Abstract
Some of the most serious consequences of ageing are its effects on skeletal muscle. The term ‘sarcopenia’ describes the slow but progressive loss of muscle mass with advancing age and is characterised by a deterioration of muscle quantity and quality leading to a gradual slowing of movement and a decline in strength. The loss of muscle mass and strength is thought to be attributed to the progressive atrophy and loss of individual muscle fibres associated with the loss of motor units, and a concomitant reduction in muscle ‘quality’ due to the infiltration of fat and other non-contractile material. These age-related changes in skeletal muscle can be largely attributed to the complex interaction of factors affecting neuromuscular transmission, muscle architecture, fibre composition, excitation–contraction coupling, and metabolism. Given the magnitude of the growing public health problems associated with sarcopenia, there is considerable interest in the development and evaluation of therapeutic strategies to attenuate, prevent, or ultimately reverse age-related muscle wasting and weakness. The aim is to review our current understanding of some of the cellular and molecular mechanisms responsible for age-related changes in skeletal muscle.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction: description of the problem
Sarcopenia—age-related muscle wasting is characterised by not only the loss of skeletal muscle mass, but also the gradual decline in muscle function, including a decrease in force producing capacity, maximum velocity of shortening, and a general slowing of contraction and relaxation (Fig. 1a). Intimately linked to the decrease in muscle mass is a ‘metabolic dysregulation’, which includes a reduction in insulin sensitivity, impaired oxidative defense, and decreased mitochondrial function (Giresi et al. 2005; Dela and Kjaer 2006).
Representative isometric twitch contractile responses (a) and myosin ATPase stained cross-sections (b) of EDL muscles from adult (16-month-old), and aged (28-month-old) rats (modified from Schertzer et al. 2005; Ryall et al. 2007). Note the reduction in maximum force, the slowing of twitch response and the increase in the proportion of dark stained type I fibres in old muscles. Adapted from Schertzer et al. 2005 with permission
Sarcopenia affects all elderly and does not discriminate based on ethnicity, gender, or wealth. It can deprive a person of their functional independence, and increase their risk for sudden falls and fractures (Szulc et al. 2005). As the number and proportion of older persons in the population continues to escalate, sarcopenia will impact dramatically on quality of life and place ever-increasing demands on public health care (see Lynch 2004a for review). During ageing, the loss of muscle mass and strength is hypothesised to be due to the progressive atrophy (decrease in myofibre cross-sectional area) and loss of muscle fibres (Einsiedel and Luff 1992; Brooks and Faulkner 1994; McNeil et al. 2005) (Fig. 1b), and a reduction in muscle ‘quality’ due to the infiltration of fat and other non-contractile material such as connective tissue as well as changes in muscle metabolism and insulin resistance (Conley et al. 1995; Cree et al. 2004). These changes are attributed to a complex interaction of many factors that affect neuromuscular transmission, muscle architecture, fibre composition, excitation–contraction (E–C) coupling, and muscle metabolism (Larsson et al. 1979; Edström and Larsson 1987; Plant and Lynch 2002).
With ageing there is also a slowing of movement that affects stability and balance during walking and other activities, which contributes to the increased risk for falls and subsequent fractures in the elderly (Yu et al. 2007). The age-related slowing of contraction has been reported to occur well before the onset of severe muscle wasting indicating that changes intrinsic to the muscle fibres cannot be excluded (Narayanan et al. 1996). Although these age-related changes in skeletal muscle structure and function are influenced by reduced levels of physical activity concomitant with advancing age, it must also be recognised that some of these changes can be attributed specifically to biological processes such as oxidative stress (Hagen et al. 2004). This theory states that a proportion of the age-related changes to skeletal muscle are due to the accumulation of intracellular damage caused by free radical generation across the lifespan (Nagley et al. 1992; Sohal and Weindruch 1996). Based on the findings from numerous studies, Hagen et al. (2004) concluded that “oxidative damage over time leads to mitochondrial DNA mutation deletions that result in dysfunctional mitochondria, and that skeletal muscle is one tissue that is particularly susceptible to this phenomenon (Hagen et al. 2004; Hepple et al. 2006). Thus, independent of age-related changes in physical activity patterns, other deleterious effects of advancing age on skeletal muscle structure, function and metabolism, can be attributed to oxidative damage and other biological processes. These other mechanisms will not be discussed in detail in this review.
Thus, while physical activity can help slow the rate of these neuromuscular impairments, it should be recognised that even very active older adults, such as ‘Master’ athletes who train and compete regularly throughout their adult life, also exhibit a progressive loss of muscle mass and strength that affects sports performance (for review see Faulkner et al. 2007). Therefore, exercise alone cannot prevent age-related changes in skeletal muscle function. Other factors, such as age-related changes in circulating levels of muscle anabolic hormones and growth factors, must also be considered as contributing mechanisms underlying the sarcopenic phenotype. Factors such as general health status and nutrition in conjunction with appropriate physical activity can help attenuate the rate of physical decline, preserve functional independence and maintain quality of life. Although it is generally accepted that age-related changes in skeletal muscle structure and function are inevitable, whether these deleterious effects on skeletal muscle can be stopped or reversed is debatable.
The aim of this brief review is to provide a description of our current understanding of some of these mechanisms including age-related changes to the systemic environment and changes intrinsic to skeletal muscle.
Age-related impairments in neuromuscular function
Muscle contraction is initiated and sustained through the successive recruitment of motor units; a motor unit defined as an alpha-motor neuron and all the muscle fibres it innervates. Motor unit remodelling, whereby muscle fibres are progressively denervated and either lost completely or subsequently reinnervated by sprouting of remaining neurons, is considered a major contributing factor to the age-related loss of muscle force and power, and studies on animals and humans have demonstrated a preferential loss of fast motor units with advancing age (reviewed in Faulkner et al. 2007). However, the extent of these motor unit losses appears to vary considerably, and could influenced by the neurotrophic effects of circulating growth factors [e.g. insulin-like growth factor-I (IGF-I)] that can promote motor neuron survival (Messi and Delbono 2003). Recent evidence indicates that these motoneuron losses might be relatively small, in the order of ∼10–15% even in advanced age (Edstrom et al. 2007). Regardless, the deleterious changes to the neuromuscular system are progressive and can impact severely on motor performance.
The neuromuscular junction (NMJ) has been observed to undergo significant periods of remodelling during early development and during ageing. While the remodelling of the NMJ during embryogenesis is required for successful development, the remodelling during advancing age often results in detrimental changes that can impair neuromuscular transmission (for review see Delbono 2003). Interestingly, fast-twitch skeletal muscles appear to experience a greater level of NMJ remodelling than slow-twitch muscles (Rosenheimer and Smith 1985; Prakash and Sieck 1998).
Cohen et al. (2007) found that histone deacetylase 4 (HDAC4) played an important role in connecting neural activity to skeletal muscle gene expression, and that HDAC4 was localised to the NMJ. When innervation was compromised (either through surgical denervation or as a consequence of neuromuscular disease) HDAC4 translocated to the nucleus, which resulted in altered transcription of genes regulating synaptic proteins (such as nicotinic acetylcholine receptors), and the ubiquitin ligase atrogin-1 (also known as muscle atrophy F-box, MAFbx). It is interesting to speculate on a potential role for HDAC4 in the age-related changes in skeletal muscle.
Age-related changes to the systemic environment
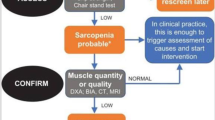
Age-related alterations in circulating (blood-borne) endocrine factors have been the main focus of research linking hormones, growth factors and cytokines to the sarcopenic phenotype (Fig. 2a). The systemic environment of an aged organism appears to be a critical factor for changes in the function of skeletal muscles. However, it must be noted that since ageing affects fast- and slow-twitch skeletal muscles differentially, intrinsic changes to the muscle must also be considered.
Classic experiments in mammalian muscle regeneration revealed that the reduced regenerative potential of cross-transplanted muscle grafts was dictated largely by the age of the host rather than of the donor (Carlson and Faulkner 1989, 1996; Cederna et al. 2001). More recently, this effect was confirmed in a model of parabiosis where young and old mice had a shared circulation (Conboy et al. 2005). Exposure of old muscle to the blood supply from a young mouse restored the regenerative potential that was normally impaired with ageing and increased the efficacy of muscle regeneration without the recruitment of young cells from the shared circulation (Conboy et al. 2003, 2005).
