Abstract
Changes in the levels of O-linked N-acetyl-glucosamine (O-GlcNAc) on nucleocytoplasmic protein have been associated with a number of age-related diseases such as Alzheimer’s and diabetes; however, there is relatively little information regarding the impact of age on tissue O-GlcNAc levels. Therefore, the goal of this study was to determine whether senescence was associated with alterations in O-GlcNAc in heart, aorta, brain and skeletal muscle and if so whether there were also changes in the expression of enzymes critical in regulating O-GlcNAc levels, namely, O-GlcNAc transferase (OGT), O-GlcNAcase and glutamine:fructose-6-phosphate amidotransferase (GFAT). Tissues were harvested from 5- and 24-month old Brown-Norway rats; UDP-GlcNAc, a precursor of O-GlcNAc was assessed by HPLC, O-GlcNAc and OGT levels were assessed by immunoblot analysis and GFAT1/2, OGT, O-GlcNAcase mRNA levels were determined by RT-PCR. In the 24-month old animals serum insulin and triglyceride levels were significantly increased compared to the 5-month old group; however, glucose levels were unchanged. Protein O-GlcNAc levels were significantly increased with age (30–107%) in all tissues examined; however, paradoxically the expression of OGT, which catalyzes O-GlcNAc formation, was decreased by ∼30% in the heart, aorta and brain. In the heart increased O-GlcNAc was associated with increased UDP-GlcNAc levels and elevated GFAT mRNA while in other tissues we found no difference in UDP-GlcNAc or GFAT mRNA levels. These results demonstrate that senescence is associated with increased O-GlcNAc levels in multiple tissues and support the notion that dysregulation of pathways leading to O-GlcNAc formation may play an important role in the development of age-related diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The addition of O-linked N-acetylglucosamine (O-GlcNAc) to the serine and threonine residues of proteins, known as protein O-glycosylation is a highly dynamic posttranslational modification similar to phosphorylation (Haltiwanger et al. 1990; Haltiwanger et al. 1992; Gao et al. 2001; Hanover 2001; Wells et al. 2001; Vosseller et al. 2002a; Whelan and Hart 2003). Unlike other glycosylation processes O-glycosylation is specific to the nucleus and the cytosol and does not occur in the Golgi or the endoplasmic reticulum (Torres and Hart 1984; Holt and Hart 1986). It is increasing recognized that alterations in O-GlcNAc levels play an important role in regulating signal transduction pathways (Zachara and Hart 2004; Love and Hanover 2005; Buse 2006; Slawson et al. 2006; Zachara and Hart 2006). Numerous proteins have been shown to be subject to O-GlcNAc modification, including cytoskeletal proteins, transcription factors, metabolic enzymes, kinases/phosphatases, chaperons, nuclear hormone receptors and proto-oncogenes (Wells et al. 2003; Zachara and Hart 2004; Love and Hanover 2005; Davidoff 2006; Zachara and Hart 2006). O-GlcNAc has been shown to modify enzyme activity (Du et al. 2001; Federici et al. 2002), protein-protein interaction (Roos et al. 1997; Han et al. 1998), half life of proteins (Han et al. 1998), subcellular localization (Duverger et al. 1996) and transcription (Gao et al. 2003). It has also been shown that O-glycosylation and phosphorylation can be reciprocal on some proteins (e.g., c-myc (Chou et al. 1995), estrogen receptor-β (Cheng et al. 2000), eNOS (Du et al. 2001)) .
In contrast to the more than 500 kinases regulating phosphorylation (Manning et al. 2002) there is a single gene encoding O-GlcNAc transferase (Kreppel et al. 1997; Kreppel and Hart 1999), the enzyme catalyzing the addition of N-acetylglucosamine to the Ser/Thr residues of proteins. Recently, Whisenhunt and colleagues demonstrated that OGT directly associates with O-GlcNAcase (Whisenhunt et al. 2006), the other enzyme regulating the removal the single N-acetylglucosamine moiety from the O-GlcNAc modified proteins (Dong and Hart 1994). However, the regulation of the activity these enzymes is complex and not yet fully understood. It is known that OGT is very sensitive to UDP-N-acetylglucosamine (UDP-GlcNAc) concentrations (Haltiwanger et al. 1992), which is the endproduct of the hexosamine biosynthesis pathway (HBP). The rate limiting enzyme of this pathway is glutamine: fructose 6-phospate amidotransferase (GFAT), which catalyzes the formation of glucosamine 6-phosphate from fructose 6-phosphate with glutamine as the amine donor (Kornfeld 1967).
A number of studies have reported that acute activation of pathways leading to O-GlcNAc formation are cytoprotective (Zachara et al. 2004; Liu et al. 2006). However, in contrast to the beneficial aspects of acute increases in O-GlcNAc levels, sustained increases in O-GlcNAc have been associated with the pathogenesis of diseases, such as cancer (Chou et al. 1995), neurodegenerative diseases (Hanover 2001; Wells et al. 2003; Love and Hanover 2005) as well as diabetes and diabetic complications (Zachara and Hart 2004; Love and Hanover 2005; Buse 2006; Zachara and Hart 2006; Fulop et al. 2007a). However, despite the potential importance of O-GlcNAc in the development of age-related diseases, relatively little is known about the impact of aging on the regulation of O-GlcNAc levels. Rex-Mathes et al. reported age-dependent changes in O-GlcNAc in mouse brain (Rex-Mathes et al. 2001), which were characterized by a significant increase between 3 and 7 months of age and a subsequent decline up to 13 months. We recently found that in rats, between adolescence (6 week old) and young adult (22 week old), there was a significant decrease in O-GlcNAc levels in the heart that was associated with reduced OGT expression (Fulop et al. 2007b).
