Abstract
Chemsex—the use of specific drugs during planned sexual activity to sustain or enhance sexual functioning (Bourne et al., 2015)—is widely reported as a major public health issue among gay, bisexual, and other men who have sex with men (GBM) in Western countries. Considering current evidence surrounding Chemsex, we conducted a mixed-methods systematic review regarding psychological and interpersonal factors associated with Chemsex behaviors among GBM. Publications covering Chemsex and psychological or social variables were eligible. Theoretical papers and studies solely presenting physical health outcomes were excluded. 35 English papers published between January 2008 and June 2019 were identified through PubMed, Scopus, and PsycINFO. We performed a parallel-results convergent synthesis (Hong, Pluye, Bujold, & Wassef, 2017) on results extracted from qualitative and quantitative studies comprising the final corpus. Qualitative data suggest that six mechanisms promote Chemsex-related behaviors: dealing with painful emotions or stressful events; normalization and risk minimization of sexualized drug use; giving into interpersonal pressure or fulfilling desire for community belonging; increasing intimacy or connectedness; enhancing sexual performance and functioning; lessening interpersonal and sexual inhibitions. In quantitative reports, six variable categories emerged: sexual control and self-efficacy; sexual functioning; mental health; attitudes toward substance use; life stressors and internalized stressors; and identification with sexual identities or scenes. This review summarizes key psychological and interpersonal correlates of Chemsex among GBM. Further research is needed to replicate current findings and explore new hypotheses across multiple GBM sociodemographic groups and cultural contexts, following best practices in sampling for hard-to-reach populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sexualized drug use (SDU) refers to the use of drugs in a sexual context and is widely reported as a major public health issue among gay, bisexual, and other men who have sex with men (GBM; Giorgetti et al., 2017). Chemsex—a specific type of SDU—refers to the combined use of specific drugs (i.e. crystal methamphetamine, GHB/GBL, and/or mephedrone), before or during planned sexual activity, to sustain or enhance sexual experience or performance (Bourne et al., 2015; Edmundson et al., 2018). Other drugs, such as ketamine, cocaine, or cathinone are also used in Chemsex but to a lesser extent (Ma & Perera, 2016). Colloquially, the expressions Party and Play (PnP) or intensive sex partying also refer to the sexualized use of these substances (Bourne, Reid, Hickson, Torres Rueda, & Weatherburn, 2014; Hammoud et al., 2018). In this review, we therefore use “Chemsex” to designate a sub-type of SDU associated with specific patterns of behavior and levels of risk while under the influence of psychoactive substances, and characterized by the use of crystal methamphetamine, GHB/GBL, mephedrone, ketamine, and/or cocaine (or “Chemsex-related drugs”), with the intent of engaging in sexual activity.
GBM are more likely than men who only have sex with women to use recreational drugs (Abdulrahim, Moncrieff, & Bowden-Jones, 2016; Tomkins, George, & Kliner, 2019) and Chemsex-related drugs (Heinsbroek, Glass, Edmundson, Hope, & Desai, 2018; Lawn, Aldridge, Xia, & Winstock, 2019) in association with sex. Moreover, patterns of drug use among GBM have changed in the last few years (Blais, Otis, Lambert, Cox, & Haig, 2018; Bourne et al., 2015; Sewell et al., 2018) with a notable shift from club drugs (e.g., MDMA) to the use of Chemsex-related drugs (Edmundson et al., 2018). Euphoria and lowered inhibitions induced by Chemsex-related drugs, combined with the frequently prolonged length of Chemsex episodes (which can last several hours or days), partly explains why it is associated with an increase in sexual risk-taking behaviors and a lesser propensity to practice safer-sex (Bourne et al., 2015; Knoops, Bakker, van Bodegom, & Zantkuijl, 2015).
Prevalence of Chemsex
While prevalence of Chemsex among GBM is difficult to estimate, the current available data suggest that, if up to 45% of GBM have engaged in Chemsex at least once (e.g., Lawn et al., 2019), far fewer report recent or recurrent Chemsex behaviors (e.g., Frankis, Flowers, McDaid, & Bourne, 2018; Schmidt et al., 2016). A large amount of research into Chemsex has been conducted in the United Kingdom, focusing mainly on London and surrounding metropolitan areas. In their review of national prevalence of Chemsex in the UK, Edmundson et al. (2018) reported that prevalence estimates for Chemsex range from 17% among men who have sex with men (MSM) attending sexual health clinics to 31% among HIV-positive MSM inpatients from a London clinic. In a cross-sectional online survey in Scotland, Wales, Northern Ireland, and the Republic of Ireland (Frankis et al., 2018), while nearly half of MSM participants reported lifetime illicit substance use, lifetime Chemsex-related substance use was less common (18.0%), and far fewer reported Chemsex drug use in the previous year (8.2%) or month (3.0%). In a large European Internet-based survey across 44 cities (Schmidt et al., 2016), the use of Chemsex-related drugs in the previous 4 weeks ranged between 0.4% and 16.3%. In a recent multi-site cross-sectional survey implemented in 13 European cities (Rosinska et al., 2018), 11.8% of MSM respondents reported polysubstance use during their last sexual encounter. By drug class, however, Chemsex drugs were used by 3.4% of the participants. Baseline data from a large multi-site survey in the United States has reported lifetime prevalence of Chemsex ranging from 9% among White GBM to 27% among minority GBM (Gordon et al., 2017). Results from a global survey of substance use report at least one occurrence of sexualized use of Chemsex-related substances in 39 to 45% of GBM (Lawn et al., 2019). Finally, evidence from both community (Blais et al., 2018) and clinic samples (Pakianathan, Lee, Kelly, & Hegazi, 2016) suggests that Chemsex is increasing among GBM. Variations in prevalence estimates are likely due to differences in the substances considered in the definition of Chemsex, sample composition, substance availability across sites, and local Chemsex scenes (Edmundson et al., 2018; Tomkins et al., 2019). Moreover, stigma and discrimination associated with drug use may lead to an underestimation of the phenomenon among GBM population and limit robust data collection (Melendez-Torres & Bourne, 2016). Finally, prevalence data is rarely specific to drug use before or during sexual activity (“event-level data”; Edmundson et al., 2018; Taggart et al., 2019).
Chemsex, Risk-Taking Behaviors, and Public Health Concerns
Most research about Chemsex among GBM has focused on sexual behaviors (Daskalopoulou et al., 2017; Dearing & Flew, 2015; Glynn et al., 2018; Hegazi et al., 2017; Ottaway et al., 2017a; Weatherburn, Hickson, Reid, Torres-Rueda, & Bourne, 2017). Patterns of sexual behaviors and practices associated with increased HIV and sexually transmitted infection (STI) risks have been reported among GBM who practice Chemsex. A higher prevalence of unprotected anal intercourse (Daskalopoulou et al., 2017; Glynn et al., 2018; Ottaway, Finnerty, Buckingham, & Richardson, 2017b)—including between serodiscordant partners (Pufall et al., 2018) or with partners of unknown HIV status (Dearing & Flew, 2015; González-Baeza et al., 2018), multiple sexual partners (Glynn et al., 2018; Hegazi et al., 2017; Melendez-Torres, Bourne, Hickson, Reid, & Weatherburn, 2018; Rosinska et al., 2018; Sewell et al., 2017), group sex (Hegazi et al., 2017), fisting, sharing sex toys, and the use of bareback sexual networking applications (Daskalopoulou et al., 2017; Hegazi et al., 2017; Ottaway et al., 2017a) have been documented. As a result, GBM Chemsex users are more likely than non-users to have received a diagnosis of HIV infection, acute bacterial STIs, rectal STIs, and hepatitis (Dearing & Flew, 2015; Drückler, Van Rooijen, & De Vries, 2018; González-Baeza et al., 2018; Ottaway et al., 2017a; Page & Nelson, 2016; Pakianathan et al., 2018; Rosinska et al., 2018; Sewell et al., 2017; Wu, Shen, Chiou, Fang, & Lo, 2019). GBM who inject substances in the context of Chemsex parties (referred to as “Slamsex” or “slamming”) with shared needles also face increased exposure to blood-borne viruses such has HIV, hepatitis, or syphilis (González-Baeza et al., 2018; Melendez-Torres & Bourne, 2016; Pufall et al., 2018).
Aim of This Review
Compared to the accumulating data on sexual behaviors and health-related outcomes related to Chemsex, data on psychological and interpersonal factors are scarce. Yet, the relationships between mental health, drug use, and sexual risk behavior appear to be affected by multifaceted and complex psychosocial factors among GBM who practice Chemsex (Power et al., 2018; Weatherburn et al., 2017). As recent reviews on Chemsex have focused on its prevalence and associated risk-taking behaviors, health-related outcomes, and interventions (Edmundson et al., 2018; Knight et al., 2019; Maxwell, Shahmanesh, & Gafos, 2019; Tomkins et al., 2019), the present review aims to examine psychological and interpersonal correlates of Chemsex among GBM, to provide a more refined picture on our current understanding of the phenomenon. The search question addressed in this review was: What are the psychological and interpersonal factors associated with Chemsex among GBM?
