Abstract
Worldwide prevalence of diabetes mellitus motivates a number of association studies to be conducted throughout the world. Eleven polymorphisms from nine candidate genes in oxidative stress pathway have been analyzed in eastern Indian type 2 diabetic patients (n = 145) and healthy controls (n = 100). Different biochemical parameters were also analyzed for their association with the disease. Significant associations were observed for rs2070424 A>G SOD1 (OR 3.91, 95% CI 2.265–8.142, P < 0.001), rs854573 A>G PON1 (OR 3.415, 95% CI 2.116–5.512, P < 0.001), rs6954345 G>C PON2 (OR 3.208, 95% CI 2.071–4.969, P < 0.001), RAGE rs1800624 −374 T>A (OR 3.58, 95% CI 2.218–5.766, P < 0.001), and NOS3 −786 T>C (OR 3.75, 95% CI 2.225–6.666, P < 0.001). Haplotype containing two risk alleles of PON1 and PON2 genes was significantly associated with disease (OR 8.34, 95% CI 1.554–44.804, P < 0.002). Our results suggest that carriers of major and efficient alleles of oxidative stress genes are more likely to survive the comorbid complications and single copy of risk allele is sufficient for developing the disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type 2 diabetes mellitus (T2DM) is a multifactorial metabolic disorder which is growing in epidemic proportions throughout the world and the greatest increase in prevalence is predicted to occur in Asia and Africa by 2030 (Wild et al. 2004). Several lines of evidence suggests that the aetiopathogenesis of the common form of T2DM includes strong genetic components contributed by several common genetic variants, each with relatively modest effect, acting in combination with each other and with environmental and lifestyle triggers (Adak et al. 2010).
T2DM, or non-insulin-dependent diabetes mellitus (NIDDM), is characterized by insulin resistance with significant metabolic dysfunction that includes obesity, impaired insulin function and secretion, and increased endogenous glucose output. Insulin resistance or defective insulin action occurs when physiological level of insulin produces a subnormal response. This abnormal insulin secretion may be a result of defective β-cell function, chronic exposure to free fatty acids and hyperglycemia, and the loss of inhibitory feedback through plasma glucagon levels (Del Prato and Marchetti 2004).
A growing body of evidence suggests that oxidative stress plays a key role in the pathogenesis of micro- and macrovascular diabetic complications. The increased oxidative stress in subjects with T2DM is a consequence of several abnormalities, including hyperglycemia, insulin resistance, hyperinsulinemia, and dyslipidemia, each of which contributes to mitochondrial superoxide overproduction in endothelial cells of large and small vessels as well as the myocardium. Major pathophysiological mechanisms that underlie diabetic complications could be explained by increased production of reactive oxygen species (ROS) via: (1) the polyol pathway flux, (2) increased formation of advanced glycation end products (AGEs), (3) increased expression of the receptor for AGEs, (4) activation of protein kinase C isoforms, and (5) overactivity of the hexosamine pathway (Brownlee 2001; King and Loeken 2004; Leon and Raij 2005; Sheetz and King 2002).
Oxidative stress can promote both diabetic cell injury and the development of insulin resistance by decreasing insulin sensitivity and destroying the insulin-producing cells within the pancreas (Maiese et al. 2007). For example, ROS can penetrate through cell membranes and cause damage to β-cells of pancreas (Chen et al. 2005). Free fatty acids, which can lead to ROS generation, have been shown to contribute to mitochondrial DNA damage and impaired pancreatic β-cell function (Rachek et al. 2006). Oxidative stress also is believed to modify a number of the signaling pathways that can ultimately lead to insulin resistance. Conversely hyperglycemia can lead to increased production of ROS in endothelial cells, liver and pancreatic β-cells (Yano et al. 2004). In rats, hyperglycemia has been shown to result in a significant decrease in insulin-stimulated glucose uptake, a significant increase in muscle protein carbonyl content (used as an indicator of oxidative stress), and elevated levels of malondialdehyde and 4-hydroxynonenal as an indicator of lipid peroxidation (Haber et al. 2003). Studies on oxidative stress and insulin resistance unequivocally suggest that ROS contribute to the pathogenesis of hyperglycemia-induced insulin resistance (Haber et al. 2003).