In humans, several hormonal systems show a gradual decline in activity during ageing, as defined by their bioactive hormone concentrations (van den Beld and Lamberts 2002; Chahal and Drake 2007). Of particular interest to sarcopenia is the decline in circulating levels of muscle anabolic hormones such as testosterone, dehydroepiandrosterone (DHEA), growth hormone (GH) and IGF-I and the terms “andropause” and “somatopause”, relate to the decrease in testosterone and its precursors, and somatostatins, respectively (van den Beld and Lamberts 2002). In addition to the well-documented decline in these anabolic hormones, other endocrine systems (including circulating levels of catecholamines) and paracrine/autocrine systems (including local IGF-I production) may play an important role in sarcopenia (Solomon and Bouloux 2006).
Testosterone and its precursors
Well-controlled, double-blinded studies have demonstrated unequivocally that androgens, such as testosterone, regulate muscle mass in humans (Herbst and Bhasin 2004). Testosterone is secreted primarily by testicular Leydig cells in males and ovarian thecal cells in females, and in skeletal muscle bind directly to androgen receptors (ARs) resulting in transformation and dimerisation of the receptor, nuclear localization and subsequent DNA binding (for review see Chen et al. 2005).
Satellite cells and myonuclei are the predominant sites of AR expression (Altuwaijri et al. 2004; Sinha-Hikim et al. 2004) and androgen administration increases satellite cell numbers in animals and humans in a dose-dependent manner (Sinha-Hikim et al. 2004, 2006). Currently, the mechanisms by which androgens increase satellite cell number are unknown but it is thought that they may potentially regulate satellite cell proliferation and differentiation (Chen et al. 2005).
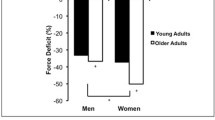
In healthy males, bioavailable testosterone levels drop by as much as 64% between the ages of 25 and 85 years, while in women it falls by 28% (Vermeulen 1991; Morley et al. 1997; Khosla et al. 1998). In addition, the plasma concentration of the testosterone precursor DHEA is ∼5 times lower at age 85 than at age 30 years (Herbert 1995; Nair et al. 2006). Interestingly, the progressive decline in anabolic hormones during ageing is not associated with declines in transcript levels of their respective receptors in skeletal muscle (Marcell et al. 2001). Therefore, the results to date, support the hypothesis that the progressive decline in specific anabolic hormones during ageing is mediated by post-transcriptional alterations.
Several studies have demonstrated a relationship between serum testosterone levels and muscle strength in older men, whereas DHEA levels have not been linked directly to muscle mass or strength. In contrast, a decrease in bioavailable testosterone has not been linked to a decline in muscle mass or strength in women (Iannuzzi-Sucich et al. 2002; Waters et al. 2003; Schaap et al. 2005), indicating a divergent influence of testosterone during ageing. An attractive hypothesis for these disparate results relates to the fact that the sex hormone-binding globulin (SHBG) increases by more than twofold over the male lifespan, and remains unchanged in women (Khosla et al. 1998; van den Beld et al. 2000).
Growth hormone
The circulating (blood-borne) levels of GH declines progressively after ∼30 years of age at an average rate greater than 1% per annum (Zadik et al. 1985; Hermann and Berger 2001). GH predominantly synthesised in the anterior pituitary, is secreted in response to GH releasing hormone (GHRH) and is inhibited by somatostatin (Giustina and Veldhuis 1998). The actions of GH are mediated via the GH receptor (GHR), which subsequently activates the janus kinase 2 (JAK2)—signal transducer and activator of transcription (STAT) pathway (for review see Lanning and Carter-Su 2006).
One of the downstream targets for GH/STAT5b mediated transcription is liver derived IGF-I (Chia et al. 2006). It is therefore not surprising that the age-related decline in GH was believed initially to be indirectly responsible for age-related changes in skeletal muscle via IGF-I (see Sherlock and Toogood 2007 for review). However, GH also has a number of IGF-I independent actions. Sotiropoulos et al. (2006) used mutant mice lacking the GHR to demonstrate that GH signalling promotes skeletal muscle growth by increasing nuclear factor of activated T-cells (NFAT)c2-dependent myogenic precursor cell fusion to existing myotubes, independent of changes to IGF-I. Due to many and varied signalling cascades activated by GH, it is likely that its age-related decline has numerous outcomes for skeletal muscle structure and function. The hypertrophic effects of the GH–IGF-I growth axis are well documented (Isgaard et al. 1988; Turner et al. 1988) and despite a widely held belief that sarcopenia was directly associated with an age-related decline in GH secretion, this view has been contested and studies in humans do not support GH administration as a means for stimulating muscle protein synthesis (for review see Lynch 2004b). However, GH also affects other cellular processes in skeletal muscle, which may be important during ageing. For example, GH acutely regulates muscle mitochondrial function by increasing the transcript levels of several key mitochondrial proteins and shifting fuel utilisation toward increased fat oxidation (Short et al. 2008). Similarly, when recombinant IGF-I was administered exogenously to mice (for several weeks) there was an increase in muscle oxidative enzymes and increased fatigue resistance (Gregorevic et al. 2002, 2004; Schertzer et al. 2006).
Insulin and insulin-like growth factors
Skeletal muscle contains a population of heterotetrameric transmembrane receptors that bind insulin, IGF-I and/or IGF-II to regulate various stages of myogenesis, including proliferation, differentiation and fusion of muscle precursor cells (Florini et al. 1986; Allen and Boxhorn 1989). In addition to the mature IGF-I produced by the liver, skeletal muscle is an important source of this hormone. Studies have revealed at least two different kinds of IGF-I produced by skeletal muscle, which are derived from the IGF-I gene by alternative splicing (Goldspink and Yang 2004). One of the splice variants is expressed in response to physical activity and is called ‘mechano growth factor’ or MGF and the other is similar to the systemic or liver type (IGF-IEa) important for providing the mature IGF-I required to up-regulate protein synthesis (Musarò et al. 2001; Barton et al. 2002; Goldspink and Harridge 2004; Petrella et al. 2006).
In skeletal muscle IGF-I acts via binding to heterotetrameric transmembrane receptors that act as tyrosine protein kinases and subsequently activate complex intracellular signals, including (but not limited to) phosphoinositol 3-kinase (PI3Kinase)/Akt, extracellular signal-regulated kinase (ERK)/mitogen-activated protein kinase (MAPK) and protein kinase C (PKC) (Rommel et al. 2001; Czifra et al. 2006). Activation of one or more of these pathways has been linked to anabolic, anti-catabolic, chemotactic, and anti-apoptotic responses (Firth and Baxter 2002). Thus, disruption of this important signalling molecule could have serious implications for the regulation of skeletal muscle mass and force production (Janssen et al. 1998).
Associated with the age-related decline in GH is a decrease in the production of liver derived IGF-I (Benbassat et al. 1997), which has been linked to deleterious changes in predictive physical health parameters, such as body mass index (O’Connor et al. 1998). The age-related decline in GH and liver-derived IGF-I has been studied extensively and is reviewed elsewhere (Veldhuis et al. 1997).
Similar to liver-derived IGF-I, MGF levels are altered with age. However, to date, all work examining MGF levels with ageing have been conducted at the mRNA level, which can often be unreliable when predicting changes at the protein level. Owino et al. (2001) found that the increase in skeletal muscle mRNA levels of MGF after mechanical overload was significantly less in old compared with young rats. In another study, Hameed et al. (2003) found a similar increase in skeletal muscle MGF mRNA levels in young but not old men, after a single bout of resistance exercise. These findings indicate an age-related decrease in both systemic and locally derived IGF-I, which may be responsible, at least in part, for the age-related decline in skeletal muscle structure and function.
In addition to its direct actions on skeletal muscle, IGF-I enhances motor neuron survival and proteins involved in E–C coupling. Messi and Delbono (2003) using wildtype and S1S2 transgenic (IGF-I overexpressing) mice reported that IGF-I overexpression prevented the detrimental age-related changes in the nerve terminal and the NMJ. Zheng et al. (2002) and more recently Schertzer et al. (2007), demonstrated that IGF-I can regulate the transcription of the dihydropyridine receptor (DHPRα1S), a protein that plays a key role in the transformation of an action potential to the release of Ca2+ from the sarcoplasmic reticulum. These findings suggest that the age-related decline in E–C coupling may result from the reduced concentrations of both local and systemic IGF-I (Table 1).
The cellular actions of IGF-I are modulated through the actions of a family of six IGF binding proteins (IGFBP1-6), which also have a number of IGF-I independent actions (for review see Firth and Baxter 2002). While the predominant source of circulating IGFBPs is the liver, skeletal muscle myoblasts undergoing differentiation produce and release IGFBP-2, 3, 4 and 5 (Foulstone et al. 2003; Pampusch et al. 2003). While the precise role of these IGFBPs in the control of skeletal muscle growth and development has yet to be elucidated, the disruption of IGFBP expression has been found to impair myoblast proliferation, differentiation and maturation (Fligger et al. 1998; Foulstone et al. 2003; Pampusch et al. 2003, 2005).