Method
Search Method and Inclusion Criteria
Following PRISMA standards (Moher, Liberati, Tetzlaff, & Altman, 2009), we conducted a systematic review of studies examining the association between Chemsex and psychosocial factors, published between January 2008 and June 2019 (see Table 1 for PICO search strategy). Papers were identified through PubMed, Scopus, and PsycINFO databases. The search strategy was based on variations and Boolean connections of Chemsex or alike issues (i.e., party and play, intensive sex partying, slamsex/slamming, sexualized drug use) and psychological or social factors. Considering the late appearance of Chemsex as a concept (Bourne et al., 2014), the research syntax also included the use of psychoactive Chemsex-related substances such as mephedrone (4-methylmethcathinone), GHB (γ-hydroxybutyrate), GBL (γ-butyrolactone), methamphetamines (e.g., N-methylamphetamine or derivatives), as well as ketamine, cocaine, and cathinone (β-keto-amphetamine) which are sometimes taken in combination with other Chemsex-related substances. The list of psychosocial variables was established by the research team, composed of a mental health expert [DL], an expert in sexual behaviors and health [MB], and an information specialist, who determined the terms of the research syntax in natural and controlled language for each database explored. To identify the relevant terms for the research syntax, we adopted a broad approach including indicators known to be associated with psychological, sexual and interpersonal functioning outcomes in GBM substance users (e.g., mental disorders, sexual satisfaction, resilience, life stressors, coping strategies, perceptions of HIV-related stigma, perceived social support; see Table 2 for an example of search strategy regarding psychosocial indicators). Following the search, all identified citations were collated and uploaded into EndNote reference manager software (version 9.0).
Studies were included for full review if they met the following criteria: (1) included the sexualized use of at least one Chemsex-related drug; (2) tested or reported at least one association between Chemsex and a psychosocial variable or theme; (3) included GBM individuals in the sample; (4) reported empirical results; (5) and were published in English. Considering the aforementioned criteria, studies presenting outcome variables related solely to physical health—including no psychological or interpersonal factor—or strictly theoretical papers that did not report original empirical data were excluded.
Potential articles were first screened by reviewing article title and abstract. Articles that were considered relevant after the initial screening process were then fully reviewed for final consideration of inclusion in the review. The first author [DL] and two graduate research assistants evaluated 20% of the sources, selected randomly from the database after the initial screening. Any uncertainties regarding the eligibility of a manuscript for inclusion was discussed before the full screening of remaining articles. Additional sources were identified from references cited in eligible papers.
The first two authors [DL, MB] independently completed the full-text review of each selected manuscript to make the final eligibility decision for the corpus. Eligible studies were critically appraised for methodological quality. Any disagreements that arose between the reviewers were resolved through discussion.
Data Extraction, Transformation, and Synthesis
A multi-level synthesis approach was used on qualitative and quantitative results from the selected papers (Noyes et al., 2018, 2019; Noyes, Popay, Pearson, Hannes, & Booth, 2008). Multi-level synthesis method consists in carrying out qualitative and quantitative analyses and syntheses separately, and then combining them later in a structured fashion. The aims of that mixed methods synthesis were to (1) provide a broader and in-depth understanding the psychosocial factors associated with Chemsex among GBM, (2) identify the most well-documented factors, (3) pinpoint variables, dimensions or themes that were less or not explored by one or both research paradigms, and (4) suggest recommendations for research.
Qualitative and quantitative syntheses were conducted separately by the first two authors, considering their respective expertise in qualitative [DL] and quantitative [MB] methods. The quantitative data was extracted and “qualitized,” a process involving the transformation of reported data into textual descriptions of the quantitative results (from experimental or observational studies) in a way that answers the review questions. Quantitative results from each study were then compared, discussed, and consolidated in the form of a narrative synthesis. For qualitative papers, a thematic analysis of emerging data from the selected studies was conducted (Thomas & Harden, 2008). In order to synthesize data, we copied the authors’ findings in primary research (e.g., verbatim, descriptions) into QSR’s NVivo software (12.0 version) and followed guidelines for the thematic analysis to generate descriptive themes relevant to the review question (Hong, Pluye, Bujold, & Wassef, 2017; Thomas et al., 2003). Finally, the product of each synthesis was juxtaposed and discussed to produce the final synthesis. For this purpose, the respective conclusions of quantitative and qualitatives results were entered into a matrix to identify the matches and mismatches between reported factors associated to Chemsex. Precisely, the matrix was structured tabularly by indicating, in four columns, (1) the qualitative conclusions, (2) the quantitative conclusions, (3) an indicator of the nature of relationship between qualitative and quantitative data (i.e., congruent, divergent, silent), for (4) each theme or variable. The significance to be given to emerging relationships in the matrix was discussed between the first two authors [DL, MB], while taking into account the nature of the studies considered (qualitative or quantitative) and their respective aims (e.g., “examining the experience of disinhibition among GBM who practice Chemsex” versus “examining associations between sexual self-efficacy and Chemsex”).
To present the review conclusions, we opted for a parallel-result convergent synthesis design (Hong et al., 2017), where qualitative and quantitative findings are analyzed and presented separately. The integration of findings occurs during the interpretation of results in the discussion and recommendation sections (see Fig. 1 for the review process).
Results
Search Outcome
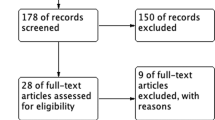
Figure 2 details the inclusion and exclusion process for the systematic review. A total of 2167 papers were initially identified. Once duplicates were removed (n = 401), a total of 1766 paper titles and abstracts were screened for relevance, and excluded if they failed to meet the aforementioned inclusion criteria (n = 1633). The full-text of the 133 remaining articles was assessed by the first two authors [DL, MB] and two graduate research assistants to confirm eligibility. Of the 133 quantitative articles initially identified, inter-researcher agreement was met for more than 85% of papers. After discussion of any emerging disagreements from the independent assessment, a total of 18 qualitative articles and 14 quantitative reports were included. Three additional sources were identified from references cited in eligible papers, not initially identified through the systematic search, providing a total of 35 original articles (18 qualitative; 17 quantitative) included in the final synthesis.
Data Synthesis of Qualitative Reports
Overall, 18 articles presented data from 453 GBM across 16 original studies, with papers by Ahmed et al. (2016), Bourne et al. (2015), and Weatherburn et al. (2017) reporting outcomes of the same study. Most studies overrepresented self-identified White gay men and were conducted in Western countries (U.S., U.K., Canada, Australia, France, and Germany), which share relatively similar cultural, economic and political influences. Only 2 studies focused on Black men (Harawa et al., 2008; Jerome & Halkitis, 2009) or on those who do not identify as gay (Harawa et al., 2008). It is likely that results from eligible papers may differ due to differences in sociodemographic characteristics and self-identified sexual orientation of interviewees, cultural differences and regional availability of drugs, Chemsex definition or substances used, as well as data collection strategies, analyses, and aims of each study (see Table 3 for demographic details of participants, studies aims and characteristics). Moreover, since not all studies solely include GBM who engage in Chemsex (e.g., GBM who use related substances in multiple contexts, including but not limited to sex), only data regarding GBM’s sexualized use of Chemsex-related substances was analysed.
Quality Appraisal of Qualitative Studies
We used the Critical Appraisal Skills Programme (CASP) (2018) tool for qualitative research to assess study quality in terms of methodological rigor, results and transferability. CASP quality appraisal criteria are listed at the end of Table 3. The minimal score for inclusion was set to 4 out of 10 criteria, indicating medium quality; scores of 6 and above indicated high quality. All qualitative articles were independently reviewed by the first author [DL] and a research assistant for scoring. Any disagreement was discussed until consensus was met. One study received a medium score of 5; every other study received high quality scores ranging from 7 to 10 (see Table 3 for an overview of the strengths and limitations of each paper included in the qualitative synthesis).
Findings
Synthesis of published qualitative data on psychological and interpersonal factors suggests that Chemsex behaviors are developed or maintained through six main mechanisms: (1) as a way of dealing with painful emotions or stressful events; (2) in a context of normalization of sexualized drug use and risk minimization; (3) under the influence of interpersonal pressure or the desire to belong to a community; (4) as a way to increase intimacy/connectedness; (5) to enhance sexual performance and functioning; or (6) to lessen interpersonal and sexual inhibitions.
Dealing with Painful Emotions or Stressful Events
In 13 original papers, participants explained that engaging in Chemsex occurred either in contexts of painful emotions (Amaro, 2016; Deimel et al., 2016; Harawa et al., 2008; Hunter et al., 2012; Jerome & Halkitis, 2009; Knight et al., 2014; Liu & Detels, 2012; McCready & Halkitis, 2008; Pollard, Nadarzynski, & Llewellyn, 2018) or in reaction to significant or lasting stressful events (Ahmed et al., 2016; Amaro, 2016; Pollard et al., 2018; Weatherburn et al., 2017). Specifically, GBM in several studies experienced Chemsex as a strategy to cope with unpleasant or painful emotional states such as loneliness (Amaro, 2016; Pollard et al., 2018), boredom (Amaro, 2016; Liu & Detels, 2012), anxiety (Deimel et al., 2016; Knight et al., 2014), stigma associated with HIV-positive status (McCready & Halkitis, 2008), feelings of rejection (Hunter et al., 2012; Weatherburn et al., 2017), guilt related to having sex with men (Deimel et al., 2016; Harawa et al., 2008; Jerome & Halkitis, 2009; Weatherburn et al., 2017), and negative body-image (Weatherburn et al., 2017). For instance, a participant explained how combining sex with drugs was a means to overcome a strong and persisting feeling of boredom: “I wasn’t doing anything at the time, that’s why I did it [GHB and cocaine]. I wasn’t working, I had a lot of spare time, so I did it all the time […]. I used drugs out of boredom, and I was very bored” (26-year-old gay participant; Amaro, 2016, p. 222).
As part of a longitudinal mixed–methods study, McCready and Halkitis (2008) conducted semi-structured interviews with 19 HIV-positive methamphetamine users to explore HIV serostatus disclosure to sexual partners when they practice sexualized drug use. For some participants, condom was perceived as a reminder of their HIV status and was interfering with sexual pleasure, while methamphetamine use was perceived as a mean to gain release and escape from the burdens of HIV stigma: “Every time I have sex when I’m sober, I just feel […] that the condom is always a reminder of being positive. With the crystal, it just kind of takes that away. At a certain point, like after a couple of lines, I really don’t care anymore” (23-year-old mixed-ethnicity participant, McCready & Halkitis, 2008, p. 22).