Proximal hyperglycemia-induced changes affect multiple cell signaling pathways through activation of protein kinase C (PKC), NADPH oxidase, poly-ADP-ribose polymerase (PARP), and other more upstream events, which finally activate transcription factors AP-1 and nuclear factor kappa beta (NFķβ) (Fig. 1). Hyperglycemia-induced metabolic alterations lead to activation of PARP-mediated energy depletion and NFķB-mediated inflammation which may be abolished by overexpression of mitochondrial superoxide dismutase (SOD) or mitochondrial SOD (MnSOD) (Nishikawa et al. 2000). In addition, hyperglycemia-induced expression of endothelial and inducible forms of nitric oxide synthetase (NOS) has been shown to enhance production of nitric oxide (NO) (Kankova and Sebekova 2005). Reactive dicarbonyls (mainly methylglyoxal), if not sufficiently metabolized by glyoxalase system (GLO1 and 2), are precursors of AGEs. Reactive oxygen species (ROS) and AGEs activate transcription factors AP-1 and NFķβ causing DNA damage. PARP-1 transfers poly-ADP-ribose units to several nuclear proteins including glyceraldehyde-3-phosphate dehydrogenase (GAPDH) preventing translocation of GAPDH from nucleus to cytoplasm and thus prevents its function as a glycolytic enzyme which leads to the accumulation of the upstream intermediate compounds of the glycolytic pathway. The activation of these pathways, in turn, results in the secondary production of ROS and induces oxidative stress (Baragetti et al. 2013). The involvement of different oxidative stress related genes encoding SOD (SOD1, SOD2), NOS, high density lipoprotein and low density lipoprotein associated paraxonase (PON1, PON2), NADPH oxidase (CYBA1), receptor for AGEs (RAGE) in the above mentioned pathways are thus well accepted. This underscores the importance of association study of these genes for understanding diabetic complications more properly.
A pathway for RAGE-induced intracellular cell signaling (Kankova and Sebekova 2005)
Polymorphisms in SOD and RAGE genes are implicated in diabetes pathogenesis by a number of association studies conducted in South Asian and Caucasian populations (Tiwari et al. 2009; Matsunaga-Irie et al. 2004; Prasad et al. 2010). Human serum PON1 gene protects from atherosclerosis by preventing LDL-C from oxidation as well as by hydrolyzing the oxidized form of LDL-C. PONase activity has been found to be decreased in patients with diabetes (Altuner et al. 2011; Ergun et al. 2011) and familial hyperlipidemia. Nearly 200 single-nucleotide polymorphisms (SNPs) of PON1 gene have been identified so far (Richter et al. 2010), of which most studied are −909 G/C [rs854572], A/G [rs854573], 108 C/T [rs705379], and L55M [rs 854560] [Costa et al.2003]. Several sequence variants particularly Arg148Gly and Cys311Ser variants on PON2 have received much attention for their association with microvascular complications in type1 and type 2 diabetes mellitus (Mayer and Hemmens 1997). Endothelial NOS (eNOS), a key regulator of vascular nitric oxide production, has been investigated extensively to determine the relevance of DNA variants in the eNOS gene to vascular and renal diseases. eNOS or NOS3 gene, is mapped to chromosome 7q36 is highly polymorphic and several studies are undertaken to investigate the potential association of polymorphisms and risk of atherothrombotic vascular disease in Caucasian and Asian populations. A SNP in the promoter region (−786 T/C), a G/T substitution at nucleotide 894 in exon7 leading to an amino acid change (Glu298Asp), and a 27 bp variable number of tandem repeats (27 bp-VNTR) in intron 4 have received much attention because of their functional relevance to eNOS activity and association with cardiovascular and renal diseases (Thameem et al. 2008). An increased risk of hypertension for individuals homozygous for the −786C allele was observed in Caucasians. Also the, variants in Aldoketo Reductase family 1 member B1 (AKR1B1) genes have been investigated for their association with different disease conditions. AKR1B1 variants have been shown to be associated with diabetic neuropathy (Sivenius et al. 2004; Donaghue et al. 2005), nephropathy (Makiishi et al. 2003), and retinopathy (Wang et al. 2003). Given genetic impact of the mentioned stress-related genes in diabetic patients around the world, the present study compares the distribution of genotype and allele frequencies of eleven polymorphisms from nine major oxidative stress-related genes between 145 eastern Indian diabetic populations and 100 healthy controls. In addition, genotypic dependence of different clinical parameters such as BMI, blood sugar, and glycated hemoglobin (HbA1C) levels was also explored in diabetic patients.
Materials
Study Subjects
A total of 145 T2DM patients and 100 healthy controls participated in this case control association study. Blood samples were collected from 45 to 55 years old unrelated individuals suffering from type 2 diabetes for the period of 1–5 years and sex and age matched healthy volunteers from IPGMER/SSKM hospital, Kolkata, India. The study was guided by World Health Organisation criteria and University and Hospital ethical committees’ guidelines. All the clinical data were obtained from outpatient departments of SSKM. All type 2 diabetes patients represented BMI of 18–35 kg/m2, HbA1C > 7%. The 2 h post-glucose tolerance test of blood sugar level (after a 75 g glucose load) for diabetic patients is greater than 200 mg/dL (11.11 mmol/L) while the value is less than 140 mg/dL (7.8 mmol/L) for control healthy subjects (without any family history of diabetes or hypertension). None of the subjects (both control and patients) were smokers. Complete clinical and demographic characteristics of the study population have been reported in Table 1.
