Abstract
An age-dependent decline in skeletal muscle mass, strength, and endurance during the aging process is a physiological development, but several factors may exacerbate this process, leading to the threatening state of sarcopenia, frailty, and eventually higher mortality rates. Obesity appears to be such a promoting factor and has been linked in several studies to sarcopenia. The reason for this causal association remains poorly understood. Notwithstanding the fact that a higher body mass might simply lead to diminished physical activity and therefore contribute to a decline in skeletal muscle, several molecular mechanisms have been hypothesized. There could be an obesity derived intracellular lipotoxicity (i.e., elevated intramuscular levels of lipids and their derivatives), which induces apoptosis by means of an elevated oxidative stress. Paracrine mechanisms and inflammatory cytokines, such as CRP and IL-6 could be confounders of the actual underlying pathological mechanism. Due to a cross-talk of the hypothalamo-pituitary axis with nutritional status, obese subjects are more in a catabolic state of metabolism, with a higher susceptibility to muscle wasting under energy restriction. Obesity induces insulin resistance in the skeletal muscle, which consequently leads to perturbed metabolism, and misrouted signaling in the muscle cells. In obesity, muscle progenitor cells could differentiate to an adipocyte-like phenotype as a result of paracrine signals from (adipo)cytokines leading to a reduced muscular renewal capacity. The present review outlines current knowledge concerning possible pathways, which might be involved in the molecular pathogenesis of sarcopenic obesity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
As we age, skeletal muscle mass and muscle function (strength and/or performance) progressively decline. Sarcopenia in the strict sense refers to a status in which this decline exceeds normal age-dependent development (Cruz-Jentoft et al. 2010; Fielding et al. 2011). Sarcopenia is a functionally relevant decline of muscle mass and function and is closely related to physical disability and a propensity to have falls and has even been linked to increased mortality (Cooper et al. 2011; Landi et al. 2013; Batsis et al. 2014). Sarcopenia is also regarded as being a major component of frailty and may be promoted by disuse, altered endocrine function, chronic diseases, inflammation, insulin resistance, and malnutrition (Baumgartner 2000; Bouchard et al. 2009; Bollheimer et al. 2012; Volkert and Sieber 2011). In the development of sarcopenia atrophy of muscle fibers, especially type II fibers occurs and the number of motor neuron decreases (Muscaritoli et al. 2010). Currently, there are two major consensus definitions for the diagnosis of sarcopenia. Both the European Working Group on Sarcopenia in Older People (EWGSOP) and the International Working Group on Sarcopenia recommend objectively measured low appendicular muscle mass and diminished gait speed (either ≤ 0.8 or <1 m/s) for diagnosing of sarcopenia (Cruz-Jentoft et al. 2010; Fielding et al. 2011). In addition to these two key components of muscle mass and muscle performance, the European definition suggests quantifying hand grip strength as a surrogate of muscle power for further inclusion of patients with normal walking speed, but low muscle mass (Cruz-Jentoft et al. 2010). Notwithstanding these accepted standards for the operationalization of sarcopenia, most studies published in this field have used individually adjusted classifications. Consequently, the prevalence of sarcopenia differs considerably from about 10 % to over 80 % in individuals older than 60 years (Batsis et al. 2013).
Aging is not only accompanied by a decline in muscle mass, but is also associated with an increasing fat mass, resulting in lower physical activity (Baumgartner 2000). Fat distribution changes with age so that there is an increase in visceral fat but also fat deposits occurs in skeletal muscle, the liver, heart and pancreas (Sakuma and Yamaguchi 2013; Wei et al. 2006; Shimabukuro et al. 1998; Sparangna and Hickson-bick 2000; Garris 2005; Summers 2006). Obesity is characterised by endocrine changes and visceral fat deposits produce more pro-inflammatory adipokines leading to a low-grade inflammatory state (Schrager et al. 2007). Loss of lean body mass, reduced immune function, cognitive decline, accelerated atherosclerosis and insulin resistance are the consequences of this low-grade inflammatory state (Kennedy et al. 2004; Zamboni et al. 2005; Florez and Troen 2008; Zamboni et al. 2008; Waters et al. 2010). Increased levels of inflammatory molecules like TNFα and IL-6 have catabolic effects on skeletal muscle mass and are involved in sarcopenia (Zamboni et al. 2008; Waters et al. 2010).
Sarcopenic obesity denotes the combination of sarcopenia and obesity, which means a concomitant overriding of abnormal age-dependent muscle loss and fat accumulation (Baumgartner et al. 2004; Bouchard et al. 2009). In a landmark study by Rolland and colleagues, it was shown that sarcopenic obesity, in particular, leads to an increase in functional impairment, which was higher for sarcopenic obesity than either sarcopenia or obesity alone (Rolland et al. 2009). Since about three out of four European adults are overweight, obesity will become an important challenge for the health system in the near future (Doak et al. 2012). However, just as for sarcopenia, many discrepant definitions have been used for the classification of obesity, especially in the context of compound sarcopenic obesity. In a recent cross-sectional analysis of non-institutionalized persons in the United States who took part in the National Health and Nutrition Examination Surveys 1999–2004 the prevalence of sarcopenic obesity was examined with eight different definitions from former studies. Consequently, the percentage of participants over the age of 60 years meeting the criteria of sarcopenic obesity reached 4.4–84.0 % for men and 3.6–94.0 % for women (Batsis et al. 2013). Against this background of observational studies, it should also be noted that, up until now, obesity has not been proven to be an independent risk factor for sarcopenia (Rolland et al. 2009; Baumgartner 2000). Nevertheless, some clinical studies have indicated that insulin resistance may underlie the development of sarcopenia and inflammatory (adipo)cytokines, as well as growth hormone, testosterone, and high levels of circulating free fatty acids appear to play a role in the development of sarcopenic obesity (Stenholm et al. 2008a). In addition, laboratory research has suggested some pathways and potential culprits that might link obesity with pathological muscle loss (Stenholm et al. 2008a). Therefore, a closer look at the molecular pathology of sarcopenia in the context of accompanying obesity might be helpful in distinguishing between causes, consequences, and potential confounders of these co-morbidities.
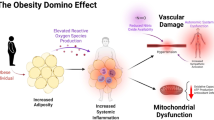
Pathways potentially involved in the pathogenesis of sarcopenic obesity are highlighted in Fig. 1.
The figure presents possible pathways involved in sarcopenic obesity. Pathways which favour proper functionality of the skeletal muscle are depicted in blue, blocking of these pathways by obesity is shown in red. An excess of fatty acids in the organism leads to apoptosis of pancreatic β-cells (green) and consequently to reduced secretion of insulin. This results in deregulation of the muscular PKB/Akt pathway and a decreased translocation of GLUT4 transporters leading to insulin insensitivity. Moreover, protein turnover is altered due to changes in S6K1 activity. Secretion of IL-15, a paracrine anabolic myokine, is suppressed by adipose tissue. Hence, TNFα induces muscle atrophy by stimulation of apoptosis as well as by upregulation of the proteasomal decay of filament proteins. Satellite cells dedifferentiate to an adipocyte-like phenotype stunting regeneration of muscle fibres. (Color figure online)
Excessive accumulation of fatty acids and their derivates (IMCL)
Up to 50 % of the body weight of young adults is lean muscle mass. During aging, approximately half of this muscle mass vanishes. In parallel, fat mass—particularly visceral fat—increases (Sakuma and Yamaguchi 2013). The excess of fat(ty acids) is not only stored in adipocytes, but can also spill over to several other tissues such as the liver, heart, pancreas, or skeletal muscle (Shimabukuro et al. 1998; Sparangna and Hickson-bick 2000; Garris 2005; Summers 2006; Wei et al. 2006). According to a broader interpretation of the theory of lipotoxicity, the intracellular oversupply of fat and/or its derivatives could be a reason not only for insulin resistance, but also for the decline in muscle mass in obesity. In the heart, liver, and pancreas, corresponding mechanisms of apoptotic deterioration due to an intracellular excess of fatty acids have been described. (Shimabukuro et al. 1998; Sparangna and Hickson-bick 2000; Garris 2005; Summers 2006; Wei et al. 2006). Muscle morphology, size, and function may also be altered by a high uptake and storage of fatty acids. In obesity, high circulating levels of lipids accumulate in skeletal muscle as triacylglycerol or derivates, such as diacylglycerol (DAG), long chain acyl CoA, and ceramide (Adams et al. 2004; Watt et al. 2006). These intramyocellular lipids (IMCL) are associated with decreased insulin sensitivity (Jacob et al. 1999; Krssak et al. 1999). DAG, long chain acyl CoA, and ceramides are a biochemical link between increase in IMCL and insulin resistance (Griffin et al. 1999; Choi et al. 2008). These molecules can interact directly or indirectly with different targets of the insulin signalling pathway, e.g., insulin-receptor substrate or protein kinase B and may inhibit insulin signal transduction (Consitt et al. 2009). Increase in fat(ty) acids, as a result of a diet with a high fat content, and/or adipositas, is responsible for an increase in IMCL in the context of insulin resistance. A high concentration of fatty acids also has a toxic effect on β-cell function. Lipids, especially saturated palmitic acid, induce β-cell apoptosis and reduce proliferation in pancreatic islets leading to decreased insulin secretion (Van Herpen and Schrauwen-Hinderling 2008). Elevated levels of palmitic acid correlate with de novo synthesis of ceramides and cause activation of apoptotic pathways in several cell types, including the β-cells (Van Herpen and Schrauwen-Hinderling 2008).