In four reports (Ahmed et al., 2016; Amaro, 2016; Pollard et al., 2018; Weatherburn et al., 2017), life stressors were repeatedly recognized as factors for engaging in Chemsex. The reported primary triggers were romantic breakups (Ahmed et al., 2016; Amaro, 2016; Pollard et al., 2018), receiving an HIV diagnosis (Ahmed et al., 2016; Amaro, 2016; Weatherburn et al., 2017), the death of a close friend or family member, and the accumulation of professional or domestic pressures (Pollard et al., 2018).
Normalization and Risk Minimization of Sexualized Drug Use
In five qualitative publications (Aguinaldo & Myers, 2008; Ahmed et al., 2016; Bourne et al., 2015; Deimel et al., 2016; Pollard et al., 2018), interviewees reported a perceived normalization of Chemsex within the gay scene (Deimel et al., 2016, p. 7), as if sexualized drug use was customary (Ahmed et al., 2016, p. 31) or generalized among gays (Aguinaldo & Myers, 2008; Ahmed et al., 2016; Deimel et al., 2016; Payne, Lawrence, Soni, Llewellyn, & Dean, 2017; Pollard et al., 2018). For instance, Amhed et al. (2016) investigated social norms related to Chemsex among gay men and their influence on health-related and risk-taking behaviors. They observed that nearly all participants perceived most club-goers as either crystal methamphetamine, mephedrone, or GHB/GBL users. Along the same line, one-sixth expressed a belief that injecting drugs had recently become more common and accepted, with two of their participants describing slamming as “trendy” (p. 33). Furthermore, a participant in Pollard et al. (2018) mentioned the perception of the marginality of not taking drugs during sex: “It feels like everyone is doing it. I mean socially you can’t not do them. It’s considered almost unsocial if you don’t do drugs. Everyone I know […] are taking drugs and are doing the same things” (35-year-old gay participant, Pollard et al., 2018, p. 416).
Bourne et al. (2015) investigated the personal and social contexts associated with sexualized drug use. Data revealed that maintenance of Chemsex-related behaviors appeared often facilitated by minimizing their severity or harmfulness. Authors describe the cognitive minimization process as resulting from participants positively assessing their own drug use as less problematic in comparison to others’ more frequent use or more harmful delivery methods: “Those men that did not take crystal methamphetamine considered it a much more dangerous drug than those who were taking it. Among crystal methamphetamine users, those who did not inject held only this delivery mechanism as the problem behavior. Even among those that injected, some described this act as relatively safe because, unlike others they heard of, they were not sharing needles and not using heroin” (Bourne et al., 2015, p. 1174).
Interpersonal Pressure or Desire for Belonging
In total, six studies have highlighted the role of interpersonal context on initiating Chemsex-related behaviors (Amaro, 2016; Bourne et al., 2015; Deimel et al., 2016; Liu & Detels, 2012; Lyons, Chandra, Goldstein, & Ostrow, 2010; Pollard et al., 2018). Interpersonal factors identified by participants were peer pressure from friends (Bourne et al., 2015; Pollard et al., 2018), being introduced to Chemsex by sexual or romantic partner(s) (Amaro, 2016; Bourne et al., 2015; Pollard et al., 2018), and the more global influence of the gay scene (Bourne et al., 2015; Deimel et al., 2016; Lyons et al., 2010; Pollard et al., 2018). One of the participants in Amaro (2016) explained how he started injecting drugs (slamming) after beginning a relationship with a drug-using partner who initiated him to the practice.
Participants from three studies (Amaro, 2016; Deimel et al., 2016; Pollard et al., 2018) reported that a need for social connectedness—described as a desire to develop a sense of belonging, acceptance and inclusion in a community—motivated their practice of Chemsex. Notably, Deimel et al. (2016) observed that, for some, practicing Chemsex with groups of friends created a sense of community and was a means to obtain recognition among users. In some cases (Pollard et al., 2018), Chemsex was interrelated to emotional and contextual patterns of marginalization and loneliness, until arriving into an accepting, but highly sexualized, environment that the Chemsex scene represents.
Increasing Intimacy/Connectedness
In eight original publications, Chemsex was constructed by participants as a means to facilitate intimacy or to develop a stronger connection with sexual partners (Amaro, 2016; Bourne et al., 2015; Chartier et al., 2009; Deacon, Mooney-Somers, Treloar, & Maher, 2013; Deimel et al., 2016; Parry et al., 2008; Pollard et al., 2018; Weatherburn et al., 2017). For instance, Weatherburn et al. reported that over two-thirds of their interviewees mentioned how drugs enhanced the sense of connection they felt with their partner. In the Pollard et al. (2018) and Weatherburn et al. (2017), Chemsex was described by some participants as a method to overcome emotional or social barriers, offering more instant access to feelings of emotional closeness. Regarding slamming specifically, some participants explained how drug-injecting sessions were experienced as a significant and special bond (Amaro, 2016; Deacon et al., 2013): “We all knew what each other had in terms of illnesses and we deliberately exchanged blood. […] I wanted to connect with this guy in particular. […] It’s intimacy, it’s connection” (42-year-old gay participant, Deacon et al., 2013, p. 406).
However, while all aforementioned studies report that Chemsex increased feelings of emotional and sexual intimacy, three articles (Chartier et al., 2009; Pollard et al., 2018; Weatherburn et al., 2017) nuanced this observation and pointed out that, conversely, Chemsex is experienced by some as a barrier to or incompatible with developing meaningful emotional relationships (Pollard et al., 2018) or intimacy during sex (Chartier et al., 2009; Weatherburn et al., 2017).
Enhancing Sexual Performance and Functioning
Across eight studies, Chemsex was motivated for many by the desire to enhance sexual performance, pleasure, and functioning at different stages of the sexual response (Bourne et al., 2015; Chartier et al., 2009; Deimel et al., 2016; Hunter et al., 2012; Liu & Detels, 2012; Lyons et al., 2010; Parry et al., 2008; Weatherburn et al., 2017). Precisely, participants used drugs instrumentally, because Chemsex-related substances increase either sexual arousal (Deimel et al., 2016; Parry et al., 2008; Weatherburn et al., 2017), pleasure (Chartier et al., 2009; Parry et al., 2008), physical sensations (Hunter et al., 2012; Weatherburn et al., 2017), orgasm intensity (Lyons et al., 2010; Weatherburn et al., 2017) or sexual performance (Chartier et al., 2009; Deimel et al., 2016; Hunter et al., 2012; Parry et al., 2008; Weatherburn et al., 2017).
Regarding sexual arousal specifically, participants mentioned that drugs provide an “edge” (Bourne et al., 2015, p. 1173) or add excitement to a familiar sexual setting (Weatherburn et al., 2017), particularly with a regular or long-term partner. Participants from Deimel et al. (2016) and Weatherburn et al. (2017) reported how Chemsex provided them with stronger sexual desires towards sexual partners: “Within ten to fifteen minutes of taking it [mephedrone] the world is a prettier place, so everybody becomes more attractive. People have got bigger muscles, bigger penises, their legs are more powerful” (50-year-old gay participant, Weatherburn et al., 2017, p. 205). In Weatherburn et al., many were motivated to use drugs because they provide the automatic urge to engage in sex, by creating or awakening sexual arousal. For instance, several interviewees described the ability for certain drugs to alleviate factors interfering with sexual response (such as pain, physical exhaustion, or apprehension), thus allowing them to engage in sexual activities. For other participants who reported low sexual interest or desire without Chemsex, drugs were an opportunity to increase libido: “I don’t have a sex drive any longer. It’s one of the reasons why I started slamming, […] because when I slam, I get horny” (53-year-old gay man, Weatherburn et al., 2017, p. 204).
Regarding sexual performance, several GBM reported using drugs to increase sexual performance or the duration or frequency of sexual intercourse (Chartier et al., 2009; Deimel et al., 2016; Hunter et al., 2012; Parry et al., 2008; Weatherburn et al., 2017). For gay men who value long sexual sessions especially, Weatherburn et al. (2017) noticed that Chemsex is often construed as a means of increasing sexual stamina, enabling users to either delay ejaculation or reduce the length of their postejaculatory refractory period. About a third of the sample in this study reported Chemsex encounters in which sexual experiences involved numerous men and lasted 24 hours or more.
Lessening Interpersonal and Sexual Inhibitions
The desire to lose inhibitions was explicitly reported as a motivation to practice Chemsex in ten publications (Ahmed et al., 2016; Bourne et al., 2015; Deimel et al., 2016; Harawa et al., 2008; Hunter et al., 2012; Knight et al., 2014; Lyons et al., 2010; Payne et al., 2017; Pollard et al., 2018; Weatherburn et al., 2017). Specifically, participants reported how the drugs allowed them to overcome their inhibitions and related fears (Deimel et al., 2016; Harawa et al., 2008; Hunter et al., 2012; Knight et al., 2014; Lyons et al., 2010; Payne et al., 2017; Pollard et al., 2018; Weatherburn et al., 2017), leading some of them to explore new sexual practices (Bourne et al., 2015; Deimel et al., 2016; Hunter et al., 2012; Lyons et al., 2010; Pollard et al., 2018; Weatherburn et al., 2017). For instance, some participants in Deimel et al. (2016) explained how practicing Chemsex was a way of letting go of self-control and inhibitions, so as to abandon themselves to the sexual experience.
Four articles (Deimel et al., 2016; Harawa et al., 2008; Lyons et al., 2010; Weatherburn et al., 2017) reported how Chemsex-related substances are used to facilitate sexual encounters that might otherwise be avoided, reducing the participants’ fear of rejection. Some methamphetamine users in Lyons et al. (2010) claimed that drugs allow them to approach partners when they would otherwise abstain, thus substance use acting as a tool to be able to experience sexual encounters at all. As Deimel et al. (2016), Harawa et al. (2008), and Weatherburn et al. (2017) note, substance use makes it easier for some to approach partners or to take sexual opportunities that would be challenging or unimaginable without drugs: “If I’m using drugs or alcohol, I might be less inhibited, […] if I see somebody I wanted to be with, I might be more likely to go up to them. [That influence] gives me more courage to say what I want to say.” (HIV-negative African American MSM, Harawa et al., 2008, p. 757).
