Abstract
The HIV epidemic in Latin America is highly concentrated in men who have sex with men (MSM). In the United States, multiple co-occurring psychosocial conditions have been shown to act as intertwined epidemics to potentiate HIV transmission among MSM. To date, no study has examined the role of syndemics and condomless sex among MSM in Latin America. In 2012, an online survey was conducted among members of the largest social/sexual networking website for MSM in Latin America. Participants were asked about demographics, sexual behaviors, HIV/STI diagnoses, and psychosocial well-being, including depression, suicidal ideation, hazardous alcohol use, hard drug use during sex, history of childhood/adolescent sexual abuse, intimate partner violence, and sexual compulsivity. Multivariable logistic generalized estimation equations were used to assess the relationship of syndemic factors and (1) engagement in higher risk condomless anal sex and (2) self-report of prior HIV diagnosis. Among 24,274 survey respondents, 74.6 % of the sample had at least one syndemic factor. In an additive model, syndemics were associated with increased odds of higher risk condomless anal sex, ranging from adjusted odds ratio of 1.31 (95 % CI 1.20, 1.43) for one syndemic factor to 4.06 (95 % CI 3.25, 5.09) for 6/7 syndemic factors. Similarly, syndemics were associated with increased odds of HIV infection (p < .0001). This study provides initial evidence that intertwined syndemics increase HIV risk behavior and HIV infection among MSM in Latin America. In the Latin American context, comprehensive HIV prevention interventions for MSM should be developed and tested that simultaneously address co-occurring psychosocial conditions and HIV risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
While overall HIV incidence is stabilizing in many countries, concentrated epidemics have emerged and persist among men who have sex with men (MSM) across the world (De Cock, Jaffe, & Curran, 2012; Sullivan et al., 2009). Estimates of HIV prevalence among MSM vary widely between countries in part due to surveillance gaps that result from persistent stigmatization of MSM and criminalization of same-sex behavior (Beyrer et al., 2012). This discrimination also contributes to high levels of distress and numerous other health problems among MSM including depression and psychosocial conditions (Berlan, Corliss, Field, Goodman, & Austin, 2010; Cochran & Mays, 2000; Cochran, Mays & Sullivan, 2003; Gilman et al., 2001; King et al., 2008; Meyer, 2003; Mimiaga et al., 2009; Safren & Heimberg, 1999), many of which have been found to promote sexual risk taking (Chesney et al., 2003; Koblin et al., 2003; Reisner et al., 2009; Rogers et al., 2003). Research has shown that several of these psychosocial problems co-occur (Cochran, Ackerman, Mays, & Ross, 2004; Hirshfield, Remien, Humberstone, Walavalkar, & Chiasson, 2004; Marshal et al., 2008; Stall et al., 2001), acting as intertwined epidemics or “syndemics” that promote HIV transmission among MSM (Mustanski, Garofalo, Herrick, & Donenberg, 2007; Stall et al., 2003).
Syndemic frameworks highlight how the clustering of and interactions between multiple epidemics adversely affect health (Singer et al., 2006), particularly among socioeconomically disadvantaged populations (Singer & Clair, 2003). This framework was originally developed by Singer after observing how adverse social and structural conditions gave rise to the co-occurring epidemics of substance abuse, violence, and AIDS among poor urban communities (i.e., the “SAVA” syndemic) (Singer, 1994). Unlike traditional epidemiologic approaches to investigating the causes and consequences of distinct diseases, research that adopts a syndemic perspective tends to focus on how co-occurring epidemics adversely affect the health of particularly marginalized populations (Farmer, 1999).
Studies applying the syndemic framework to U.S. MSM have found that having increasing numbers of interacting psychosocial conditions is associated with increased odds of sexual risk taking and prevalent HIV (Mustanski et al., 2007; Stall et al., 2003). In addition to the co-occurring conditions of depression, victimization, and substance abuse (Brennan et al., 2012; Ferlatte, Hottes, Trussler, & Marchand, 2014; Meyer, 2003; Safren, Reisner, Herrick, Mimiaga, & Stall, 2010; Stall, Friedman, & Catania, 2008), recent research has also confirmed the role of sexual compulsivity, stimulant abuse, intimate partner violence (IPV), stress, and childhood sexual abuse in contributing to syndemics among MSM (Dyer et al., 2012; Herrick et al., 2013; Mimiaga et al., 2009; Parsons, Grov, & Golub, 2012).