Benbassat et al. (1997) examined the protein levels of circulating IGFBPs and reported a two-fold increase in IGFBP1 and an ∼15% decrease in IGFBP3, in old compared with young men (Table 1). Similarly, van den Beld et al. (2003) found an age-associated increase in the circulating protein levels of IGFBP1 and a decrease in IGFBP3. These authors also found an age-associated increase in the serum levels of IGFBP2. IGFBP1 is a 30 kDa protein produced predominantly by the liver and plays a role in the acute regulation of IGF-I bioavailablity. IGFBP2 appears to primarily inhibit the actions of IGF-I and IGF-II, while the majority of circulating IGF-I is bound in a ternary complex with IGFBP3 and an acid-labile subunit which limits the metabolic effects of large amounts of IGF-I (Firth and Baxter 2002).
While IGFBP4 and IGFBP5 have yet to be examined in human models of ageing, Spangenburg et al. (2003) examined mRNA and protein levels of IGFBP3, 4 and 5 in soleus muscles from young, adult and old rats. In that study, IGFBP4 mRNA was not altered with age (protein was not detectable); IGFBP3 protein levels were elevated in adult, but not old rats; and IGFBP5 protein levels were reduced by ∼50% compared with young and adult rats (Table 1). These findings indicate the need to measure IGFBP protein levels in both the systemic circulation, as well as the local (skeletal muscle) environment, and indicate that their expression is significantly altered by the ageing process. What effect this may have on skeletal muscle has yet to be elucidated fully.
Thyroid hormone
Thyroid hormones modulate transcription through binding nuclear receptors and are key regulators of many cellular processes, particularly those related to metabolism (Viguerie and Langin 2003). A number of changes in thyroid hormone concentrations have been described with ageing, including a decrease in thyroid-stimulating hormone (TSH) and triiodothyronine (T3). In contrast, thyroxine (T4) levels remain unchanged (for review see Mariotti et al. 1995). Hypothyroidism has been linked to muscular weakness and a shift in myosin heavy chain isoforms (from fast to intermediate isoforms, Salviati et al. 1985). Thus, it appears likely that the age-related decrease in thyroid function plays an important role in the sarcopenic phenotype. In addition to its actions on myosin heavy chain isoforms, thyroid hormone is known to regulate the transcription of other proteins involved in E–C coupling including the expression of the sarco/endoplasmic reticulum Ca2+ ATPase (SERCA1), since the SERCA1 gene promoter contains thyroid hormone response elements (van der Linden et al. 1992; Simonides et al. 1996).
Catecholamines and β-adrenoceptors
Catecholamines and the β-adrenoceptor signalling pathway have been implicated in skeletal muscle growth and regeneration (for review see Lynch and Ryall 2008). As β-adrenoceptors are endogenously stimulated by adrenaline and have been implicated in skeletal muscle regeneration (Beitzel et al. 2004, 2007), it is interesting to postulate a role for this pathway in conditions where muscle wasting and weakness are indicated.
While there has been much conjecture as to the exact changes in catecholamine levels as a consequence of ageing, it is now accepted that there is an increase in the plasma level of noradrenaline and a decrease in adrenaline, in both rats and humans (Esler et al. 1995; Larkin et al. 1996; Kaye and Esler 2005). In addition, work from our laboratory has demonstrated an age-related change in β-adrenoceptor signalling in skeletal muscle (Ryall et al. 2007). Chronic administration of the β-adrenoceptor agonist formoterol for 4 weeks increased the mass of the slow-twitch soleus muscle in young (3 months), but not adult (16 months) or old (27 months) rats. In contrast, formoterol increased the mass of the fast-twitch extensor digitorum longus muscle in rats of all three age groups tested (Ryall et al. 2007). These findings suggest that the β-adrenergic signaling pathway and especially stimulation of that pathway leading to striated muscle hypertrophy, is altered by age in slow- but not in fast-twitch skeletal muscles, an effect independent of β-adrenoceptor density.
Cytokines and inflammatory pathways
The ageing process in skeletal muscle is associated with an increased rate of protein degradation (Yarasheski 2003). Irreparably damaged skeletal muscle will undergo autolysis with cellular debris removed to allow for the growth and replacement of lost myofibres. Skeletal muscle autolysis is predominantly dependent on Ca2+-activated processes, such that if the magnitude of the injury results in an increase in intracellular [Ca2+] that cannot be buffered adequately, muscle fibre autolysis will ensue (Gissel 2005). The subsequent highly synchronised inflammatory response is critical for efficient muscle regeneration. A number of studies have suggested a link between aberrant inflammatory/cytokine signalling and sarcopenia (Visser et al. 2002; Hamada et al. 2005; Przybyla et al. 2006; Thompson et al. 2006). Tumor necrosis factor alpha (TNFα) and interleukin-6 (IL-6) have been implicated in the inflammatory response in skeletal muscle and an age-related increase in the expression of these inflammatory markers is thought to contribute to the sarcopenic phenotype (see Roubenoff 2003 for review).
Elevated TNFα levels in aged muscle has been postulated to increase apoptosis and impair the inflammatory response to injury (Dirks and Leeuwenburgh 2006). TNFα activates nuclear factor kappa B (NFκB), resulting in the expression of genes involved in pro-inflammatory responses and cell survival (Dirks and Leeuwenburgh 2006). However, apoptosis (after chronic exposure to high levels of TNFα), can be induced in skeletal muscle via the cleavage and subsequent activation of procaspase 8 (Stewart et al. 2004).
IL-6 is a recently identified myokine that is increased in the skeletal muscles of aged humans (Roubenoff et al. 1998; Visser et al. 2002). When expressed at low levels IL-6 can act as a skeletal muscle growth factor, but at higher levels it can initiate muscle wasting (Tsujinaka et al. 1996). Serrano et al. (2008) used IL-6 deficient mice to demonstrate a clear role for IL-6 in satellite cell proliferation, and in the regulation of skeletal muscle growth.
IL-6 also plays a role in metabolic signalling following exercise, via phosphorylation of the fuel-sensing enzyme AMP activated protein kinase (AMPK) (Kelly et al. 2004). While resting levels of systemic IL-6 increase with ageing in humans (Roubenoff et al. 1998; Visser et al. 2002), local skeletal muscle IL-6 levels at rest appear similar between young and old subjects (Pedersen et al. 2004). Immunohistochemical detection of IL-6 in skeletal muscles of healthy young humans revealed higher expression in type I than type II muscle fibres (Plomgaard et al. 2005). Whether this fibre specificity (in IL-6 levels) is affected by age has not been determined. Results are equivocal as to whether there is a difference in the local increase of IL-6 in skeletal muscle in response to injury and/or exercise (Pedersen et al. 2004; Hamada et al. 2005; Sacheck et al. 2006).
It is interesting to note that the muscle atrophy observed in mice overexpressing systemic IL-6 can be reversed completely after treatment with an IL-6 neutralising antibody (Tsujinaka et al. 1996). To date, no study has examined the potential of IL-6 inhibition to prevent or reverse sarcopenia but this might also not be helpful since recent evidence suggests that IL-6, especially that released by contracting muscles during exercise, may facilitate an anti-inflammatory milieu that inhibits the pro-inflammatory actions of TNF-α (Pedersen and Fischer 2007).
Intrinsic changes to skeletal muscle with old age
While the underlying causes of sarcopenia have yet to be elucidated completely, one potential mechanism involves the age-related decline in muscle regenerative capacity, possibly as a consequence of a decreased number and/or function of quiescent skeletal muscle precursor cells (satellite cells) (Conboy et al. 2003, 2005; Kadi et al. 2004) (Fig. 2b). Satellite cells represent the endogenous source of muscle precursor cells which undergo activation, proliferation and differentiation to form ‘new’ muscle fibres, a process regulated by the myogenic regulatory factors (MRFs) (for review see Chargé and Rudnicki 2004). The myogenic basic helix-loop-helix (bHLH) proteins; myogenic determination factor (MyoD), myogenin, myogenic factor 5 (myf-5) and myogenic regulatory factor 4 (MRF4) are members of the MRF family of transcription factors, and have been implicated in the process of muscle growth and development (for review see Buckingham 2006). Myf5 and MyoD, in addition to the paired-box transcription factor Pax7, have been implicated in the process of satellite cell specification, while myogenin appears important for differentiation and MRF4 in maturation (Chargé and Rudnicki 2004).