Furthermore, participants in three studies (Chartier et al., 2009; Hunter et al., 2012; Weatherburn et al., 2017) perceived Chemsex as a solution to reduce concerns about sexual performance and body image. In Hunter et al. (2012) and Weatherburn et al. (2017), several participants expressed perceiving that they were not as “good at sex” (p.204) or as sexy as they wished to be. For them, Chemsex was motivated by a desire to increase sexual confidence, since it resulted in feeling more attractive, being less concerned about fear of rejection, or not fearing underperformance. According to Weatherburn et al. (2017), men who lacked self-confidence or self-esteem might be particularly prone to Chemsex-related substance use. For their participants, drugs served either to remove cognitive barriers to engage in conversation or sexual contact (e.g., perceived high probability of rejection) or to lessen the pain of rejection when it occurs. During focus groups (Hunter et al., 2012), crystal methamphetamine smokers strongly endorsed the positive effect of smoking crystal on inhibitions as making them feel sexier and less afraid of being rejected: “It kind of allows me to get past those fears of rejection, or fears of not being good enough for somebody or not being sexy enough for somebody, because it makes you feel sexy” (gay man, Hunter et al., 2012, p. 4).
Lastly, five qualitative papers (Ahmed et al., 2016; Bourne et al., 2015; Deimel et al., 2016; Hunter et al., 2012; Lyons et al., 2010; Weatherburn et al., 2017) reported how Chemsex was a means to initiate more diverse, extreme, risky, or novel sexual behaviors and fantasies. For instance, Hunter et al. (2012) noted that for some participants who disliked condom use, smoking crystal methamphetamine was a means to give themselves “permission” not to wear one during sex (p. 6). In Weatherburn et al. (2017), all participants described Chemsex as more intense and adventurous than sex while sober. Interviewees usually engaged in a broader range of sexual practices while under the influence, such as group sex, use of toys, bondage and domination, graphic talk, role playing, urolagnia, and fisting.
Data Synthesis of Quantitative Reports
Overall, 17 articles presenting data from 16 studies investigated the relationship between Chemsex and psychological variables. Articles reported data from the United States (n = 10), the United Kingdom (n = 4), Canada (n = 1), France (n = 1), or Australia (n = 1). Three articles were based on the same sample (Grov, Parsons, & Bimbi, 2010; Kelly, Bimbi, Izienicki, & Parsons, 2009a; Kelly, Bimbi, Nanin, Izienicki, & Parsons, 2009b). The samples included participants aged 18 or older (n = 14), or 16 and older (n = 2; Lea et al., 2019; Voisin, Hotton, & Schneider, 2017), from various ethnic backgrounds. Four studies were conducted specifically with HIV-negative participants (Miltz et al., 2019; Noor et al., 2018; Reisner et al., 2009; West & Szymanski, 2008), and 2 specifically with HIV-positive participants (Kelly et al., 2009a; Pufall et al., 2018). Most papers reported convenience sampling data. Of those that did not, Pufall et al. (2018) used a national sampling of HIV-positive MSM accessing care in the UK and weighted their sample to account for the unequal sampling probability at different participating clinics to produce more accurate representative estimates. Grov et al. (2010), Kelly et al. (2009a), and Kelly et al. (2009b) used a street-intercept sampling strategy, which yields similarly representative data to more methodologically complex or rigorous approaches. Voisin et al. (2017) used respondent-driven sampling to provide weighted estimates for the population under study. Sample sizes varied from 66 to 7001 participants. The proportion of GBM engaging in Chemsex varies from 6 to 40.6%; user sub-sample sizes vary from 14 to 1680 (see Table 4 for demographic details of participants, studies aims and characteristics).
Quality Appraisal of Quantitative Studies
While the reports on quantitative studies were generally detailed, the research designs were of varying quality. While participants were recruited from multiple venues, allowing for GBM from various sociodemographic and ethnic backgrounds to be reached, the findings can’t be generalized to all GBM populations (whether from the US or from other cultural contexts). This is the case not only because of the absence of probabilistic sampling, but also given that Chemsex-related practices can only be understood in relation to the specific sociolegal context in which they occur, notably since any sociolegal context influences both the substance market on a general level and specific substance availability at any given time. Moreover, as only a few studies used robust sampling alternatives, possibly due to the implementation complexity and costs of such approaches, the generalisability of Chemsex research is likely limited. Because most research relies on cross-sectional data, the causal relationship between co-occurring phenomenon is impossible to establish. Methodological considerations such as the breadth of topics covered and the variations in Chemsex definitions across studies limit data synthesis and results comparability. However, as users practices depend on evolving substances availability and legal and cultural contexts, among other factors, establishing a strict Chemsex definition might not be possible nor desirable. The small user sub-sample size in most samples suggests that these studies are underpowered, reiterating the need for replication and posing a threat to result validity.
Findings
Six outcome categories were identified: (1) sexual control and self-efficacy; (2) sexual functioning; (3) mental health; (4) attitudes toward substance use; (5) life stressors and internalized stressors; and (6) identification with sexual identities or scenes.
Sexual Control and Self-efficacy
Five studies investigated the association between Chemsex and variables related to sexual control such as sexual compulsivity, feeling of control over sexuality, sexual self-efficacy, and sexual sensation seeking (Grov et al., 2010; Hibbert, Brett, Porcellato, & Hope, 2019; Kashubeck-West & Szymanski, 2008; Kelly et al., 2009b; Melendez-Torres, Hickson, Reid, Weatherburn, & Bonell, 2016). In bivariate analyses, Chemsex is significantly associated with higher sexual compulsivity (Grov et al., 2010; Kelly et al., 2009b) and lower feelings of control over sexual activity, specifically when using crystal methamphetamine; Melendez-Torres et al., 2016). In multivariate analyses, Chemsex is associated with lower sexual self-efficacy (Hibbert et al., 2019; Voisin et al., 2017) and, counterintuitively, lower sexual sensation seeking (Kashubeck-West & Szymanski, 2008).
Sexual Functioning
Three studies investigated relationships between Chemsex and dimensions of sexual function such as sexual dysfunctions, satisfaction, and pleasure (Hibbert et al., 2019; Hirshfield et al., 2010; Melendez-Torres et al., 2016). Hirshfield et al. investigated sexual dysfunction symptoms (low sexual desire, erection problems, performance anxiety, sex being unpleasurable, inability to achieve orgasm, premature ejaculation, and pain during sex) in an Internet sample of 7001 GBM. Those engaging in Chemsex in the previous year were more likely to report at least one sexual dysfunction symptom during that year, with 80% of users reporting sexual dysfunction symptoms. When controlling for demographic and behavioral characteristics, multinomial logistic regression models revealed that the GBM classified as experiencing “high sexual dysfunction and sexual pain” in a latent class model were also more likely to report Chemsex engagement in the past year.
Hibbert et al. (2019) found that those who engaged in any SDU—including but not limited to Chemsex-related substances—reported higher sexual satisfaction in both bivariate and multivariate analyses compared to non-users. Those reporting exclusively Chemsex-related substance use were not different from the other sexualized drug users. Bivariate comparisons revealed no difference of sexual pleasure between users and non-users (Melendez-Torres et al., 2016) or in body satisfaction (Hibbert et al., 2019).
Mental Health Indicators
Six studies investigated associations between Chemsex and mental health indicators such as having ever received a clinical diagnosis of depression or anxiety, psychological distress or depressive symptoms, loneliness, sleep problems, lower life satisfaction, body satisfaction, and problematic alcohol use, binge drinking, and nonsexual drug use (Boone, 2014; Hibbert et al., 2019; Millar, Parsons, Redline, & Duncan, 2019; Mimiaga et al., 2008, 2010; Pufall et al., 2018). Diagnosed depression and/or anxiety in the past were investigated in two studies. Mimiaga et al. (2008) compared those reporting the use of three or more substances concurrently (including at least one Chemsex-related substance) during sex to those reporting the use of two or fewer substances during sex in the past 12 months. Bivariate analyses revealed no difference lifetime depression and/or anxiety diagnostic rates. However, Pufall et al. (2018), reported that those with a diagnosis of depression or anxiety were more likely to report any Chemsex in the past year (39%) compared to those without such diagnosis (25%).
Depressive symptoms were investigated in four studies (Boone, 2014; Hibbert et al., 2019; Mimiaga et al., 2008, 2010), with only one detecting significantly higher current depressive symptoms with stimulant use at least monthly during sex in the past year (Mimiaga et al., 2010). However, in a daily-diary longitudinal study, Boone (2014) observed no significant relationship between weekly symptoms of psychological distress and Chemsex at most recent sexual encounter. Hibbert et al. (2019) also found no significant difference in psychological distress levels between Chemsex substance users and non-users. In a clinical sample, Mimiaga et al. (2008) reported no difference in the experience of depressive symptoms two or more days per week between those reporting the use of three or more substances concurrently (including at least one Chemsex-related substance) during sex and those reporting the use of two or fewer substances. Mimiaga et al. (2010) reported that clinically significant depressive symptoms were associated to having used cocaine, crack cocaine, and/or crystal methamphetamine during sex at least once monthly in the past 12 months.
Hibbert et al. (2019) also investigated loneliness, life satisfaction, and body satisfaction. While loneliness and body satisfaction scores did not significantly differ between users (either SDU or Chemsex) and non-users, those engaging in any SDU (including Chemsex) reported lower life satisfaction in multivariate analyses.
To investigate sleep outcomes associated with Chemsex, Millar et al. (2019) assessed sleep quality, onset, duration, and problems staying awake during wake-time activities. Bivariate comparisons revealed that users suffered from significantly lower sleep quality and showed more sleep-onset difficulties compared to non-users, while there was no difference in sleep duration and alertness during daytime.
