Abstract
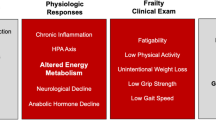
The frailty syndrome is increasingly recognized by geriatricians to identify elders at an extreme risk of adverse health outcomes. The physiological changes that result in frailty are complex and up to now have been extremely difficult to characterize due to the frequent coexistence of acute and chronic illness. Frailty is characterized by an decline in the functional reserve with several alterations in diverse physiological systems, including lower energy metabolism, decreased skeletal muscle mass and quality, altered hormonal and inflammatory functions. This altered network leads to an extreme vulnerability for disease, functional dependency, hospitalization and death. One of the most important core components of the frailty syndrome is a decreased reserve in skeletal muscle functioning which is clinically characterized by a loss in muscle mass and strength (sarcopenia), in walking performance and in endurance associated with a perception of exhaustion and fatigue. There are a number of physiological changes that occur in senescent muscle tissues that have a critical effect on body metabolism. The causes of sarcopenia are multi-factorial and can include disuse, changing hormonal function, chronic diseases, inflammation, insulin resistance, and nutritional deficiencies. In this review, we will explore the dysregulation of some biological mechanisms that may contribute to the pathophysiology of the frailty syndrome through age-related changes in skeletal muscle mass and function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Aging is associated with a reduced ability to respond to internal and external stressors. An age-related reduction of functional reserve occurs in many physiological systems leaving older persons vulnerable to diverse diseases and at an increased risk of functional dependence. A continuous decline in the functional reserve activates a vicious cycle leading to the frailty syndrome. Frailty is a geriatric syndrome that compromises the ability to maintain a stable homeostasis (Fried et al. 2001) and is associated with an increased risk for multiple adverse health-related outcomes, including falls, fractures, disability, institutionalization and death (Fried et al. 2001; Bandeen-Roche et al. 2006). Frailty is considered a continuum rather than a discrete process, where several stages or degrees of severity can be reversed with appropriate interventions.
In 2001, Fried et al. developed an interpretive framework that combined the elements of the “body composition” and “mobility” domains of the frailty syndrome into a pathophysiologic pathway where sarcopenia by limiting mobility and physical activity reduces total energy expenditure and nutritional intake, which in turn, leads to weight loss and a further worsening of sarcopenia.
Even though there are conflicting ideas on the criteria defining frailty, as well as it’s relationship with aging, disability and disease, the general consensus is that frailty may be clinically identified through the following domains: (a) mobility, such as lower extremity performance and gait abnormalities; (b) muscle weakness; (c) poor exercise tolerance; (d) unstable balance; (e) factors related to body composition such as malnutrition, sarcopenia and weight loss. The validity of these factors as components of frailty is provided by studies showing that in older, non-disabled persons, individual components are associated with geriatric syndromes like falls, depression, urinary incontinence and functional impairment which are all strong and independent risk factors for disability and death. We will discuss the intricate alterations of age-related skeletal muscle functioning, sarcopenia, and the center role it plays in the development of the frailty syndrome.
Frailty
The term “frailty” is widely used to characterize a multidimensional syndrome of the loss of reserves that gives rise to vulnerability, weakness, instability and limitation. Even though there still is not a clear definition of frailty, there is a general agreement that the main feature of frailty is increased vulnerability to stressors due to impairments in multiple, inter-related systems that lead to decline in the homeostatic reserve (Bergman et al. 2007).
At the moment there are numerous clinical approaches for identifying frailty in older persons. Most of these definitions include mobility, balance, muscle strength, nutritional status, and physical activity as clinical markers of frailty (Fried et al. 2001; Studenski et al. 2004; Xue et al. 2008; Ensrud et al. 2008; García-González et al. 2009). Other operational definitions also include clinical parameters of depression, urinary incontinence and cognitive impairment (Rockwood et al. 2005; Rolfson et al. 2006).
The most frequently used methods for identifying Frailty was described by Fried et al. using data from the Cardiovascular Health Study. Fried et al. (2001) proposed an operational definition of frailty with the presence of at least one of the following clinical features: poor grip strength, self-reported exhaustion, unexplained weight loss, slow walking speed, and reduced physical activity. The absence of any feature suggests that the individual is not frail. Using this operational definition, the presence of at least three of these five features would characterize and individual as frail and an individual with two of these features would be considered as “pre-frail”.
Tables 1 and 2 summarize some of the clinical markers used to identify the frailty syndrome components using data from large population studies.