Numerous studies have demonstrated an age-associated decrease in satellite cell number in rodents (Snow 1977; Brack et al. 2005) and humans (Renault et al. 2002; Kadi et al. 2004). Verdijk et al. (2007) reported that the mean number of satellite cells decreased in type II, but not type I fibres of the vastus lateralis muscle of healthy elderly men which may help to explain the differential response of fast type II fibres compared with slow type I fibres with ageing (Larsson et al. 1978; Lexell 1997; Luff 1998; Dedkov et al. 2003a). However, it should be noted that the notion of changes in satellite cell number with ageing is controversial since many studies in humans have reported either no change, or even a slight increase in satellite cell number with age (Roth et al. 2000; Dreyer et al. 2006). If an age-related decline in satellite cell number does occur, or if their ability to activate, proliferate and differentiate is reduced, this would likely impair skeletal muscle structure and function, particularly in response to injury.
MRF co-regulators
A number of studies in rats have reported that expression of MyoD and myogenin mRNA (and protein) are increased in old age (Musarò et al. 1995; Kostrominova et al. 2000; Alway et al. 2002a; Dedkov et al. 2003b). While these results could indicate a compensatory mechanism for the age-related decline in skeletal muscle mass, studies examining the MRF response to muscle functional overload have found that the increase in MRF expression in muscles from young rats is not observed in old rats (Alway et al. 2002a; Gallegly et al. 2004). A similar response has been observed in humans, with impaired differentiation of myoblasts in the elderly (Bigot et al. 2008), which was attributed to reduced and delayed expression of MyoD, Myf5 and myogenin. Thus, it appears that the impaired plasticity or adaptability of aged skeletal muscle is associated with aberrations in the transcriptional hierarchy required for myogenesis, possibly due to changes in the expression of MRF co-regulators.
A family of related HLH proteins, inhibitors of DNA binding (Id), bind to and negatively regulate the function of numerous bHLH proteins, including MRF proteins (Zebedee and Hara 2001). Alway et al. (2002a, b) reported an increased expression of Id-1, Id-2 and Id-3 in skeletal muscles of aged compared with young rats. These results indicated that while aging was associated with an increase in the basal level of MRF proteins, a concomitant increase in the expression of proteins that negatively repress MRF activity was also observed; a possible explanation for the impaired or delayed response of MRF proteins to injury.
Notch signalling pathway
The expression of the MRF family of transcription factors is regulated carefully by a number of morphogenic signalling pathways, including the evolutionarily conserved Notch pathway (Conboy and Rando 2002). Notch signalling is initiated through the binding of either Delta or Jagged ligands (or Serrate in invertebrates) to one of the Notch family of transmembrane receptors. Ligand binding to Notch initiates cleavage of the receptor and release of the active Notch intracellular domain (NICD), which in turn translocates to the nucleus where it binds members of the Cp-binding factor (CBF1, also known as recombination signal sequence-binding protein-J, RBP-J), Suppressor of Hairless (Su(H)), and Lag-1 family of transcriptional repressors (together forming the CSL family of regulators), converting them to transcriptional activators to ultimately increase satellite cell proliferation (Luo et al. 2005).
The first study to examine a link between the age-related impairment in satellite cell proliferation and Notch signalling was conducted by Conboy et al. (2003). The expression of the Notch ligand Delta and an endogenous inhibitor of Notch, termed Numb, were measured in satellite cells from regenerating skeletal muscles in young, adult and old rats. Satellite cells from regenerating old muscles exhibited a decreased expression of Delta and increased expression of Numb, likely resulting in reduced activation of Notch and ultimately, impaired proliferation (Conboy et al. 2003). Administration of a Jagged fusion protein (Jagged-FC) to inhibit Notch signalling in regenerating skeletal muscles of young and old rats, decreased satellite cell proliferation and impaired muscle regeneration.
In another study, Conboy et al. (2005) utilized parabiotic pairings of young and old mice to examine the role of the systemic environment on satellite cell proliferation. Exposure of old muscles to a young systemic environment resulted in a significant increase in proliferation of the resident satellite cell pool. Increased satellite cell proliferation was associated with an increase in the activation of the Notch signalling pathway, reinforcing the importance of systemic environment in age-related muscle wasting (Conboy et al. 2005).
In a follow up study, Brack et al. (2007) demonstrated that exposure of aged muscle to a youthful systemic environment not only enhanced regeneration but reduced fibrosis, an effect associated with increased proliferation of muscle progenitor cells. The age-related increase in fibrotic tissue was attributed to an increased conversion of myogenic cells into non-myogenic cells, possibly mediated through increased activation of the Wnt signalling pathway (Brack et al. 2007).
Myostatin
In a now seminal study, McPherron et al. (1997) identified a novel member of the transforming growth factor β (TGF-β) superfamily that was a potent inhibitor of muscle growth and development. Originally termed growth and differentiating factor 8 (GDF-8), but later renamed myostatin, this factor inhibits satellite cell proliferation and differentiation (Langley et al. 2002; McCroskery et al. 2003).
Myostatin is believed to mediate its actions on skeletal muscle via the activin type II receptors (ActRIIA and ActRIIB) and subsequent phosphorylation of Smad proteins (Fig. 2b), which appear to be key regulators of myostatin signalling (for review see Lee 2004). Myostatin inhibits satellite cell proliferation through up-regulation of p21, and decreases in the levels of cyclin-dependent kinase 2 (Cdk2) and phosphorylated retinoblastoma protein (Rb, Langley et al. 2002). In contrast, myostatin-mediated inhibition of myoblast differentiation is believed to occur due to downregulation of specific muscle regulatory factors including MyoD and myogenin (Langley et al. 2002).
While much work has focussed on the potential therapeutic benefits of myostatin inhibition in animal models of muscle wasting and weakness, it is only recently that studies have examined a role for this protein in sarcopenia. Kawada et al. (2001) examined the myostatin protein content in male mice from 5 to 92 weeks of age, and found that myostatin protein levels remained constant in gastrocnemius and soleus muscles after 11 weeks of age. In contrast, Baumann and colleagues (2003) found an increase in the amount of myostatin protein in the gastrocnemius muscle as rats aged from 1.5 to 27 months. These different findings suggested that myostatin regulation with age varied between species. In more recent studies using myostatin-null mice, a lack of myostatin attenuated age-related muscle wasting and enhanced muscle fibre regenerative capacity, indicating that antagonism of myostatin had therapeutic potential for sarcopenia (McCroskery et al. 2005; Wagner et al. 2005; Siriett et al. 2006, 2007).
While a wealth of data exists on the function of myostatin in animal models of muscle wasting (Kawada et al. 2001; Baumann et al. 2003; Siriett et al. 2007), our understanding of this important protein in human conditions of muscle wasting is still incomplete. Welle et al. (2002) examined myostatin mRNA expression in the vastus lateralis muscle of young (21–31-year-old) and old (62–77-year-old) men, and found no change in myostatin expression. In contrast Raue et al. (2006) found a 56% increase in myostatin mRNA expression in the vastus lateralis muscles of old (80–89-year-old) compared to young (18–30-year-old) women. These results indicate a potential sexual dimorphism in the role of myostatin in sarcopenia, however, further investigation of myostatin in ageing is warranted, particularly in relation to myostatin protein levels.
Intracellular calcium
One mechanism implicated in the ageing of skeletal muscle is that of age-related alterations in Ca2+ homeostasis. In addition to its role in force production, Ca2+ plays an important role as a second messenger. While a detailed description of Ca2+-mediated signalling in skeletal muscle is beyond the scope of this review, the reader is referred to a number of excellent reviews (Berchtold et al. 2000; Berridge et al. 2003). Important for the current discussion is the finding that resting intracellular [Ca2+] has been found to increase in skeletal muscle fibres with advancing age (Fulle et al. 2005; Fraysse et al. 2006).
Dargelos et al. (2007) examined the protein levels and activity of calpain (calcium-dependent cystein proteases) and calpastatin (a specific endogenous inhibitor of calpain) in skeletal muscles from young and old rats. Ageing was associated with an overall increase in calpain and a concomitant decrease in calpastatin protein and activity levels, indicating an overall age-related increase in calcium-dependent proteolysis.
Conclusions
As the proportion of older persons in the world’s population continues to increase, sarcopenia will dramatically impact many lives and place ever-increasing demands on health care systems. To address these issues, therapeutic strategies are needed to ameliorate the effects of ageing on skeletal muscle structure and function. While the exact cellular and molecular mechanisms for the age-related loss of protein have yet to be elucidated fully, they are likely highly complex and involve multiple cell signalling pathways. This review has highlighted some of the important age-related changes to the systemic environment (testosterone, GH/IGF-I axis, thyroid hormones, catecholamines and cytokines) and those changes intrinsic to skeletal muscle (MRFs, notch, myostatin and calcium). Considerable research efforts are needed to better understand the mechanisms underlying sarcopenia and to help identify novel treatments.