Despite this expansion of syndemic research, however, few studies have been conducted outside of North America (Biello, Colby, Closson, & Mimiaga, 2014a; Jie, Ciyong, Xueqing, Hui, & Lingyao, 2012; Santos et al., 2014; Wim, Christiana, & Marie, 2014; Yu et al., 2013), and few studies to date have assessed the existence of syndemics in large, multinational samples of MSM. As a region, Latin America has one of the greatest burdens of HIV among MSM in the world (Beyrer et al., 2012), but to our knowledge, no study has investigated the role of syndemics in potentiating the HIV epidemic in Latin America. Syndemics may be particularly salient for MSM in this context, where there remain high levels of stigma, discrimination, and violence against MSM that can be internalized and manifest as one or more psychosocial conditions (Ferlatte et al., 2014; Geibel, Tun, Tapsoba, & Kellerman, 2010).
The high rates of discrimination and lifelong adversity that promote syndemics among MSM (Herrick et al., 2013) likely prevent many men from openly identifying as MSM or attending traditional MSM venues (e.g., public sex environments, gay bars/dance clubs), making them more likely to be excluded from epidemiologic surveys (Marcus, Schmidt, Hamouda, & Bochow, 2009). Due to their anonymity, internet-based social networking sites have proliferated and are now the most popular venues for MSM to meet male sexual partners in many settings (Curioso, Blas, Nodell, Alva, & Kurth, 2007). Globally, it is estimated that up to six million MSM use the Internet for finding sexual partners (Liau, Millett, & Marks, 2006). The increasing affordability and accessibility of the Internet make it a promising new avenue for HIV research and prevention among MSM and other sexual minority populations (Chiasson et al., 2006) particularly in understudied international settings (Swendeman & Rotheram-Borus, 2010).
While several large online studies have recently described the sexual behaviors and health of MSM in North America, Europe, and parts of Asia (Marcus, Hickson, Weatherburn, & Schmidt, 2012; Stupiansky et al., 2010; Wang et al., 2012), no studies have assessed syndemics using multinational Internet data in Latin America. Thus, we drew from a large online survey with the objective of examining syndemic production among men who are active members of a popular MSM social networking website in Latin America. Based on the MSM syndemics literature, we hypothesized that the intertwined epidemics of psychosocial health conditions would be positively associated with condomless anal sex and HIV prevalence in this large multinational internet sample of MSM. Given the persistent HIV risk among MSM internationally and the increasing prominence of internet-based social and sexual networking tools (Beyrer et al., 2012; Swendeman & Rotherman-Borus, 2010), the findings from this study may help inform large-scale HIV prevention interventions for MSM online.
Method
Participants and Procedure
Data for this analysis came from an anonymous online survey of members (18 years of age or older) of a social/sexual networking site for MSM in Latin America, Spain, and Portugal. The survey aimed to collected data on sexual health and psychosocial risk among MSM using the internet for sexual networking. Details of this study have been published elsewhere (Biello et al., 2014b). In brief, an email with a link to the survey was sent to nearly 643,000 active members (i.e., had logged on in past 90 days). Approximately 36,500 initiated the survey (83.3 % in Latin America, 5.0 % in Spain, and 11.7 % in Portugal). For this analysis, we limited the analytic sample to respondents who reported living in any Spanish- and Portuguese-speaking country in Latin America, male sex at birth and currently identified as a male, as well as those who reported having had sex with another man in the past year (N = 24,274). For participants who did not complete the full survey, data were analyzed for all questions that were answered. As such, the total number of respondents is given for each of the measures reported. The study was approved by the Institutional Review Board at the Fenway Institute at Fenway Health.
Sample characteristics are described in Table 1. The average age of respondents (N = 24,274) was 30.4 years (SD = 9.1). Most participants had completed university or post-graduate education (79.0 %), considered themselves to be middle class (75.2 %) and lived in urban areas (96.1 %). Additionally, while most identified as being homosexual or gay (77.4 %), a substantial proportion (19.0 %) identified as bisexual.
Measures
Respondents completed an anonymous survey to characterize sexual health, including sexual practices, substance use, relevant psychological concerns, factors associated with the use of condoms, sexual identity, and general health issues. The measures used for this analysis are described below.
Demographic Variables
Respondents were asked about their age, sexual orientation (coded as heterosexual/straight, bisexual, homosexual/gay, and unsure/questioning/other), education (coded as less than university vs. university/post-graduate), and income/class (no income, low income/lower class, middle income/middle class, and high income/upper class). Additionally, respondents were asked to self-select whether they lived in an urban or rural area.
