Abstract
Mutations in SLC26A4 cause either syndromic or nonsyndromic hearing loss. We identified a link between hearing loss and DFNB4 in 3 of the 50 families participating in this study. Sequencing analysis revealed two SLC26A4 mutations, p.V239D and p.S57X, in affected members of the 3 families. These mutations have been previously reported in deaf individuals from the subcontinent, all of whom manifested profound deafness. The patients investigated in our study exhibited moderate to severe hearing loss. Our results show that inactivating SLC26A4 mutations that cause profound deafness can also be involved in the etiology of moderate to severe hearing loss. The type of mutation cannot predict the severity of the hearing loss in all cases, and there may be additional epistatic interactions that could modify the phenotype.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hearing loss is one of the most prevalent sensory impairments in humans. Hundreds of syndromic and nonsyndromic forms of deafness have been described. Pendred syndrome (MIM 274600) involves sensorineural hearing loss along with enlarged vestibular aqueduct and also includes thyroid dysfunction, which can be manifested as a goiter (Pendred 1896). DFNB4 (MIM 600791) is described as nonsyndromic deafness with enlarged vestibular aqueduct (Li et al. 1998). Recessively inherited mutations in SLC26A4 cause both Pendred syndrome and DFNB4 (Li et al. 1998; Everett et al. 1997).
SLC26A4 encodes pendrin, a membrane protein of 85 kDa comprising 780 amino acids. It functions in mediating the exchange of chloride with bicarbonate, formate, and iodide (Scott et al. 1999). SLC26A4 is expressed in the thyroid (Royaux et al. 2000), the inner ear (Everett et al. 1999), and the kidney (Soleimani et al. 2001). More than 300 mutations of the gene causing hearing loss have been described. These include missense, nonsense, splice site, and frameshift mutations.
To understand the role of SLC26A4 in the pathogenesis of the inner ear, researchers have generated many mouse mutants that have engineered mutations or lack the gene. These include two knockout Slc26a4 −/− mice (Everett et al. 2001; Kim and Wangemann 2011) and two knock-in mice: Slc26a4 loop/loop with the engineered missense mutation p.S408F (Dror et al. 2010) and Slc26a4 tm1Dontuh/tm1Dontuh with the c.919-2 A→G mutation (Lu et al. 2011). The loss of hearing in these mouse models is profound in degree and offers no clues to the molecular basis of the observed differences in hearing thresholds due to a few particular SLC26A4 mutations in humans. Experiments with transgenic mice Tg[E];Tg[R];Slc26a4 Δ/Δ, however, in which Slc26a4 expression is inducible by doxycycline on a background of absent endogenous pendrin, have demonstrated that expression of Slc26a4 at early embryonic stages of E0-E17.5 is required for acquisition of normal hearing in these mice (Choi et al. 2011). Ablating expression of Slc26a4 at the early embryonic stages results in complete hearing loss in the mice, and its absence in early postnatal stages results in partial hearing loss. This variability in hearing loss recapitulates the phenotypes documented for many humans with mutations in SLC26A4.
It has been suggested that many missense mutations affect pendrin function severely and cause profound deafness, whereas some mutations (p.V480D, p.V653A) retain residual function of pendrin and cause a less severe phenotype (Campbell et al. 2001). Moreover, nonsense mutations usually result in profound deafness. We have found, however, that identical mutations in SLC26A4, previously known to cause profound deafness, can also result in moderate to severe hearing loss in humans.
Materials and Methods
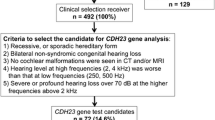
Three consanguineous families from Pakistan, HLRB2, HLRB7, and HLRB10, were recruited as part of a larger study on the genetics of moderate to severe hearing loss, which included 47 additional families from Pakistan with less than profound hearing loss. All families had multiple affected individuals. Approval was obtained from the institutional review board of the School of Biological Sciences, University of the Punjab, Lahore. Samples were obtained with written informed consent from all participants or from their parents in the case of children. DNA was extracted from blood samples from the participants (Grimberg et al. 1989; Miller et al. 1988).