Methods
Sample Preparation and Genotyping
Following salting out (Miller et al. 1988) of genomic DNA from 5 mL of venous blood, the yield and purity of DNA were confirmed by spectrophotometric analysis by estimating the absorbance at 260 and 280 nm. Primers for eleven SNPs distributed over nine candidate genes (Table 2) were designed for the study. Approximately 100–150 ng of genomic DNA from each individual was amplified using specific primer pairs (Table 3). Briefly, the PCR was performed in a Veriti® thermocycler (Applied Biosystem), following a standard protocol. Eight to ten microliters of PCR product was digested with 5 U of respective restriction endonucleases from New England Biolabs (NEB) (Table 3) in a final volume of 20 mL following the manufacturer’s instructions. The resulting fragments were separated on 2–3% agarose gel, visualized in Gel-Documentation System 2000 (Bio-Rad Laboratories (UK) Ltd). Genotype assignment was based on size discrimination of PCR-digested products. Samples with known genotypes were included in each set of digestion to ensure that the observed genotypes were not due to partial/incomplete digestion (Fig. 2).
Statistical Analysis
The clinical variables were represented as mean/median ± SE (Table 1). All the clinical parameters were log transformed for normal distribution and subjected to Pearson correlation in pair-wise combinations. Hardy–Weinberg equilibrium was tested using the χ 2 goodness-of-fit test in cases and controls. In all the polymorphic region the 11 genotype corresponds to the first allele, e.g., Ala 9 Val C>T 11 = CC, 12 = CT, 22 = TT genotypes. Strength of association was tested by odds ratio estimates at 95% confidence interval. P values <0.05 were considered significant. Bonferroni correction and false discovery rate (FDR) and power of the sample size for each of the SNPs at 5% significance level was calculated. Simple linear regression analysis was done on significantly correlated parameters. Taking one specific parameter as dependent and other correlated parameters as predictor variables, standardized residuals were obtained and clarified for association analyses. Association between disease phenotype and genotype(s) of a particular locus was analyzed by parametric independent t test and ANOVA to examine equality of means and non-parametric Kruskal–Wallis H test which makes no assumption of normal distribution or equality of means/variances of the quantitative index under different genetic model (Fig. 2). For linked loci, the haplotypes and their frequencies were estimated using Haploview separately in T2DM patients and controls. An assessment of allele/haplotype-based risk was performed by comparing the frequency of an individual allele/haplotype with that of the most prevalent one taken as reference using a two-way contingency table. This enabled us to estimate the odds ratios (ORs) with 95% confidence intervals (CI’s), χ 2 and P values.
Results
Clinical Demography
The differences of all the clinical parameters between cases and control groups for both the baseline (data collected before treatment of cases) and endpoint data (data collected after treatment of cases) were found to be statistically significant. The log transformation of the crude data reduced the skewness property for mean value of the distribution of each clinical parameter and log transformed data of clinical variables approximated the features of normal distribution (Table 1). Gender, log transformed mean value of BMI baseline, and endpoint data did not yield any statistical significance between case and controls.
Genetic Analysis
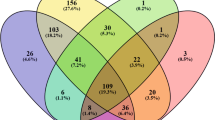
Eleven SNPs from 9 oxidative stress-related genes such as SOD1, SOD2, SOD3, PON1, PON2, AGER, AKR1B1, NOS3, and NADPH p22 phox CYBA1 were tested in all diabetic and healthy populations. Hardy–Weinberg equilibrium (HWE) prevailed for each gene for both cases and controls. Statistically significant association was observed for SOD1 (rs2070424, A>G), PON1 (rs854573, A>G), PONII (rs6954345, G>C), RAGE −374 (rs1800624, T>A), and NOS3 (−786, T>C) genotype frequencies observed in diabetic group was compared with that in healthy controls (Table 4; Figs. 3, 4, 5). This could be attributed to a significant excess of major or wild-type allele and major homozygous genotypes in both diabetic as well as healthy groups. A dominant model of inheritance with respect to minor allele frequencies (ranged from 28 to 40%; Table 4) was observed in all 5 associated loci of disease groups. The larger odds of rare homozygous genotype to common homozygous genotype than odds of heterozygotes genotype to common homozygous genotype was observed between cases and controls in all associations. The remaining markers such as SOD2 (rs1799725, C>T), SOD3 (rs699473, T>C), AGER 1704 G/A, AKR1B1, and CYBA1 were not found to be associated with the disease in this study population.