Thus, while data indicate that OGT and O-GlcNAc levels change with age there is no information regarding the development of senescence on tissue O-GlcNAc levels in otherwise healthy animals. Therefore, we investigated the effect of aging on the HBP, O-GlcNAc levels and on the expression of the regulating enzymes in the cardiovascular system, brain and skeletal muscle from 5 and 24 month old Brown Norway rats.
Methods
Animals
Animal experiments were approved by the University of Alabama Institutional Animal Care and Use Committee and conformed to the Guide for the Care and Usage of Laboratory Animals published by the National Institutes of Health (NIH Publication No. 85–23, 1996). Non-fasted, 5 (n = 5) and 24 month old (n = 5), male Brown Norway rats (National Institute of Aging, NIH) were used.
Materials
All chemicals were purchased from Sigma-Aldrich unless otherwise stated.
Analysis of serum metabolites
Blood samples were collected immediately after decapitation from all animals. Serum glucose, insulin, lipid and free fatty acid levels were measured as previously described (Wang and Chatham 2004).
Real time RT-PCR analysis
RNA was extracted from tissues using TRIzol (Invitrogen Corp, Carlsbad, CA), treated with DNA-ase I to remove genomic DNA, purified using an RNA purification kit (Invitrogen), and reverse transcribed to cDNA using the SYBR Green RT-PCR kit (Applied Biosystems, Foster City, CA) and specific primers as described in Table 1. cDNA was amplified by PCR in the iCycler for 40 cycles, and relative RNA levels were calculated using the iCycler software and a standard equation (Applied Biosystems) and normalized using GAPDH mRNA. Results were standardized to the mean value of the 5 month-old group.
Immunoblot analysis
Hearts, abdominal aorta, liver, brain and skeletal muscle (m. gluteus) were freshly isolated and ground to a fine powder under liquid nitrogen and homogenized in T-PER (Pierce) containing 5% protease inhibitor cocktail, 40 μmol/l PUGNAc (Carbogen), 1 mmol/l sodium-orthovanadate and 20 mmol/l sodium-fluoride on ice and centrifuged for 10 min at 15000×g. The protein concentration of the supernatant was measured using Bio-Rad Protein Assay Kit. Tissue lysates were separated on 7% or 10% SDS-PAGE and transferred to PVDF membrane (Pall). Equal loading of protein was confirmed by Sypro Ruby staining (Bio-Rad) on the membranes. Blots were probed with the appropriate antibody in casein blocking buffer. Anti-O-GlcNAc antibody, CTD110.6 (a kind gift of Mary-Ann Accavitti), anti-OGT (SQ-17, Sigma) antibodies were used. Blots were visualized with enhanced chemiluminescent assay (Pierce) and the signal was detected with UVP BioChemi System (UVP). Densitometry was quantified using Labworks analysis software (UVP).
HPLC analysis
Approximately 50 mg of frozen tissue powder was homogenized in 1 ml ice-cold 0.3 mol/l perchloric acid and centrifuged for 15 min at 15000×g at 4°C. PCA was removed from the supernatant with 2 volumes of 1:4 trioctylamine:1,1,2-trichloro-trifluoroethan mixture. Samples were loaded on Partisil 10 SAX column (Beckman), nucleotide sugars were measured at 262 nm using 2 ml/min flow rate and linear salt and pH gradient from 5 to 750 mmol/l (NH4)H2PO4and from pH 2.8 to 3.7 (Robinson et al. 1995). This method cannot separate UDP-GlcNAc from UDP-N-acetyl galactosamine so the results are presented as the sum of UDP-GlcNAc and UDP-GalNAc; however in the heart the ratio of UDP-GlcNAc to UDP-GalNAc is approximately 3:1 (Clark et al. 2003).
Statistical analysis
Data are presented as means ± standard errors. Differences between experimental groups were evaluated with Student’s t-test for unpaired data. Statistical significant differences between groups were defined as P values <0.05 and are indicated in the legends of figures.
Results
Animal characteristics
Body weight, heart weight, serum glucose, insulin, lipids and free fatty acid levels in the 5 and 24- month-old animals are summarized in Table 2. Body weight, heart weight and serum insulin levels were significantly increased in the 24-month group. There was no difference in the heart weight: body weight ratio; however, since Brown-Norway rats exhibit increased adiposity and decreased lean body mass (Wolden-Hanson et al. 1999; Feely et al. 2000; Pausova et al. 2003) we cannot rule out the possibility that the ratio of heart weight to lean body mass could be increased in the 24 month group. Although triglyceride levels were increased by ∼45% this difference was not statistically significant (P = 0.068). There were no changes in cholesterol, HDL or FFA levels with age.
Tissue O-GlcNAc levels
Anti-O-GlcNAc immunoblots from heart, aorta, brain and skeletal muscle from 5 and 24-month groups are shown in Figs. 1a, d and 2a, d. In the heart overall O-GlcNAc levels were increased ∼2-fold in the 24-month group (Fig. 1b); the pattern of O-GlcNAcylated proteins was also altered, with several protein bands appearing below 50 kDa molecular weight (Fig. 1a). In the abdominal aorta overall O-GlcNAc levels were increased ∼50% in the 24-month group (Fig. 1e); however, there were no marked changes in the pattern of O-GlcNAc modified proteins. In the brain O-GlcNAc levels increased ∼30% in the 24-month group compared to the 5-month group (Fig. 2b) and we observed the appearance of a new O-GlcNAc band at around 80 kD as indicated by the arrow in Fig. 2a. In skeletal muscle there was also a significant increase in overall O-GlcNAc (Fig. 2e) and we also found an approx. 50 kDa band appearing in the 24-month group (Fig. 2d).