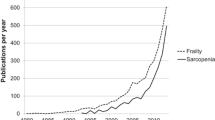
Sarcopenia
Changes in skeletal muscle loss include three categories: cachexia, sarcopenia, and inactivity (atrophy) (Evans 2010). Each of these conditions results in a metabolic adaptation of increased protein degradation (cachexia), decreased rate of muscle protein synthesis (inactivity), or an alteration in both (sarcopenia). Cachexia is characterized by a loss of skeletal muscle and body weight and is considered a metabolic condition associated with an underlying illness and inflammation (Evans 2010). Sarcopenia is the age-associated loss of skeletal muscle and function (Evans 2010; Cruz-Jentoft et al. 2010) Sarcopenia is a complex syndrome that may also be associated with muscle mass loss alone or in combination with increased fat mass. The causes of sarcopenia are multi-factorial and can include disuse, changing endocrine function, chronic diseases, inflammation, insulin resistance, and nutritional deficiencies (Morley et al. 2002). Sarcopenia is considered a major component in the pathway leading to frailty (Fig. 1).
A number of physiological functions that take place within muscle tissues have a critical effect on human metabolism in the development of sarcopenia: muscles are a reservoir of body proteins and energy that can be utilized in periods of extreme stress or malnutrition; amino-acids can be mobilized during acute infections and are used as building blocks for antibodies; hormones are produced and catabolized in muscle tissue. Thus, age-related muscle mass reduction may explain the lower metabolic adaptation and immunological response to disease. Indeed, poor muscle strength is a strong predictor of mortality, independent of any other known risk factors for poor muscle strength. The rate of decline varies among individuals and is influenced by factors that modulate the balance between catabolic and anabolic processes. There are several possible mechanisms that may be involved in the genesis of sarcopenia. Several hypotheses have been proposed, which include: (1) intrinsic biochemical and physical changes leading to muscle atrophy (Carmeli et al. 2002); (2) reduced neuronal stimulation due to reduction in the number of α-motoneurons or their activity (Erim et al. 1999); (3) oxidative damage of mitochrondrial DNA with accumulations of mutations that reduce the efficiency of the metabolic pathways aimed at energy production (McKenzie et al. 2002); (4) influence of external factors such as, malnutrition, sedentary life-style and disease typically observed in older persons (Baumgartner et al. 1996); (5) loss of endogenous hormone production (Kamel et al. 2002); (6) dysregulation of catabolic cytokines (Roubenoff 1997). Over the aging process, there is an increase in intramuscular lipid content, myosteatosis (Delmonico et al. 2007) which may also be contribute to altered muscle function. The most studied of these above mechanisms include: malnutrition, changes in anabolic hormonal signaling and a prolonged pro-inflammatory state.
One approach to a clinical assessment of sarcopenia has been recently proposed by the European Working Group on Sarcopenai in Older People (EWGSOP) (Cruz-Jentoft 2010). These authors proposed the following parameters for the diagnosis of sarcopenia in older persons: (1) presence of low muscle mass plus (2) low muscle strength and/or (3) low physical performance. The assessment techniques in the clinical practice for measuring muscle mass include: the use of bioimpedance analysis, dual energy x-ray absorptiometry, computed tomography, magnetic resonance imaging or total or partial body potassium per fat-free soft tissue; for measuring muscle strength include: handgrip strength, knee extension/flexion, peak expiratory flow; for measuring physical performance include: short physical performance battery, usual gait speed, timed get-up-and-go test, stair climb power test. Lastly, using cut-off determinations based on the reference studies for such clinical parameters, this group has proposed a working definition for the diagnosis of sarcopenia in older adults (Cruz-Jentoft et al. 2010).
Sarcopenia and it’s role on frailty syndrome
Frailty and sarcopenia are considered high relevant and interconnected conditions with regard to functional independence (Theou et al. 2008). Although frailty is considered a geriatric syndrome, sarcopenia is a clinical finding linked to the changes in body composition including those that occur over aging. As one ages, fat mass increases and accumulates preferentially in the abdominal area, while a parallel decline in muscle mass and bone density occurs. The changes in body composition that are seen during early adulthood may be partially explained by a decrease in physical activity, basal metabolic rate, decreased energy needs coupled with a maintenance in energy intake resulting in a persistent positive energy balance. In older adults, however, these changes are accelerated compared to younger cohorts, and cannot be explained by an imbalance between energy intake and expenditure, alone.