References
Allen RE, Boxhorn LK (1989) Regulation of skeletal muscle satellite cell proliferation and differentiation by transforming growth factor-beta, insulin-like growth factor I, and fibroblast growth factor. J Cell Physiol 138:311–315
Altuwaijri S, Lee DK, Chuang KH, Ting HJ, Yang Z, Xu Q, Tsai MY, Yeh S, Hanchett LA, Chang HC, Chang C (2004) Androgen receptor regulates expression of skeletal muscle-specific proteins and muscle cell types. Endocrine 25:27–32
Alway SE, Degens H, Krishnamurthy G, Smith CA (2002a) Potential role for Id myogenic repressors in apoptosis and attenuation of hypertrophy in muscles of aged rats. Am J Physiol Cell Physiol 283:C66–C76
Alway SE, Degens H, Lowe DA, Krishnamurthy G (2002b) Increased myogenic repressor Id mRNA and protein levels in hindlimb muscles of aged rats. Am J Physiol Regul Integr Comp Physiol 282:R411–R422
Amin S, Riggs BL, Atkinson EJ, Oberg AL, Melton LJ 3rd, Khosla S (2004) A potentially deleterious role of IGFBP-2 on bone density in aging men and women. J Bone Miner Res 19:1075–1083
Barton ER, Morris L, Musaro A, Rosenthal N, Sweeney HL (2002) Muscle-specific expression of insulin-like growth factor I counters muscle decline in mdx mice. J Cell Biol 157:137–148
Baumann AP, Ibebunjo C, Grasser WA, Paralkar VM (2003) Myostatin expression in age and denervation-induced skeletal muscle atrophy. J Musculoskelet Neuronal Interact 3:8–16
Beitzel F, Gregorevic P, Ryall JG, Plant DR, Sillence MN, Lynch GS (2004) β2-adrenoceptor agonist fenoterol enhances functional repair of regenerating rat skeletal muscle after injury. J Appl Physiol 96:1385–1392
Beitzel F, Sillence MN, Lynch GS (2007) β-Adrenoceptor signaling in regenerating skeletal muscle after β-agonist administration. Am J Physiol Endocrinol Metab 293:E932–E940
Benbassat CA, Maki KC, Unterman TG (1997) Circulating levels of insulin-like growth factor (IGF) binding protein-1 and -3 in aging men: relationships to insulin, glucose, IGF, and dehydroepiandrosterone sulfate levels and anthropometric measures. J Clin Endocrinol Metab 82:1484–1491
Berchtold MW, Brinkmeier H, Muntener M (2000) Calcium ion in skeletal muscle: its crucial role for muscle function, plasticity, and disease. Physiol Rev 80:1215–1265
Berridge MJ, Bootman MD, Roderick HL (2003) Calcium signalling: dynamics, homeostasis and remodelling. Nat Rev Mol Cell Biol 4:517–529
Bigot A, Jacquemin V, Debacq-Chainiaux F, Butler-Browne GS, Toussaint O, Furling D, Mouly V (2008) Replicative aging down regulates the myogenic regulatory factors in human myoblasts. Biol Cell 100:189–199
Brack AS, Bildsoe H, Hughes SM (2005) Evidence that satellite cell decrement contributes to preferential decline in nuclear number from large fibres during murine age-related muscle atrophy. J Cell Sci 118:4813–4821
Brack AS, Conboy MJ, Roy S, Lee M, Kuo CJ, Keller C, Rando TA (2007) Increased Wnt signaling during aging alters muscle stem cell fate and increases fibrosis. Science 317:807–810
Brooks SV, Faulkner JA (1994) Skeletal muscle weakness in old age: underlying mechanisms. Med Sci Sports Exerc 26:432–439
Buckingham M (2006) Myogenic progenitor cells and skeletal myogenesis in vertebrates. Curr Opin Genet Dev 16:525–532
Carlson BM, Faulkner JA (1989) Muscle transplantation between young and old rats: age of host determines recovery. Am J Physiol 256:C1262–C1266
Carlson BM, Faulkner JA (1996) The regeneration of noninnervated muscle grafts and marcaine-treated muscles in young and old rats. J Gerontol A Biol Sci Med Sci 51:B43–B49
Cederna PS, Asato H, Gu X, van der Meulen J, Kuzon WM Jr, Carlson BM, Faulkner JA (2001) Motor unit properties of nerve-intact extensor digitorum longus muscle grafts in young and old rats. J Gerontol A Biol Sci Med Sci 56:B254–B258
Chahal HS, Drake WM (2007) The endocrine system and ageing. J Pathol 211:173–180
Chargé SB, Rudnicki MA (2004) Cellular and molecular regulation of muscle regeneration. Physiol Rev 84:209–238
Chen Y, Zajac JD, MacLean HE (2005) Androgen regulation of satellite cell function. J Endocrinol 186:21–31
Chia DJ, Ono M, Woelfle J, Schlesinger-Massart M, Jiang H, Rotwein P (2006) Characterization of distinct Stat5b binding sites that mediate growth hormone-stimulated IGF-I gene transcription. J Biol Chem 281:3190–3197
Cohen TJ, Waddell DS, Barrientos T, Lu Z, Feng G, Cox GA, Bodine SC, Yao TP (2007) The histone deacetylase HDAC4 connects neural activity to muscle transcriptional reprogramming. J Biol Chem 282:33752–33759
Conboy IM, Rando TA (2002) The regulation of Notch signaling controls satellite cell activation and cell fate determination in postnatal myogenesis. Dev Cell 3:397–409
Conboy IM, Conboy MJ, Smythe GM, Rando TA (2003) Notch-mediated restoration of regenerative potential to aged muscle. Science 302:1575–1577
Conboy IM, Conboy MJ, Wagers AJ, Girma ER, Weissman IL, Rando TA (2005) Rejuvenation of aged progenitor cells by exposure to a young systemic environment. Nature 433:760–764
Conley KE, Cress ME, Jubrias SA, Esselman PC, Odderson IR (1995) From muscle properties to human performance, using magnetic resonance. J Gerontol A Biol Sci Med Sci 50(Spec No):35–40
Cree MG, Newcomer BR, Katsanos CS, Sheffield-Moore M, Chinkes D, Aarsland A, Urban R, Wolfe RR (2004) Intramuscular and liver triglycerides are increased in the elderly. J Clin Endocrinol Metab 89:3864–3871
Czifra G, Toth IB, Marincsak R, Juhasz I, Kovacs I, Acs P, Kovacs L, Blumberg PM, Biro T (2006) Insulin-like growth factor-I-coupled mitogenic signaling in primary cultured human skeletal muscle cells and in C2C12 myoblasts. A central role of protein kinase Cδ. Cell Signal 18:1461–1472
Dargelos E, Brule C, Combaret L, Hadj-Sassi A, Dulong S, Poussard S, Cottin P (2007) Involvement of the calcium-dependent proteolytic system in skeletal muscle aging. Exp Gerontol 42:1088–1098
Dedkov EI, Borisov AB, Carlson BM (2003a) Dynamics of postdenervation atrophy of young and old skeletal muscles: differential responses of fiber types and muscle types. J Gerontol A Biol Sci Med Sci 58:984–991
Dedkov EI, Kostrominova TY, Borisov AB, Carlson BM (2003b) MyoD and myogenin protein expression in skeletal muscles of senile rats. Cell Tissue Res 311:401–416
Dela F, Kjaer M (2006) Resistance training, insulin sensitivity and muscle function in the elderly. Essays Biochem 42:75–88
Delbono O (2003) Neural control of aging skeletal muscle. Aging Cell 2:21–29
Dirks AJ, Leeuwenburgh C (2006) Tumor necrosis factor alpha signaling in skeletal muscle: effects of age and caloric restriction. J Nutr Biochem 17:501–508
Dreyer HC, Blanco CE, Sattler FR, Schroeder ET, Wiswell RA (2006) Satellite cell numbers in young and older men 24 hours after eccentric exercise. Muscle Nerve 33:242–253
Edström L, Larsson L (1987) Effects of age on contractile and enzyme-histochemical properties of fast- and slow-twitch single motor units in the rat. J Physiol 392:129–145
Edstrom E, Altun M, Bergman E, Johnson H, Kullberg S, Ramirez-Leon V, Ulfhake B (2007) Factors contributing to neuromuscular impairment and sarcopenia during aging. Physiol Behav 92:129–135
Einsiedel LJ, Luff AR (1992) Alterations in the contractile properties of motor units within the ageing rat medial gastrocnemius. J Neurol Sci 112:170–177
Esler M, Kaye D, Thompson J, Jennings G, Cox H, Turner A, Lambert G, Seals D (1995) Effects of aging on epinephrine secretion and regional release of epinephrine from the human heart. J Clin Endocrinol Metab 80:435–442