Anti O-GlcNAc and anti OGT Western blot results from brains (a, b, c) and skeletal muscles (d, e, f) of 5- and 24-month old Brown-Norway rats. (a, d), representative Western blots; (b, e), mean area densities of anti O-GlcNAc blots; and (c, f), mean area densities of anti OGT blots. * P < 0.05 versus control
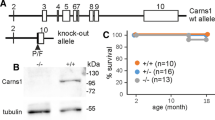
OGT and O-GlcNAcase
To better understand the factors contributing to the increase in O-GlcNAc levels we examined OGT and O-GlcNAcase mRNA levels in heart, brain and skeletal muscle (Table 3). We found that with age O-GlcNAcase mRNA levels were significantly increased in the heart in the 24-month group, whereas OGT mRNA levels were unchanged (Table 3). There were no changes in OGT or O-GlcNAcase mRNA in brain or skeletal muscle with age. There is no readily available O-GlcNAcase antibody; therefore, we were only able to determine OGT protein levels. We found that OGT protein levels were significantly decreased in heart, aorta and brain, and unchanged in skeletal muscle (Figs 1c, f; 2c, f).
Hexosamine biosynthesis pathway
The decrease in OGT protein levels and the increase in O-GlcNAcase mRNA described above is more consistent with a decrease in overall O-GlcNAc levels, rather than the increase seen in the 24-month group. Therefore, we examined GFAT1 and GFAT2 mRNA levels and UDP-GlcNAc levels in heart, brain and skeletal muscle to determine whether increased HBP activity could account for the increase in O-GlcNAc. In the heart, mRNA levels of GFAT1 and GFAT2 were markedly increased in the 24-month group compared to the 5 month old (Fig. 3a); however, the increase in GFAT1 was not significant (p = 0.14). Unfortunately, because there is no readily available antibody against GFAT we were not able to determine whether there were also changes in GFAT protein levels. However, consistent with an increase in GFAT mRNA levels and the increase in O-GlcNAc, UDP-HexNAc levels were significantly higher in hearts from 24-month old rats (Fig. 3a). In skeletal muscle there was no change in GFAT1 mRNA; however, there was ∼2-fold increase in GFAT2 mRNA (p = 0.22) (Fig. 3c). Skeletal muscle UDP-HexNAc levels were not significantly different between 5 and 24-month groups. In the brain there were no changes in GFAT1, GFAT2 or UDP-GlcNAc levels between 5 and 24-month groups (Fig. 3b).
Discussion
There is increasing recognition that O-GlcNAc modification of serine and threonine residues on cytosolic and nuclear proteins is an important regulatory mechanism involved in signal transduction (Zachara and Hart 2004; Love and Hanover 2005; Buse 2006; Slawson et al. 2006; Zachara and Hart 2006) and changes in O-GlcNAc levels have been implicated in the development of age-related diseases. Rex-Mathes et al. showed aged related changes in O-GlcNAc in the mouse brain between 3 and 13 months of age (Rex-Mathes et al. 2001) and we have reported a decrease in O-GlcNAc and OGT expression in the heart between 6 and 22 weeks of age (Fulop et al. 2007b). We show here for the first time that, in senescent rats compared to young adult rats, O-GlcNAc levels in heart, aorta, brain and skeletal muscle were significantly increased. However, paradoxically the protein levels of OGT, which catalyzes O-GlcNAc synthesis, were significantly decreased with senescence. The increased O-GlcNAc levels in the heart were associated with increased levels of GFAT2 mRNA and increased UDP-HexNAc concentration, consistent with increased HBP activity. However, no such changes were seen in brain or skeletal muscle. Taken together these results support the notion that aging is associated with dysregulation of the pathways involved in regulating O-GlcNAc levels and this may be a contributing factor to the increased prevalence of age-related diseases such as diabetes, cancer or neurodegenerative disease.
Regulation of O-GlcNAc levels is complex and remains poorly understood, being dependent on the activity and expression levels of OGT and O-GlcNAcase, which catalyze O-GlcNAc synthesis and removal respectively. OGT is very sensitive to UDP-GlcNAc concentrations; the Km value for UDP-GlcNAc of OGT is one of the lowest among galactosyltransferases. This gives OGT a competitive advantage over the UDP-GlcNAc transporters (Haltiwanger et al. 1992), which are responsible for moving UDP-GlcNAc from the cytosol to the Golgi apparatus or to the endoplasmic reticulum. UDP-GlcNAc is a product of the HBP and has been shown to be increased in hearts from both type-1 and type-2 diabetic rats (Clark et al. 2003; Fulop et al. 2007b), in which O-GlcNAc levels were also increased. Flux through the HBP is regulated in part by GFAT and we found here that in the heart GFAT2 mRNA levels were increased ∼3 fold and this was also associated with a significant increase in UDP-GlcNAc levels in the heart. Thus, in the heart the increase in O-GlcNAc levels in the 24-month group, could be attributed at least in part by increased HBP flux.
Surprisingly, however, there were no significant changes in either GFAT mRNA or UDP-GlcNAc levels in either brain or skeletal muscle, despite the fact that O-GlcNAc levels were significantly increased in the 24-month group. The increase in O-GlcNAc levels in brain and skeletal muscle were more modest (∼30–40%) than those in heart (∼2-fold increase), which suggests that the heart is more susceptible to the age-dependent increases in HBP and O-GlcNAc. It is also important to note, that while UDP-GlcNAc levels are frequently used as a surrogate marker for HBP flux, the levels will only increase under conditions where the rate of synthesis is greater that the rate of consumption via OGT and other pathways. Thus, a modest increase in HBP flux if matched by an increase in flux through OGT, could lead to an increase in O-GlcNAc levels without any change in UDP-GlcNAc levels. Similarly, a lack of change in GFAT mRNA levels does not necessarily indicate that GFAT protein levels or GFAT activity are unchanged. It should be noted that the GFAT activity can be modulated by PKA-mediated phosphorylation (Chang et al. 2000); thus, an increase in HBP flux could occur in the absence of any change in GFAT mRNA or protein. Clearly further studies are warranted to better understand the effect of age of the regulation of the HBP.