Two studies investigated nonsexual substance use problems (Mimiaga et al., 2010; Pufall et al., 2018). In terms of dependence, Mimiaga et al. found a significant association between Chemsex stimulant use at least monthly and non-clinical alcohol dependence, in both bivariate and multivariate models. In terms of problematic alcohol use, no bivariate association between Chemsex and binge drinking frequency were found, nor was Chemsex associated with nonsexual drug use in the past year (Pufall et al., 2018).
Attitudes Toward Substance Use
Two studies investigated attitudes toward substance use and Chemsex substance use during sex (Kashubeck-West & Szymanski, 2008; Lea et al., 2019). In bivariate analyses, Kashubeck-West and Szymanski found that engaging in Chemsex in the past 3 months was significantly associated with higher sexual-enhancing expectancies from substance use, but not from alcohol consumption. Furthermore, users show stronger endorsement of drug use for social and sexual enhancement, higher perceived acceptability of drug use among gay friends, and lower perceptions of drug risk, when compared to non-users.
Life Stressors and Internalized Stressors
Three studies have explored the association between Chemsex and various life stressors (Hibbert et al., 2019; Miltz et al., 2019; Voisin et al., 2017). Voisin et al. surveyed particularly marginalized Black GBM from the South Side of Chicago and adjacent majority Black neighborhoods. They found that any SDU—Chemsex-related substances and others—was significantly associated with exposure to stressful events in both bivariate and multivariate models. Hibbert et al. (2019) found no difference in experiences of sexuality-based discrimination between those reporting Chemsex and those reporting other SDU.
In bivariate analyses, Hibbert et al. (2019) found that both SDU and Chemsex were associated with experiencing or being unsure of having experienced non-consensual sexual contact, but multivariate analyses returned no significant results. Similarly, a study on intimate partner violence showed that lifetime and past-year victimization and perpetration of intimate partner violence were more likely reported by GMB engaging in Chemsex (Miltz et al., 2019). While three studies investigated minority stress, (Boone, 2014; Hibbert et al., 2019; Kashubeck-West & Szymanski, 2008), none yielded significant associations between Chemsex and internalized homophobia and homonegativity as proximal stressors.
Identification with Sexual Scenes
Three studies reported data on Chemsex and identification with specific sexual scenes (Kelly et al., 2009a; Noor et al., 2018; Reisner et al., 2009). In latent class analyses, Noor et al. found that GBM that most likely belonged to a BDSM-Bear-Leather class were also more likely to report engaging in Chemsex. Two studies reported conflicting results regarding the association between self-identifying as barebackers and reporting party or club drugs during sex. Kelly et al. (2009) reported that barebackers were more likely to report engaging in Chemsex. However, Reisner et al. (2009) reported no significant difference in Chemsex participation between self-identified barebackers and non-barebackers.
Discussion
This systematic review provides an overview of the psychological and interpersonal factors associated with Chemsex among GBM. The following points offer a summary of outcomes from both qualitative and quantitative syntheses and recommendations for future research.
Combining Insights from Quantitative and Qualitative Data
Several qualitative reports suggest that Chemsex plays a role as a coping mechanism to help deal with painful emotions or stressful events. In this regard, qualitative studies identified romantic breakups, receiving an HIV diagnosis, the death of a relative, and accumulation of professional or domestic pressures as such events (e.g., Ahmed et al., 2016). Participants considered these difficult events as triggers of Chemsex-related substance use. Similar data can be found in quantitative reports, which have shown that exposure to stressful events was associated with Chemsex. In accordance with a stress and coping framework, Voisin et al. (2017) suggest that exposure to stressful events may lead to poorer health behaviors such as risk-taking related to Chemsex, as well as to non-optimal coping mechanisms such as engaging in Chemsex as self-medication, since Chemsex-related substance use reduces the burden of negative emotional consequences to stressful events. Moreover, qualitative reports strongly support that Chemsex was, for users, a strategy to cope with distressing emotions such as anxiety, loneliness, boredom, feelings of rejection, stigma associated with HIV-positive status, or guilt related to having sex with men (e.g., Amaro, 2016). On an interpersonal level, Chemsex also serves a dual purpose of social enhancement and a pathway to feelings of acceptance, inclusion, emotional closeness, self-esteem, and feeling of attractiveness, via access to social networks and positive social interaction (e.g., Weatherburn et al., 2017). Such sought-after outcomes could, at least partially, explain the mixed results of quantitative studies regarding the association between Chemsex and mental health indicators such as depression and anxiety, as well as the absence of significant associations between Chemsex and internalized stressors such as internalized homophobia or homonegativity—insofar as the practice of Chemsex may also, by proxy, buffer the effects of minority stress or significant negative events.
Regarding sexual functioning, both qualitative and quantitative research provides evidence that Chemsex is associated with sexual pleasure and satisfaction. Participants in qualitative research report that Chemsex was practiced for the purpose of increasing sexual arousal, physical sensations, orgasm intensity, and sexual performance (e.g., Chartier et al., 2009); in quantitative studies, Chemsex users generally present higher scores of sexual satisfaction (Hibbert et al., 2019) and higher sexual-enhancing expectancies (Kashubeck-West & Szymanski, 2008). While quantitative studies report higher prevalence of sexual dysfunctions and pain among Chemsex users (Hirshfield et al., 2010), qualitative data suggests that Chemsex both increased libido among GBM who report low sex drive and alleviated factors inhibiting sexual response, such as pain (Weatherburn et al., 2017). This suggest that Chemsex may serve to overcome inhibiting factors of the sexual response (e.g., pain, body concerns, performance anxiety or fear of rejection)—which may be associated with sexual dysfunctions—by providing favorable and immediate conditions for sexual arousal, performance, and confidence. Combined quantitative and qualitative evidence suggest that Chemsex-related substances are used as a tool to alleviate pre-existing mental and sexual health functioning problems. Further research is needed to determine the causal direction of the relationship between psychological, sexual, or interpersonal distress (e.g., depression, life stressors, sexual dysfunction, sexual pain, hypersexuality, performance anxiety, negative body-image, intimate partner violence) and the practice of Chemsex among GBM.
Regarding sexual control and self-efficacy, some quantitative evidence suggests an association between Chemsex and lower feelings of control over sexual activity (e.g., Melendez-Torres et al., 2016). Qualitative reports offer an explanation by suggesting that for many GBM, the loss of control related to Chemsex is intentional. Some report using Chemsex as a strategy to lower social and sexual inhibitions (e.g. Weatherburn et al., 2017). Others report motives related to alleviate the guilt or the stress of having sex with men, coming out, or having to live the hetero-persona among heavily stigmatized communities (e.g., Jerome & Halkitis, 2009), reinforcing the need to further explore the relationship between internalized homophobia and Chemsex. Therefore, losing control may be part of the appeal of Chemsex itself. Similar associations have been found regarding sexual compulsivity, found to be higher among GBM practicing Chemsex (Grov et al., 2010; Kelly et al., 2009b). Participants in qualitative studies explained how Chemsex-related substances were deliberately used to enhance the frequency and duration of sexual intercourse. In this respect, additional research is needed to explore whether control over sexual activity is positively associated with sexual self-efficacy in Chemsex, especially since disinhibition and hypersexuality induced by Chemsex-related substances may lead to unwanted sexual experiences that users later regret (Ma & Perera, 2016). While Chemsex was credited with improving sexual confidence in qualitative reports (Chartier et al., 2009; Hunter et al., 2012; Weatherburn et al., 2017), quantitative studies have found Chemsex associated with lower sexual self-efficacy (Hibbert et al., 2019; Voisin et al., 2017). These findings are not necessarily contradictory; lower sexual self-efficacy may drive the use of Chemsex-related drugs to boost such efficacy and confidence, and both research designs capture a different facet of the intricacies inherent to Chemsex practices.
Some variables explored in quantitative research pertaining to control (e.g., sexual compulsivity, sexual sensation seeking) were not explicit themes in qualitative reports. However, qualitative studies do suggest that Chemsex-related drugs use is associated with an increase in the urge to engage in sex, sexual arousal, and in frequency of sexual intercourse (e.g., Deimel et al., 2016), which might be indicative of sexual compulsivity. While relationship directionality can be inferred neither from cross-sectional surveys nor qualitative reports to date, current evidence from both bodies of literature does suggest that Chemsex fulfills the satisfaction of compulsive sexual needs (Deimel et al., 2016; Grov et al., 2010; Kelly et al., 2009b; Weatherburn et al., 2017). The only study that has explored sexual sensation seeking in relation to Chemsex found that men with higher levels of sensation seeking reported less substance use during sexual activity (Kashubeck-West & Szymanski, 2008). Maintaining their causal hypothesis that sensation seeking should drive Chemsex-related substance use, the authors suggested that—if Chemsex were to be considered a risk behavior—participants from their sample may not have been risk takers, thus reporting lower Chemsex use despite higher sensation seeking. Another possible explanation is that, if Chemsex indeed helps fulfilling sexual sensation seeking, Chemsex users might feel that this quest is partly satisfied, thus reporting less sexual sensation seeking than non-users from a cross-sectional perspective. Such a hypothesis is coherent with the impact of Chemsex on sexual pleasure and experience enhancement. Repeated-measure designs, such as daily diaries, are promising in uncovering the temporal relationships between Chemsex and these variables.
Lower self-regulation and adverse health behaviors, including substance use, have been associated with poorer sleep (Millar et al., 2019). As for the findings that Chemsex users report poorer sleep quality and more sleep-onset problems than non-users in multivariate analyses, Millar et al. (2019) proposed a mutually reinforcing dynamic. They posit that for some, Chemsex may initially stem from the exhaustion associated with sleep-onset latency and insomnia as a way to remain sufficiently stimulated and awake during sex, while in turn preventing restorative sleep or the establishment of hygienic sleep habits, and negatively affecting circadian cycles and sleep quality. This proposition is convergent with qualitative reports suggesting that Chemsex is sometimes used to counteract tiredness during sexual activities (Weatherburn et al., 2017).