In addition, the translocation of the glucose transport protein GLUT4 to the membrane is blocked, lowering the storage capacity of muscle cells for blood glucose (Kusminski et al. 2009). As a consequence, IMCL and not glucose is used preferentially as an energy source in skeletal muscle. In the case of a permanent positive fat balance, the storage of intracellular fat is also not balanced by an increased oxidative capacity (Goodpaster et al. 2001). Accordingly, diabetes develops as a result of a high fat content and produces metabolic dysregulation of the muscle, finally leading to sarcopenia.
However, an age-dependent increase in IMCL is primarily based on mitochondrial dysfunction, which it is claimed is an essential element of the pathogenesis of sarcopenia (Reznick et al. 2007). Mitochondrial dysfunction is generated by different processes and has various molecular, cell-biological and cytological levels. For the development of sarcopenia, increased reactive oxygen species formation (ROS), an age-dependent decrease in central mitochondrial regulator peroxisome-proliferator-activated-receptor-γ coactivator 1 α (PGC-1α) and induced mitochondrial apoptosis of muscle cells are important (Harman 1956; Anderson and Prolla 2009; Marzetti et al. 2010). Apart from lipids, mitochondrial DNA (mtDNA) may be a target for oxidative stress (Herbst et al. 2007). Oxidative damage to mtDNA has a close link to reduced ATP production, which relates to a possible pathomechanism in the development of sarcopenia. Transcription factor PGC-1α decreases ROS formation (St-Pierre et al. 2006), equilibrates lipid oxidation and synthesis with direct effects on IMCL levels (Espinoza et al. 2010) and promotes mitochondrial biogenesis (Wende et al. 2007). An animal model has suggested a functional connection between an age-dependent decrease in PGC-1α and sarcopenia (Wenz et al. 2009). Transgene muscular over-expression of PGC-1α in 22-month-old rats showed an improvement in morphological, functional and biochemical parameters of sarcopenia comparison to wild-type animals. Transgene animals showed a lower fat percentage, together with a higher mitochondrial capacity and a higher capacity for oxidative phosphorylation and increased insulin sensitivity, suggesting a PGC-1α-mediated mitochondrial dysfunction in muscular aging (Wenz et al. 2009). Finally, a mitochondrial-mediated apoptosis may be a part of the development of sarcopenia. The relevance of mitochondrial triggered apoptosis pathways and elicitors needs to be further investigated (Marzetti et al. 2010).
Paracrine mechanism and inflammation
Among many other adipo(cyto)kines, adipose tissue releases the hormone adiponectin whose plasma concentration is negatively correlated with whole body fat mass. Accordingly, weight loss raises adiponectin blood levels while a further gain in fat mass decreases them (Sakuma and Yamaguchi 2013). Adiponectin increases insulin sensitivity by facilitating glucose uptake in skeletal muscle and adipose tissue and stimulates fatty acid oxidation (Yamauchi et al. 2002). In addition, adiponectin triggers the preferential use of fatty acids as a fuel in skeletal muscle. These effects are mediated by the activation of the 5′-AMP-activated protein kinase (AMPK) signaling pathway (Yamauchi et al. 2002; Kusminski et al. 2009). Adiponectin interacts with at least two cellular receptors (ADIPOR1 and ADIPOR2; Yamauchi et al. 2003). Activation of ADIPOR1 and/or ADIPOR2 stimulates peroxisome-proliferator-activated receptor-α (PPARα), AMPK and p38 mitogen-activated protein kinase (Tilg and Moschen 2006). Activation of AMPK signaling is reduced in obesity, due to the lack of adiponectin, although expression of ADIPOR1 and ADIPOR2 is similar (Chen et al. 2005). Serum concentrations of adiponectin are not only low in obesity, but additionally decreases with advancing age (Vilarrasa et al. 2005). Moreover, adiponectin regulates the expression of several pro- and anti-inflammatory cytokines. It decreases the inflammatory response by inhibiting TNFα and interleukin-γ (IL-γ) secretion and elevates production of anti-inflammatory cytokines, such as IL-10 and IL-1 receptor antagonist, by human monocytes, macrophages, and dendritic cells (Tilg and Moschen 2006).
In contrast to adiponectin, leptin, another major adipokine, is positively correlated with fat mass (Sakuma and Yamaguchi 2013). Leptin is mainly responsible for the control of appetite. In addition to this function, leptin regulates neuroendocrine function, energy homeostasis, haematopoiesis, and angiogenesis, and is a mediator of immune-mediated diseases and inflammatory processes (La Cava and Matarese 2004). In contrast to adiponectin, leptin has a pro-inflammatory effect by up-regulating the production of IL-6, IL-12 and TNF-α (Tilg and Moschen 2006).
Adipocytes and to an even higher extent proadipocytes themselves have also been shown to express IL-6, tumor necrosis factor α (TNFα) and monocyte chemotactic protein-1 (MCP-1; Sepe et al. 2011). MCP-1 promotes migration and differentiation of monocytes to adipose tissue macrophages that produce, apart from TNF-α and IL-6, additional inflammatory cytokines, such as IL-1β (Schrager et al. 2007). Consistent with this, C-reactive protein (CRP) and IL-6 are positively correlated with obesity, particularly with central obesity (Schrager et al. 2007). A higher fat mass results in activation of macrophages, inflammatory T lymphocytes, and mast cells, creating a pro-inflammatory state. Taken together, visceral adipose tissue provokes higher concentrations of pro-inflammatory cytokines directly by its own secretion and indirectly by stimulation of monocytes through leptin and down-regulation of the anti-inflammatory adiponectin (Sepe et al. 2011).
The molecular link between adiponectins and obesity is underpinned by the observation that a loss of muscle mass, as well as strength, are associated with higher levels of the “geriatric cytokines” IL-6 and CRP (Schrager et al. 2007; Schaap et al. 2006). Multiple mechanisms have been proposed to explain this correlation. For example, higher mRNA expressions of IL-6, IL-1ß and IL-8 in human adipose tissue are associated with increased MAP3K8 expression. MAP3K8 is an important signal transducer and activator of pro-inflammatory pathways (Ballak et al. 2014). These pathways could be linked to obesity-induced adipose tissue inflammation, but do not seem to have systemic effects on insulin resistance (Ballak et al. 2014).
IL-6 also has an anti-inflammatory potential, which has been proposed to be a feedback inhibition pathway for TNFα (Roubenoff 2003). In addition, IL-6 is secreted by the muscle itself on physical exercise, accelerated by low glycogen storage. Consequently, it stimulates the energy sensing AMPK and PI3-Kinase pathways to increase insulin sensitivity and oxidation of fatty acids. After release in the blood stream, IL-6 enhances gluconeogenesis in the liver and lipolysis in adipose tissue (Pedersen and Febbraio 2008). In addition, IL-6 and TNFα are able to lower the anabolic hormone insulin-like growth factor-1 (IGF-1) and induce insulin resistance, leading to a catabolic state (Roubenoff 2003). TNFα excreted either from adipose tissue or stimulated immune cells might induce apoptosis in muscle cells (Marzetti et al. 2009). Consequently, intraperitoneal administration of TNFα in rats for 8 days directly leads to apoptotic DNA laddering in muscle without external necrotic induction (Carbó et al. 2002). Besides its role in programmed cell death TNFα also upregulates the expression of the muscle atrophying ubiquitin ligase MuRF1 via the NF-κB pathway (Cai et al. 2004).