While the effect of age on GFAT mRNA and UDP-GlcNAc levels were variable between tissues, with the exception of skeletal muscle, we found a significant decrease in OGT expression levels in all tissues examined. Somewhat surprisingly however, despite the decrease in protein there was no change in OGT mRNA levels. Marshall et al reported that the turnover of OGT is relatively slow, suggesting that changes in OGT expression do not play a role in the short term regulation of O-GlcNAc (Marshall et al. 2005). O-GlcNAcylation of proteins has been reported to regulate translation (Comer and Hart 2000) and to modify the half life of proteins (Han et al. 1998). Since, OGT is also known to be a target of O-glycosylation (Kreppel et al. 1997), the lower OGT protein levels in the 24 month old animals could be due to enhanced degradation. Alternatively, there is also a growing appreciation of the role of microRNA in the post-transcriptional regulation of protein expression, which may occur via inhibition of target mRNA translation after the translation initiation step (Jackson and Standart 2007). Thus, microRNAs can decrease translation of specific proteins, without affecting mRNA abundance. While, it remains to be determined whether OGT expression is modulated by mircoRNA, it has been proposed that dysregulation of microRNAs could contribute to age-dependent diseases (Wang 2007).
The decrease in OGT expression is also at odds with the increase in O-GlcNAc levels seen in the same tissues; however, as noted above the regulation of O-GlcNAc levels is complex and poorly understood. Other factors such as decreased O-GlcNAcase activity could contribute to an increase in O-GlcNAc; although this would seem to be contradicted by the increase in O-GlcNAcase mRNA in the heart. On the other hand, as seen with OGT, changes in mRNA do not necessarily reflect protein levels and unfortunately, the lack of a commercially available O-GlcNAcase antibody, precluded determination of O-GlcNAcase protein levels in these experiments. Nevertheless, it should also be noted that in hearts from diabetic mice there was an increase in O-GlcNAcase mRNA despite an overall increase in O-GlcNAc levels (Hu et al. 2005). These contradictory changes in O-GlcNAc, mRNA and protein levels seen with age, emphasize our limited understanding of the regulation of these pathways and highlight the need for the development of new techniques designed to quantify rates of O-GlcNAc synthesis and degradation in intact cells and tissues.
Increased levels of O-GlcNAc are associated with the development of insulin resistance and diabetes (Zachara and Hart 2004; Love and Hanover 2005; Buse 2006; Zachara and Hart 2006; Fulop et al. 2007a). For example, in cultured adipocytes increased levels of O-GlcNAc resulted in impaired insulin-signaling and insulin stimulated glucose uptake (Vosseller et al. 2002b). (Park et al. 2005). Furthermore, Akimoto et al showed that in Goto-Kakizaki rats the development of insulin resistance was associated with increased O-GlcNAc in pancreatic islets (Akimoto et al. 2007). It is noteworthy that in the 24-month old rats not only were tissue O-GlcNAc levels increased, but the animals were also markedly insulin resistant as evident by the ∼4-fold increase in serum insulin levels. This is consistent with reports of impaired glucose tolerance and decreased insulin sensitivity associated with aging (Basu et al. 2003; Burattini et al. 2006), which could exacerbate the imbalance between death and survival signals and contribute to increased apoptosis and cell loss associated with aging and senescence (Zhang and Herman 2002). It is important to note that, while tempting to suggest that the increase in skeletal muscle O-GlcNAc is causative in the development of insulin resistance seen with aging, such a relationship cannot be established from these data. It is also possible that if in the 24-month group, the heart retained a higher level of insulin sensitivity relative to other tissues this could contribute to greater increase in UDP-GlcNAc and O-GlcNAc levels in heart. However, it should be noted that in adipocytes, insulin alone had no direct effect on increasing HBP metabolites (Traxinger and Marshall 1991).
In the heart increased HBP flux and O-GlcNAc levels have been associated with impaired function, particularly in the context of diabetes. For example, we found that a brief period of streptozotocin (STZ)-induced diabetes and acute glucosamine treatment, interventions known to increase HBP flux and O-GlcNAc levels in the heart, blunted the inotropic response of the isolated perfused heart to phenylephrine, (Pang et al. 2004). Clarke et al. demonstrated that in neonatal cardiomyocytes increasing protein O-GlcNAc levels either by hyperglycemia or glucosamine treatment resulted in impaired SR function (Clark et al. 2003). Subsequently, Hu et al. showed that increased O-GlcNAcase expression improved whole heart function in diabetic mice (Hu et al. 2005). We have recently reported that in type-2 diabetic animals increased O-GlcNAc levels were associated with impaired cardiomyocyte EC-coupling (Fulop et al. 2007b). It is also intriguing to note that a contributing factor to impaired diastolic function in the aged heart appears to be decreased SERCA expression, which could be reversed by overexpression of SERCA (Schmidt-Schweda and Holubarsch 2000). In hearts from diabetic animals, with increased O-GlcNAc levels, SERCA expression was also significantly reduced and this was reversed by overexpression of O-GlcNAcase (Hu et al. 2005). Thus, the increase in cardiac O-GlcNAc levels seen here in the 24-month group could be an important contributing factor to the impaired contractility associated with the senescent heart (Lakatta 1993).
It is also of interest that pressure overload cardiac hypertrophy was associated with an increase in GFAT2 expression and UDP-GlcNAc levels (Young et al. 2007), which is very similar to our observations in the 24 month group. There is evidence of an age dependent increase in cardiac hypertrophy in Brown Norway rats (Walker et al. 2006). Although we found no significant increase in heart weight to body weight in the 24 month groups (Table 2); this may not be a good marker of cardiac hypertrophy due to the increase in adiposity and decrease in lean body mass seen with age in these animals (Wolden-Hanson et al. 1999; Feely et al. 2000; Pausova et al. 2003). Thus, the ratio of heart weight to tibia length would be a more accurate measure of determining the effect of age on cardiac hypertrophy (Yin et al. 1982). The use of molecular markers such as mRNA or protein levels of ANF would also provide additional insight to the potential contribution of cardiac hypertrophy to the increase in O-GlcNAc levels seen in the 24 month group.