Genotype-Based Effect of Different Clinical Parameters by Parametric and Non-Parametric Analyses
Correlation between different clinical parameters was explored for both crude and log transformed data. Significant correlation was observed between BMI baseline and fasting baseline data, BMI baseline data and fasting endpoint data, Fasting and PP among diabetic populations (Fig. 6). The baseline and endpoint value of HbA1C explored no significant correlation with any other clinical parameter. The correlated parameters were then linearly regressed to nullify the probable impact of the factor that was found to be correlated. The residuals of each specific parameter was analyzed for association study. We examined the effect of individual genotype in pair-wise comparisons of all 5 associated loci on different clinical parameter levels using non-parametric Kruskal–Wallis test (Tables 5, 6) which explored asymptomatic significance in accordance with different genotypic groups, based on different clinical parameters. The asymptomatic significance of mean differences in HbA1c level however, observed in 11 versus 12 genotype combinations of SOD1 A>G (Ala9Val, rs2070424) SNP, PON2 (rs6954345 G>C) SNP, between 11 versus 22 genotypic groups of SOD1 A>G and RAGE rs 1800624 T>A SNP, 12 versus 22 genotype combinations of RAGE rs 1800624 T>A SNP (Table 5). Mean HbA1C level in diabetic populations also revealed parametric differences in 11 versus 12 gp of SOD1 A>G (Ala9Val, rs2070424) and PON2 (rs6954345 G>C) SNPs (Table 5) and 12 versus 22 gp of RAGE rs 1800624 T>A SNP. In all aspect baseline values of clinical parameters gave differences. The residuals of all the correlated parameters revealed marginal differences in 11 versus 12 genotypes of PON1 A>G (rs854573) SNP (Table 6). None of the correlated parameters revealed significant difference in any genotypic groups when residuals were considered in parametric analysis in cases.
Haplotype-Based Risk Assessment in PON1 and PON2 SNPs
Haplotypes pertaining to PON1 and PON2 SNPs and maximum likelihood estimates of their frequencies were obtained using Haploview (Table 7). For PON1, A>G (rs854573) SNP, the A-allele was coded by 0 and the G-allele by 1. For PON2 (rs6954345 G>C) SNPs, the G-allele was coded by 0 and the C-allele by 2. A total of four haplotypes (00, 01, 10. 11) were observed in the patients and control samples. Most common haplotype in both cases and controls was 00 (Table 7). Since proportion of common haplotype was larger in control group, risk assessment of each individual haplotype was performed with reference to this (00). Haplotype 11 represented a greater odds ratio when compared both with a single reference haplotype as well as against all other haplotypes pooled as single reference haplotype. The other two risk haplotypes 01 and 10 produced significant difference between cases and controls when compared against most prevalent 00 haplotype but no significant differences when compared against pooled haplotypes (Table 7).
Discussion
Diabetes mellitus (DM) is a chronic disorder characterized by impaired metabolism of glucose and lipids due to defect in insulin secretion (beta cell dysfunction) or action (insulin resistance). The characteristic properties of diabetes mellitus are chronic hyperglycemia, microvascular (e.g., retina, renal glomerulus, and peripheral nerve) as well as macrovascular [e.g., atherosclerosis, coronary artery disease (CAD), stroke] pathologies with more than 17.5 million deaths worldwide attributable to cardiovascular complications (Moore et al. 2009). According to International Diabetes Federation (IDF), 371 million people have been reported with DM and the number is expected to rise to >552 million by 2030. The 2012 Indian statistics showed 63.0 million diabetic cases and a prevalence of 8.37% in adult population while a 4.0% prevalence of type 2 diabetes mellitus (T2DM) was reported in north Indian population (Banerjee and Saxena 2012).