The Trial of Angiotensin Converting Enzyme Inhibition and Novel Cardiovascular Risk Factors (TRAIN) study investigated the relationship between BMI, total fat mass, appendicular lean mass and CRP and IL-6 (Cesari et al. 2005). CRP and IL-6 showed a positive correlation with BMI and total fat mass and were inversely correlated with fat-adjusted appendicular lean mass. However, there were no significant associations between CRP and IL-6 concentrations with obesity or sarcopenia. Obesity showed a significantly correlation with high CRP and IL-6 levels after adaption for sarcopenia (Cesari et al. 2005). For individuals with low body fat, the prevalence of limitations on walking obviously increases with elevated concentrations of CRP in the blood, whereas no changes were found for the group with the highest amount of adipose tissue (Stenholm et al. 2008b). In line with this, in a recent study by Levine and Crimmins (2012), CRP was not able to significantly vary the power to predict physical functioning problems in either the group of solely sarcopenic, solely obese or sarcopenic obese participants, even though a correlation of CRP levels and the risk of physical disabilities was revealed. Remarkably, the highest concentrations of CRP were detected in sarcopenic non-obese subjects, followed by a significantly lower mean by obese participants, independent of muscle status (Levine and Crimmins 2012). In summary, the role of inflammatory cytokines in the development of sarcopenic obesity is not well understood at present, since CRP and IL-6 could simply be confounders of the true underlying pathological mechanism.
Endocrinological adaptions
Testosterone and GH
Body composition is mainly influenced by endocrinological factors which include hormonal signals, either anabolic or catabolic, throughout an individual`s lifespan. Testosterone appears to be an important factor for building up skeletal muscle and it increases muscle protein synthesis (Urban et al. 1995). Levels of this hormone decline with age and are individually influenced by nutrition and physical activity, with a trend towards decreasing in obese men (Sakuma and Yamaguchi 2013; Allan et al. 2007). Short-term (4 weeks) testosterone administration to elderly men to increase levels to ranges similar to young men elevates skeletal muscle strength and protein synthesis (Urban et al. 1995).
Growth hormone (GH) coordinates the postnatal growth of different tissues, including skeletal muscle (Florini et al. 1996). The highest GH levels are measured at puberty, which are accompanied by high levels of circulating liver-derived, insulin-like growth factor-I (IGF-I) and decline during throughout the lifespan (Ryall et al. 2008). GH acts directly via the GH receptor which activates different signaling pathways (Lanning and Carter-Su 2006), but also indirectly via liver-derived IGF-I as a downstream target for GH-mediated transcription (Chia et al. 2006). Different signaling cascades are activated by GH and its decrease with age has numerous consequences for skeletal muscle structure and function (Ryall et al. 2008). The age-related decline in GH results in reduced liver-derived IGF-I. This anabolic hormone might also be lowered by an excess of adipose tissue (Roubenoff 2003). Coincidence of low testosterone together with a decline in IGF-I has been shown to increase the probability of developing frailty (Yeap et al. 2012). However, supplementation of testosterone for 6 months in healthy men between the ages of 60 and 80 years with low endogenous testosterone levels did not result in an increase in functional mobility or muscle strength (Emmelot-Vonk et al. 2008). Taken together, testosterone and GH/IGF-1 are undoubtedly major players in muscle health. The above analysis might indicate a pathophysiological relationship.
Myostatin and oxytocin
Another important growth factor regulating muscle growth is myostatin. This protein acts as a negative regulator of skeletal muscle mass (Lee 2004). Muscle atrophy due to lower limb unloading for 2 weeks raises myostatin levels (Sakuma et al. 2009). The influence of advancing age on myostatin is, at present, unclear. In a cross-sectional study of younger, middle-aged and older men and women, the serum myostatin concentrations were shown to increase with age and were inversely correlated with skeletal muscle mass (Yarasheski et al. 2002). Obesity and insulin resistance increase expression of myostatin in skeletal muscle (Hittel et al. 2009; Allen et al. 2011) and adipose tissue samples obtained from obese and extremely obese women revealed elevated levels of circulating myostatin (LeBrasseur 2012). As a consequence of obesity, an increase in myostatin represents a risk for skeletal muscle health and systemic metabolism in older individuals (Sakuma et al. 2014). Therefore, the possibility of using myostatin as a potential target for the therapy of sarcopenia deserves further investigation (White and LeBrasseur 2014).
Oxytocin, whose functions in lactation, parturition and social behaviour have been well documented, seems also to be involved in several other functions. In an animal model study, oxytocin-receptor-deficient mice developed late onset obesity with normal food intake (Takayanagi et al. 2008; Camerino 2009). Otherwise, a central oxytocin infusion in diet-induced obese mice results in a body weight loss (Zhang et al. 2011). Deblon et al. (2011) using a model of diet-induced obese rats, reported a dose-dependent decrease in body weight, increased adipose tissue lipolysis, and fatty acid β-oxidation, as well as reduced glucose intolerance and insulin resistance, as a result of central oxytocin infusion. Probably, oxytocin plays essential roles in the regulation of energy homeostasis and the administration of oxytocin may be a promising therapeutic approach for the treatment of human obesity and type 2 diabetes (Deblon et al. 2011).
Impaired hypothalamo-pituitary-signals
Central adiposity elevates whole body metabolism and resting energy expenditure through up-regulation of the hypothalamo-pituitary-thyroid axis (Kok et al. 2005). For elderly people, there is a greater need for a sufficiently high-quality protein intake to maintain adequate muscle protein synthesis (Volkert and Sieber 2011). Moreover, during aging, individuals become more and more prone to malnutrition and unintentional weight loss, accompanied by wasting of muscle mass. Therefore, apparently the intake of essential nutrients shows tendentially an uncoupling from the actual requirement in old people (Volkert 2013). Consequential energy deficiency leads to diverse endocrinological adaptions. Obese subjects, in particular, who have elevated levels of thyroid hormone, should have problems in adapting their resting energy expenditure in the short-term to actual demand (Sainsbury and Zhang 2012). Since thyroxin (T4) has a metabolic half-life of 7 days and its conversion to the more active form triiodothyronine (T3) is even up-regulated in fasting by improved activity of the enzyme 5′-deiodinase, there is a gap between energy uptake and expenditure in the first few days following caloric restrictions (Sainsbury and Zhang 2012). If the dietary limitations continue for longer periods, T3 levels will be reduced, resulting in greater fatty acid accumulation and stunted fatty acid oxidation. Accordingly, amino acids may be preferentially used as a fuel while protein synthesis is blocked (Iossa et al. 2001). Therefore, obesity seems to provoke a higher catabolic endocrinological state while it blocks anabolic signals. Consequently, obese elderly subjects especially are more prone to muscle wasting, due to generally elevated energy expenditure, despite frequent episodes of malnutrition.
Muscle regeneration
In response to injury or trauma, skeletal muscle is able to regenerate substantially by means of mesenchymal progenitor cells called satellite cells. In adults, satellite cells are quiescent. Muscle fiber necrosis will lead to a fusion of steam cells, resulting in new myofibers, which replace damaged fibers. Proliferation of satellite cells and fusion with existing myofibers to substitute or enhance myonuclei is the result of activation via muscle load (Ciciliot and Schiaffino 2010). Even though there have been conflicting results regarding the changes in satellite cell numbers during aging, most studies have reported a decrease in these progenitor cells throughout an individual`s lifetime (Kadi and Ponsol 2010). Investigations of the experimental aspects of human muscle have been limited. Most knowledge about satellite cells in relation to age and under pathophysiological conditions has been obtained using experimental setups of rodent models and transgenic and knockout mouse models. Boldrin et al. (2010) highlighted the differences and similarities between human and mouse satellite cells. The involvement of stem cells in the pathogenesis of sarcopenia and sarcopenic obesity are still a subject of debate, because of our incomplete understanding of human satellite cells (Thornell 2011).