There is growing evidence that the core target of the frailty syndrome is motor organization, and specifically of the skeletal muscle and nervous systems. Age-related changes in neuro-muscular morphology and function have been studied (Porter et al. 1995; Roos et al. 1997; Evans 2010) showing a significant decline in muscle strength and quality. Disease, disuse and aging trigger mechanisms that weaken the redundancy of muscular and nervous backups systems, leading to a measurable decline of motor performance and maximal aerobic capacity.When the damage goes beyond the threshold of possible compensation, a measurable decline of motor performance occurs. Furthermore, reduced neuronal stimulation due to an age-related decline in the number of the motor units leads to both lower muscle mass and strength. Once the process is activated, its consequences follow a common pathway leading to a more generalized loss of motor functioning, contributing to sarcopenia. Considering that the mechanisms leading to sarcopenia often overlap with those of frailty, it should be emphasized that sarcopenia, in turn, plays a role toward the development of the frailty syndrome in older adults. Indeed, poor nutrition status, age-related decline in hormonal signaling and a prolonged pro-inflammatory state are interconnected and are likely to be powerful influences on frailty and disability in old age (Fig. 1). Some biomarkers and pathways associated with muscle metabolism dysregulation and frailty in such an interconnected age-related system will be highlighted.
Poor appetite regulation in the elderly and the role of poor nutrition on muscle metabolism
It is now well-known that a physiological anorexia in elderly people can play an important role in the decline of function in older persons (Morley 2001). Specific nutritional deficiencies (dietary protein and vitamin D) are considered major contributors to sarcopenia, which in turn starts the initial cycle of the frailty spiral (Visser et al. 2003).
In older persons, a decline in serum cholesterol levels, which is a marker of both malnutrition and pro-inflammatory cytokine overload, is also considered a marker for frailty (Volpato et al. 2001a, b). A vitamin deficiency will cause a deficiency in defense mechanisms against free radicals (Weindruch 1995). An age-related deficit in Vitamin D is related to muscle weakness (Visser et al. 2003) and lower physical performance in older persons (Wicherts et al. 2007). Furthermore, data from the InCHIANTI study (Bartali et al. 2006) showed that a low intake of vitamins D (OR: 2.35; 95% CI: 1.48–3.73), E (OR: 2.06; 95% CI: 1.28–3.33), C (OR: 2.15; 95% CI: 1.34–3.45) were independently associated with frailty. Indeed, multi-vitamin supplementation has been shown to improve muscle functioning during exercise protocols (Fry et al. 2006).
Total body protein, lean body mass and the rates of protein synthesis decline with aging. More importantly, such alterations are components of an impaired homeostatic phenomenon, which is not always equilibrated with adequate dietary protein intake. Lipid and lipoprotein concentrations vary over the lifespan. In particular, total cholesterol and triglyceride levels tend to increase up until 50 years of age and then a gradual decline starts to occur. A positive correlation exists between total cholesterol and/or triglyceride levels with the incidence of cardiovascular disease up to the age of 50 years. However, the ability of total cholesterol to predict coronary heart disease persons over the age of 70 years remains controversial. Raiha et al. (1997) reported that an elevated level of total cholesterol was not a cardiovascular risk in older persons, but predicted survival for non-cardiovascular disease mortality, while Manolio et al. (1993) did not find any correlation between total cholesterol and all-cause mortality in older subjects. Furthermore, studies have reported that persistently low cholesterol levels increased the risk of mortality in males aged 71 to 93 (Schatz et al. 2001). Such discrepancies may be explained by the fact that one of the major differences between middle-aged and older populations is the presence of an increased prevalence of poorer health status of older individuals. In fact, older frail persons with low total cholesterol levels are more likely to have a decreased survival rate than older persons with little or no disease in the presence of chronically low cholesterol values (Pekkanen et al. 1994). Interestingly, after adjusting for frailty markers in a large sample of older persons, elevated total cholesterol levels predicted an increased risk for death from coronary heart disease (CHD), and the risk of death from CHD decreased as cholesterol levels declined (Corti et al. 1997). These authors also emphasized the finding that frailty markers were consistently associated with low cholesterol levels, thus confirming those of previous reports.
Regarding lipoproteins, high density lipoprotein cholesterol (HDL-C) has been hypothesized to be a reliable marker of frailty and poor prognosis among the oldest elderly (Zuliani et al. 1999). Lower HDL cholesterol was considered a risk factor for not only ischemic heart disease but also cerebrovascular disease, especially in diseased elderly (Hayashi et al. 2009). Furthermore, it has been shown that reduced HDL-C also predicted non-CHD/stroke mortality in older persons (Volpato et al. 2001a). A recent report tested the impact of HDL cholesterol on the risk of all-cause mortality in a large population of frail community dwelling elders (Landi et al. 2008). These authors found that the serum levels of HDL cholesterol were inversely associated with all-cause deaths in frail men and women. This finding may be explained by a lack of ‘protective’ functions of HDL cholesterol including its promotion of reverse cholesterol transport, anticoagulant properties, antioxidant activity, and anti-inflammatory actions on endothelial cells (Zuliani et al. 1999).Thus, low HDL-C may also be considered a valid biomarker for chronic disease and frailty in old age.