Sexual Risk Variables
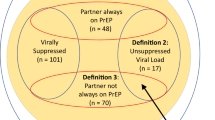
Condomless anal sex with a cisgender male or transgender partner of a different or unknown HIV status (herein, higher risk condomless anal sex) in the past 3 months was assessed by asking respondents a series of questions regarding gender of sexual partners, type of sex, condom use, and HIV status of the partner. Additionally, respondents were asked to report whether they had ever been diagnosed with HIV.
Syndemic Psychosocial Variables
The syndemic condition was assessed by creating count scores for the number of the seven psychosocial factors endorsed—depression, suicidal ideation, alcohol abuse/dependence, hard drug use during sex, childhood sexual abuse, IPV, and sexual compulsivity. Many of these measures have been widely used in other samples of MSM, and their reliability and validity have been empirically examined across diverse samples (Ballester-Arnal, Gomez-Martinez, Llario, & Salmeron-Sanchez, 2013; Ruiz-Grosso et al., 2012; Saitz, Lepore, Sullivan, Amaro, & Samet, 1999), supporting the appropriateness of their use in the current study.
Depressive symptoms were assessed using the CES-D 10—a shortened version of the 20-item Center for Epidemiologic Studies Depression Scale, a validated survey of clinically significant distress as a marker for clinical depression (Cronbach’s alpha = 0.78) (Andresen, Malmgren, Carter, & Patrick, 1994). The 10-items were scored on a 4-point Likert scale from 0 to 3, with a score of 10 or greater suggestive of clinical depression. Suicidal ideation was assessed by responses to the question, “in the past month, did you think about suicide?” Hazardous alcohol use was determined using the 4-item validated CAGE scale (Ewing, 1984; Fiellin, Reid & O’Connor, 2000). A score of 2 or greater is suggestive of hazardous alcohol use. Hard drug use during sex was assessed by asking respondents whether they had used any drugs during sex in the past 3 months. Hard drugs were considered stimulants (e.g., crystal meth, speed, crack, and cocaine), ecstasy, gamma hydroxybutyrate, ketamine, or heroin. Stimulant use during sex was endorsed by 4 % of the sample and ecstasy use by 2 %. Use of all other hard drugs during sex was endorsed by less than 1 % of the sample. Childhood or adolescent sexual abuse (CSA) was determined by asking respondents a series of questions regarding unwanted or forced sexual touching or intercourse with a person when 17 years old or younger. IPV was assessed by asking participants whether they had experienced any emotional, physical, or sexual violence by a male partner in the past 5 years (Greenwood et al., 2002). Finally, sexual compulsivity was assessed using the sexual compulsivity scale, which assesses the extent that the respondent’s sexual desires get in the way of their life (Kalichman & Rompa, 1995). This scale has been validated in Spanish-speaking populations (Ballester-Arnal et al., 2013). The 10-items were scored on a 4-point Likert scale from 1 to 4, with a score of 24 or greater suggestive of sexual compulsivity.
The syndemic measure was calculated as a count score based on the number of psychosocial health problems each respondent reported, resulting in scores ranging from 0 to 7. The score was calculated as the sum of the 7 items weighted by the number of non-missing items. If more than 2 items were missing, the scale was not scored. The weighted scores were then rounded to the nearest integer to simplify interpretation of the measure.
Statistical Analysis
Percentages were calculated for each measure overall and by higher risk condomless anal sex and reported in Table 1. In order to examine whether the interconnection of these psychosocial health problems magnifies the odds of engaging in higher risk condomless anal sex and HIV prevalence, we calculated frequencies and percentages of each outcome by the syndemic count score. Additionally, using generalized estimating equations (GEE) to account for clustering by country, we performed unadjusted and multivariable logistic regression adjusted for the demographic measures to examine the associations between the syndemic count score (treated as both nominal and ordinal) and higher risk condomless anal sex and self-reported HIV status. We also assessed interactions between syndemic psychosocial conditions and demographic measures within final models to examine potential moderation in the associations between the syndemic count score and each outcome. Intraclass correlations (ICCs) were estimated for each psychosocial health problem and the higher risk condomless anal sex outcome using generalized linear mixed models (random intercept only) and the equation: \( \rho = \frac{{\text{variance}_{country - level} }}{{\text{variance}_{country - level} + {\raise0.7ex\hbox{${\pi^{2} }$} \!\mathord{\left/ {\vphantom {{\pi^{2} } 3}}\right.\kern-0pt} \!\lower0.7ex\hbox{$3$}}}} \) (Fitzmaurice, Laird, & Ware, 2004). The ICCs are as follows: depression = .016, suicidal ideation = .023, hazardous alcohol use = .038, any hard drug use in context of sex = .039, childhood/adolescent sexual abuse = .015, intimate partner violence = .003, sexually compulsive = .010, higher risk condomless anal sex = .008, and HIV diagnosis = .065.