In accordance with this perspective, an increase in total fat mass resulting in lipotoxicity and inflammation lead progenitor cells to dedifferentiate into mesenchymal adipocyte-like default cells (MAD cells) that express typical genes of fatty tissue, such as Peroxisome proliferator-activated receptor-γ (PPAR-γ). These MAD cells could accumulate inter-muscular adipose tissue (IMAT) which reduces the self-renewal capacity of the muscle (Sepe et al. 2011). In addition to this, IMAT secretes several paracrine active hormones and inflammatory cytokines, like adipose tissue, and may possibly enable a feed-forward cycle of IMAT generation. This gathering of intramuscular fat infiltration results in worse lower extremity performance in elderly persons, independent of whole body fat mass and muscle cross-sectional area (Roubenoff 2003).
Recently the hormone oxytocin was shown to be involved in muscle regeneration and homeostasis (Elabd et al. 2014). Oxytocin levels decline with age, as well as oxytocin receptor expression in the old muscle stem cells. A consequence of age-specific systemic decrease in oxytocin is the decline in muscle regeneration accompanied by increased fibrosis (Elabd et al. 2014). Systemic administration of oxytocin increases muscle regeneration by improving aged muscle stem cell activation and/or proliferation. Oxytocin knockout mice do not show a defect in muscle development, but this deficit results in premature sarcopenia. Oxytocin may probably also be a therapeutic approved for the treatment or prevention of skeletal muscle aging and/or sarcopenia (Elabd et al. 2014).
Energy supply and internal remodelling of skeletal muscle
To achieve functionality of the myofibers, an adequate energy supply and a sufficient amount of myofibrillar protein has to be provided. The oxidative production of energy is maintained by the mitochondria, whose biogenesis is in turn driven by the peroxisome proliferator-activated receptor gamma coactivator 1-alpha (PGC-1α) (Summermatter et al. 2012). Various stimuli, including exercise training, cold induction, and thyroid treatment, are able to activate PGC-1α. These inducers fail to up-regulate PGC-1α and its downstream effector nuclear response factor-1 (NRF1) in old rats, resulting in low mitochondrial biogenesis (Derbré et al. 2012). Further chronic overload with fat raised by a high fat diet reduce the mRNA level of PGC-1α in the muscle of old rats (Bollheimer et al. 2012). These studies suggest that an excess of fatty acids, together with old age, might lead to lower concentrations of PGC-1α thereby further stunting the anabolic response of physical activity.
Mice that were fed with a high fat diet for 12 weeks, as well as their littermates receiving standard rodent chow, showed a similar amount of centrally nucleated myofibrils as a marker for the regeneration of muscle. In line with these findings, no changes were detected in the percentage muscle fiber composition. In contrast, the mean diameter of all three fiber types (type I; IIA and IIB) was evenly elevated for the group of mice that had a higher intake of dietary fat (Turpin et al. 2009). Nevertheless, the greater fiber area may possibly have been due to the short duration of the trial, since several other animal studies have found a decrease in muscle thickness which was seen to be dependent on obesity (Fellner et al. 2014). Sprague–Dawley rats receiving a diet in which fatty acids constituted 45 % of the energy source had lower cross-sectional areas in the quadriceps muscle compared to the group that was fed with standard rodent chow (Fellner et al. 2014).
Two contrasting processes define the levels of myofibrillar proteins. Firstly, synthesis of these proteins is regulated as a function of the cells (Magnuson et al. 2012). Wistar rats receiving a high fat diet (45 % energy provided by fat) until the age of 20 months showed a greater decrease in their quadriceps muscle volume with aging than littermates receiving standard rodent chow. In this animal model, the energy-sensing AMPK and PKB/Akt pathways are deregulated (Magnuson et al. 2012). Both pathways are known to modulate muscle protein synthesis via phosphorylation by stimulating the ribosomal protein S6 kinase beta-1 (S6K1) and inhibiting the eukaryotic translation initiation factor 4E-binding protein 1 (4E-BP1). Taken together, it is proposed that long-term feeding with a high fat diet decreases both S6K1, as well as 4E-BP1 activity, resulting in deregulated muscle protein synthesis (Bollheimer et al. 2012). In a recent study, 20-week-old obese and lean Zucker rats were compared in terms of their fractional protein synthesis (Nilsson et al. 2013). Even though obese rats showed atrophied hind limb muscle, their basal protein synthesis rates were higher than in the lean littermates. Here, S6K1, which enhances protein synthesis, is activated whereas DEPTOR as an inhibitor of translation is down-regulated. Therefore, the authors concluded that there has to be a higher protein turnover favouring degradation. Consistent with this, obese animals failed to adequately induce protein synthesis after stimulation (Nilsson et al. 2013). Therefore, both studies showed a deregulation of protein turnover due to an overload of fatty acids, while the cellular concentration of S6K1 seemingly depended on the age of the rats and the animal model used.
Secondly, proteins are degraded, mainly by the proteasomal or the lysosomal pathway, to utilize the liberated amino acids for new protein synthesis or for energy production (Magnuson et al. 2012). FOXO1 is known to induce transcription of the E3 ubiquitin ligases MAFbx and MuRF-1, thereby accelerating proteasomal decay of muscle proteins. Expression of these proteins, consequent ubiquitination, and finally proteolytic activity in muscle cells are not altered with a high fat diet or leptin deficiency. Likewise, degradation of intracellular proteins via the lysosomal pathway, also called autophagy, showed no differences between the various animal groups in this study (Turpin et al. 2009).
In recent years, skeletal muscle has been shown to secrete several hormone-like proteins called myokines. These molecules include IL-6, IL-8, IL-15, brain-derived neurotrophic factor (BDNF) and leukemia inhibitory factor (LIF). Even though discussed as a negative predictor of muscle mass in obese elderly subjects, IL6 seems to have an anabolic and insulin-sensitizing effect on muscle cells (Pratesi et al. 2013). IL-15 is an anabolic cytokine that stimulates protein synthesis while stunting proteolysis in cultured myotubes (Quinn et al. 2002). The IL-15 protein content of the gastrocnemius muscle decreases in senescent ad libitum fed male Fischer 344 × Brown Norway hybrid rats, while levels for animals receiving a 40 % caloric restriction diet until 37 months of age remained constant (Marzetti et al. 2009). Consequently, the increase in TNFα and subsequent apoptotic signaling as monitored by caspase 3 and caspase 8 was stunted in the group of caloric-restricted rats (Marzetti et al. 2009). Consequently, it may be hypothesized that over nutrition and obesity anabolic IL-15 production of the aging muscle may be reduced, making it more susceptible to TNFα-dependent induction of apoptosis.
Exercise training
Exercise training has a beneficial effect on muscle strength and physical activity (Frimel et al. 2008) and may affect different aspects of sarcopenic obesity.
Exercise may consist of resistance and/or aerobic training like endurance exercise, flexibility training, balance training, high intensity interval training or a combination of different kinds of exercise with various influences on sarcopenic obesity.
Resistance training
Resistance training reduces body weight and enhances muscle strength and mass effectively in aging individuals (Frontera et al. 1988; Fiatarone et al. 1990). Resistance training directly increases human skeletal muscle protein synthesis and causes muscle hypertrophy (Walker et al. 2011). Actually in older people with obesity, it leads to muscle mass gain and improves body composition (Donnelly et al. 2009). Additionally, resistance exercise also diminishes the pathological progression of sarcopenic obesity by reducing inflammatory cytokines IL-6 and TNFα and CRP (Lambert et al. 2008; Donges et al. 2010). In summary, resistance exercise has a high potential for the effective treatment of sarcopenia because it improves muscle performance and functional capacity as clinically important outcome parameters (Latham et al. 2003).
Aerobic training
On the one hand, accumulation of IMCL blunted the anabolic effect of insulin on the muscle (Choi et al. 2008). On the other hand, Goodpaster et al. (2001) were able to show that IMCL is enriched in the muscles of endurance athletes, without causing any obvious functional impairment. In addition, the skeletal muscle of trained endurance athletes is markedly more insulin sensitive than the skeletal muscle of sedentary individuals (Goodpaster et al. 2001). Therefore, aerobic exercise counteracts the negative effects of IMCL by improving oxidative capacity. Consequently, endurance training results in recovery of skeletal muscle sensitivity to the anabolic effect of insulin (Fujita et al. 2007), increased mitochondrial function (Lanza and Nair 2009), decreased circulating myostatin (Argiles et al. 2012), upregulated muscle protein synthesis (Villareal et al. 2011) and enhancement of nutrient stimulated vasodilatation and nutrient delivery to muscle (Timmerman et al. 2012). It also reduces body weight by decreasing abdominal and visceral fat mass (Mathus-Vliegen 2012). Accordingly, aerobic exercise has an anti-inflammatory potential by reducing obesity-associated cytokines like IL-6, IL-18, TNFα and CRP (Kohut et al. 2006).
