a population-based cohort study. Gastroenterology 129:113–121
Beutler B, Cerami A (1985) Cachectin and tumour necrosis factor as two sides of the same biological coin. Nature 320:584–588
Browning JD, Szczepaniak LS, Dobbins R (2004) Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology 40:1387–1395
Bugianesi E, Gastaldelli A, Vanni E, Gambino R, Cassader M, Baldi S et al (2005) Insulin resistance in non-diabetic patients with non-alcoholic fatty liver disease: sites and mechanisms. Diabetologia 48:634–642
Day C, Grove J, Daly AK, Stewart MW, Avery PJ, Walker M (1998) Tumour necrosis factor-alpha gene promoter polymorphism and decreased insulin resistance. Diabetologia 41:430–434
Friedewald WT, Levy RI, Fredrickson DS (1972) Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18:499–502
Gaggini M, Morelli M, Buzzigoli E, DeFronzo RA, Bugianesi E, Gastaldelli A (2013) Non-alcoholic fatty liver disease (NAFLD) and its connection with insulin resistance, dyslipidemia, atherosclerosis and coronary heart disease. Nutrients 5:1544–1560
Hedayati M, Sharifi K, Rostami F, Daneshpour M, Yeganeh M, Azizi F (2012) Association between TNF-α promoter G-308A and G-238A polymorphisms and obesity. Mol bio rep 39:825–829
Kalafati I, Borsa D, Dedoussis GVZ (2014) The genetics of nonalcoholic fatty liver disease: role of diet as a modifying factor. Curr Nutr Rep 3:223–232
Lomonaco R, Ortiz-Lopez C, Orsak B, Webb A, Hardies J, Darland C et al (2012) Effect of adipose tissue insulin resistance on metabolic parameters and liver histology in obese patients with nonalcoholic fatty liver disease. Hepatology 55:1389–1397
Marchesini G, Bugianesi E, Forlani G, Cerrelli F, Lenzi M, Manini R et al (2003) Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology 37:917–923
McGraw J, Waller D (2012) Cytochrome P450 variations in different ethnic populations. Expert Opin Drug Metab Toxicol 8:371–382
Miller S, Dykes D, Polesky H (1988) A simple salting out procedure for extracting DNA from nucleated cells. Nucleic Acid Res 16:1215
Mirmiran P, Hosseini Esfahani F, Mehrabi Y, Hedayati M, Azizi F (2009) Reliability and relative validity of an FFQ for nutrients in the Tehran lipid and glucose study. Public Health Nutr 13:654–662
Moore J (2010) Non-alcoholic fatty liver disease: the hepatic consequence of obesity and the metabolic syndrome. Proc Nutr Soc 69:211–220
Oliveira C, Stefano J (2015) Genetic polymorphisms and oxidative stress in non-alcoholic steatohepatitis (NASH): a mini review. Clin Res Hepatol Gastroenterol 39:S35–S40
Ostad Rahimi A, Mahdavi R, Somi MH, Tarzemani MK (2011) Oxidative stress-related parameters and antioxidant status in non-alcoholic fatty liver disease patients. IJEM 12:493–499
Tokushige K, Takakura M, Tsuchiya-Matsushita N, Taniai M, Hashimoto E, Shiratori K (2007) Influence of TNF gene polymorphisms in Japanese patients with NASH and simple steatosis. J Hepatol 46:1104–1110
Utzschneider K, Kahn S (2006) The role of insulin resistance in nonalcoholic fatty liver disease. J Clin Endocrinol Metab 91:4753–4761
Valenti L, Fracanzani AL, Dongiovanni P, Santorelli G, Branchi A, Taioli E et al (2002) Tumor necrosis factor α promoter polymorphisms and insulin resistance in nonalcoholic fatty liver disease. Gastroenterology 122:274–280
Videla L, Rodrigo R, Orellana M, Fernandez V, Tapia G, Quinones L et al (2004) Oxidative stress-related parameters in the liver of non-alcoholic fatty liver disease patients. Clin Sci 106:261–268
Vikram N, Bhatt S, Bhushan B, Luthra K, Misra A, Poddar PK et al (2011) Associations of −308G/A polymorphism of tumor necrosis factor (TNF)-α gene and serum TNF-α levels with measures of obesity, intra-abdominal and subcutaneous abdominal fat, subclinical inflammation and insulin resistance in Asian Indians in North India. Dis Markers 31:39–46
Wang J, Feng Z, Li Y, Li Q, Tao XY (2012) Association of tumor necrosis factor-α gene promoter polymorphism at sites-308 and-238 with non-alcoholic fatty liver disease: a meta-analysis. J Gastroenterol Hepatol 27:670–676
Weiß J, Rau M, Geier A (2014) Non-alcoholic fatty liver disease: epidemiology, clinical course, investigation, and treatment. Dtsch Arzteblatt Int 111:447–452
Wong V, Wong G, Tsang SW, Hui AY, Chan AW, Choi PC et al (2008) Genetic polymorphisms of adiponectin and tumor necrosis factor-alpha and nonalcoholic fatty liver disease in Chinese people. J Gastroenterol Hepatol 23:914–921
Xu Y, Liang L, Wang CL, Fu JF, Liu PN, Lv LQ et al (2013) Association between UCP3 gene polymorphisms and nonalcoholic fatty liver disease in Chinese children. World J Gastroenterol 19:5897–5903
Yesilova Z, Yaman H, Oktenli C, OzcanA UA, Cakir E et al (2005) Systemic markers of lipid peroxidation and antioxidants in patients with nonalcoholic fatty liver disease. Am J Gastroenterol 100:850–855
Zelber-Sagi S, Nitzan-Kaluski D, Goldsmith R, Webb M, Blendis L, Halpern Z et al (2007) Long term nutritional intake and the risk for non-alcoholic fatty liver disease (NAFLD): a population based study. J Hepatol 47:711–717
Zhou Y, Li Y, Nie Y, Yang H, Zhan Q, Huang J et al (2010) Influence of polygenetic polymorphisms on the susceptibility to non-alcoholic fatty liver disease of Chinese people. J Gastroenterol Hepatol 25:772–777
Acknowledgments
We appreciate all of the participants in the current study. We also thank Nutrition Research Center of Tabriz University of Medical Sciences and Cellular and Molecular Research Center of Qazvin University of Medical Science for providing laboratory facilities.
Funding
This research was supported by a grant from cellular and molecular research center of Qazvin University of Medical Sciences.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Mohseni, F., Rashvand, Z., Najafipour, R. et al. Evaluating −238 G>A Polymorphism Association in TNF-α Gene with Metabolic Parameters and Nutritional Intakes Among the Iranian NAFLD Patients. Biochem Genet 54, 685–695 (2016). https://doi.org/10.1007/s10528-016-9747-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10528-016-9747-8