Although the rate of muscle protein synthesis in the fasted state may not change with aging (Volpi et al. 2001) it is lower in older people (compared to young) in the post-prandial state when amino acid availability does not limit rate of synthesis (Katsanos et al. 2005). Despite a lower muscle mass, older people have increased protein needs compared to those of younger people (Campbell et al. 2001). Protein supplementation in combination with resistance training have been shown to increase muscle mass, strength and functional performance in older and very old frail adults (Fiatarone et al.1994).
This age-related reduced rate of muscle protein synthesis may not only be explained by decreased levels of physical activity, but also by lower levels of anabolic signaling to muscle function in hormones, including Insulin-like Growth Factor-1 (IGF-1), Growth hormone (GH), Testosterone or an increased degree of insulin resistance (IR).
Changes in anabolic hormonal signaling
Insulin-like growth factor-1 and growth hormone
High IGF-1 concentrations are associated with characteristics that are opposite to those typical of aging, including decreased body fat content, increased muscle mass and improved metabolic homeostasis of glucose and lipids. At the muscular level, IGF-1 stimulates protein synthesis and satellite cell differentiation. Many studies have provided insight into the signaling pathways by which IGF-1 affects muscle anatomy and function (Cappola et al. 2002, Cappola et al. 2003). Circulating IGF-1 concentrations decrease with advancing age. The age-associated decline in IGF-1 plasma concentrations is influenced by reduced GH levels, and also by nutritional status, insulin and inflammatory cytokines. Specifically, the biologic activity of IGF-1 on muscle strength can be inhibited by Interleukin-6 (IL-6) suggesting that the detrimental effect of inflammation on muscle functioning may be mediated by IGF-1. Furthermore, studies provide evidence that the higher concentrations of pro-inflammatory cytokines found in older persons directly interfere with the IGF-1 gene protein expression and receptor sensibility in muscles (Cappola et al. 2003; Barbieri et al. 2003). High IL-6 and low IGF-1 plasma concentrations are considered risk factors for poor muscle strength, poor lower extremity performance and disability.
An age-related decline of GH negatively influences IGF-1 muscle response. There is evidence that the age-associated decline in GH levels in combination with lower IGF-1 levels contributes to the development of sarcopenia (Ferrucci et al. 2002). The reduced pituitary secretion of GH is probably due to age-related changes in the GH-releasing hormone (GHRH). Unfortunately, treatment with GH has demonstrated many adverse effects such as, peripheral edema, arthralgias, glucose intolerance and type 2 diabetes (Blackman et al. 2002). One investigation demonstrated that therapy with GHRH (somatorelin) in older persons was capable of restoring the age-related decline of the GH response (Kelijam 1991). More studies are underway in order to verify whether such pharmacological approaches can restore muscle functioning, as well as metabolic homeostasis in elderly persons while minimizing side effects.
Testosterone
Testosterone affects muscle mass and muscle strength both directly and indirectly. It has been reported that testosterone increases protein synthesis and intramuscular mRNA concentrations of IGF-1 and decreases inhibitory IGF binding protein 4 concentrations (Urban et al. 1995). Due to evidence that testosterone levels decline with advancing age, a negative impact on muscle function is not surprising. Older men with low circulating levels of testosterone tend to have lower muscle strength than men of the same age with normal testosterone, and studies utilizing supplemental therapy with testosterone have shown an increase in muscle mass and strength in elderly males. Testosterone has also been linked to body composition changes such as an increase in muscle mass and a decrease in fat mass (Sattler et al. 2009). A small number of studies have suggested an improvement in muscle mass and strength with testosterone treatment with aging (Caminiti et al. 2009; Sattler et al. 2009).