Combined resistance and aerobic training
The combination of resistance and aerobic exercise seems to be more effective than either of them alone (Villareal et al. 2011) resulting in weight loss, enhancement of muscle mass, performance and functionality as well as decrease of abdominal and visceral fat mass. Consequently, inversion of inflammatory processes could be achieved, at least in part, by combined exercise training in frail, obese older adults (Lambert et al. 2008; Nicklas et al. 2008; Donges et al. 2010).
However, there are contradictory data concerning which cytokines are altered during treatment. While one study demonstrated down-regulation of IL-6, IL-18, TNFα and CRP, others found only one of these factors to be suppressed. Consequential exercise and/or strength training were described as being effective anti-inflammatory therapies for improving muscle function (Kohut et al. 2006; Donges et al. 2010; Nicklas et al. 2008).
High intensity interval training (HIT)
HIT is an enhanced form of interval training, an exercise strategy alternating periods of short intense aerobic exercise with less-intense recovery periods (Wisloff et al. 2007). This exercise reduces body mass, waist circumference, subcutaneous and abdominal fat Boutcher 2011) besides increasing muscle mass (Tapp et al. 2008; Boudou et al. 2003). Mitochondrial biogenesis and lipidoxidation and synthesis are improved by HIT via increased levels of PGC-1α in skeletal muscle (Wisloff et al. 2007). Enhanced insulin sensitivity, improved muscle capacity for fatty acid oxidation and glycolytic enzyme content are the result of HIT (Boutcher 2011).
At present, the most successful treatment for sarcopenic obesity is regular multi-component exercise training combined with a diet-induced waste loss and maintenance of an adequate protein supply (Thornell 2011; Bouchonville and Villareal 2013). Further studies are needed to assess other therapy options, such as pharmacological treatment.
Summary
The pathomechanism of sarcopenia and particularly sarcopenic obesity are currently not well understood. The loss of muscle mass and strength is considered in many studies to be sufficient to define sarcopenia. However, this point of view overlooks the need for elevated muscle mass and strength in people with sarcopenia raised by obesity to counteract the increased body weight. Moreover, as muscle mass declines, the predictive power of BMI drops and other factors, such as body fat distribution, become more important in the definition of adiposity. Future studies should increasingly focus on physical functioning and the ability to perform the tasks associated with daily live, to develop an adequate cut-off point for characterisation of sarcopenia resulting from obesity.
At present, a direct induction of apoptosis and muscle wasting due to short- to medium-term fatty acid overload has not been described. However, chronic exposure to high dietary fatty acids seems to deregulate the endocrinologic insulin system. This is caused by impairment of pancreatic β-cell function, as well as a decrease in insulin sensitivity of the skeletal muscle itself. Another important factor of sarcopenic obesity is the process of inflamm-aging. In the past few years, several studies have revealed that adipose tissue produces numerous (pro)-inflammatory cytokines and releases them into the blood stream. In addition, both muscle mass and strength have been shown to be negatively associated with these cytokines. However, apart from the direct induction of apoptosis through the TNFα pathway, the molecular mechanism of inflammation-induced muscle wasting is still a matter of ongoing discussion. Possibly the elevated cytokines, especially IL-6, are simply confounders of the underlying pathology. For chronic exposure to high amounts of fat, a dedifferentiation of myotube progenitor cells to mesenchymal adipocyte-like default cells has been proposed. Consequently, this process would decrease the regenerative capacity of the skeletal muscle with aging. In addition to direct effects on muscle cells, the whole body metabolism is set to a higher expenditure of energy as a result of obesity. Against the background of frequent malnutrition in the elderly, this might lead to an elevated use of proteins as fuel and finally muscle wasting.
The molecular pathology of sarcopenia is difficult to unravel for several reasons. Firstly, elderly subjects have a high level of co-morbidities, which often leads to confounding results. Secondly, sarcopenia, and presumably sarcopenic obesity as well, are syndromes with multiple overlapping causes and feedback mechanisms. Finally, muscle wasting during aging is a slowly accumulating process beginning at the age of 30. Based on the assumption of continuous 3–8 % muscle loss per decade, this would translate into a change of about 0.05 % per month. Even with advanced analysis techniques, it is almost impossible to detect functional and biochemical differences in short- to mid-term experiments. Therefore, long-term studies are necessary—either longitudinal clinical or in a controlled setting an animal model—to further unravel the molecular pathology of sarcopenic obesity.
References
Adams JM, Pratipanawatr T, Berria R, Wand E, DeFronzo RA, Sullards MC, Mandarino LJ (2004) Ceramide content is increased in skeletal muscle from obese insulin-resistant humans. Diabetes 53:25–31
Allan CA, Strauss BJG, McLachlan RI (2007) Body composition, metabolic syndrome and testosterone in ageing men. Int J Impot Res 19:448–457
Allen DL, Hittel DS, Mcpherron AC (2011) Expression and function of myostatin in obesity, diabetes, and exercise adaptation. Med Sci Sports Exerc 43:1828–1835
Anderson R, Prolla T (2009) PGC 1 alpha in aging and anti-aging interventions. Biochim Biophys Acta 1790:1059–1066
Argiles JM, Orpi M, Busquets S, Lopez-Sorian F (2012) Myostatin: more than just a regulator of muscle mass. Drug Discov Today 17:702–709
Ballak DB, Van Essen P, Van Diepen JA, Jansen H, Hijams A, Matsuguchi T, Sparrer H, Tack CJ, Netea MG, Joosten LAB, Stienstra R (2014) MAP3K8 (TPL2/COT) affects obesity-induced adipose tissue inflammation without systemic effects in humans and mice. PLOS ONE 9
Batsis JA, Barre LK, Mackenzie TA, Pratt SI, Lopez-Jimenez F, Bartels SJ (2013) Variation in the prevalence of sarcopenia and sarcopenic obesity in older adults associated with different research definitions: dual-energy x-ray absorptiometry data from the National Health and Nutrition Examination Survey 1999–2004. J Am Geriatr Soc 61:974–980
Batsis JA, Mackenzie TA, Barre LK, Lopez-Jimenez F, Bartels SJ (2014) Sarcopenia, sarcopenic obesity and mortality in older adults: results from the National Health and Nutrition Examination Survey III. Eur J Clin Nutr 68:1001–1007
Baumgartner RN (2000) Body composition in healthy aging. Ann N Y Acad Sci 904:437–448
Baumgartner RN, Wayne SJ, Waters DL, Janssen I, Gallagher D, Morley JE (2004) Sarcopenic obesity predicts instrumental activities of daily living disability in the elderly. Obes Res 12:1995–2004
Boldrin L, Muntoni F, Morgan JE (2010) Are human and mouse satellite cells really the same? J Histochem Cytochem 58:941–955
Bollheimer LC, Buettner R, Pongratz G, Brunner-Ploss R, Hechtl C, Banas M et al (2012) Sarcopenia in the aging high-fat fed rat: a pilot study for modeling sarcopenic obesity in rodents. Biogerontology 13:609–620