Clinical Investigation
Detailed medical examinations and histories were completed for the participants. HLRB2 was a consanguineous family with three affected children aged 8–11 years. HLRB7 had five affected individuals aged 14–70 years, and HLRB10 had three affected individuals, aged 9–14 years, in a single consanguineous loop (Fig. 1). Hearing status was evaluated by pure tone audiometry using a portable audiometer (Danplex DA65, Denmark). Hearing was evaluated at frequencies of 250, 500, 1,000, 2,000, 4,000, and 8,000 Hz. The severity of hearing loss was graded according to hearing thresholds: mild (20–40 dB), moderate (41–55 dB), moderately severe (56–70 dB), severe (71–90 dB), and profound (95–120 dB) (Smith et al. 2005). Vestibular function was assessed by Romberg and tandem gait tests. Thyroid status was evaluated by palpation.
Genotyping and Sequencing
We sequenced the coding exon of GJB2 and genotyped DNA samples from all 50 families with microsatellite markers specific for 16 deafness loci, including DFNB4. These loci were known to be either a common cause of deafness in Pakistan or responsible for less severe or progressive hearing loss in humans. Genotyping data were analyzed using GeneMapper ID version 3.2 (Applied Biosystems, Foster City, CA). Two-point likelihood of odds (LOD) scores for each marker were calculated using the MLink program of the Linkage package (Terwilliger and Ott 1994). Deafness was coded as a fully penetrant recessive disorder with a disease allele frequency of 0.001.
The 21 exons of SLC26A4 and their flanking intronic regions greater than 60 bp were PCR-amplified with specifically designed primers. The PCR products were treated with exonuclease I and shrimp alkaline phosphatase (Fermentas, Glen Burnie, MD) to remove excess primer and dNTPs. Sequencing was completed with a BigDye Terminator version 3.1 Cycle Sequencing Kit (Applied Biosystems) as described previously (Malik et al. 2010).
Results
Subjects and Clinical Investigation
Clinical history, interviews, and physical examinations revealed no apparent phenotype except hearing loss in the participants. Palpable goiters were absent in the individuals with hearing loss. Pure tone audiometry revealed moderate to severe sensorineural hearing loss in all affected individuals in families HLRB2, HLRB7, and HLRB10 (Fig. 2). Romberg and tandem gait tests were normal, suggesting that vestibular function was not impaired.
Pure tone audiograms for three children of family HLRB2 (top), two children of family HLRB7 (center), and three children of family HLRB10 (bottom). All affected individuals (identified by codes in Fig. 1) have moderate to severe hearing loss. Hearing thresholds are depicted for the left ear (solid lines) and the right ear (dotted lines)
Genotyping and Mutational Analysis
Genotyping with microsatellite markers and haplotype analysis of the affected members in the three families revealed linkage of hearing loss to the DFNB4/PDS locus on chromosome 7q31. Markers D7S2459, D7S2420, and D7S496 were homozygous in affected individuals and heterozygous in the obligate carriers. Maximum two-point LOD scores of 2.5 were obtained with markers D7S2459 and D7S2420 at recombination fraction θ = 0 for family HLRB2. For family HLRB7, marker D7S496 yielded an LOD score of 3.5. Markers D7S2420 and D7S496 supported an LOD score of 1.6 for family HLRB10. Hearing loss did not segregate with markers specific for DFNB4/PDS in any of the other 47 participating families.
We sequenced the 21 exons of SLC26A4 from one affected individual for each family demonstrating linkage to DFNB4/PDS. Two mutations were identified in SLC26A4 that were subsequently determined to segregate with hearing loss in members of families HLRB2, HLRB7, and HLRB10 (Fig. 3). The transversion mutation c.716 T→A (p.V239D) was detected in exon 6, on both alleles of SLC26A4, in affected individuals of HLRB2 and HLRB7. This mutation is predicted to affect transmembrane domain 5 of SLC26A4. Another transversion mutation, c.170 C→A, was identified in exon 3 of SLC26A4 as a homozygous mutation among affected members of family HLRB10. This mutation causes termination of pendrin at amino acid 57 (p.S57X). The termination occurs at the amino terminus of SLC26A4, and the protein is predicted to lack most of the important domains.
Discussion
Mutations in SLC26A4 are a common cause of hearing loss in humans, with no single prevalent mutation worldwide. A few mutations, however, are specifically found in particular ethnic groups in some populations (Park et al. 2003; Tsukamoto et al. 2003). Mutations in SLC26A4 are one of the most common causes of recessively inherited profound deafness in Pakistan, accounting for 7.2% of the disorder (Anwar et al. 2009). Our results demonstrate that the ratio of SLC26A4 mutations is similarly high in individuals with less than profound deafness in Pakistan and account for hearing loss in 6% of the families in our cohort.