While we did not assess cardiac function in this study, impaired diastolic and systolic function has been reported with age in Brown-Norway rats (Walker et al. 2006). Diabetes also leads to impaired cardiac function and is also associated with increased O-GlcNAc levels in cardiomyocytes (Fulop et al. 2007b) and the intact heart (Hu et al. 2005); furthermore, increasing O-GlcNAcase expression in the heart from diabetic animals decreased O-GlcNAc levels and improved cardiac function (Hu et al. 2005). However, it should be noted that acute increases in O-GlcNAc levels induced by glucosamine in the perfused rat heart had no adverse effects on cardiac function (Fulop et al. 2007c). It is possible that the different effects of acute versus chronic increases in O-GlcNAc levels on cardiac function could be due to modification of different proteins. However, with diabetes increases in O-GlcNAc levels were mainly seen in high molecular weight proteins, while with age we have seen bands appearing below 50 kDa. This observation suggests that pathomechanism of the functional impairment seen in diabetic animals may be different from those seen with age.
A number of proteins identified as targets for O-GlcNAc modification are found in the heart, including cytoskeletal proteins, metabolic enzymes, and members of signaling pathways (Zachara and Hart 2004; Love and Hanover 2005; Fulop et al. 2007a). However, to date there has been no comprehensive survey of O-GlcNAc modified proteins in the heart and such extensive experiments were beyond the scope of this study. However, several nervous system specific proteins have been shown to be O-glycosylated and alteration in O-GlcNAc levels of these proteins have been implicated playing an important role in the development of neurodegenerative disorders (Hanover 2001; Wells et al. 2003; Love and Hanover 2005). Changes in O-glycosylation levels of cytoskeletal proteins such as neurofilaments and synapsin (Dong et al. 1993; Cole and Hart 1999; Deng et al. 2008) tau (Arnold et al. 1996; Lefebvre et al. 2003), β-amyloid precursor (Griffith et al. 1995), clathrin assembly protein 3 (Yao and Coleman 1998b) and AP180 (Yao and Coleman 1998a) have been implicated in the pathophysiological mechanisms underlying the development of Alzheimer’s disease Furthermore the chromosomal localization of O-GlcNAcase has been identified as the locus of Alzheimer disease on the chromosome 10 (Hanover 2001; Love and Hanover 2005). Increased O-GlcNAc levels have been shown to inhibit proteasomal function in the brain, which was associated with increased neuronal apoptosis (Liu et al. 2004); it was proposed that this may contribute to neurodegeneration. Thus, the increase in protein O-GlcNAc levels in the brain in the 24-month group supports the notion that O-GlcNAc may contribute to the age related increase in neurodegenerative diseases.
The potential consequences of increased O-GlcNAc in aorta is somewhat less clear; however, increased HBP flux and O-GlcNAc levels have been associated with impaired eNOS activity (Du et al. 2001), increased PAI-1 expression (Goldberg et al. 2006) and TGF-ß1 expression (Kolm-Litty et al. 1998; Du et al. 2000; James et al. 2000). Thus, elevated O-GlcNAc levels in the 24-month old group, could contribute to the development of impaired vascular reactivity and increased incidence of atherosclerosis commonly associated with aging (Marin 1995).
This study is intrinsically descriptive in nature and definitive conclusions regarding the regulation of O-GlcNAc levels are hampered by the lack of available antibodies for GFAT and O-GlcNAcase. Although, there were some tissue specific differences in GFAT and O-GlcNAcase mRNA levels, there was a consistent increase in O-GlcNAc with age in all tissues examined. Therefore, it seems reasonable to propose that senescence leads to dysregulation of pathways regulating O-GlcNAc levels resulting in a sustained increase in O-GlcNAc in multiple tissues. Given that increased O-GlcNAc levels are associated with impaired insulin signaling, decreased cardiac function and increased neuronal loss, the results from this study support the notion that increased O-GlcNAc levels may contribute to the development of age related disease such as diabetes, heart failure and neurodegenerative diseases. Clearly, further studies are needed better understand the impact of aging on the regulation of O-GlcNAc levels and to identify specific mechanisms by which increased O-GlcNAc contribute to cellular dysfunction associated with senescence.