Bouchard DR, Dionne IJ, Brochu M (2009) Sarcopenic/obesity and physical capacity in older men and women: data from the nutrition as a determinant of successful aging (NuAge)—the Quebec Longitudinal Study. Obesity 17:2082–2088
Bouchonville MF, Villareal DT (2013) Sarcopenic obesity: how do we treat is? Endocrinology 20:412–419
Boudou P, Sobngwi F, Mauvais-Jarvis P, Vexiau P, Gautier JF (2003) Absence of exercise-induced variations in adiponectin levels despite decreased abdominal adiposity and improved insulin sensitivity in type 2 diabetic men. Eur J Endocrin 149:421–424
Boutcher SH (2011) High-intensity intermittent exercise and fat loss. J Obes. doi:10.1155/2011/868305
Cai D, Frantz JD, Tawa NE Jr et al (2004) IKKβ/NF-κB activation causes severe muscle wasting in mice. Cell 119:285–298. doi:10.1016/j.cell.2004.09.027
Camerino C (2009) Low sympathetic tone and obese phenotype in oxytocin-deficient mice. Obesity 17:980–984
Carbó N, Busquets S, van Royen M, Alvarez B, Lopez-Soriano FJ, Argiles JM (2002) TNF-alpha is involved in activating DNA fragmentation in skeletal muscle. Br J Cancer 86:1012–1016. doi:10.1038/sj.bjc.6600167
Cesari M, Kritchevsky SB, Baumgartner RN, Atkinson HH, Penninx BW, Lenchik L et al (2005) Sarcopenia, obesity, and inflammation—results from the trial of angiotensin converting enzyme inhibition and novel cardiovascular risk factors study. Am J Clin Nutr 8(82):428–434
Chen MB, McAinch AJ, Macaulay SL, Castelli LA, O’brien PE, Dixon JB, Cameron-Smith D, Kemp BE, Steinberg GR (2005) Impaired activation of AMP-kinase and fatty acid oxidation by globular adiponectin in cultured human skeletal muscle of obese type 2 diabetics. J Clin Endocrinol Metab 90:3665–3672
Chia DJ, Ono M, Woelfle J, Schlesinger-Massart M, Jiang H, Rotwein P (2006) Characterization of distinct Stat5b binding sites that mediate growth hormone-stimulated IGF-I gene transcription. J Biol Chem 281:3190–3197
Choi CS, Befroy DE, Codella R, Kim S, Reznick RM, Hwang YJ, Liu ZX, Lee HY, Distefano A, Samuel VT, Zhang D, Cline GW, Handschin C, Lin J, Petersen KF, Spiegelman BM, Shulman GI (2008) Paradoxical effects of increased expression of PGC-1 alpha on muscle mitochondrial function and insulin-stimulated muscle glucose metabolism. Proc Nat Acad Sci 105:19926–19931
Ciciliot S, Schiaffino S (2010) Regeneration of mammalian skeletal muscle. Basic mechanisms and clinical implications. Curr Pharm Des 16:906–914
Consitt LA, Bell JA, Houmard JA (2009) Intramuscular lipid metabolism, insulin action and obesity. IUBMB Life 61:47–55
Cooper R, Kuh D, Cooper C, Gale CR, Lawlor DA, Matthews F, Hardy R, The FALCon and HALCyon Study Teams (2011) Objective measures of physical capability and subsequent health: a systematic review. Age Ageing 40:4–23
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F et al (2010) Sarcopenia: European consensus on definition and diagnosis. Age Ageing 39:412–423
Deblon N, Veyrat-Durebex C, Bourgoin L, Caillon AK, Bussier A-L, Petrosino S, Piscitelli F, Legros J-J, Geenen V, Foti M, Wahli W, Di Marzo V, Rohner-Jeanrenaud F (2011) Mechanisms of the ant-obesity effects of oxytocin in diet-induced obese rats. PLoS ONE 6:e25565
Derbré F, Gomez-Cabrera MC, Nascimento AL, Sanchis-Gomar F, Martinez-Bello VE, Tresguerres JAF et al (2012) Age associated low mitochondrial biogenesis may be explained by lack of response of PGC-1α to exercise training. AGE 34:669–679
Doak CM, Wijnhoven TMA, Schokker DF, Visscher TLS, Seidell JC (2012) Age standardization in mapping adult overweight and obesity trends in the WHO European Region. Obes Rev 13:174–191
Donges CE, Duffield R, Drinkwater EJ (2010) Effects of resistance or aerobic exercise training on interleukin-6, C-reactive protein, and body composition. Med Sci Sports Exerc 42:304–313
Donnelly JE, Blair S, Jakicic J, Manore M, Rankin J, Smith B (2009) American college of sports medicine position stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc 41:459–471
Elabd C, Cousin W, Upadhyayula P, Chen RY, Chooljian MS, Li J, Kung S, Jiang KP, Conboy IM (2014) Oxytocin is an age-specific circulation hormone that is necessary for muscle maintenance and regeneration. Nat Commun 5:4082/doi: 10.1038/ncomms5082
Emmelot-Vonk MH, Verhaar HJ, Nakhai Pour HR, et al (2008) Effect of testosterone supplementation on functional mobility, cognition, and other parameters in older men: a randomized controlled trial. JAMA 299:3952
Espinoza DO, Boros LG, Crunkhorn S, Gami H, Patti ME (2010) Dual modulation of both lipid oxidation and synthesis by peroxisome proliferator-activated receptor-gamma coactivator -1alpha and -1beta in cultured myotubes. FASEB 24:1003–1014
Fellner C, Schick F, Kob R, Hecht C, Vorbuchner M, Büttner R, Hamer OW, Sieber CC, Stroszczynski C, Bollheimer LC (2014) Diet-induced and age-related changes in the quadriceps muscle: MRI and MRS in a rat model of sarcopenia. Gerontology. doi:10.1159/000360289
Fiatarone MA, Marks EC, Ryan ND, Meredith CN, Lipsitz LA, Evans WJ (1990) High-intensity strength training in nonagenarians. Effects on skeletal muscle. JAMA 263:3029–3034
Fielding RA, Vellas B, Evans WJ, Bhasin S, Morley JE et al (2011) Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology and consequences. J Am Med Dir Assoc 12:249–256
Florez H, Troen BR (2008) Fat and inflammaging: a dual path to unfitness in elderly people? J Am Geriatr Soc 56:558–560
Florini JR, Ewton DZ, Coolican SA (1996) Growth hormone and the insulin-like growth factor system in myogenesis. Endocr Rev 17:481–517
Frimel TN, Dinacore DR, Villarreal T (2008) Exercise attenuates the weight-loss-induced reduction in muscle mass in frail obese older adults. Med Sci Sports Exerc 40:1213–1219
Frontera WR, Meredith CN, O’Reilly KP, Knuttgen HG, Evans WJ (1988) Strength conditioning in older men: skeletal muscle hypertrophy and improved function. J Appl Physiol 64:1038–1044
Fujita S, Rasmussen BB, Cadenas JG, Drummond MJ, Glynn EL, Sattler FR, Volpi E (2007) Aerobic exercise overcomes the age-related insulin resistance of muscle protein metabolism by improving endothelial function and Akt/mammalian target of rapamycin signaling. Diabetes 56:1615–1622
Garris D (2005) Cytochemical analysis of pancreatic islet lipoapoptosis: hyperlipidemia-induced cytoinvolution following expression of the diabete (db/db) mutation. Pathobiology 72:124–132
Goodpaster BH, He J, Watkins S, Kelley DE (2001) Skeletal muscle lipid content and insulin resistance: evidence for a paradox in endurance-trained athletes. J Clin Endocrinol Metab 86:5755–5761
Griffin ME, Marcucci MJ, Clone GW, Bell K, Barucci N, Lee D, Goodyear LJ, Kraegen EW, White MF, Shulman GI (1999) Free fatty acid-induced insulin resistance is associated with activation of protein kinase c theta and alteration in the insulin signaling cascade. Diabetes 48:1270–1274
Harman D (1956) Aging: a theory based on free radical and radiation chemistry. J Geront 11:298–300
Herbst A, Pak JW, McKenzie D, Bua E, Bassiouni M, Aiken JM (2007) Accumulation of mitochondrial DNA mutations in aged muscle fibers: evidence for a causal role in muscle fiber loss. J Geront A Biol Sci Med Sci 62:235–245
Hittel DS, Berggren JR, Shearer J, Boyle K, Houmard JA (2009) Increased secretion and expression of myostatin in skeletal muscle from extremely obese women. Diabetes 58:30–38