Previously, a few splice site mutations in SLC26A4 have been reported to cause intrafamilial variability in degree of hearing loss (Van Hauwe et al. 1998). These splice site mutations affect the C-terminus of SLC26A4 and are hypothesized to produce truncated proteins, which may maintain the residual function of pendrin and therefore could explain the presence of less severe phenotype in the affected patients (Van Hauwe et al. 1998). Moreover, two mutations, IVS4+7 A→G (Lopez-Bigas et al. 1999) and IVS8+4 A→G (Park et al. 2003), have been described that affect nucleotides away from the canonical splice junction sequences and create new splice sites within SLC26A4. The use of these newly created splice sites leads to frameshifts of the open reading frame of SLC26A4. It is hypothesized that some correctly spliced SLC26A4 may still be produced, since the actual splice sites are intact. The presence of residual wild-type SLC26A4 may explain the less severe hearing loss observed in some patients in families with these mutations (Lopez-Bigas et al. 1999).
Hearing loss associated with Pendred syndrome is profound. Nonsyndromic deafness (DFNB4) may be profound or may vary from mild to moderate in degree. Mutations p.T416P, p.L236P, and p.E384G (Campbell et al. 2001; Van Hauwe et al. 1998), which cause Pendred syndrome, have been demonstrated to result in retention of pendrin within the endoplasmic reticulum in an in vitro functional study. Because three frequent mutations observed in Caucasians and associated with DFNB4 (p.V653A and p.I490L/p.G497S) allow continued pendrin activity (Scott and Karniski 2000; Rotman-Pikielny et al. 2002), it has been hypothesized to constitute the difference between mutations that cause Pendred syndrome or DFNB4. Other SLC26A4 mutations in patients with nonsyndromic hearing loss also cause the retention of protein in the endoplasmic reticulum (Taylor et al. 2002). The mutation p.V239D has been described in Pakistani, Indian (Park et al. 2003), Turkish, and Palestinian families (Fitoz et al. 2007; Tekin et al. 2003; Walsh et al. 2006). It is involved in the etiology of both Pendred syndrome and DFNB4. Trafficking of wild-type and intracellular localization of mutant (p.V239D) pendrin has also been evaluated, showing that p.V239D mutant protein is retained in the endoplasmic reticulum and wild-type protein is targeted to the plasma membrane (Walsh et al. 2006). A similar spectrum of mutations in Pendred syndrome and the DFNB4 population contradicts the molecular study of pendrin. It has been hypothesized that since in vitro functional studies show outcomes for single mutations, other factors (including intervention of regulatory elements, modifier genes, or nutrition affecting iodine uptake) may determine the thyroid phenotype in vivo (Albert et al. 2006).
The mutation p.S57X has previously been reported only in deaf individuals from Pakistan and India (Anwar et al. 2009; Park et al. 2003) and may be confined to the subcontinent because of a founder effect. Previously, the nonsense mutations p.K440X and p.Q514X were reported to cause less severe hearing loss, each in one of two affected individuals (Wang et al. 2007). It was hypothesized that the p.K440X mutation affects transmembrane domain 10 and that p.Q514X affects the carboxy terminus of SLC26A4, conserving many of the functional domains of the protein. This may be sufficient for preserving some degree of hearing. All other reported truncating mutations (p.S23X, p.E37X, and p.S57X) cause profound deafness. In family HLRB10, the p.S57X mutation is associated with moderate to severe hearing loss, even though no functional pendrin is predicted to be present in the affected members, either because the most important protein domains are lacking or because of nonsense-mediated decay of the SLC26A4 transcript.
Identification of identical mutations (p.V239D, p.S57X) in both those individuals with profound deafness and those with moderate to severe hearing loss (Table 1) suggests that the effects of some pathogenic mutations in SLC26A4 may be modified by genetic and epigenetic factors. Research on individuals from other populations segregating moderate to severe hearing loss should reveal whether additional missense and nonsense mutations in SLC26A4 can cause similar variability in hearing thresholds.