Quantitative and qualitative bodies of literature both converge in documenting attitudes and norms supporting, if not promoting, the practice of Chemsex among GBM. In qualitative research, interviewees feel that Chemsex use is generalized, common, and trendy among GBM (Ahmed et al., 2016), and participants endorse higher perceived acceptability of drug use among their friends in quantitative studies (Lea et al., 2019). Similarly, the harmfulness of Chemsex-related behaviors is minimized by Chemsex users in qualitative reports (Bourne et al., 2015), and quantitative research report lower perception of drug risk among users (Lea et al., 2019).
The two quantitative studies on the association between Chemsex and non-sexual substance use problems in the past year show significant association with stimulant use and likely alcohol dependence (Mimiaga et al., 2010), but not with binge drinking and non-sexual drug use (Pufall et al., 2018). Alcohol problems were not a prominent theme in qualitative studies. More research is needed to understand whether Chemsex is part of a general pattern of substance use among these men or limited to specific sexual encounters. Moreover, quantitative studies revealed that Chemsex is more prevalent in specific scenes, such as the barebacking, BDSM, Bear, or Leather scenes (Kelly et al., 2009a; Noor et al., 2018; Reisner et al., 2009); qualitative studies suggest that Chemsex may provide a sense of belonging and acceptance in Chemsex-related scenes and communities (e.g., Pollard et al., 2018). Future person-centered analyses, such as latent class analyses, are likely to reveal multiple profiles of sexual and non-sexual substance use among GBM, as well as its interplay with specific sexual scenes.
Finally, some studies highlight the importance of considering Chemsex a more complex (and sometimes beneficial) behavior, as opposed to focusing solely on potentially negative outcomes (Melendez-Torres et al., 2016). While Chemsex carries certain health risks, the social contexts in which its associated substances are used and the quality of the sexual experience attributed to Chemsex may provide benefits on physical, psychological and social well-being—particularly for some GBM who may be subjected to stigma outside the Chemsex scene, such as HIV-positive men (Power et al., 2018). This highlights the importance of considering the social motives underlying engagement in Chemsex, notably as a means to develop sexual intimacy and emotional closeness, an opportunity to strengthen belonging to a community (e.g., friends, sexual scenes), or an escape from patterns of marginalization and loneliness. While it seems that Chemsex is associated with positive social outcomes, the causal mechanisms between social connectedness and the practice of Chemsex remain unclear; it is currently difficult to assess whether Chemsex promotes one’s access to community, whether access to community leads to practicing Chemsex, or if a more complex interaction between Chemsex practices and community belonging might be at play (Prestage et al., 2018).
Limitations
This review has some limitations, notably specific to systematic reviews and narrative syntheses (Grant & Booth, 2009). One such limitation stems from how empirical results are reported in publications—since primary data are rarely available, our interpretation relies on the data presented by the authors and their interpretations. While triangulation and mixed-methods at the level of primary research are more common, these strategies are less customary at the review level and are mostly done in intervention evaluation (Harden & Thomas, 2005; Noyes et al., 2019). While no clear international consensus exists on the degree to which quantitative and qualitative components can be integrated, we remained as rigorous as possible in the analytic process to preserve the integrity of the findings and avoid conflation of misinterpretations. Finally, since this review only includes articles published in English, it may be subject to language or cultural biases.
Conclusion
Despite these limitations, this systematic review summarizes key psychological and interpersonal motivations and factors associated with Chemsex-related substance use before or during sex among GBM. Further research is needed to replicate current findings and explore new hypotheses across multiple GBM sociodemographic groups and cultural contexts from adequately powered prospective studies (such as daily diaries), based on the best sampling methods available for hidden and hard-to-reach populations. Chemsex-related substance users are not a homogeneous group; developing a better, more accurate understanding of the motivational, psychological and interpersonal profiles of GBM who practice Chemsex is instrumental in developing and improving further prevention and intervention programs.
References
Abdulrahim, D. W., Moncrieff, C., & Bowden-Jones, M. O. (2016). Club drug use among lesbian, gay, bisexual and trans (LGBT) people. London: Novel Psychoactive Treatment UK Network (NEPTUNE).
Aguinaldo, J. P., & Myers, T. (2008). A discursive approach to disinhibition theory: The normalization of unsafe sex among gay men. Qualitative Health Research, 18(2), 167–181. https://doi.org/10.1177/1049732307311362.
Ahmed, A. K., Weatherburn, P., Reid, D., Hickson, F., Torres-Rueda, S., Steinberg, P., & Bourne, A. (2016). Social norms related to combining drugs and sex (“chemsex”) among gay men in South London. International Journal of Drug Policy, 38, 29–35. https://doi.org/10.1016/j.drugpo.2016.10.007.
Amaro, Z. (2016). Taking chances for love? Reflections on love, risk, and harm reduction in a gay slamming subculture. Contemporary Drug Problems, 43(3), 216–227. https://doi.org/10.1177/0091450916658295.
Blais, M., Otis, J., Lambert, G., Cox, J., & Haig, T. (2018). Consommation de substances en contexte sexuel chez des hommes gbHSH de Montréal : 2009–2016. Drogues, santé et société, 17(2). https://doi.org/10.7202/1062117ar
Boone, M. R. (2014). Internalized homophobia, psychological distress, and resilience as correlates of substance use during sexual encounters in young adult black men who have sex with men. ProQuest Information & Learning.
Bourne, A., Reid, D., Hickson, F., Torres-Rueda, S., Steinberg, P., & Weatherburn, P. (2015). “Chemsex” and harm reduction need among gay men in South London. International Journal of Drug Policy, 26(12), 1171–1176. https://doi.org/10.1016/j.drugpo.2015.07.013.
Bourne, A., Reid, D., Hickson, F., Torres Rueda, S., & Weatherburn, P. (2014). The Chemsex Study: Drug use in sexual settings among gay and bisexual men in Lambeth, Southwark and Lewisham. London: Sigma Research.
Chartier, M., Araneta, A., Duca, L., McGlynn, L. M., Gore-Felton, C., Goldblum, P., & Koopman, C. (2009). Personal values and meaning in the use of methamphetamine among HIV-positive men who have sex with men. Qualitative Health Research, 19(4), 504–518. https://doi.org/10.1177/1049732309333018.
Critical Appraisal Skills Programme. (2018). CASP Qualitative Checklist. Retrieved from https://casp-uk.net/wp-content/uploads/2018/03/CASP-Qualitative-Checklist-2018_fillable_form.pdf.
Daskalopoulou, M., Rodger, A. J., Phillips, A. N., Sherr, L., Elford, J., McDonnell, J., … Johnson, A. M. (2017). Condomless sex in HIV-diagnosed men who have sex with men in the UK: Prevalence, correlates, and implications for HIV transmission. Sexually Transmitted Infections, 93(8), 590–598. https://doi.org/10.1136/sextrans-2016-053029.
Deacon, R. M., Mooney-Somers, J., Treloar, C., & Maher, L. (2013). At the intersection of marginalised identities: Lesbian, gay, bisexual and transgender people’s experiences of injecting drug use and hepatitis C seroconversion. Health and Social Care in the Community, 21(4), 402–410. https://doi.org/10.1111/hsc.12026.
Dearing, N., & Flew, S. (2015). P211|Msm the cost of having a good time? A survey about sex, drugs and losing control. Sexually Transmitted Infections, 91, A86–A86.
Deimel, D., Stover, H., Hosselbarth, S., Dichtl, A., Graf, N., & Gebhardt, V. (2016). Drug use and health behaviour among German men who have sex with men: Results of a qualitative, multi-centre study. Harm Reduction Journal, 13(1), 36. https://doi.org/10.1186/s12954-016-0125-y.
Drückler, S., Van Rooijen, M. S., & De Vries, H. J. C. (2018). Chemsex among men who have sex with men: A sexualized drug use survey among clients of the sexually transmitted infection outpatient clinic and users of a gay dating app in Amsterdam, the Netherlands. Sexually Transmitted Diseases, 45(5), 325–331. https://doi.org/10.1097/OLQ.0000000000000753.
Edmundson, C., Heinsbroek, E., Glass, R., Hope, V., Mohammed, H., White, M., & Desai, M. (2018). Sexualised drug use in the United Kingdom (UK): A review of the literature. International Journal of Drug Policy, 55, 131–148. https://doi.org/10.1016/j.drugpo.2018.02.002.
Frankis, J., Flowers, P., McDaid, L., & Bourne, A. (2018). Low levels of chemsex among men who have sex with men, but high levels of risk among men who engage in chemsex: Analysis of a cross-sectional online survey across four countries. Sexual Health, 15(2), 144–150. https://doi.org/10.1071/SH17159.
Giorgetti, R., Tagliabracci, A., Schifano, F., Zaami, S., Marinelli, E., & Busardò, F. P. (2017). When “chems” meet sex: A rising phenomenon called “chemsex”. Current Neuropharmacology, 15(5), 762–770. https://doi.org/10.2174/1570159X15666161117151148.
Glynn, R. W., Byrne, N., O’Dea, S., Shanley, A., Codd, M., Keenan, E., … Clarke, S. (2018). Chemsex, risk behaviours and sexually transmitted infections among men who have sex with men in Dublin, Ireland. International Journal of Drug Policy, 52, 9–15. https://doi.org/10.1016/j.drugpo.2017.10.008.
González-Baeza, A., Dolengevich-Segal, H., Pérez-Valero, I., Cabello, A., Téllez, M. J., Sanz, J., … Bisbal, O. (2018). Sexualized Drug Use (Chemsex) Is associated with high-risk sexual behaviors and sexually transmitted infections in HIV-positive men who have sex with men: Data from the U-SEX GESIDA 9416 study. AIDS Patient Care and STDs, 32(3), 112–118. https://doi.org/10.1089/apc.2017.0263.