Iossa S, Lionetti L, Mollica MP, Crescenzo R, Barletta A, Liverini G (2001) Fat balance and serum leptin concentrations in normal, hypothyroid, and hyperthyroid rats. Int J Obes Relat Metab Disord J Int Assoc Study Obes 25:417–425
Jacob S, Machann J, Rett K, Brechtel K, Volk A, Renn W, Maerker E, Matthaei S, Schick F, Claussen CD, Häring HU (1999) Association of increased intramyocellular lipid contend with insulin resistance in lean nondiabetic offspring of type 2 diabetic subjects. Diabetes 42:1113–1119
Kadi F, Ponsol E (2010) The biology of satellite cells and telomeres in human skeletal muscle: effects of aging and physical activity. Scan J Med Sci Sports 20:39–48
Kennedy RL, Chokkalingham K, Srinivasan R (2004) Obesity in the elderly: who should we be treating, and why, and how? Curr Opin Clin Nutr Metab Care 7:3–9
Kohut ML, McCann DA, Russell DW, Konopka DN, Cunnick JE, Franke WD et al (2006) Aerobic exercise, but not flexibility/resistance exercise, reduces serum IL-18, CRP, and IL-6 independent of β-blockers, BMI, and psychosocial factors in older adults. Brain Behav Immun 20:201–209
Kok P, Roelfsema F, Langendonk JG, Frölich M, Burggraaf J, Meinders AE et al (2005) High circulating thyrotropin levels in obese women are reduced after body weight loss induced by caloric restriction. J Clin Endocrinol Metab 90:4659–4663
Krssak M, Falk Petersen K, Dresner A, DiPietro L, Vogel SM, Rothman DL, Roden M, Shulman GI (1999) Intramyocellular lipid concentrations are correlated with insulin sensitivity in humans: a 1H NMR spectroscopy study. Diabetologia 42:113–116
Kusminski CM, Shetty S, Orci L, Unger RH, Scherer PE (2009) Diabetes and apoptosis: lipotoxicity. Apoptosis 14:1484–1495
La Cava A, Matarese G (2004) The weight of leptin in immunity. Nature Rev Immunol 4:371–379
Lambert CP, Wright NR, Finck BN, Villareal DT (2008) Exercise but not diet-induced weight loss decreases skeletal muscle inflammatory gene expression in frail obese elderly persons. J Appl Physiol 105:473–478
Landi F, Cruz-Jentoft AJ, Liperoti R, Russo A, Giovannini S, Tosato M, Capoluongo E, Bernabei R, Graziano O (2013) Sarcopenia and mortality risk in frail older persons aged 80 years and older: result from ilSIRENTE study. Age Ageing 42:203–209
Lanning NJ, Carter-Su C (2006) Recent advances in growth hormone signaling. Rev Endocr Metab Disord 7:225–235
Lanza IR, Nair KS (2009) Muscle mitochondrial changes with aging and exercise (2009) Muscle mitochondrial changes with aging and exercise. Am J Clin Nutr 89:467S–471S
Latham N, Anderson C, Bennet D, Stretton C (2003) Progressive resistance strength training for physical disability in older people. Cochrane Database Syst Rev 2:CD002759
LeBrasseur NK (2012) Building muscle, browning fat and preventing obesity by inhibiting myostatin. Diabetologia 55:13–17
Lee S-J (2004) Regulation of muscle mass by myostatin. Ann Rev Cell Dev Biol 20:61–86
Levine ME, Crimmins EM (2012) The impact of insulin resistance and inflammation on the association between sarcopenic obesity and physical functioning. Obesity 20:2101–2106
Magnuson B, Ekim B, Fingar DC (2012) Regulation and function of ribosomal protein S6 kinase (S6 K) within mTOR signaling networks. Biochem J 441:1–21
Marzetti E, Carter CS, Wohlgemuth SE, Lees HA, Giovannini S, Anderson B et al (2009) Changes in IL-15 expression and death-receptor apoptotic signaling in rat gastrocnemius muscle with aging and life-long calorie restriction. Mech Ageing Dev 130:272–280
Marzetti E, Hwang JC, Less HA, Wohlgemuth SE, Dupont-Versteegden EE, Carter CS, Benabei R, Leeuwenburgh C (2010) Mitochondrial death effectors: relevance to sarcopenia and disuse muscle atrophy. Biochim Biophys Acta 1800:235–244
Mathus-Vliegen EMH, on behalf of the Obesity Management Task Force (OMTF) of the European Association for the Study of Obesity (EASO) (2012) Prevalence, pathophysiology, health consequences and treatment of obesity in the elderly: a guideline. Obes Facts 5:460–483
Muscaritoli M, Anker SD, Argiles J, Aversa Z, Bauer JM, Biolo G, Boirie Y, Bosaeus I, Cederholm T, Costelli P, Gearon KC, Laviano A, Maggio M, Rossi Fanelli F, Schneider SM, Schols A, Sieber CC (2010) Consensus definition of sarcopenia, cachexia and pre-cachexia: joint document elaborated by special interest groups (SIG) Cachexia-anorexia in chronic wasting diseases and nutrition in geriatrics. Clin Nutr 29:154–159
Nicklas BJ, Hsu F-C, Brinkley TJ, Church T, Goodpaster BH, Kritchevsky SB et al (2008) Exercise training and plasma C-reactive protein and interleukin-6 in the elderly. J Am Geriatr Soc 56:2045–2052
Nilsson MI, Dobson JP, Greene NP, Wiggs MP, Shimkus KL, Wudeck EV et al (2013) Abnormal protein turnover and anabolic resistance to exercise in sarcopenic obesity. FASEB J. doi:10.1096/fj.12-224006
Pedersen BK, Febbraio MA (2008) Muscle as an endocrine organ: focus on muscle-derived interleukin-6. Physiol Rev 88:1379–1406
Pratesi A, Tarantini F, Di Bari M (2013) Skeletal muscle: an endocrine organ. Clin Cases Miner Bone Metab 10:11–14
Quinn LS, Anderson BG, Drivdahl RH, Alvarez B, Argilés JM (2002) Overexpression of interleukin-15 induces skeletal muscle hypertrophy in vitro: implications for treatment of muscle wasting disorders. Exp Cell Res 280:55–63
Reznick RM, Zhong H, Li J, Morino K, Moore IK, Yu HJ, Liu ZX, Dong J, Mustard KJ, Hawley SA, Befroy D, Pypaert M, Hardie DG, Young LH, Shulman GI (2007) Aging-associated reductions in AMP-activated protein kinase activity and mitochondrial biogenesis. Cell 5:151–156
Rolland Y, Lauwers-Cances V, Cristini C, van Kan GA, Janssen I, Morley JE et al (2009) Difficulties with physical function associated with obesity, sarcopenia, and sarcopenic-obesity in community-dwelling elderly women: the EPIDOS (EPIDemiologie de l’OSteoporose) Study. Am J Clin Nutr 89:1895–1900
Roubenoff R (2003) Catabolism of aging: is it an inflammatory process? Curr Opin Clin Nutr Metab Care 6:295–299
Ryall JG, Schertzer JD, Lynch GS (2008) Cellular and molecular mechanisms underlying age-related skeletal muscle wasting and weakness. Biogerontology 9:213–228
Sainsbury A, Zhang L (2012) Role of the hypothalamus in the neuroendocrine regulation of body weight and composition during energy deficit. Obes Rev 13:234–257
Sakuma K, and Yamaguchi A (2013) Sarcopenic obesity and endocrinal adaptation with age. Int J Endocrinol 204164. doi: 10.1155/2013/204164
Sakuma K, Watanabe K, Hotta N, Koike T, Ishida K, Katayama K, Akima H (2009) The adaptive responses in several mediators linked with hypertrophy and atrophy of skeletal muscle after lower limb unloading in humans. Acta Physiol 197:151–159
Sakuma K, Aoi W, Yamaguchi A (2014) Current understanding of sarcopenia: possible candidates modulating muscle mass. Pflugers Arch—Eur J Physiol 1–17
Schaap LA, Pluijm SMF, Deeg DJH, Visser M (2006) Inflammatory markers and loss of muscle mass (sarcopenia) and strength. Am J Med 119:526.e9–526.e1
Schrager MA, Metter EJ, Simonsick E, Ble A, Bandinelli S, Lauretani F, Ferrucci L (2007) Sarcopenic obesity and inflammation in the InCHIANTI study. J Appl Physiol 102:919–925
Sepe A, Tchkonia T, Thomou T, Zamboni M, Kirkland JL (2011) Aging and regional differences in fat cell progenitors—a mini-review. Gerontology 57:66–75