Faulkner JA, Larkin LM, Claflin DR, Brooks SV (2007) Age-related changes in the structure and function of skeletal muscles. Clin Exp Pharmacol Physiol 34:1091–1096
Firth SM, Baxter RC (2002) Cellular actions of the insulin-like growth factor binding proteins. Endocr Rev 23:824–854
Fligger JM, Malven PV, Doumit ME, Merkel RA, Grant AL (1998) Increases in insulin-like growth factor binding protein-2 accompany decreases in proliferation and differentiation when porcine muscle satellite cells undergo multiple passages. J Anim Sci 76:2086–2093
Florini JR, Ewton DZ, Falen SL, Van Wyk JJ (1986) Biphasic concentration dependency of stimulation of myoblast differentiation by somatomedins. Am J Physiol 250:C771–C778
Foulstone EJ, Savage PB, Crown AL, Holly JM, Stewart CE (2003) Role of insulin-like growth factor binding protein-3 (IGFBP-3) in the differentiation of primary human adult skeletal myoblasts. J Cell Physiol 195:70–79
Fraysse B, Desaphy JF, Rolland JF, Pierno S, Liantonio A, Giannuzzi V, Camerino C, Didonna MP, Cocchi D, De Luca A, Conte Camerino D (2006) Fiber type-related changes in rat skeletal muscle calcium homeostasis during aging and restoration by growth hormone. Neurobiol Dis 21:372–380
Fulle S, Di Donna S, Puglielli C, Pietrangelo T, Beccafico S, Bellomo R, Protasi F, Fano G (2005) Age-dependent imbalance of the antioxidative system in human satellite cells. Exp Gerontol 40:189–197
Gallegly JC, Turesky NA, Strotman BA, Gurley CM, Peterson CA, Dupont-Versteegden EE (2004) Satellite cell regulation of muscle mass is altered at old age. J Appl Physiol 97:1082–1090
Giresi PG, Stevenson EJ, Theilhaber J, Koncarevic A, Parkington J, Fielding RA, Kandarian SC (2005) Identification of a molecular signature of sarcopenia. Physiol Genomics 21:253–263
Gissel H (2005) The role of Ca2+ in muscle cell damage. Ann NY Acad Sci 1066:166–180
Giustina A, Veldhuis JD (1998) Pathophysiology of the neuroregulation of growth hormone secretion in experimental animals and the human. Endocr Rev 19:717–797
Goldspink G, Harridge SD (2004) Growth factors and muscle ageing. Exp Gerontol 39:1433–1438
Goldspink G, Yang SY (2004) The splicing of the IGF-I gene to yield different muscle growth factors. Adv Genet 52:23–49
Gregorevic P, Plant DR, Leeding KS, Bach LA, Lynch GS (2002) Improved contractile function of the mdx dystrophic mouse diaphragm muscle after insulin-like growth factor-I administration. Am J Pathol 161:2263–2272
Gregorevic P, Plant DR, Lynch GS (2004) Administration of insulin-like growth factor-I improves fatigue resistance of skeletal muscles from dystrophic mdx mice. Muscle Nerve 30:295–304
Hagen JL, Krause DJ, Baker DJ, Fu MH, Tarnopolsky MA, Hepple RT (2004) Skeletal muscle aging in F344BN F1-hybrid rats: I. Mitochondrial dysfunction contributes to the age-associated reduction in VO2max. J Gerontol A Biol Sci Med Sci. 59:1099–1110
Hamada K, Vannier E, Sacheck JM, Witsell AL, Roubenoff R (2005) Senescence of human skeletal muscle impairs the local inflammatory cytokine response to acute eccentric exercise. Faseb J 19:264–266
Hameed M, Orrell RW, Cobbold M, Goldspink G, Harridge SD (2003) Expression of IGF-I splice variants in young and old human skeletal muscle after high resistance exercise. J Physiol 547:247–254
Herbert J (1995) The age of dehydroepiandrosterone. Lancet 345:1193–1194
Herbst KL, Bhasin S (2004) Testosterone action on skeletal muscle. Curr Opin Clin Nutr Metab Care 7:271–277
Hepple RT, Baker DJ, McConkey M, Murynka T, Norris R (2006) Caloric restriction protects mitochondrial function with aging in skeletal and cardiac muscles. Rejuvenation Res 9:219–222
Hermann M, Berger P (2001) Hormonal changes in aging men: a therapeutic indication? Exp Gerontol 36:1075–1082
Iannuzzi-Sucich M, Prestwood KM, Kenny AM (2002) Prevalence of sarcopenia and predictors of skeletal muscle mass in healthy, older men and women. J Gerontol A Biol Sci Med Sci 57:M772–M777
Isgaard J, Carlsson L, Isaksson OG, Jansson JO (1988) Pulsatile intravenous growth hormone (GH) infusion to hypophysectomized rats increases insulin-like growth factor I messenger ribonucleic acid in skeletal tissues more effectively than continuous GH infusion. Endocrinology 123:2605–2610
Janssen JA, Stolk RP, Pols HA, Grobbee DE, Lamberts SW (1998) Serum free and total insulin-like growth factor-I, insulin-like growth factor binding protein-1 and insulin-like growth factor binding protein-3 Levels in healthy elderly individuals. Relation to self-reported quality of health and disability. Gerontology 44:277–280
Kadi F, Charifi N, Denis C, Lexell J (2004) Satellite cells and myonuclei in young and elderly women and men. Muscle Nerve 29:120–127
Kawada S, Tachi C, Ishii N (2001) Content and localization of myostatin in mouse skeletal muscles during aging, mechanical unloading and reloading. J Muscle Res Cell Motil 22:627–633
Kaye D, Esler M (2005) Sympathetic neuronal regulation of the heart in aging and heart failure. Cardiovasc Res 66:256–264
Kelly M, Keller C, Avilucea PR, Keller P, Luo Z, Xiang X, Giralt M, Hidalgo J, Saha AK, Pedersen BK, Ruderman NB (2004) AMPK activity is diminished in tissues of IL-6 knockout mice: the effect of exercise. Biochem Biophys Res Commun 320:449–454
Khosla S, Melton LJ 3rd, Atkinson EJ, O’Fallon WM, Klee GG, Riggs BL (1998) Relationship of serum sex steroid levels and bone turnover markers with bone mineral density in men and women: a key role for bioavailable estrogen. J Clin Endocrinol Metab 83:2266–2274
Kostrominova TY, Macpherson PC, Carlson BM, Goldman D (2000) Regulation of myogenin protein expression in denervated muscles from young and old rats. Am J Physiol Regul Integr Comp Physiol 279:R179–R188
Langley B, Thomas M, Bishop A, Sharma M, Gilmour S, Kambadur R (2002) Myostatin inhibits myoblast differentiation by down-regulating MyoD expression. J Biol Chem 277:49831–49840
Lanning NJ, Carter-Su C (2006) Recent advances in growth hormone signaling. Rev Endocr Metab Disord 7:225–235
Larkin LM, Halter JB, Supiano MA (1996) Effect of aging on rat skeletal muscle β-AR function in male Fischer 344 x brown Norway rats. Am J Physiol 270:R462–R468
Larsson L, Sjödin B, Karlsson J (1978) Histochemical and biochemical changes in human skeletal muscle with age in sedentary males, age 22–65 years. Acta Physiol Scand 103:31–39
Larsson L, Grimby G, Karlsson J (1979) Muscle strength and speed of movement in relation to age and muscle morphology. J Appl Physiol 46:451–456
Lee SJ (2004) Regulation of muscle mass by myostatin. Annu Rev Cell Dev Biol 20:61–86
Lexell J (1997) Evidence for nervous system degeneration with advancing age. J Nutr 127:1011S–1013S
Luff AR (1998) Age-associated changes in the innervation of muscle fibers and changes in the mechanical properties of motor units. Ann NY Acad Sci 854:92–101
Luo D, Renault VM, Rando TA (2005) The regulation of Notch signaling in muscle stem cell activation and postnatal myogenesis. Semin Cell Dev Biol 16:612–622
Lynch GS (2004a) Tackling Australia’s future health problems: developing strategies to combat sarcopenia–age-related muscle wasting and weakness. Intern Med J 34:294–296
Lynch GS (2004b) Emerging drugs for sarcopenia: age-related muscle wasting. Expert Opin Emerg Drugs 9:345–361
Lynch GS, Ryall JG (2008) Role of β-adrenoceptor signaling in skeletal muscle—implications for muscle wasting and disease. Physiol Rev. doi:10.1152/physrev.00028.2007