Gordon, K. S., Edelman, E. J., Justice, A. C., Fiellin, D. A., Akgün, K., Crystal, S., … Bryant, K. J. (2017). Minority men who have sex with men demonstrate increased risk for HIV transmission. AIDS and Behavior, 21(5), 1497–1510. https://doi.org/10.1007/s10461-016-1590-8.
Grant, M. J., & Booth, A. (2009). A typology of reviews: An analysis of 14 review types and associated methodologies. Health Information & Libraries Journal, 26(2), 91–108. https://doi.org/10.1111/j.1471-1842.2009.00848.x.
Grov, C., Parsons, J. T., & Bimbi, D. S. (2010). Sexual compulsivity and sexual risk in gay and bisexual men. Archives of Sexual Behavior, 39(4), 940–949. https://doi.org/10.1007/s10508-009-9483-9.
Hammoud, M. A., Bourne, A., Maher, L., Jin, F., Haire, B., Lea, T., … Prestage, G. (2018). Intensive sex partying with gamma-hydroxybutyrate: Factors associated with using gamma-hydroxybutyrate for chemsex among Australian gay and bisexual men-results from the Flux Study. Sexual Health, 15(2), 123–134. https://doi.org/10.1071/SH17146.
Harawa, N. T., Williams, J. K., Ramamurthi, H. C., Manago, C., Avina, S., & Jones, M. (2008). Sexual behavior, sexual identity, and substance abuse among low-income bisexual and non-gay-identifying African American men who have sex with men. Archives of Sexual Behavior, 37(5), 748–762. https://doi.org/10.1007/s10508-008-9361-x.
Harden, A., & Thomas, J. (2005). Methodological issues in combining diverse study types in systematic reviews. International Journal of Social Research Methodology, 8(3), 257–271. https://doi.org/10.1080/13645570500155078.
Hegazi, A., Lee, M. J., Whittaker, W., Green, S., Simms, R., Cutts, R., … Pakianathan, M. R. (2017). Chemsex and the city: Sexualised substance use in gay bisexual and other men who have sex with men attending sexual health clinics. International Journal of STDs and AIDS, 28(4), 362–366. https://doi.org/10.1177/0956462416651229.
Heinsbroek, E., Glass, R., Edmundson, C., Hope, V., & Desai, M. (2018). Patterns of injecting and non-injecting drug use by sexual behaviour in people who inject drugs attending services in England, Wales and Northern Ireland, 2013–2016. International Journal of Drug Policy, 55, 215–221. https://doi.org/10.1016/j.drugpo.2018.02.017.
Hibbert, M. P., Brett, C. E., Porcellato, L. A., & Hope, V. D. (2019). Psychosocial and sexual characteristics associated with sexualised drug use and chemsex among men who have sex with men (MSM) in the UK. Sexually Transmitted Infections, 95(5), 342–350. https://doi.org/10.1136/sextrans-2018-053933.
Hirshfield, S., Chiasson, M. A., Wagmiller, R. L., Jr., Remien, R. H., Humberstone, M., Scheinmann, R., & Grov, C. (2010). Sexual dysfunction in an internet sample of US men who have sex with men. Journal of Sexual Medicine, 7(9), 3104–3114. https://doi.org/10.1111/j.1743-6109.2009.01636.x.
Hong, Q. N., Pluye, P., Bujold, M., & Wassef, M. (2017). Convergent and sequential synthesis designs: Implications for conducting and reporting systematic reviews of qualitative and quantitative evidence. Systematic Reviews, 6(1), 61. https://doi.org/10.1186/s13643-017-0454-2.
Hunter, C., Strike, C., Barnaby, L., Busch, A., Marshall, C., Shepherd, S., & Hopkins, S. (2012). Reducing widespread pipe sharing and risky sex among crystal methamphetamine smokers in Toronto: Do safer smoking kits have a potential role to play? Harm Reduction Journal. https://doi.org/10.1186/1477-7517-9-9.
Jerome, R. C., & Halkitis, P. N. (2009). Stigmatization, stress, and the search for belonging in Black men who have sex with men who use methamphetamine. Journal of Black Psychology, 35(3), 343–365. https://doi.org/10.1177/0095798409333620.
Kashubeck-West, S., & Szymanski, D. M. (2008). Risky sexual behavior in gay and bisexual men. The Counseling Psychologist, 36(4), 595–614. https://doi.org/10.1177/0011000007309633.
Kelly, B. C., Bimbi, D. S., Izienicki, H., & Parsons, J. T. (2009a). Stress and coping among HIV-positive barebackers. AIDS and Behavior, 13(4), 792–797. https://doi.org/10.1007/s10461-009-9586-2.
Kelly, B. C., Bimbi, D. S., Nanin, J. E., Izienicki, H., & Parsons, J. T. (2009b). Sexual compulsivity and sexual behaviors among gay and bisexual men and lesbian and bisexual women. Journal of Sex Research, 46(4), 301–308. https://doi.org/10.1080/00224490802666225.
Knight, K. R., Das, M., DeMicco, E., Raiford, J. L., Matheson, T., Shook, A., … Colfax, G. N. (2014). A roadmap for adapting an evidence-based HIV prevention intervention: Personal cognitive counseling (PCC) for episodic substance-using men who have sex with men. Prevention Science, 15(3), 364–375. https://doi.org/10.1007/s11121-013-0364-z.
Knight, R., Karamouzian, M., Carson, A., Edward, J., Carrieri, P., Shoveller, J., … Fast, D. (2019). Interventions to address substance use and sexual risk among gay, bisexual and other men who have sex with men who use methamphetamine: A systematic review. Drug and Alcohol Dependence, 194, 410–429. https://doi.org/10.1016/j.drugalcdep.2018.09.023.
Knoops, L., Bakker, I., van Bodegom, R., & Zantkuijl, P. (2015). Tina and slamming: MSM, crystal meth use and injecting drugs in a sexual setting. Amsterdam: Mainline & SOA AIDS.
Lawn, W., Aldridge, A., Xia, R., & Winstock, A. R. (2019). Substance-linked sex in heterosexual, homosexual, and bisexual men and women: An online, cross-sectional “global drug survey” report. Journal of Sexual Medicine, 16(5), 721–732. https://doi.org/10.1016/j.jsxm.2019.02.018.
Lea, T., Hammoud, M., Bourne, A., Maher, L., Jin, F., Haire, B., … Prestage, G. (2019). Attitudes and perceived social norms toward drug use among gay and bisexual men in Australia. Substance Use and Misuse, 54(6), 944–954. https://doi.org/10.1080/10826084.2018.1552302.
Liu, S., & Detels, R. (2012). Recreational drug use: An emerging concern among venue-based male sex workers in China. Sexually Transmitted Diseases, 39(4), 251–252. https://doi.org/10.1097/OLQ.0b013e31824a0903.
Lyons, T., Chandra, G., Goldstein, J., & Ostrow, D. G. (2010). Breaking the bond between stimulant use and risky sex: A qualitative study. Substance Abuse, 31(4), 224–230. https://doi.org/10.1080/08897077.2010.514240.
Ma, R., & Perera, S. (2016). Safer ‘chemsex’: GPs’ role in harm reduction for emerging forms of recreational drug use. British Journal of General Practice, 66(642), 4–5. https://doi.org/10.3399/bjgp16X683029.
Maxwell, S., Shahmanesh, M., & Gafos, M. (2019). Chemsex behaviours among men who have sex with men: A systematic review of the literature. International Journal of Drug Policy, 63, 74–89. https://doi.org/10.1016/j.drugpo.2018.11.014.
McCready, K. C., & Halkitis, P. N. (2008). HIV serostatus disclosure to sexual partners among HIV-positive methamphetamine-using gay, bisexual, and other men who have sex with men. AIDS Education and Prevention, 20(1), 15–29. https://doi.org/10.1521/aeap.2008.20.1.15.
Melendez-Torres, G. J., & Bourne, A. (2016). Illicit drug use and its association with sexual risk behaviour among MSM: More questions than answers? Current Opinion in Infectious Diseases, 29(1), 58–63. https://doi.org/10.1097/QCO.0000000000000234.
Melendez-Torres, G. J., Bourne, A., Hickson, F., Reid, D., & Weatherburn, P. (2018). Correlates and subgroups of injecting drug use in UK gay and bisexual men: Findings from the 2014 Gay Men’s Sex Survey. Drug and Alcohol Dependence, 187, 292–295. https://doi.org/10.1016/j.drugalcdep.2018.03.014.
Melendez-Torres, G. J., Hickson, F., Reid, D., Weatherburn, P., & Bonell, C. (2016). Nested event-level case–control study of drug use and sexual outcomes in multipartner encounters reported by men who have sex with men. AIDS and Behavior, 20(3), 646–654. https://doi.org/10.1007/s10461-015-1127-6.
Millar, B. M., Parsons, J. T., Redline, S., & Duncan, D. T. (2019). What’s sleep got to do with it?: Sleep health and sexual risk-taking among men who have sex with men. AIDS and Behavior, 23(3), 572–579. https://doi.org/10.1007/s10461-018-2288-x.
Miltz, A. R., Lampe, F. C., Bacchus, L. J., McCormack, S., Dunn, D., White, E., … McOwan, A. (2019). Intimate partner violence, depression, and sexual behaviour among gay, bisexual and other men who have sex with men in the PROUD Trial. BMC Public Health, 19(1), 431. https://doi.org/10.1186/s12889-019-6757-6.
Mimiaga, M. J., Reisner, S. L., Fontaine, Y. M., Bland, S. E., Driscoll, M. A., Isenberg, D., … Mayer, K. H. (2010). Walking the line: stimulant use during sex and HIV risk behavior among Black urban MSM. Drug and Alcohol Dependence, 110(1–2), 30–37. https://doi.org/10.1016/j.drugalcdep.2010.01.017.