There are considerable amounts of data indicating that the chronic elevation of plasma glucose causes many of the major complications of diabetes, including nephropathy, retinopathy, neuropathy, and macro- and microvascular damage (DeFronzo 1997). Increased levels of free fatty acids (FFAs) are positively correlated with both insulin resistance (McGarry 2002) and the deterioration of cell function in the context of concomitant hyperglycemia (Poitout and Robertson 2002). These latter effects may result from oxidative stress. There is evidence that oxidative stress, defined as a persistent imbalance between the production of highly reactive molecular species (chiefly oxygen and nitrogen) and antioxidant defenses, leads to tissue damage (Rosen et al. 2001). Oxidative stress results from increased content of ROS and/or reactive nitrogen species (RNS) (Ray Haldar and Bhattacharyya 2014). There are data indicating that ROS formation is a direct consequence of hyperglycemia (Brownlee 2001); more recent studies have suggested that increased FFA levels may also result in ROS formation. DNA, protein, and lipid, ROS are believed to play a key direct role in the pathogenesis of late diabetic complications (Rosen et al. 2001; Nishikawa et al. 2000). In addition to their ability to directly inflict macromolecular damage, ROS can function as signaling molecules to activate a number of cellular stress-sensitive pathways that cause cellular damage, and are ultimately responsible for the late complications of diabetes. These same pathways are linked to insulin resistance and decreased insulin secretion. In vivo studies have revealed that oxidative stress caused by hyperglycemia (and perhaps FFAs) occurs before the complications of diabetes become clinically evident (Rosen et al. 2001). Wolff and Dean (1987) suggested that non-enzymatic protein glycation, a mechanism proposed early on to account for glucose cytotoxicity, was dependent on ROS (superoxide and hydroxyl) formation through transition metal-catalyzed glucose auto oxidation. Research in numerous laboratories has indicated that hyperglycemia activates several major, well-characterized biochemical pathways that play a significant role in the etiology of diabetic complications. These pathways include AGEs and RAGE (Brownlee 2001), PKC (Koya and King 1998), and the polyol pathway (Stevens et al. 2000). More recently, hyperglycemia has been implicated in the activation of additional biochemical pathways, including the stress-activated signaling pathways of NF-ķβ, NH2-terminal Jun kinases/stress-activated protein kinases (JNK/SAPK), p38 mitogen-activated protein (MAP) kinase, and hexosamine. Data now indicate that activation of these pathways is linked not only to the development of the late complications of diabetes, but also to insulin resistance and β-cell dysfunction. There is certain evidence of the involvement of different oxidative stress-related genes such as SOD2, PON1, PON2, AKR1B1, AGE, and eNOS, in these pathways and they are regarded to harbor causal polymorphisms leading to diabetic microvascular complications. Considering the impact of these oxidative stress-related genes in diabetes pathogenesis, we have analyzed, in a pilot study, the role of 11 polymorphisms from 9 major genes involved in the maintenance of cellular redox balance and important physiological functions in the development of diabetes in populations from eastern India.
The study was initiated with demographic data of different clinical parameters such as BMI, fasting blood glucose level, PP sugar level, and HbA1C between diseased and healthy groups as recorded in the case history of outpatient department of government hospitals. All of the parameters significantly differed in mean values between cases and controls. In all aspects baseline values showed significant differences from endpoint values of clinical parameters. This fact supports the enhanced effect of clinical parameter before treatment in comparison to reduced effect of same parameter after treatment. However, the objective of present study was not only to clarify the means of different clinical parameters between diseased and healthy groups, but also to assess the disease pathogenesis with respect to different candidate genes along with their clinical impacts. Preliminarily this association study was conducted with 11 SNPs of 9 oxidative stress-related candidate genes with previous reports of their association in disease pathogenesis. Out of these 11 SNPs, statistically significant association was observed for SOD1 (rs2070424, A>G), PON1 (rs854573, A>G), PONII (rs6954345, G>C), RAGE −374 (rs1800624, T>A), and NOS3 (−786, T>C) in diabetic group compared against healthy controls (Table 4; Figs. 3, 4, 5). The associations observed in present study do not tally completely with other results of associations of same SNPs, in worldwide as well as in India. For example, previously in Indian population, RAGE −374 (rs1800624, T>A) promoter polymorphism was found to be associated in non-proliferative diabetic retinopathy subjects (Ramprasad et al. 2007) similar to the present observation. Our study failed to detect any association of RAGE G82S A/G and 1704G/T polymorphisms, whereas these two polymorphisms were found to be associated in the population of Japan (Matsunaga-Irie et al. 2004). The disparity of genetic association observed in regional populations of a country may be contributed by population heterogeneity as well as the limited sample size of the present study. However, the study also explored some similar patterns of results such as PON1 A>G polymorphism in Turkish population, in north Indian population with coronary artery disease (Ergun et al. 2011; Agrawal et al. 2009), and SOD1 A>G polymorphism in Chinese population. Tanus-Santos et al., examined the distribution of the T-786C, Glu298Asp, and 27 bp-VNTR variants of the eNOS gene in a sample of 305 individuals of different ethnicity (100 Caucasians, 100 African Americans, and 105 Asians). They found that the −786C variant was more common in Caucasians (42%) than in African Americans (18%) or Asians (14%), though only one study in Caucasians has been associated with an increased risk of hypertension (adjusted OR 1/4 2.16, 95% CI 1.3, 3.7) for individuals homozygous for the −786C allele (Tanus-Santos et al. 2001).