Insulin resistance
A significant increase in peripheral insulin resistance (IR) develops as individuals age, and recent reports have consistently demonstrated that age-related IR is an independent determinant of poor muscle strength in older persons (Lazarus et al. 1997; Abbatecola et al. 2005). It is also widely known that insulin plays a pivotal role for valid muscle functioning by increasing glucose uptake and promoting intracellular glucose metabolism, thus it is plausible that age-related IR may be a determinant of sarcopenia. Lower peripheral activity of insulin may reduce the muscle tissue anabolic rate leading to a relative catabolic state and in turn, facilitating sarcopenia. The contraction of type I fibers is especially dependent on glucose entry and metabolism compared to type II fibers (Song et al. 1999). Type I fibers are more responsive to insulin, and are more representative of the muscle in older persons (Staron et al. 2000). Inactivity is a potent cause of insulin resistance and exercise results in improved mitochondrial function and improved insulin sensitivity (Hughes et al. 1993). Over the aging process, both changes in the contractile efficiency of muscle fibers and changes in tissue quality, such as an increase in connective tissue and peri-cellular fat infiltration may also be contribute to altered muscle function. IR-linked myosteatosis is most probably explained by a mitochondrial defect leading to failure in the use of intracellular fat, or from an increase in circulating triglycerides, or from reduced levels of physical activity (Morino et al. 2006). An accumulation of fatty acids in muscle cells will lead to an abnormal phosphorylation of the insulin receptor substrate, which in turn will inhibit the GLUT-4 translocation pathway. Therefore, lower muscle functioning due to altered insulin action in skeletal muscle seems to be more evident in older persons.
Inflammation of aging
Normally, cytokines or other biomarkers of inflammation initiate and regulate the acute phase inflammatory response during an infection, a trauma or any other type of stress. However, it has been suggested that over aging, a primary dysregulation of the mechanisms that initiate, modulate and shut off an inflammatory response often occurs (Brunnsgard et al. 2001). This phenomenon has been defined as “inflammaging” and is characterized by high plasma levels of circulating pro-inflammatory cytokines, including tumor necrosis factor-α (TNF-α), interleukin-6 (IL-6) interleukin-1 (IL-1), as well as acute phase proteins in older persons (Franceschi et al. 2000).
The proinflammatory state of aging has been implicated in the development of sarcopenia due to the effect of increased cytokines on reduced muscle protein synthesis. In particular, IL-6 appears to play a role in accelerating sarcopenia and frailty. In particular, TNF-α and IL-6 have been associated with muscle loss and lower strength in a large sample of older persons (Visser et al. 2002; Schaap et al. 2009). In extreme situations, such as diseases that cause prolonged hypercatabolic states, severe muscle “wasting” or cachexia may develop over a short period due to TNF-α induced muscle proteolysis. However, a certain degree of muscle “decline” has been attributed to the reduced capacity of skeletal muscles to synthesize new proteins in the aging process. Therefore, an imbalance between muscle protein synthesis and degradation occurs, ultimately leading to reduced muscle mass, protein content and strength. Such imbalance may be partially explained by a direct impact of cytokines, such as TNF-α and IL-6 on protein proteolysis, or indirectly through the interference of IGF-1 signaling at the skeletal muscle level (Albright and Albright 2000).
Conclusions
The frailty syndrome is associated with simultaneous alterations in different physiological systems. In this review, we have tried to highlight one of the core elements in the development of frailty- sarcopenia. Even though more studies are necessary to advance the concepts between frailty and aging, its determinants and pathophysiology, preventive measures of sarcopenia need to be investigated. Regularly performed exercise, particularly resistance exercise, has been demonstrated to increase muscle mass, function, walking speed, basal metabolic rate, improve bone health, and increase physical activity even in very old, frail men and women. Strategies to increase levels of activity and improve nutritional status in the frail elderly will have powerful effects on maintaining independence. Only future prevention trials for primary outcomes related to sarcopenia such as muscle mass, muscle strength and physical performance in older persons will be determine factors related to reducing the risk of frailty over aging.