References
Albert S, Blons H, Jonard L, Feldmann D, Chauvin P, Loundon N, Sergent-Allaoui A, Houang M, Joannard A, Schmerber S, Delobel B, Leman J, Journel H, Catros H, Dollfus H, Eliot MM, David A, Calais C, Drouin-Garraud V, Obstoy MF, Tran Ba Huy P, Lacombe D, Duriez F, Francannet C, Bitoun P, Petit C, Garabedian EN, Couderc R, Marlin S, Denoyelle F (2006) SLC26A4 gene is frequently involved in nonsyndromic hearing impairment with enlarged vestibular aqueduct in caucasian populations. Eur J Hum Genet 14:773–779
Anwar S, Riazuddin S, Ahmed ZM, Tasneem S, Ateeq ul J, Khan SY, Griffith AJ, Friedman TB, Riazuddin S (2009) SLC26A4 mutation spectrum associated with DFNB4 deafness and Pendred’s syndrome in Pakistanis. J Hum Genet 54:266–270
Campbell C, Cucci RA, Prasad S, Green GE, Edeal JB, Galer CE, Karniski LP, Sheffield VC, Smith RJ (2001) Pendred syndrome, DFNB4, and PDS/SLC26A4 identification of eight novel mutations and possible genotype–phenotype correlations. Hum Mutat 17:403–411
Choi BY, Kim HM, Ito T, Lee KY, Li X, Monahan K, Wen Y, Wilson E, Kurima K, Saunders TL, Petralia RS, Wangemann P, Friedman TB, Griffith AJ (2011) Mouse model of enlarged vestibular aqueducts defines temporal requirement of Slc26a4 expression for hearing acquisition. J Clin Invest 121:4516–4525
Dror AA, Politi Y, Shahin H, Lenz DR, Dossena S, Nofziger C, Fuchs H, Hrabe de Angelis M, Paulmichl M, Weiner S, Avraham KB (2010) Calcium oxalate stone formation in the inner ear as a result of an Slc26a4 mutation. J Biol Chem 285:21724–21735
Everett LA, Glaser B, Beck JC, Idol JR, Buchs A, Heyman M, Adawi F, Hazani E, Nassir E, Baxevanis AD, Sheffield VC, Green ED (1997) Pendred syndrome is caused by mutations in a putative sulphate transporter gene (PDS). Nat Genet 17:411–422
Everett LA, Morsli H, Wu DK, Green ED (1999) Expression pattern of the mouse ortholog of the Pendred’s syndrome gene (Pds) suggests a key role for pendrin in the inner ear. Proc Natl Acad Sci USA 96:9727–9732
Everett LA, Belyantseva IA, Noben-Trauth K, Cantos R, Chen A, Thakkar SI, Hoogstraten-Miller SL, Kachar B, Wu DK, Green ED (2001) Targeted disruption of mouse Pds provides insight about the inner-ear defects encountered in Pendred syndrome. Hum Mol Genet 10:153–161
Fitoz S, Sennaroglu L, Incesulu A, Cengiz FB, Koc Y, Tekin M (2007) SLC26A4 mutations are associated with a specific inner ear malformation. Int J Pediatr Otorhinolaryngol 71:479–486
Grimberg J, Nawoschik S, Belluscio L, McKee R, Turck A, Eisenberg A (1989) A simple and efficient non-organic procedure for the isolation of genomic DNA from blood. Nucl Acids Res 17:8390
Kim HM, Wangemann P (2011) Epithelial cell stretching and luminal acidification lead to a retarded development of stria vascularis and deafness in mice lacking pendrin. PLoS ONE 6:e17949
Li XC, Everett LA, Lalwani AK, Desmukh D, Friedman TB, Green ED, Wilcox ER (1998) A mutation in PDS causes non-syndromic recessive deafness. Nat Genet 18:215–217
Lopez-Bigas N, Rabionet R, de Cid R, Govea N, Gasparini P, Zelante L, Arbones ML, Estivill X (1999) Splice-site mutation in the PDS gene may result in intrafamilial variability for deafness in Pendred syndrome. Hum Mutat 14:520–526
Lu YC, Wu CC, Shen WS, Yang TH, Yeh TH, Chen PJ, Yu IS, Lin SW, Wong JM, Chang Q, Lin X, Hsu CJ (2011) Establishment of a knock-in mouse model with the SLC26A4 c.919-2A > G mutation and characterization of its pathology. PLoS ONE 6:e22150
Malik S, Kakar N, Hasnain S, Ahmad J, Wilcox E, Naz S (2010) Epidemiology of Van der Woude syndrome from mutational analyses in affected patients from Pakistan. Clin Genet 78:247–256
Miller S, Dykes D, Polesky H (1988) A simple salting out procedure for extracting DNA from human nucleated cells. Nucl Acids Res 16:1215