Each associated SNP obeyed the Hardy–Weinberg equilibrium and a dominant model of inheritance, with minor allele confirming the risk and relative risk of allele was in the range of 3.41–3.91 OR (95% CI >1). Again in each associated SNP the OR of rare homozygous genotype was much higher than heterozygous genotype and may be contributing to risk of rare allele when present in two copies in an individual. In support of this fact, a dominant model of inheritance in all associated SNPs conclude that homozygous for rare alleles are more susceptible to diabetes than homozygous of wild-type alleles and that the single copy of risk allele is sufficient for producing the disease pathogenesis.
A common feature observed in the present study was the excess of the major allele among the patients with T2DM (Table 4). This is intriguing considering the well-defined and important role of these genes in the maintenance of cellular homeostasis (Tiwari et al. 2009).
One of the drawbacks of the present investigation is that the lower power (0.6–0.7) in control groups than a larger power of diseased population (0.8–0.9). Statistical power is a function of the proportion of variation in exposure variable (genetic predictor) and the true causal association between exposure and outcome variable. Since the limitation of power may affect the results of association, different parametric tests such as t test and ANOVA and non-parametric Kruskal–Wallis test were conducted between case and control and in cases only, to assess the genotypic dependence of clinical parameters. All of the clinical parameters at first were log transformed to normalize the data and subjected to Pearson correlation test. Significant correlation was observed between BMI baseline and fasting sugar level baseline and endpoint data, between fasting sugar and PP sugar level among diabetic populations. The correlated parameters were then linearly regressed to nullify the probable impact of the factor that was found to be correlated. The residuals of each specific parameter was analyzed for association study. High level of fasting and PP sugar level, and lower HbA1C level in cases gave more consistent insights of association with disease stress. The non-parametric asymptomatic significance of mean differences in HbA1c level observed between different genotypic comparisons in case of SOD1 A>G (Ala9Val, rs2070424), PON2 (rs6954345 G>C), and RAGE rs1800624 T>A SNPs (Table 5) clearly demonstrates the genetic dependence of HbA1C level. The lower glycated hemoglobin contents in risk genotypes is supported by a recent study which hypothesized that substitution of fat for carbohydrate is associated with low concentrations of HbA1c in high calorie consuming type 2 diabetic patients (Shadman et al. 2013). The residuals of all the correlated parameters also revealed marginal differences in 11 versus 12 genotypes of PON1 A>G (rs854573) SNP (Table 6) in non-parametric tests. Therefore, the non-parametric Kruskal–Wallis test was found to be more supportive to explore the genotypic dependence of clinical parameters.
In haplotype analysis, the A-allele was coded by 0 and the G-allele by 1 for PON1, A>G (rs854573) SNP and the G-allele was coded by 0, and the C-allele by 2 for PON2 (rs6954345 G>C) SNP. A total of four haplotypes (00, 01, 10, 11) were observed in the patients and control samples with 00 as most common and reference haplotype (Table 7). The other three were considered as risk haplotypes. Haplotype 11 represented a greater odds ratio than two other haplotypes, when compared both with a single reference haplotype as well as against all other haplotypes pooled as single reference haplotype. The risk haplotype explored population characteristics in response to two linked markers with increased risk of GC haplotype.
We can conclude the oxidative stress to be an important controller in developing complications in type 2 diabetes subjects. The carriers of non-mutated and efficient alleles of oxidative stress-related genes are more likely to survive the comorbid complications and these alleles may be disease protective. The present study of 11 polymorphisms in 9 different genes identified 5 loci significantly associated with diabetic phenotypes in eastern Indian population. The genotype-based association of different clinical parameters such as BMI, fasting blood sugar level, HbA1C, revealed the metabolic nature of disease both in parametric and non-parametric manners. The outcome of the present study also indicates importance for further analysis of the risk associated genes, in the light of pharmacogenetic approach.