Marcell TJ, Harman SM, Urban RJ, Metz DD, Rodgers BD, Blackman MR (2001) Comparison of GH, IGF-I, and testosterone with mRNA of receptors and myostatin in skeletal muscle in older men. Am J Physiol Endocrinol Metab 281:E1159–E1164
Mariotti S, Franceschi C, Cossarizza A, Pinchera A (1995) The aging thyroid. Endocr Rev 16:686–715
McCroskery S, Thomas M, Maxwell L, Sharma M, Kambadur R (2003) Myostatin negatively regulates satellite cell activation and self-renewal. J Cell Biol 162:1135–1147
McCroskery S, Thomas M, Platt L, Hennebry A, Nishimura T, McLeay L, Sharma M, Kambadur R (2005) Improved muscle healing through enhanced regeneration and reduced fibrosis in myostatin-null mice. J Cell Sci 118:3531–3541
McNeil CJ, Doherty TJ, Stashuk DW, Rice CL (2005) Motor unit number estimates in the tibialis anterior muscle of young, old, and very old men. Muscle Nerve 31:461–467
McPherron AC, Lawler AM, Lee SJ (1997) Regulation of skeletal muscle mass in mice by a new TGF-β superfamily member. Nature 387:83–90
Messi ML, Delbono O (2003) Target-derived trophic effect on skeletal muscle innervation in senescent mice. J Neurosci 23:1351–1359
Morley JE, Kaiser F, Raum WJ, Perry HM 3rd, Flood JF, Jensen J, Silver AJ, Roberts E (1997) Potentially predictive and manipulable blood serum correlates of aging in the healthy human male: progressive decreases in bioavailable testosterone, dehydroepiandrosterone sulfate, and the ratio of insulin-like growth factor 1 to growth hormone. Proc Natl Acad Sci U S A 94:7537–7542
Musarò A, Cusella De Angelis MG, Germani A, Ciccarelli C, Molinaro M, Zani BM (1995) Enhanced expression of myogenic regulatory genes in aging skeletal muscle. Exp Cell Res 221:241–248
Musarò A, McCullagh K, Paul A, Houghton L, Dobrowolny G, Molinaro M, Barton ER, Sweeney HL, Rosenthal N (2001) Localized IGF-1 transgene expression sustains hypertrophy and regeneration in senescent skeletal muscle. Nat Genet 27:195–200
Nagley P, Mackay IR, Baumer A, Maxwell RJ, Vaillant F, Wang ZX, Zhang C, Linnane AW (1992) Mitochondrial DNA mutation associated with aging and degenerative disease. Ann NY Acad Sci 673:92–102
Nair KS, Rizza RA, O’Brien P, Dhatariya K, Short KR, Nehra A, Vittone JL, Klee GG, Basu A, Basu R, Cobelli C, Toffolo G, Dalla Man C, Tindall DJ, Melton LJ 3rd, Smith GE, Khosla S, Jensen MD (2006) DHEA in elderly women and DHEA or testosterone in elderly men. N Engl J Med 355:1647–1659
Narayanan N, Jones DL, Xu A, Yu JC (1996) Effects of aging on sarcoplasmic reticulum function and contraction duration in skeletal muscles of the rat. Am J Physiol 271:C1032–C1040
O’Connor KG, Tobin JD, Harman SM, Plato CC, Roy TA, Sherman SS, Blackman MR (1998) Serum levels of insulin-like growth factor-I are related to age and not to body composition in healthy women and men. J Gerontol A Biol Sci Med Sci 53:M176–M182
Owino V, Yang SY, Goldspink G (2001) Age-related loss of skeletal muscle function and the inability to express the autocrine form of insulin-like growth factor-1 (MGF) in response to mechanical overload. FEBS Lett 505:259–263
Pampusch MS, Kamanga-Sollo E, White ME, Hathaway MR, Dayton WR (2003) Effect of recombinant porcine IGF-binding protein-3 on proliferation of embryonic porcine myogenic cell cultures in the presence and absence of IGF-I. J Endocrinol 176:227–235
Pampusch MS, Xi G, Kamanga-Sollo E, Loseth KJ, Hathaway MR, Dayton WR, White ME (2005) Production of recombinant porcine IGF-binding protein-5 and its effect on proliferation of porcine embryonic myoblast cultures in the presence and absence of IGF-I and Long-R3-IGF-I. J Endocrinol 185:197–206
Pedersen BK, Fischer CP (2007) Physiological roles of muscle-derived interleukin-6 in response to exercise. Curr Opin Clin Nutr Metab Care 10:265–271
Pedersen M, Steensberg A, Keller C, Osada T, Zacho M, Saltin B, Febbraio MA, Pedersen BK (2004) Does the aging skeletal muscle maintain its endocrine function? Exerc Immunol Rev 10:42–55
Petrella JK, Kim JS, Cross JM, Kosek DJ, Bamman MM (2006) Efficacy of myonuclear addition may explain differential myofiber growth among resistance-trained young and older men and women. Am J Physiol Endocrinol Metab 291:E937–E946
Plant DR, Lynch GS (2002) Excitation–contraction coupling and sarcoplasmic reticulum function in mechanically skinned fibres from fast skeletal muscles of aged mice. J Physiol 543:169–176
Plomgaard P, Penkowa M, Pedersen BK (2005) Fiber type specific expression of TNF-alpha, IL-6 and IL-18 in human skeletal muscles. Exerc Immunol Rev 11:53–63
Prakash YS, Sieck GC (1998) Age-related remodeling of neuromuscular junctions on type-identified diaphragm fibers. Muscle Nerve 21:887–895
Przybyla B, Gurley C, Harvey JF, Bearden E, Kortebein P, Evans WJ, Sullivan DH, Peterson CA, Dennis RA (2006) Aging alters macrophage properties in human skeletal muscle both at rest and in response to acute resistance exercise. Exp Gerontol 41:320–327
Raue U, Slivka D, Jemiolo B, Hollon C, Trappe S (2006) Myogenic gene expression at rest and after a bout of resistance exercise in young (18–30 yr) and old (80–89 yr) women. J Appl Physiol 101:53–59
Renault V, Thornell LE, Eriksson PO, Butler-Browne G, Mouly V (2002) Regenerative potential of human skeletal muscle during aging. Aging Cell 1:132–139
Rommel C, Bodine SC, Clarke BA, Rossman R, Nunez L, Stitt TN, Yancopoulos GD, Glass DJ (2001) Mediation of IGF-1-induced skeletal myotube hypertrophy by PI(3)K/Akt/mTOR and PI(3)K/Akt/GSK3 pathways. Nat Cell Biol 3:1009–1013
Rosenheimer JL, Smith DO (1985) Differential changes in the end-plate architecture of functionally diverse muscles during aging. J Neurophysiol 53:1567–1581
Roth SM, Martel GF, Ivey FM, Lemmer JT, Metter EJ, Hurley BF, Rogers MA (2000) Skeletal muscle satellite cell populations in healthy young and older men and women. Anat Rec 260:351–358
Roubenoff R (2003) Catabolism of aging: is it an inflammatory process? Curr Opin Clin Nutr Metab Care 6:295–299
Roubenoff R, Harris TB, Abad LW, Wilson PW, Dallal GE, Dinarello CA (1998) Monocyte cytokine production in an elderly population: effect of age and inflammation. J Gerontol A Biol Sci Med Sci 53:M20–M26
Ryall JG, Schertzer JD, Lynch GS (2007) Attenuation of age-related muscle wasting and weakness in rats after formoterol treatment: therapeutic implications for sarcopenia. J Gerontol A Biol Sci Med Sci 62:813–823
Sacheck JM, Cannon JG, Hamada K, Vannier E, Blumberg JB, Roubenoff R (2006) Age-related loss of associations between acute exercise-induced IL-6 and oxidative stress. Am J Physiol Endocrinol Metab 291:E340–E349
Salviati G, Zeviani M, Betto R, Nacamulli D, Busnardo B (1985) Effects of thyroid hormones on the biochemical specialization of human muscle fibers. Muscle Nerve 8:363–371
Schaap LA, Pluijm SM, Smit JH, van Schoor NM, Visser M, Gooren LJ, Lips P (2005) The association of sex hormone levels with poor mobility, low muscle strength and incidence of falls among older men and women. Clin Endocrinol (Oxf) 63:152–160
Schertzer JD, Plant DR, Ryall JG, Beitzel F, Stupka N, Lynch GS (2005) β2-agonist administration increases sarcoplasmic reticulum Ca2+-ATPase activity in aged rat skeletal muscle. Am J Physiol Endocrinol Metab 288:E526–E533
Schertzer JD, Ryall JG, Lynch GS (2006) Systemic administration of IGF-I enhances oxidative status and reduces contraction-induced injury in skeletal muscles of mdx dystrophic mice. Am J Physiol Endocrinol Metab 291:E499–E505