References
Abbatecola AM, Ferrucci L, Ceda G, Russo CR, Lauretani F, Bandinelli S, Barbieri M, Valenti G, Paolisso G (2005) Insulin resistance and muscle strength in older persons. J Gerontol A Biol Sci Med Sci 60:1278–1282
Albright JW, Albright JF (2000) Soluble receptors and other substances that regulate proinflammatory cytokines in young and aging humans. J Gerontol A Biol Sci Med Sci 55:20–25
Bandeen-Roche K, Xue QL, Ferrucci L, Walston J, Guralnik JM, Chaves P, Zeger SL, Fried LP (2006) Phenotype of frailty: characterization in the women’s health and aging studies. J Gerontol A Biol Sci Med Sci 61(3):262–266
Barbieri M, Ferrucci L, Ragno E, Corsi A, Bandinelli S, Bonafe M, Olivieri F, Giovagnetti S, Franceschi C, Guralnik JM, Paolisso G (2003) Chronic inflammation and the effect of IGF-I on muscle strength and power in older persons. Am J Physiol Endocrinol Metab 284(3):E481–E487
Bartali B, Frongillo EA, Bandinelli S, Lauretani F, Semba RD, Fried LP, Ferrucci L (2006) Low nutrient intake is an essential component of frailty in older persons. J Gerontol A Biol Sci Med Sci 61(6):589–593
Baumgartner R, Koehler K, Romero L, Garry P (1996) Serum albumin is associated with skeletal muscle in elderly men and women. Am J Clin Nutr 64:552–558
Bergman H, Ferrucci L, Guralnik J, Hogan DB, Hummel S, Karunananthan S, Wolfson C (2007) Frailty: an emerging research and clinical paradigm–issues and controversies. J Gerontol A Biol Sci Med Sci 62(7):731–737
Blackman MR, Sorkin JD, Munzer T, Bellantoni MF, Busby-Whitehead J, Stevens TE, Jayme J, O’Connor KG, Christmas C, Tobin JD, Stewart KJ, Cottrell E, St Clair C, Pabst KM, Harman SM (2002) Growth hormone and sex steroid administration in healthy aged women and men: a randomized controlled trial. JAMA 288(18):2282–2292
Brunnsgard H, Pederson M, Pederson BK (2001) Aging and proinflammatory cytokines. Curr Opin Hematol 8:131–136
Caminiti G, Volterrani M, Iellamo F, Marazzi G, Massaro R, Miceli M, Mammi C, Piepoli M, Fini M, Rosano GM (2009) Effect of long-acting testosterone treatment on functional exercise capacity, skeletal muscle performance, insulin resistance, and baroreflex sensitivity in elderly patients with chronic heart failure a double-blind, placebo-controlled, randomized study. J Am Coll Cardiol 54(10):919–927
Campbell WW, Trappe TA, Wolfe RR, Evans WJ (2001) The recommended dietary allowance for protein may not be adequate for older people to maintain skeletal muscle. J Gerontol A Biol Sci Med Sci 56:M373–M380
Cappola AR, Bandeen-Roche K, Wand GS, Volpato S, Fried LP (2002). Association of IGF-I levels with muscle strength and mobility in older women. J Clin Endocrinol Metab. 2001;86(9):4139-46
Cappola A, Qian-Li X, Ferrucci L, Guralnik JM, Volpato S, Fried LP (2003) Insulin-like Growth Factor I and Interleukin-6 Contribute Synergistically to Disability and Mortality in Older Women. J Clin Endocrinol Metab 88:2019–2025
Carmeli E, Coleman R, Reznick AZ (2002) The biochemistry of aging muscle. Exp Gerontol 37:477–489
Corti MC, Guralnik J, Salive M, Harris T, Ferrucci L, Glynn R, Havlik R (1997) Clarifying the direct relation between total cholesterol levels and death from coronary heart disease in older persons. Annuals of Internal Medicine 126:753–760
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, Michel JP, Rolland Y, Schneider SM, Topinková E, Vandewoude M, Zamboni M (2010) Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. (Epub ahead of print)
Delmonico MJ, Harris TB, Lee JS, Visser M, Nevitt M, Kritchevsky SB, Tylavsky FA, Newman AB (2007) Alternative definitions of sarcopenia, lower extremity performance, and functional impairment with aging in older men and women. J Am Geriatr Soc 55:769–774
Ensrud KE, Ewing SK, Taylor BC, Fink HA, Cawthon PM, Stone KL, Hillier TA, Cauley JA, Hochberg MC, Rodondi N, Tracy JK, Cummings SR (2008) Comparison of 2 frailty indexes for prediction of falls, disability, fractures, and death in older women. Arch Intern Med 25 168:382–389
Erim Z, Beg MF, Burke DT, de Luca CJ (1999) Effects of aging on motor-unit control properties. J Neurophysiol 82(5):2081–2091
Evans WJ (2010) Skeletal muscle loss: cachexia, sarcopenia, and inactivity. Am J Clin Nutr. Feb 17