References
Adak S, Sengupta S, Chowdhury S, Bhattacharyya M (2010) Co existence of risk and protective haplotypes of Calpain 10 gene to type 2 diabetes in the eastern Indian population. Diab Vasc Dis Res 7:63–68
Agrawal S, Tripathi G, Prajnya R, Sinha N, Gilmour A, Bush L, Mastana S (2009) Paraxonase 1 gene polymorphisms contribute to coronary artery disease risk among north Indians. Ind J Med Sci 63:335–344
Altuner D, Suzen SH, Ates I, Koc GV, Aral Y et al (2011) Are PON1 Q/R 192 and M/L 55 polymorphisms risk factors for diabetes complications in Turkish population? Clin Biochem 44:372–376
Banerjee M, Saxena M (2012) An overview and molecular genetics of type 2 diabetes mellitus. In: Caplis I, Frangopoulos S (eds) Type 2 diabetes mellitus: causes, treatment and preventive strategies. Nova Science Publishers, New York
Baragetti I, Norata D, Sarcina C et al (2013) 374 T/A RAGE polymorphism is associated with chronic kidney disease progression in subjects affected by nephrocardiovascular disease. PLoS One 8:e0060089
Brownlee M (2001) Biochemistry and molecular cell biology of diabetic complications. Nature 414:813–820
Chen H, Li X, Epstein PN (2005) MnSOD and catalase transgenes demonstrate that protection of islets from oxidative stress does not alter cytokine toxicity. Diabetes 54:1437–1446
Costa LG, Cole TB, Jarvik GP, Furlong CE (2003) Functional genomics of the paraoxonase (PON1) polymorphisms: effects on pesticide sensitivity, cardiovascular disease, and drug metabolism. Annu Rev Med 54:371–392
DeFronzo RA (1997) Pathogenesis of type 2 diabetes: metabolic and molecular implications for identifying diabetes genes. Diabetes Rev 5:177–269
Del Prato S, Marchetti P (2004) Beta and alpha-cell dysfunction in type 2 diabetes. Horm Metab Res 36:775–781
Donaghue KC, Margan SH, Chan AK, Holloway B, Silink M, Rangel T, Bennetts B (2005) The association of aldose reductase gene (AKR1B1) polymorphisms with diabetic neuropathy in adolescents. Diabet Med 22:1315–1320
Ergun MA, Yurtcu E, Demirci H, Ilhan MN, Barkar V et al (2011) PON1 55 and 192 gene polymorphisms in type 2 diabetes mellitus patients in a Turkish population. Biochem Genet 49:1–8
Haber CA, Lam TK, Yu Z, Gupta N, Goh T, Bogdanovic E, Giacca A, Fantus IG (2003) N-acetylcysteine and taurine prevent hyperglycemia-induced insulin resistance in vivo: possible role of oxidative stress. Am J Physiol Endocrinol Metab 285:E744–E753
Kankova K, Sebekova K (2005) Genetic variability in the RAGE gene: possible implications for nutrigenetics, nutrigenomics, and understanding the susceptibility to diabetic complications. Mol Nutr Food Res 49:700–709
King GL, Loeken MR (2004) Hyperglycemia-induced oxidative stress in diabetic complications. Histochem Cell Biol 122:333–338
Koya D, King GL (1998) Protein kinase C activation and the development of diabetic complications. Diabetes 47:859–866
Leon CA, Raij L (2005) Interaction of haemodynamic and metabolic pathways in the genesis of diabetic nephropathy. J Hypertens 23:1931–1937
Maiese K, Morhan SD, Chong ZZ (2007) Oxidative stress biology and cell injury during type 1 and type 2 diabetes mellitus. Curr Neurovasc Res 4:63–71
Makiishi T, Araki S, Koya D, Maeda S, Kashiwagi A, Haneda M (2003) C-106T polymorphism of AKR1B1 is associated with diabetic nephropathy and erythrocyte aldose reductase content in Japanese subjects with type 2 diabetes mellitus. Am J Kidney Dis 42:943–951
Matsunaga-Irie S, Maruyama T, Yamamoto Y et al (2004) Relation between development of nephropathy and the p22phox C242T and receptor for advanced glycation end product G1704T gene polymorphisms in type 2 diabetic patients. Diabet Care 27:303–307
Mayer B, Hemmens B (1997) Biosynthesis and action of nitric oxide in mammalian cells. Trends Biochem Sci 22:477–481
McGarry JD (2002) Banting Lecture 2001. Dysregulation of fatty acid metabolism in the etiology of type 2 diabetes. Diabetes 51:7–18
Miller SA, Dykes DD, Polesky HF (1988) A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res 16(3):1215
Moore DJ, Gregory JM, Kumah-crystal YA, Simmons JH (2009) Mitigating micro- and macro-vascular complications of diabetes beginning in adolescence. Vasc Health Risk Manag 5:1015–1031
Nishikawa T, Edelstein D, Du XL, Yamagishi S, Matsumura T, Kaneda Y, Yorek MA, Beebe D, Oates PJ, Hammes HP, Giardino I, Brownlee M (2000) Normalizing mitochondrial superoxide production blocks three pathways of hyperglycaemic damage. Nature 404:787–790