Mimiaga, M. J., Reisner, S. L., Vanderwarker, R., Gaucher, M. J., O’Connor, C. A., Medeiros, M. S., & Safren, S. A. (2008). Polysubstance use and HIV/STD risk behavior among Massachusetts men who have sex with men accessing Department of Public Health mobile van services: Implications for intervention development. AIDS Patient Care and STDs, 22(9), 745–751. https://doi.org/10.1089/apc.2007.0243.
Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. PLoS Medicine, 6(7), e1000097. https://doi.org/10.1093/ptj/89.9.873.
Noor, S. W., Adam, B. D., Brennan, D. J., Moskowitz, D. A., Gardner, S., & Hart, T. A. (2018). Scenes as micro-cultures: examining heterogeneity of HIV risk behavior among gay, bisexual, and other men who have sex with men in Toronto, Canada. Archives of Sexual Behavior, 47(1), 309–321. https://doi.org/10.1007/s10508-017-0948-y.
Noyes, J., Booth, A., Flemming, K., Garside, R., Harden, A., … Thomas, J. (2018). Cochrane Qualitative and Implementation Methods Group guidance series-paper 3: Methods for assessing methodological limitations, data extraction and synthesis, and confidence in synthesized qualitative findings. Journal of Clinical Epidemiology, 97, 49–58. https://doi.org/10.1016/j.jclinepi.2017.06.020.
Noyes, J., Booth, A., Moore, G., Flemming, K., Tuncalp, O., & Shakibazadeh, E. (2019). Synthesising quantitative and qualitative evidence to inform guidelines on complex interventions: Clarifying the purposes, designs and outlining some methods. BMJ Global Health, 4(Suppl. 1), e000893. https://doi.org/10.1136/bmjgh-2018-000893.
Noyes, J., Popay, J., Pearson, A., Hannes, K., & Booth, A. (2008). Qualitative research and Cochrane reviews. In J. Higgins & S. Green (Eds.), Cochrane handbook for systematic reviews of interventions (pp. 571–591). Chichester, England: Wiley-Blackwell. https://doi.org/10.1002/9780470712184.ch20.
Ottaway, Z., Finnerty, F., Amlani, A., Pinto-Sander, N., Szanyi, J., & Richardson, D. (2017a). Men who have sex with men diagnosed with a sexually transmitted infection are significantly more likely to engage in sexualised drug use. International Journal of STDs and AIDS, 28(1), 91–93. https://doi.org/10.1177/0956462416666753.
Ottaway, Z., Finnerty, F., Buckingham, T., & Richardson, D. (2017b). Increasing rates of reported chemsex/sexualised recreational drug use in men who have sex with men attending for postexposure prophylaxis for sexual exposure. Sexually Transmitted Infections, 93(1), 31. https://doi.org/10.1136/sextrans-2016-052877.
Page, E. E., & Nelson, M. (2016). Hepatitis C and sex. Clinical Medicine, 16(2), 189–192. https://doi.org/10.7861/clinmedicine.16-2-189.
Pakianathan, M. R., Lee, M. J., Kelly, B., & Hegazi, A. (2016). How to assess gay, bisexual and other men who have sex with men for chemsex. Sexually Transmitted Infections, 92(8), 568–570. https://doi.org/10.1136/sextrans-2015-052405.
Pakianathan, M., Whittaker, W., Lee, M. J., Avery, J., Green, S., Nathan, B., & Hegazi, A. (2018). Chemsex and new HIV diagnosis in gay, bisexual and other men who have sex with men attending sexual health clinics. HIV Medicine, 19(7), 485–490. https://doi.org/10.1111/hiv.12629.
Parry, C., Petersen, P., Dewing, S., Carney, T., Needle, R., Kroeger, K., & Treger, L. (2008). Rapid assessment of drug-related HIV risk among men who have sex with men in three South African cities. Drug and Alcohol Dependence, 95(1–2), 45–53. https://doi.org/10.1016/j.drugalcdep.2007.12.005.
Payne, L., Lawrence, D., Soni, S., Llewellyn, C., & Dean, G. (2017). Investigating factors for increased gonorrhoea re-infection in men who have sex with men attending a genitourinary clinic: A qualitative study. International Journal of STDs and AIDS, 28(9), 858–863. https://doi.org/10.1177/0956462416677916.
Pollard, A., Nadarzynski, T., & Llewellyn, C. (2018). Syndemics of stigma, minority-stress, maladaptive coping, risk environments and littoral spaces among men who have sex with men using chemsex. Culture, Health & Sexuality, 20(4), 411–427. https://doi.org/10.1080/13691058.2017.1350751.
Power, J., Mikołajczak, G., Bourne, A., Brown, G., Leonard, W., Lyons, A., … Lucke, J. (2018). Sex, drugs and social connectedness: Wellbeing among HIV-positive gay and bisexual men who use party-and-play drugs. Sexual Health, 15(2), 135–143. https://doi.org/10.1071/SH17151.
Prestage, G., Hammoud, M., Jin, F., Degenhardt, L., Bourne, A., & Maher, L. (2018). Mental health, drug use and sexual risk behavior among gay and bisexual men. International Journal of Drug Policy, 55, 169–179. https://doi.org/10.1016/j.drugpo.2018.01.020.
Pufall, E. L., Kall, M., Shahmanesh, M., Nardone, A., Gilson, R., Delpech, V., … Positive Voices Study Group. (2018). Sexualized drug use (‘chemsex’) and high-risk sexual behaviours in HIV-positive men who have sex with men. HIV Medicine, 19(4), 261–270. https://doi.org/10.1111/hiv.12574.
Reisner, S. L., Mimiaga, M. J., Case, P., Johnson, C. V., Safren, S. A., & Mayer, K. H. (2009). Predictors of identifying as a barebacker among high-risk New England HIV seronegative men who have sex with men. Journal of Urban Health, 86(2), 250–262. https://doi.org/10.1007/s11524-008-9333-4.
Rosińska, M., Gios, L., Nöstlinger, C., Berghe, W. V., Marcus, U., Schink, S., … Velicko, I. (2018). Prevalence of drug use during sex amongst MSM in Europe: Results from a multi-site bio-behavioural survey. International Journal of Drug Policy, 55, 231–241. https://doi.org/10.1016/j.drugpo.2018.01.002.
Schmidt, A. J., Bourne, A., Weatherburn, P., Reid, D., Marcus, U., & Hickson, F. (2016). Illicit drug use among gay and bisexual men in 44 cities: Findings from the European MSM Internet Survey (EMIS). International Journal of Drug Policy, 38, 4–12. https://doi.org/10.1016/j.drugpo.2016.09.007.
Sewell, J., Cambiano, V., Miltz, A., Speakman, A., Lampe, F. C., Phillips, A., … Clarke, A. (2018). Changes in recreational drug use, drug use associated with chemsex, and HIV-related behaviours, among HIV-negative men who have sex with men in London and Brighton, 2013–2016. Sexually Transmitted Infections, 94(7), 494–501. https://doi.org/10.1136/sextrans-2017-053439.
Sewell, J., Miltz, A., Lampe, F. C., Cambiano, V., Speakman, A., Phillips, A. N., … Clarke, A. (2017). Poly drug use, chemsex drug use, and associations with sexual risk behaviour in HIV-negative men who have sex with men attending sexual health clinics. International Journal of Drug Policy, 43, 33–43. https://doi.org/10.1016/j.drugpo.2017.01.001.
Taggart, T. C., Rodriguez-Seijas, C., Dyar, C., Elliott, J. C., Thompson, R. G., Jr., Hasin, D. S., & Eaton, N. R. (2019). Sexual orientation and sex-related substance use: The unexplored role of bisexuality. Behaviour Research and Therapy, 115, 55–63.
Thomas, J., & Harden, A. (2008). Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Medical Research Methodology, 8, 45. https://doi.org/10.1186/1471-2288-8-45.
Thomas, J., Sutclife, K., Harden, A., Oakley, A., Oliver, S., … Kavanagh, J. (2003). Children and healthy eating: A systematic review of barriers and facilitators. London: EPPI Centre. Retrieved from http://eppi.ioe.ac.uk/cms/Portals/0/PDF%20reviews%20and%20summaries/FinalReport-webV2.pdf?ver=2010-11-25-155950-117.
Tomkins, A., George, R., & Kliner, M. (2019). Sexualised drug taking among men who have sex with men: A systematic review. Perspect Public Health, 139(1), 23–33. https://doi.org/10.1177/1757913918778872.
Voisin, D. R., Hotton, A. L., & Schneider, J. A. (2017). The relationship between life stressors and drug and sexual behaviors among a population-based sample of young Black men who have sex with men in Chicago. AIDS Care, 29(5), 545–551. https://doi.org/10.1080/09540121.2016.1224303.
Weatherburn, P., Hickson, F., Reid, D., Torres-Rueda, S., & Bourne, A. (2017). Motivations and values associated with combining sex and illicit drugs (chemsex) among gay men in South London: Findings from a qualitative study. Sexually Transmitted Infections, 93(3), 203–206. https://doi.org/10.1136/sextrans-2016-052695.
Wu, H.-H., Shen, Y.-T., Chiou, C.-S., Fang, C.-T., & Lo, Y.-C. (2019). Shigellosis outbreak among MSM living with HIV: A case–control study in Taiwan, 2015–2016. Sexually Transmitted Infections, 95(1), 67–70. https://doi.org/10.1136/sextrans-2017-053410.
Acknowledgements
This research was funded by the Faculty of Social Sciences of the Université du Québec à Montréal.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest has been declared by the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lafortune, D., Blais, M., Miller, G. et al. Psychological and Interpersonal Factors Associated with Sexualized Drug Use Among Men Who Have Sex with Men: A Mixed-Methods Systematic Review. Arch Sex Behav 50, 427–460 (2021). https://doi.org/10.1007/s10508-020-01741-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10508-020-01741-8