Abbreviations
- AD:
-
Alzheimer disease
- AP:
-
Chlatrin assembly protein
- EC:
-
Excitation-contraction coupling
- eNOS:
-
Endothelial nitrogen oxide synthase
- FFA:
-
Free fatty acid
- GFAT:
-
Glutamine: fructose-6-phosphate amidotransferase
- GLUT:
-
Glucose transporter
- GSK:
-
Glycogen synthase kinase
- HBP:
-
Hexosamine biosynthesis pathway
- HDL:
-
High density lipoprotein
- IRS:
-
Insulin receptor substrate
- O-GlcNAc:
-
O-linked N-acetylglucosamine
- OGA:
-
N-acetylglycosidase, O-GlcNAc-ase
- OGT:
-
O-glucoronyl transferase, O-GlcNAc transferase
- PCA:
-
Perchloric acid
- PUGNAc:
-
O-(2-Acetamido-2-deoxy-d-glucopyranosylidene)amino N-phenyl carbamate
- STZ:
-
Streptozotocin
- UDP-GalNAc:
-
Uridine diphospho-N-acetyl-galactosamine
- UDP-GlcNAc:
-
Uridine diphospho-N-acetyl-glucosamine
- UDP-HexNAc:
-
Uridine diphospho-N-acetyl-hexosamine
- ZDF:
-
Zucker diabetic fatty
References
Akimoto Y, Hart GW, Wells L, Vosseller K, Yamamoto K, Munetomo E, Ohara-Imaizumi M, Nishiwaki C, Nagamatsu S, Hirano H and Kawakami H (2007) Elevation of the post-translational modification of proteins by O-linked N-acetylglucosamine leads to deterioration of the glucose-stimulated insulin secretion in the pancreas of diabetic Goto-Kakizaki rats. Glycobiology 17:127–140
Arnold CS, Johnson GV, Cole RN, Dong DL, Lee M, Hart GW (1996) The microtubule-associated protein tau is extensively modified with O-linked N-acetylglucosamine. J Biol Chem 271:28741–28744
Basu R, Breda E, Oberg AL, Powell CC, Dalla Man C, Basu A, Vittone JL, Klee GG, Arora P, Jensen MD, Toffolo G, Cobelli C, Rizza RA (2003) Mechanisms of the age-associated deterioration in glucose tolerance: contribution of alterations in insulin secretion, action, and clearance. Diabetes 52:1738–1748
Burattini R, Di Nardo F, Boemi M, Fumelli P (2006) Deterioration of insulin sensitivity and glucose effectiveness with age and hypertension. Am J Hypertens 19:98–102
Buse MG (2006) Hexosamines, insulin resistance, and the complications of diabetes: current status. Am J Physiol Endocrinol Metab 290:E1–E8
Chang Q, Su K, Baker JR, Yang X, Paterson AJ, Kudlow JE (2000) Phosphorylation of human glutamine:fructose-6-phosphate amidotransferase by cAMP-dependent protein kinase at serine 205 blocks the enzyme activity. J Biol Chem 275:21981–21987
Cheng X, Cole RN, Zaia J, Hart GW (2000) Alternative O-glycosylation/O-phosphorylation of the murine estrogen receptor beta. Biochemistry 39:11609–11620
Chou TY, Hart GW, Dang CV (1995) c-Myc is glycosylated at threonine 58, a known phosphorylation site and a mutational hot spot in lymphomas. J Biol Chem 270:18961–18965
Clark RJ, McDonough PM, Swanson E, Trost SU, Suzuki M, Fukuda M, Dillmann WH (2003) Diabetes and the accompanying hyperglycemia impairs cardiomyocyte cycling through increased nuclear O-GlcNAcylation. J Biol Chem 278:44230–44237
Cole RN, Hart GW (1999) Glycosylation sites flank phosphorylation sites on synapsin I: O-linked N-acetylglucosamine residues are localized within domains mediating synapsin I interactions. J Neurochem 73:418–428
Comer FI, Hart GW (2000) O-Glycosylation of nuclear and cytosolic proteins. Dynamic interplay between O-GlcNAc and O-phosphate. J Biol Chem 275:29179–29182
Davidoff AJ (2006) Convergence of glucose- and fatty acid-induced abnormal myocardial excitation-contraction coupling and insulin signalling. Clin Exp Pharmacol Physiol 33:152–158
Deng Y, Li B, Liu F, Iqbal K, Grundke-Iqbal I, Brandt R and Gong CX (2008) Regulation between O-GlcNAcylation and phosphorylation of neurofilament-M and their dysregulation in Alzheimer disease. Faseb J 22:138–145
Dong DL, Hart GW (1994) Purification and characterization of an O-GlcNAc selective N-acetyl-beta-D-glucosaminidase from rat spleen cytosol. J Biol Chem 269:19321–19330
Dong DL, Xu ZS, Chevrier MR, Cotter RJ, Cleveland DW, Hart GW (1993) Glycosylation of mammalian neurofilaments. Localization of multiple O-linked N-acetylglucosamine moieties on neurofilament polypeptides L and M. J Biol Chem 268:16679–16687
Du XL, Edelstein D, Dimmeler S, Ju Q, Sui C, Brownlee M (2001) Hyperglycemia inhibits endothelial nitric oxide synthase activity by posttranslational modification at the Akt site. J Clin Invest 108:1341–1348
Du XL, Edelstein D, Rossetti L, Fantus IG, Goldberg H, Ziyadeh F, Wu J, Brownlee M (2000) Hyperglycemia-induced mitochondrial superoxide overproduction activates the hexosamine pathway and induces plasminogen activator inhibitor-1 expression by increasing Sp1 glycosylation. Proc Natl Acad Sci USA 97:12222–12226
Duverger E, Roche AC, Monsigny M (1996) N-acetylglucosamine-dependent nuclear import of neoglycoproteins. Glycobiology 6:381–386
Federici M, Menghini R, Mauriello A, Hribal ML, Ferrelli F, Lauro D, Sbraccia P, Spagnoli LG, Sesti G, Lauro R (2002) Insulin-dependent activation of endothelial nitric oxide synthase is impaired by O-linked glycosylation modification of signaling proteins in human coronary endothelial cells. Circulation 106:466–472
Feely RS, Larkin LM, Halter JB, Dengel DR (2000) Chemical versus dual energy x-ray absorptiometry for detecting age-associated body compositional changes in male rats. Exp Gerontol 35:417–427
Fulop N, Marchase RB, Chatham JC (2007a) Role of protein O-linked N-acetyl-glucosamine in mediating cell function and survival in the cardiovascular system. Cardiovasc Res 73:288–297