Poitout V, Robertson RP (2002) Secondary beta-cell failure in type 2 diabetes—a convergence of glucotoxicity and lipotoxicity. Endocrinology 143:339–342
Prasad P, Tiwari AK, Prasanna K, Ammini AC, Gupta A, Gupta R, Thelma BK (2010) Association analysis of ADPRT1, AKR1B1, RAGE, GFPT2 and PAI-1 gene polymorphisms with chronic renal insufficiency among Asian Indians with type-2 diabetes. BMC Med Genet 11:52
Rachek LI, Thornley NP, Grishko VI, LeDoux SP, Wilson GL (2006) Protection of INS-1 cells from free fatty acid-induced apoptosis by targeting hOGG1 to mitochondria. Diabetes 55:1022–1028
Ramprasad S, Radha V, Mathias RA, Majumder PP, Rao MRS, Rema M (2007) RAGE gene promoter polymorphisms and diabetic retinopathy in a clinic-based population from South India. Eye 21:395–401
Ray Haldar S, Bhattacharyya M (2014) Lipid peroxidation products as predictors in disease progression. J Exp Integr Med 4:151–164
Richter RJ, Jarvik GP, Furlong CE (2010) Paraoxonase 1 status as a risk factor for disease or exposure. Adv Exp Med Biol 660:29–35
Rosen P, Nawroth PP, King G, Moller W, Tritschler HJ, Packer L (2001) The role of oxidative stress in the onset and progression of diabetes and its complications: a summary of a Congress Series sponsored by UNESCOMCBN, the American Diabetes Association, and the German Diabetes Society. Diabetes Metab Res Rev 17:189–212
Shadman Z, Khoshniat M, Poorsoltan N et al (2013) Association of high carbohydrate versus high fat diet with glycated haemoglobin in high calorie consuming type 2 diabetics. J Diabetes Metab Disord 12:27
Sheetz MJ, King GL (2002) Molecular understanding of hyperglycemia’s adverse effects for diabetic complications. J Am Med Assoc 288:2579–2588
Sivenius K, Niskanen L, Voutilainen-Kaunisto R, Laakso M, Uusitupa M (2004) Aldose reductase gene polymorphisms and susceptibility to microvascular complications in Type 2 diabetes. Diabet Med 21:1325–1333
Stevens MJ, Obrosova I, Feldman EL, Greene DA (2000) The sorbitol-osmotic and sorbitol-redox hypothesis. In: LeRoith D, Taylor SI, Olefsky JM (eds) Diabetes mellitus: a fundamental and clinical text. Lippincott Williams & Wilkins, Philadelphia
Tanus-Santos JE, Desai M, Flockhart DA (2001) Effect of ethnicity on the distribution of clinically relevant endothelial nitric oxide variants. Pharmacogenetics 11:719–725
Thameem F, Puppala S, Arar NH, Stern MP, Blangero J, Duggirala R, Abboud HE (2008) Endothelial nitric oxide synthase (eNOS) gene polymorphisms and their association with type 2 diabetes-related traits in Mexican Americans. Diab Vasc Dis Res 5:109–113
Tiwari AK, Prasad P, Thelma BK, Prasanna Kumar KM, Ammini AC, Gupta A, Gupta R (2009) Oxidative stress pathway genes and chronic renal insufficiency in Asian Indians with Type 2 diabetes. J Diabetes Complicat 23:102–111
Wang Y, Ng MC, Lee SC, So WY, Tong PC, Cockram CS, Critchley JA, Chan JC (2003) Phenotypic heterogeneity and associations of two aldose reductase gene polymorphisms with nephropathy and retinopathy in type 2 diabetes. Diabetes Care 26:2410–2415
Wild S, Roglic G, Green A, Sicree R, King H (2004) Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 27:1047–1053
Wolff SP, Dean RT (1987) Glucose autoxidation and protein modification: the potential role of autoxidative glycosylation’ in diabetes. Biochem J 245:243–250
Yano M, Hasegawa G, Ishii M, Yamasaki M, Fukui M, Nakamura N, Yoshikawa T (2004) Short-term exposure of high glucose concentration induces generation of reactive oxygen species in endothelial cells: implication for the oxidative stress associated with postprandial hyperglycemia. Redox Rep 9:111–116
Acknowledgments
We acknowledge Dr. D. S. Kothari Fellowship Scheme, UGC for providing fellowship to the first author. We are grateful to UGC-CAS, DST-FIST, World bank ICZM funding in Dept. of Biochemistry for providing infrastructure and instrumental facilities. We feel our heartfelt gratitude to Prof. Saugata Sen Roy, Dept. of Statistics, C. U. for his continuous assistance in statistical aspects. We are grateful to all of the patients and volunteer donors for providing their blood sample to us; we regret our inability to mention them individually.
Conflict of interest
The authors report no conflicts of interest.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Haldar, S.R., Chakrabarty, A., Chowdhury, S. et al. Oxidative Stress-Related Genes in Type 2 Diabetes: Association Analysis and Their Clinical Impact. Biochem Genet 53, 93–119 (2015). https://doi.org/10.1007/s10528-015-9675-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10528-015-9675-z