Park HJ, Shaukat S, Liu XZ, Hahn SH, Naz S, Ghosh M, Kim HN, Moon SK, Abe S, Tukamoto K, Riazuddin S, Kabra M, Erdenetungalag R, Radnaabazar J, Khan S, Pandya A, Usami SI, Nance WE, Wilcox ER, Riazuddin S, Griffith AJ (2003) Origins and frequencies of SLC26A4 (PDS) mutations in east and south Asians: global implications for the epidemiology of deafness. J Med Genet 40:242–248
Pendred V (1896) Deaf-mutism and goitre. Lancet 2:532
Rotman-Pikielny P, Hirschberg K, Maruvada P, Suzuki K, Royaux IE, Green ED, Kohn LD, Lippincott-Schwartz J, Yen PM (2002) Retention of pendrin in the endoplasmic reticulum is a major mechanism for Pendred syndrome. Hum Mol Genet 11:2625–2633
Royaux IE, Suzuki K, Mori A, Katoh R, Everett LA, Kohn LD, Green ED (2000) Pendrin, the protein encoded by the Pendred syndrome gene (PDS), is an apical porter of iodide in the thyroid and is regulated by thyroglobulin in FRTL-5 cells. Endocrinology 141:839–845
Scott DA, Karniski LP (2000) Human pendrin expressed in Xenopus laevis oocytes mediates chloride/formate exchange. Am J Physiol Cell Physiol 278:C207–C211
Scott DA, Wang R, Kreman TM, Sheffield VC, Karniski LP (1999) The Pendred syndrome gene encodes a chloride-iodide transport protein. Nat Genet 21:440–443
Smith R, Bale J, White K (2005) Sensorineural hearing loss in children. Lancet 365:879–890
Soleimani M, Greeley T, Petrovic S, Wang Z, Amlal H, Kopp P, Burnham CE (2001) Pendrin: an apical Cl−/OH−/HCO3 − exchanger in the kidney cortex. Am J Physiol Renal Physiol 280:F356–F364
Taylor JP, Metcalfe RA, Watson PF, Weetman AP, Trembath RC (2002) Mutations of the PDS gene, encoding pendrin, are associated with protein mislocalization and loss of iodide efflux: implications for thyroid dysfunction in Pendred syndrome. J Clin Endocrinol Metab 87:1778–1784
Tekin M, Akcayoz D, Comak E, Bogoclu G, Duman T, Fitoz S, Ilhan I, Akar N (2003) Screening the SLC26A4 gene in probands with deafness and goiter (Pendred syndrome) ascertained from a large group of students of the schools for the deaf in Turkey. Clin Genet 64:371–374
Terwilliger JD, Ott J (1994) Handbook of human genetic linkage. Johns Hopkins University Press, Baltimore
Tsukamoto K, Suzuki H, Harada D, Namba A, Abe S, Usami S (2003) Distribution and frequencies of PDS (SLC26A4) mutations in Pendred syndrome and nonsyndromic hearing loss associated with enlarged vestibular aqueduct: a unique spectrum of mutations in Japanese. Eur J Hum Genet 11:916–922
Van Hauwe P, Everett LA, Coucke P, Scott DA, Kraft ML, Ris-Stalpers C, Bolder C, Otten B, de Vijlder JJ, Dietrich NL, Ramesh A, Srisailapathy SC, Parving A, Cremers CW, Willems PJ, Smith RJ, Green ED, Van Camp G (1998) Two frequent missense mutations in Pendred syndrome. Hum Mol Genet 7:1099–1104
Walsh T, Abu Rayan A, Abu Saed J, Shahin H, Shepshelovich J, Lee MK, Hirschberg K, Tekin M, Salhab W, Avraham KB, King MC, Kanaan M (2006) Genomic analysis of a heterogeneous Mendelian phenotype: multiple novel alleles for inherited hearing loss in the Palestinian population. Hum Genomics 2:203–211
Wang QJ, Zhao YL, Rao SQ, Guo YF, Yuan H, Zong L, Guan J, Xu BC, Wang DY, Han MK, Lan L, Zhai SQ, Shen Y (2007) A distinct spectrum of SLC26A4 mutations in patients with enlarged vestibular aqueduct in China. Clin Genet 72:245–254
Acknowledgments
We are grateful to the study participants for their cooperation. We thank Dr. Thomas Friedman for providing some of the primers used in this research. The work was funded by grant no. R01TW007608 from the Fogarty International Center and National Institute of Deafness and Other Communication Disorders, National Institutes of Health, USA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Khan, M.R., Bashir, R. & Naz, S. SLC26A4 Mutations in Patients with Moderate to Severe Hearing Loss. Biochem Genet 51, 514–523 (2013). https://doi.org/10.1007/s10528-013-9582-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10528-013-9582-0