Fulop N, Mason MM, Dutta K, Wang P, Davidoff AJ, Marchase RB, Chatham JC (2007b) Impact of Type 2 diabetes and aging on cardiomyocyte function and O-linked N-acetylglucosamine levels in the heart. Am J Physiol Cell Physiol 292:C1370–1378
Fulop N, Zhang Z, Marchase RB, Chatham JC (2007c) Glucosamine cardioprotection in perfused rat hearts associated with increased O-linked N-acetylglucosamine protein modification and altered p38 activation. Am J Physiol Heart Circ Physiol 292:H2227–2236
Gao Y, Miyazaki J, Hart GW (2003) The transcription factor PDX-1 is post-translationally modified by O-linked N-acetylglucosamine and this modification is correlated with its DNA binding activity and insulin secretion in min6 beta-cells. Arch Biochem Biophys 415:155–163
Gao Y, Wells L, Comer FI, Parker GJ, Hart GW (2001) Dynamic O-glycosylation of nuclear and cytosolic proteins: cloning and characterization of a neutral, cytosolic beta-N-acetylglucosaminidase from human brain. J Biol Chem 276:9838–9845
Goldberg HJ, Whiteside CI, Hart GW, Fantus IG (2006) Posttranslational, reversible O-glycosylation is stimulated by high glucose and mediates plasminogen activator inhibitor-1 gene expression and Sp1 transcriptional activity in glomerular mesangial cells. Endocrinology 147:222–231
Griffith LS, Mathes M, Schmitz B (1995) Beta-amyloid precursor protein is modified with O-linked N-acetylglucosamine. J Neurosci Res 41:270–278
Haltiwanger RS, Blomberg MA, Hart GW (1992) Glycosylation of nuclear and cytoplasmic proteins. Purification and characterization of a uridine diphospho-N-acetylglucosamine:polypeptide beta-N-acetylglucosaminyltransferase. J Biol Chem 267:9005–9013
Haltiwanger RS, Holt GD, Hart GW (1990) Enzymatic addition of O-GlcNAc to nuclear and cytoplasmic proteins. Identification of a uridine diphospho-N-acetylglucosamine:peptide beta-N-acetylglucosaminyltransferase. J Biol Chem 265:2563–2568
Han I, Roos MD, Kudlow JE (1998) Interaction of the transcription factor Sp1 with the nuclear pore protein p62 requires the C-terminal domain of p62. J Cell Biochem 68:50–61
Hanover JA (2001) Glycan-dependent signaling: O-linked N-acetylglucosamine. FASEB J. 15:1865–1876
Holt GD, Hart GW (1986) The subcellular distribution of terminal N-acetylglucosamine moieties. Localization of a novel protein-saccharide linkage, O-linked GlcNAc. J Biol Chem 261:8049–8057
Hu Y, Belke D, Suarez J, Swanson E, Clark R, Hoshijima M, Dillmann WH (2005) Adenovirus-mediated overexpression of O-GlcNAcase improves contractile function in the diabetic heart. Circ Res 96:1006–1013
Jackson RJ and Standart N (2007) How do microRNAs regulate gene expression? Sci STKE 2007:re1
James LR, Fantus IG, Goldberg H, Ly H, Scholey JW (2000) Overexpression of GFAT activates PAI-1 promoter in mesangial cells. Am J Physiol Renal Physiol 279:F718–F727
Kolm-Litty V, Sauer U, Nerlich A, Lehmann R, Schleicher ED (1998) High glucose-induced transforming growth factor beta1 production is mediated by the hexosamine pathway in porcine glomerular mesangial cells. J Clin Invest 101:160–169
Kornfeld R (1967) Studies on l-glutamine d-fructose 6-phosphate amidotransferase. I. Feedback inhibition by uridine diphosphate-N-acetylglucosamine. J Biol Chem 242:3135–3141
Kreppel LK, Blomberg MA, Hart GW (1997) Dynamic glycosylation of nuclear and cytosolic proteins. Cloning and characterization of a unique O-GlcNAc transferase with multiple tetratricopeptide repeats. J Biol Chem 272:9308–9315
Kreppel LK, Hart GW (1999) Regulation of a cytosolic and nuclear O-GlcNAc transferase. Role of the tetratricopeptide repeats. J Biol Chem 274:32015–32022
Lakatta EG (1993) Myocardial adaptations in advanced age. Basic Res Cardiol 88:125–133
Lefebvre T, Ferreira S, Dupont-Wallois L, Bussiere T, Dupire MJ, Delacourte A, Michalski JC, Caillet-Boudin ML (2003) Evidence of a balance between phosphorylation and O-GlcNAc glycosylation of Tau proteins–a role in nuclear localization. Biochim Biophys Acta 1619:167–176
Liu J, Pang Y, Chang T, Bounelis P, Chatham JC, Marchase RB (2006) Increased hexosamine biosynthesis and protein O-GlcNAc levels associated with myocardial protection against calcium paradox and ischemia. J Mol Cell Cardiol 40:303–312
Liu K, Paterson AJ, Zhang F, McAndrew J, Fukuchi K, Wyss JM, Peng L, Hu Y, Kudlow JE (2004) Accumulation of protein O-GlcNAc modification inhibits proteasomes in the brain and coincides with neuronal apoptosis in brain areas with high O-GlcNAc metabolism. J Neurochem 89:1044–1055
Love DC, Hanover JA (2005) The hexosamine signaling pathway: deciphering the “ O-GlcNAc code”. Sci STKE 2005:re13
Manning G, Whyte DB, Martinez R, Hunter T, Sudarsanam S (2002) The protein kinase complement of the human genome. Science 298:1912–1934
Marin J (1995) Age-related changes in vascular responses: a review. Mech Ageing Dev 79:71–114
Marshall S, Okuyama R, Rumberger JM (2005) Turnover and characterization of UDP-N-acetylglucosaminyl transferase in a stably transfected HeLa cell line. Biochem Biophys Res Commun 332:263–270
Pang Y, Bounelis P, Chatham JC, Marchase RB (2004) The hexosamine pathway is responsible for the inhibition by diabetes of phenylephrine-induced inotropy. Diabetes 53:1074–1081