Shimabukuro M, Zhou Y-T, Levi M, Unger RH (1998) Fatty acid-induced β cell apoptosis: a link between obesity and diabetes. Proc Nat Acad Sci USA 95:2498–2502
Sparangna G, Hickson-bick D (2000) A metabolic role for mitochondria in palmitate-induced cardiac myocyte apoptosis. Am J Physiol Heart Circ Physiol 279:H2124–H2132
Stenholm S, Harris TB, Rantanen MS, Visser M, Kritchevsky SB, Ferrucci L (2008a) Sarcopenic obesity—definition, etiology and consequences. Curr Opin Clin Nutr Metab Care 11:693–700
Stenholm S, Rantanen T, Heliövaara M, Koskinen S (2008b) The mediating role of c-reactive protein and handgrip strength between obesity and walking limitation. J Am Geriatr Soc 56:462–469
St-Pierre J, Drori S, Uldry M, Silvaggi JM, Rhee J, Jäger S, Handschin C, Zheng K, Lin J, Yang W, Simon DK, Bachoo R, Spiegelman BM (2006) Suppression of reactive oxygen species and neurodegeneration by the PGC-1 transcriptional coactivator. Cell 20:397–408
Summermatter S, Thurnheer R, Santos G, Mosca B, Baum O, Treves S et al (2012) Remodeling of calcium handling in skeletal muscle through PGC-1α: impact on force, fatigability, and fiber type. Am J Physiol—Cell Physiol 302:C88–C99
Summers SA (2006) Ceramide in insulin resistance and lipotoxicity. Progr Lipid Res 45:42–72
Takayanagi Y, Kasahara Y, Onaka T, Takahashi N, Kaeada T, Nishimori K (2008) Oxytocin receptor-deficient mice developed late-onset obesity. NeuroReport 19:951–955
Tapp EG, Chisholm DJ, Freund J, Boutcher SH (2008) The effects of high-intensity intermittent exercise training on fat loss and fasting insulin levels of young women. Int J Obes 32:684–691
Thornell LE (2011) Sarcopenic obesity: satellite cells in the aging muscle. Curr Opin Clin Nutr Metab Care 14:22–27
Tilg H, Moschen AR (2006) Adipocytokines: mediators linking adipose tissue, inflammation and immunity. Nat Rev Immunol 6:772–783
Timmerman KL, Dhanani S, Glynn EL, Fry CS, Drummond MJ, Jennins K, Rasmussen BB, Volpi E (2012) A moderate acute increase in physical activity enhances nutritive flow and the muscle protein anabolic response to mixed nutrient intake in older adults. Am J Clin Nutr 95:1403–1412
Turpin SM, Ryall JG, Southgate R, Darby I, Hevener AL, Febbraio MA et al (2009) Examination of lipotoxicity’ in skeletal muscle of high-fat fed and ob/ob mice. J Physiol 587:1593–1605
Urban RJ, Bodenburg YH, Gilkison C, Foxworth J, Coggan AR, Wolfe RR, Ferrando A (1995) Testosterone administration to elderly men increases skeletal muscle strength and protein synthesis. Am J Physiol 32:E820–E826
Van Herpen NA, Schrauwen-Hinderling VB (2008) Lipid accumulation in non-adipose tissue and lipotoxicity. Physiol Behav 94:231–241
Vilarrasa N, Vendrell J, Maravall J, Broch M, Estepa A, Begia A, Soler J, Simon I, Richart C, Gomez JM (2005) Distribution and determinants of adiponectin, resistin and ghrelin in a randomly selected healthy population. Clin Endocrinol 63:329–335
Villareal DT, Smith GI, Sinacore DR, Shah K, Mittendorfer B (2011) Regular multi-component exercise increases physical fitness and muscle protein anabolism in frail, obese, older adults. Obesity 19:312–318
Volkert D (2013) Malnutrition in older adults-urgent need for action: a plea for improving the nutritional situation of older adults. Gerontology 59:328–333
Volkert D, Sieber CC (2011) Protein requirements in the elderly. Int J Vitam Nutr Res 81:109–119
Walker DK, Dickinson JM, Timmerman KL, Drummond MJ, Reidy PT, Fry CA, Gundermann DM, Rasmussen BB (2011) Exercise, amino acids and aging in the control of human muscle protein synthesis. Med Sci Sports Exerc 43:2249–2258
Waters DL, Baumgartner RN, Garry PJ, Vellas B (2010) Advantages of dietary, exercise-related, and therapeutic interventions to prevent and treat sarcopenia in adult patients: an update. Clin Interv Aging 5:259–270)
Watt MJ, Hebvener A, Lancaster GI, Febbraio MJ (2006) CNTF reverses obesity-induced insulin resistance by activating skeletal muscle AMPK. Nat Med 12:541–548
Wei Y, Wand D, Topczewski F, Pagliassotti MJ (2006) Saturated fatty acids induce endoplasmatic reticulum stress and apoptosis independently of ceramide in liver cells. Am J Physiol Endocrinol Metab 291:E275–E281
Wende AR, Schaeffler PJ, Parker GJ, Zechner C, Han DH, Chen MM, Hancook CR, Lehmann JJ, Huss JM, McClain DA, Hollszy JO, Kelly DP (2007) A role for the transcriptional coactivator PGC-1 alpha in muscle refueling. J Biol Chem 282:36642–36651
Wenz T, Rossi SG, Rotundo RG, Spiegelman BM, Moraes CT (2009) Increased muscle PGC-1α expression protects from sarcopenia and metabolic disease during aging. Proc Nat Acad Sci USA 106:20405–20410
White TA, LeBrasseur NK (2014) Myostatin and sarcopenia: opportunities and challenges—a mini-review. Gerontology 60:289–293
Wisloff U, Stoylen A, Loennechen JP, Bruvold M, Rognmo O, Haram PM, Tjonna AE, Helgerud J, Slordahl SA, Lee SJ, Videm V, Bye A, Smith GL, Najjar SM, Ellingsen O, Skjaerpe T (2007) Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients. A randomized study. Circulation 115:3086–3094
Yamauchi T, Kamon J, Minokoshi Y, Ito Y, Waki H, Uchida S, Yamashita S, Noda M, Kita S, Ueki K, Eto K, Ananuma Y, Froguel P, Foufelle F, Ferre P, Carling D, Kimura S, Nagai R, Kahn BB, Kadowaki T (2002) Adiponectin stimulates glucose utilization and fatty acid oxidation by activating AMP-activated protein kinase. Nat Med 11:1288–1295
Yamauchi T, Kamon J, Ito Y, Tsuchida A, Yokomizo T, Kita S, Sugiyama T, Miyagishi M, Hara K, Tsunoda M, Murakami K, Ohteki T, Uchida S, Takekaea S, Waki H, Tsuno NH, Shibata Y, Terauchi Y, Froguel P, Tobe K, Koyasu S, Taira K, Kitamura T, Shimizu T, Nagai R, Kadowaki T (2003) Cloning of adiponectin receptors that mediate antidiabetic metabolic effects. Nature 423:762–769
Yarasheski KE, Bhasin S, Sinha-Hikim I, Pak-Loduca J, Gonzalez-Cadavid NF (2002) Serum myostatin-immunoreactive protein is increased in 60-92 year old women and men with muscle wasting. J Nutr Health Aging 6:343–348
Yeap BB, Paul Chubb SA, Lopez D, Ho KKY, Hankey GJ, Flicker L (2012) Associations of insulin-like growth factor-I and its binding proteins, and testosterone, with frailty in older men. Clin Endocrinol 78:752–759
Zamboni M, Mazzali G, Zoico E, Harris TB, Meigs JB, Di Franchesco V, Fantin F, Bissoli L, Bosello O (2005) Health consequences of obesity in the elderly: a review of four unresolved questions. Int J Obes 29:1011–1029
Zamboni M, Mazzali G, Fantin F, Rossi A, Di Franchesco V (2008) Sarcopenic obesity: a new category of obesity in the elderly. Nutr Metab Cardiovasc Dis 18:388–395
Zhang G, Bai H, Zhang H, Dean C, Wu Q, Li J, Guariglia S, Meng Q, Cai D (2011) Neuropeptide exocytosis involving synaptotagmin-4 and oxytocin in hypothalamic programming of body weight and energy balance. Neuron 69:523–535
Acknowledgments
The authors would like to thank the Bayerische Forschungsstiftung which supports the working group within the research association “Amyotrophia (Sarcopenia) and Osteoporosis—Consequence of limited regeneration in age (FORMOsA).
Conflict of interest
No conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kob, R., Bollheimer, L.C., Bertsch, T. et al. Sarcopenic obesity: molecular clues to a better understanding of its pathogenesis?. Biogerontology 16, 15–29 (2015). https://doi.org/10.1007/s10522-014-9539-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10522-014-9539-7