Schertzer JD, van der Poel C, Shavlakadze T, Grounds MD, Lynch GS (2008) Muscle specific overexpression of IGF-I improves E–C coupling in skeletal muscle fibers from dystrophic mdx mice. Am J Physiol Cell Physiol 294:C161–C168
Serrano AL, Baeza-Raja B, Perdiguero E, Jardi M, Munoz-Canoves P (2008) Interleukin-6 is an essential regulator of satellite cell-mediated skeletal muscle hypertrophy. Cell Metab 7:33–44
Sherlock M, Toogood AA (2007) Aging and the growth hormone/insulin like growth factor-I axis. Pituitary 10:189–203
Short KR, Moller N, Bigelow ML, Coenen-Schimke J, Nair KS (2008) Enhancement of muscle mitochondrial function by growth hormone. J Clin Endocrinol Metab 93:597–604
Simonides WS, Brent GA, Thelen MH, van der Linden CG, Larsen PR, van Hardeveld C (1996) Characterization of the promoter of the rat sarcoplasmic endoplasmic reticulum Ca2+-ATPase 1 gene and analysis of thyroid hormone responsiveness. J Biol Chem 271:32048–32056
Sinha-Hikim I, Taylor WE, Gonzalez-Cadavid NF, Zheng W, Bhasin S (2004) Androgen receptor in human skeletal muscle and cultured muscle satellite cells: up-regulation by androgen treatment. J Clin Endocrinol Metab 89:5245–5255
Sinha-Hikim I, Cornford M, Gaytan H, Lee ML, Bhasin S (2006) Effects of testosterone supplementation on skeletal muscle fiber hypertrophy and satellite cells in community-dwelling older men. J Clin Endocrinol Metab 91:3024–3033
Siriett V, Platt L, Salerno MS, Ling N, Kambadur R, Sharma M (2006) Prolonged absence of myostatin reduces sarcopenia. J Cell Physiol 209:866–873
Siriett V, Salerno MS, Berry C, Nicholas G, Bower R, Kambadur R, Sharma M (2007) Antagonism of myostatin enhances muscle regeneration during sarcopenia. Mol Ther 15:1463–1470
Snow MH (1977) The effects of aging on satellite cells in skeletal muscles of mice and rats. Cell Tissue Res 185:399–408
Sohal RS, Weindruch R (1996) Oxidative stress, caloric restriction, and aging. Science 273:59–63
Solomon AM, Bouloux PM (2006) Modifying muscle mass - the endocrine perspective. J Endocrinol 191:349–360
Sotiropoulos A, Ohanna M, Kedzia C, Menon RK, Kopchick JJ, Kelly PA, Pende M (2006) Growth hormone promotes skeletal muscle cell fusion independent of insulin-like growth factor 1 up-regulation. Proc Natl Acad Sci U S A 103:7315–7320
Spangenburg EE, Abraha T, Childs TE, Pattison JS, Booth FW (2003) Skeletal muscle IGF-binding protein-3 and -5 expressions are age, muscle, and load dependent. Am J Physiol Endocrinol Metab 284:E340–E350
Stewart CE, Newcomb PV, Holly JM (2004) Multifaceted roles of TNF-alpha in myoblast destruction: a multitude of signal transduction pathways. J Cell Physiol 198:237–247
Szulc P, Beck TJ, Marchand F, Delmas PD (2005) Low skeletal muscle mass is associated with poor structural parameters of bone and impaired balance in elderly men–the MINOS study. J Bone Miner Res 20:721–729
Thompson RW, McClung JM, Baltgalvis KA, Davis JM, Carson JA (2006) Modulation of overload-induced inflammation by aging and anabolic steroid administration. Exp Gerontol 41:1136–1148
Tsujinaka T, Fujita J, Ebisui C, Yano M, Kominami E, Suzuki K, Tanaka K, Katsume A, Ohsugi Y, Shiozaki H, Monden M (1996) Interleukin 6 receptor antibody inhibits muscle atrophy and modulates proteolytic systems in interleukin 6 transgenic mice. J Clin Invest 97:244–249
Turner JD, Rotwein P, Novakofski J, Bechtel PJ (1988) Induction of mRNA for IGF-I and -II during growth hormone-stimulated muscle hypertrophy. Am J Physiol 255:E513–E517
van der Linden GC, Simonides WS, van Hardeveld C (1992) Thyroid hormone regulates Ca2+-ATPase mRNA levels of sarcoplasmic reticulum during neonatal development of fast skeletal muscle. Mol Cell Endocrinol 90:125–131
van den Beld AW, de Jong FH, Grobbee DE, Pols HA, Lamberts SW (2000) Measures of bioavailable serum testosterone and estradiol and their relationships with muscle strength, bone density, and body composition in elderly men. J Clin Endocrinol Metab 85:3276–3282
van den Beld AW, Lamberts SW (2002) Endocrine aspects of healthy ageing in men. In: Novartis Foundation (eds) Endocrine facets of ageing. Wiley, New York, pp 3–25
van den Beld AW, Blum WF, Pols HA, Grobbee DE, Lamberts SW (2003) Serum insulin-like growth factor binding protein-2 levels as an indicator of functional ability in elderly men. Eur J Endocrinol 148:627–634
Veldhuis JD, Iranmanesh A, Weltman A (1997) Elements in the pathophysiology of diminished growth hormone (GH) secretion in aging humans. Endocrine 7:41–48
Verdijk LB, Koopman R, Schaart G, Meijer K, Savelberg HH, van Loon LJ (2007) Satellite cell content is specifically reduced in type II skeletal muscle fibers in the elderly. Am J Physiol Endocrinol Metab 292:E151–E157
Vermeulen A (1991) Clinical review 24: Androgens in the aging male. J Clin Endocrinol Metab 73:221–224
Viguerie N, Langin D (2003) Effect of thyroid hormone on gene expression. Curr Opin Clin Nutr Metab Care 6:377–381
Visser M, Pahor M, Taaffe DR, Goodpaster BH, Simonsick EM, Newman AB, Nevitt M, Harris TB (2002) Relationship of interleukin-6 and tumor necrosis factor-alpha with muscle mass and muscle strength in elderly men and women: the Health ABC Study. J Gerontol A Biol Sci Med Sci 57:M326–M332
Wagner KR, Liu X, Chang X, Allen RE (2005) Muscle regeneration in the prolonged absence of myostatin. Proc Natl Acad Sci U S A 102:2519–2524
Waters DL, Yau CL, Montoya GD, Baumgartner RN (2003) Serum Sex Hormones, IGF-1, and IGFBP3 Exert a Sexually Dimorphic Effect on Lean Body Mass in Aging. J Gerontol A Biol Sci Med Sci 58:648–652
Welle S, Bhatt K, Shah B, Thornton C (2002) Insulin-like growth factor-1 and myostatin mRNA expression in muscle: comparison between 62–77 and 21–31 yr old men. Exp Gerontol 37:833–839
Yarasheski KE (2003) Exercise, aging, and muscle protein metabolism. J Gerontol A Biol Sci Med Sci 58:M918–M922
Yu F, Hedstrom M, Cristea A, Dalen N, Larsson L (2007) Effects of ageing and gender on contractile properties in human skeletal muscle and single fibres. Acta Physiol (Oxf) 190:229–241
Zadik Z, Chalew SA, McCarter RJ Jr, Meistas M, Kowarski AA (1985) The influence of age on the 24-hour integrated concentration of growth hormone in normal individuals. J Clin Endocrinol Metab 60:513–516
Zebedee Z, Hara E (2001) Id proteins in cell cycle control and cellular senescence. Oncogene 20:8317–8325
Zheng Z, Wang ZM, Delbono O (2002) Insulin-like growth factor-1 increases skeletal muscle dihydropyridine receptor α1S transcriptional activity by acting on the cAMP-response element-binding protein element of the promoter region. J Biol Chem 277:50535–50542
Acknowledgements
Supported by research grant funding from the Australian Research Council Discovery-Project funding scheme (DP0665071, DP0772781), the National Health and Medical Research Council of Australia (350439, 454561, 509313), the Muscular Dystrophy Association (USA, 3595, 4167), the Rebecca L. Cooper Medical Research Foundation, and Pfizer Inc. (USA).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ryall, J.G., Schertzer, J.D. & Lynch, G.S. Cellular and molecular mechanisms underlying age-related skeletal muscle wasting and weakness. Biogerontology 9, 213–228 (2008). https://doi.org/10.1007/s10522-008-9131-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10522-008-9131-0