Park SY, Ryu J, Lee W (2005) O-GlcNAc modification on IRS-1 and Akt2 by PUGNAc inhibits their phosphorylation and induces insulin resistance in rat primary adipocytes. Exp Mol Med 37:220–229
Pausova Z, Sedova L, Berube J, Hamet P, Tremblay J, Dumont M, Gaudet D, Pravenec M, Kren V, Kunes J (2003) Segment of rat chromosome 20 regulates diet-induced augmentations in adiposity, glucose intolerance, and blood pressure. Hypertension 41:1047–1055
Rex-Mathes M, Werner S, Strutas D, Griffith LS, Viebahn C, Thelen K, Schmitz B (2001) O-GlcNAc expression in developing and ageing mouse brain. Biochimie 83:583–590
Robinson KA, Weinstein ML, Lindenmayer GE, Buse MG (1995) Effects of diabetes and hyperglycemia on the hexosamine synthesis pathway in rat muscle and liver. Diabetes 44:1438–1446
Roos MD, Su K, Baker JR, Kudlow JE (1997) O glycosylation of an Sp1-derived peptide blocks known Sp1 protein interactions. Mol Cell Biol 17:6472–6480
Schmidt-Schweda S, Holubarsch C (2000) First clinical trial with etomoxir in patients with chronic congestive heart failure. Clin Sci (Lond) 99:27–35
Slawson C, Housley MP, Hart GW (2006) O-GlcNAc cycling: How a single sugar post-translational modification is changing the Way We think about signaling networks. J Cell Biochem 97:71–83
Torres CR, Hart GW (1984) Topography and polypeptide distribution of terminal N-acetylglucosamine residues on the surfaces of intact lymphocytes. Evidence for O-linked GlcNAc. J Biol Chem 259:3308–3317
Traxinger RR, Marshall S (1991) Coordinated regulation of glutamine: fructose-6-phosphate amidotransferase activity by insulin, glucose, and glutamine. Role of hexosamine biosynthesis in enzyme regulation. J Biol Chem 266:10148–10154
Vosseller K, Sakabe K, Wells L, Hart GW (2002a) Diverse regulation of protein function by O-GlcNAc: a nuclear and cytoplasmic carbohydrate post-translational modification. Curr Opin Chem Biol 6:851–857
Vosseller K, Wells L, Lane MD, Hart GW (2002b) Elevated nucleocytoplasmic glycosylation by O-GlcNAc results in insulin resistance associated with defects in Akt activation in 3T3-L1 adipocytes. Proc Natl Acad Sci USA 99:5313–5318
Walker EM Jr., Nillas MS, Mangiarua EI, Cansino S, Morrison RG, Perdue RR, Triest WE, Wright GL, Studeny M, Wehner P, Rice KM, Blough ER (2006) Age-associated changes in hearts of male Fischer 344/Brown Norway F1 rats. Ann Clin Lab Sci 36:427–438
Wang E (2007) MicroRNA, the putative molecular control for mid-life decline. Ageing Res Rev 6:1–11
Wang P, Chatham JC (2004) The onset of diabetes in Zucker diabetic fatty (ZDF) rats leads to improved recovery of function following ischemia in the isolated perfused heart. Am J Physiol Endocrin Met 286:E725–E736
Wells L, Vosseller K, Hart GW (2001) Glycosylation of nucleocytoplasmic proteins: signal transduction and O-GlcNAc. Science 291:2376–2378
Wells L, Whalen SA, Hart GW (2003) O-GlcNAc: a regulatory post-translational modification. Biochem Biophys Res Commun 302:435–441
Whelan SA, Hart GW (2003) Proteomic approaches to analyze the dynamic relationships between nucleocytoplasmic protein glycosylation and phosphorylation. Circ Res 93:1047–1058
Whisenhunt TR, Yang X, Bowe DB, Paterson AJ, Van Tine BA and Kudlow JE (2006) Disrupting the enzyme complex regulating O-GlcNAcylation blocks signaling and development. Glycobiology 16:551–563
Wolden-Hanson T, Marck BT, Smith L, Matsumoto AM (1999) Cross-sectional and longitudinal analysis of age-associated changes in body composition of male Brown Norway rats: association of serum leptin levels with peripheral adiposity. J Gerontol A Biol Sci Med Sci 54:B99–107
Yao PJ, Coleman PD (1998a) Reduced O-glycosylated clathrin assembly protein AP180: implication for synaptic vesicle recycling dysfunction in Alzheimer’s disease. Neurosci Lett 252:33–36
Yao PJ, Coleman PD (1998b) Reduction of O-linked N-acetylglucosamine-modified assembly protein-3 in Alzheimer’s disease. J Neurosci 18:2399–2411
Yin FC, Spurgein HA, Rakusan K, Weisfeldt ML, Lakatta EG (1982) Use of tibial length to quantify cardiac hypertrophy: applications in the aging rat. Am J Physiol 243:H941-H947
Young ME, Yan J, Razeghi P, Cooksey RC, Guthrie PH, Stepkowski SM, McClain DA, Tian R, Taegtmeyer H (2007) Proposed regulation of gene expression by glucose in rodent heart. Gene Reg Sys Biol 1:251–262
Zachara NE, Hart GW (2004) O-GlcNAc a sensor of cellular state: the role of nucleocytoplasmic glycosylation in modulating cellular function in response to nutrition and stress. Biochim Biophys Acta 1673:13–28
Zachara NE, Hart GW (2006) Cell signaling, the essential role of O-GlcNAc! Biochim Biophys Acta 1761:599–617
Zachara NE, O’Donnell N, Cheung WD, Mercer JJ, Marth JD, Hart GW (2004) Dynamic O-GlcNAc modification of nucleocytoplasmic proteins in response to stress. A survival response of mammalian cells. J Biol Chem 279:30133–30142
Zhang Y, Herman B (2002) Ageing and apoptosis. Mech Ageing Dev 123:245–260
Acknowledgements
This work was supported by grants from the NHLBI HL-076175 (RBM); HL-67464 and HL079364 (JCC) and HL-077100.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fülöp, N., Feng, W., Xing, D. et al. Aging leads to increased levels of protein O-linked N-acetylglucosamine in heart, aorta, brain and skeletal muscle in Brown-Norway rats. Biogerontology 9, 139–151 (2008). https://doi.org/10.1007/s10522-007-9123-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10522-007-9123-5