Ferrucci L, Penninx BW, Volpato S, Harris TB, Bandeen-Roche K, Balfour J, Leveille SG, Fried LP, Md JM (2002) Change in muscle strength explains accelerated decline of physical function in older women with high interleukin-6 serum levels. J Am Geriatr Soc 50(12):1947–1954
Fiatarone MA, O’Neill EF, Ryan ND, Clements KM, Solares GR, Nelson ME, Roberts SB, Kehayias JJ, Lipsitz LA, Evans WJ (1994) Exercise training and nutritional supplementation for physical frailty in very elderly people. N Engl J Med 330(25):1769–1775
Filho ST, Lourenço RA, Moreira VG (2010) Comparing indexes of frailty: the cardiovascular health study and the study of osteoporotic fractures. J Am Geriatr Soc 58(2):383–385
Franceschi C, Bonafè M, Valensin S, Olivieri F, De Luca M, Ottaviani E, De Benedictis G (2000) Inflamm-aging: an evoluzinary perspective on immunosenescence. Ann NY Acad Sci 908:244–254
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA, Cardiovascular Health Study Collaborative Research Group (2001) Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56:M146–M156
Fry AC, Bloomer RJ, Falvo MJ, Moore CA, Schilling BK, Weiss LW (2006) Effect of a liquid multivitamin/mineral supplement on anaerobic exercise performance. Res Sports Med 1:53–64
García-González JJ, García-Peña C, Franco-Marina F, Gutiérrez-Robledo LM (2009) A frailty index to predict the mortality risk in a population of senior mexican adults. BMC Geriatr 9:47
Hayashi T, Kawashima S, Itoh H, Yamada N, Sone H, Watanabe H, Hattori Y, Ohrui T, Yokote K, Nomura H, Umegaki H, Iguchi A, Japan CDM Group (2009) Low HDL cholesterol is associated with the risk of stroke in elderly diabetic individuals: changes in the risk for atherosclerotic diseases at various ages. Diabetes Care 32:1221–1223
Hughes VA, Fiatarone MA, Fielding RA, Kahn BB, Ferrara CM, Shepherd P, Fisher EC, Wolfe RR, Elahi D, Evans WJ (1993) Exercise increases muscle GLUT-4 levels and insulin action in subjects with impaired glucose tolerance. Am J Physiol 264:E855–E862
Kamel H, Maas D, Duthie E (2002) Role of hormones in the pathogenesis and management of sarcopenia. Drugs Aging 19:869–877
Katsanos CS, Kobayashi H, Sheffield-Moore M, Aarsland A, Wolfe RR (2005) Aging is associated with diminished accretion of muscle proteins after the ingestion of a small bolus of essential amino acids. Am J Clin Nutr 82:1065–1073
Kelijam M (1991) Age-related alterations of growth hormone/insulin-like-growth-factor J axis. J Am Geriatr Soc 39:295–307
Landi F, Russo A, Pahor M, Capoluongo E, Liperoti R, Cesari M, Bernabei R, Onder G (2008) Serum high-density lipoprotein cholesterol levels and mortality in frail, community-living elderly. Gerontology 54(2):71–78
Lazarus R, Sparrow D, Weiss ST (1997) Handgrip strength and insulin levels: cross-sectional and prospective associations in the normative aging study. Metabolism 11:1266–1269
Manolio TA, Ettinger WH, Tracy RP, Kuller LH, Borhani NO, Lynch JC, Fried LP (1993) Epidemiology of low cholesterol levels in older adults. The Cardiovascular Health Study. Circulation 87:728–737
McKenzie D, Bua E, McKiernan S, Cao Z, Aiken JM, Wanagat J (2002) Mitochondrial DNA deletion mutations: a causal role in sarcopenia. Eur J Biochem 269:2010–2015
Morino K, Petersen KF, Shulman GI (2006) Molecular mechanisms of insulin resistance in humans and their potential links with mitochondrial dysfunction. Diabetes 55:S9–S15
Morley JE (2001) Anorexia, sarcopenia, and aging. Nutrition 17:660–663
Morley JE, Perry HM 3rd, Miller DK (2002) Editorial: something about frailty. J Gerontol A Biol Sci Med Sci 57(11):M698–M704
Pekkanen J, Nissinen A, Vartiainen E, Salonen JT, Punsar S, Karvonen MJ (1994) Changes in serum cholesterol level and mortality: a 30 year follow up. Am J Epidemiol 139:155–165
Porter MM, Vandervoort AA, Lexell J (1995) Aging of human muscle: structure, function and adaptability. Scand J Med Sci Sports 5(3):129–142
Raiha I, Marniemi J, Puukka P, Toikka T, Ehnholm C, Sourander L (1997) Effect of serum lipids, lipoproteins, and apolipoproteins on vascular and nonvascular mortality in the elderly. Arterioscler Thromb Vasc Biol 17(7):1224–1232
Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, Mitnitski A (2005) A global clinical measure of fitness and frailty in elderly people. CMAJ 173(5):489–495
Rolfson DB, Majumdar SR, Tsuyuki RT, Tahir A, Rockwood K (2006) Validity and reliability of the Edmonton Frail Scale. Age Ageing 35(5):526–529
Roos MR, Rice CL, Vandervoort AA (1997) Age-related changes in motor unit function. Muscle Nerve 20(6):679–690
Roubenoff R (1997) Inflammatory and hormonal mediators of cachexia. J Nutr 127:1014S–1016S
Sattler FR, Castaneda-Sceppa C, Binder EF, Schroeder ET, Wang Y, Bhasin S, Kawakubo M, Stewart Y, Yarasheski KE, Ulloor J, Colletti P, Roubenoff R, Azen SP (2009) Testosterone and growth hormone improve body composition and muscle performance in older men. J Clin Endocrinol Metab 94(6):1991–2001
Schaap LA, Pluijm SM, Deeg DJ, Harris TB, Kritchevsky SB, Newman AB, Colbert LH, Pahor M, Rubin SM, Tylavsky FA, Visser M, Health ABC Study (2009) Higher inflammatory marker levels in older persons: associations with 5-year change in muscle mass and muscle strength. J Gerontol A Biol Sci Med Sci 64(11):1183–1189
Schatz IJ, Masaki K, Yano K, Chen R, Rodriguez BL, Curb JD (2001) Cholesterol and all-cause mortality in elderly people from the Honolulu Heart Program: a cohort study. Lancet 358(9279):351–355
Song XM, Ryder JW, Kawano Y, Chibalin AV, Krook A, Zierath JR (1999) Muscle fiber type specificity in insulin signal transduction. Am J Physiol 277:R1690–R1696
Staron R, Hagerman F, Hikida R, Murrey T, Hostler D, Crilll M, Ragg K, Toma K (2000) Fiber type composition of the vastus lateralis muscle of young men and women. J Histochem Cytochem 48:623–629
Studenski S, Hayes RP, Leibowitz RQ, Bode R, Lavery L, Walston J, Duncan P, Perera S (2004) Clinical Global Impression of Change in Physical Frailty: development of a measure based on clinical judgment. J Am Geriatr Soc 52(9):1560–1566
Theou O, Jones GR, Overend TJ, Kloseck M, Vandervoort AA (2008) An exploration of the association between frailty and muscle fatigue. Appl Physiol Nutr Metab 33(4):651–665
Urban RJ, Bodenburg YH, Gilkison C, Foxworth J, Coggan AR, Wolfe RR, Ferrando A (1995) Testosterone administration to elderly men increases skeletal muscle strength and protein synthesis. Am J Physiol 269(5 Pt 1):E820–E826
Visser M, Pahor M, Taaffe DR, Goodpaster BH, Simonsick EM, Newman AB, Nevitt M, Harris TB (2002) Relationship of interleukin-6 and tumor necrosis factor-alpha with muscle mass and muscle strength in elderly men and women: the Health ABC Study. J Gerontol A Biol Sci Med Sci 57(5):M326–M332
Visser M, Deeg DJ, Lips P (2003) Longitudinal Aging Study Amsterdam Low vitamin D and high parathyroid hormone levels as determinants of loss of muscle strength and muscle mass (sarcopenia): the Longitudinal Aging Study Amsterdam. J Clin Endocrinol Metab 88(12):5766–5772
Volpato S, Leveille S, Corti MC, Harris T, Guralnik J (2001a) The value of serum albumin and high-density lipoprotein cholesterol in defining mortality risk in older persons with low serum cholesterol. J Am Geriatr Soc 49:1142–1147
Volpato S, Zuliani G, Guralnik JM, Palmieri E, Fellin R (2001b) The inverse association between age and cholesterol level among older patients: the role of poor health status. Gerontology 47(1):36–45
Volpi E, Sheffield-Moore M, Rasmussen BB, Wolfe RR (2001) Basal muscle amino acid kinetics and protein synthesis in healthy young and older men. JAMA 286:1206–1212
Weindruch R (1995) Interventions based on the possibility that oxidative stress contributes to sarcopenia. J Gerontol A Biol Sci Med Sci 50:157–161
Wicherts IS, van Schoor NM, Boeke AJ, Visser M, Deeg DJ, Smit J, Knol DL, Lips P (2007) Vitamin D status predicts physical performance and its decline in older persons. J Clin Endocrinol Metab 92(6):2058–2065
Xue QL, Bandeen-Roche K, Varadhan R, Zhou J, Fried LP (2008) Initial manifestations of frailty criteria and the development of frailty phenotype in the Women’s Health and Aging Study II. J Gerontol A Biol Sci Med Sci 63(9):984–990
Zuliani G, Romagnoli F, Bollini C, Leoci V, Soattin L, Fellin R (1999) Low Levels of high-density lipoprotein cholesterol are a marker of disability in the elderly. Gerontology 45:317–322.
Acknowledgments
No sources of funding were used to assist in the preparation of this review. The authors have no conflicts of interest that are directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Evans, W.J., Paolisso, G., Abbatecola, A.M. et al. Frailty and muscle metabolism dysregulation in the elderly. Biogerontology 11, 527–536 (2010). https://doi.org/10.1007/s10522-010-9297-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10522-010-9297-0