Results
Overall, psychosocial health problems were common (Table 1). Nearly one-third (28.0 %) screened in for clinical depression and 9.2 % reported thinking about suicide in the past month. Sixteen percent of the sample reported hazardous alcohol use (15.8 %), and 5.3 % reported any hard drug use in the context of sex in the past 30 days. Forty-two percent reported experiencing CSA and over a third (35.7 %) reported experiencing IPV in the past 5 years. Finally, 15.2 % met the cutoff for sexual compulsivity. In bivariate analyses, each psychosocial factor was associated with all other factors (p values < 0.001) (Table 2).
Syndemics: The Interconnection of Psychosocial Health Problems
Overall, 25.4 % of the sample did not have any of the seven psychosocial health problems. Nearly a third (31.9 %) had one, 22.9 % had two, 10.6 % had three, 6.4 % had four, 2.1 % had five, 0.7 % had six, and 0.1 % had seven.
Higher risk condomless anal sex with a male or transgender partner in the past 3 months was reported by 20.4 % of the sample (Table 1). In unadjusted and adjusted models, the number of psychosocial health problems experienced was positively associated with engaging in higher risk condomless anal sex (p < .0001) (Table 3). For example, individuals with one syndemic factor had 1.3 times the odds of engaging in higher risk condomless anal sex compared to those with none of the factors. Additionally, individuals with 6 or 7 syndemic factors had 4.1 times the odds of engaging in higher risk condomless anal sex compared to those with none of the factors (Table 3). Additionally, as described in Table 3, a statistical trend was detected. Specifically, every unit increase in number of psychosocial health problems is associated with a 30 % increase in odds of higher risk condomless anal sex (p < .0001).
Similarly, in unadjusted and adjusted models, the number of psychosocial health problems experienced was associated with self-reported HIV infection (Table 3). The additive syndemic measure resulted in a greater odds of reporting being infected with HIV (p < .0001). Individuals with one syndemic factor had 1.2 times the odds of reporting an HIV diagnosis compared to those with none of the factors. Additionally, individuals with 6 or 7 syndemic factors had 2.5 times the odds of reporting an HIV diagnosis compared to those with none of the factors (Table 3). Lastly, when treated as continuous, every unit increase in number of psychosocial health problems is associated with a 25 % increase in odds of reporting being HIV-infected (p < .0001) (Table 3).
No significant interactions were identified in our analyses, indicating that there are no meaningful differences in the operation of this syndemic on higher risk condomless anal sex or self-reported HIV diagnosis by age, sexual orientation, education, income/class, or type of living area.
Discussion
In this study, we found that an increasing number of syndemic factors was associated with both self-reported prevalent HIV infection and higher risk condomless anal sex across 17 countries in Latin America. To our knowledge, this study is the first to investigate associations between multiple co-occurring psychosocial health problems and HIV among MSM in Latin America. To date, most evidence of syndemic psychosocial factors and HIV risk among MSM has arisen from the United States, and research from non-Western settings is only slowly emerging (Biello et al., 2014a, b; Jie et al., 2012; Santos et al., 2014; Yu et al., 2013). A previous analysis of a multinational sample of MSM suggested the presence of syndemics across widely diverse samples, with a similar effect noted in countries outside of North America and Western Europe compared to the entire sample (Santos et al., 2014). However, this study did not consider Latin America specifically, and overall had a considerably smaller sample size than the present study (Ayala et al., 2013). The unique contribution of the current study showing similar associations to that of other samples of MSM and representing one of the largest samples of MSM in Latin America provides additional support to the interpretation that intertwined syndemic conditions influence sexual risk behavior in greater magnitude, which ultimately leads to more HIV transmission events among these MSM. On the other hand, since the temporality of data collected is unknown (i.e., this is a cross-sectional assessment), our findings may also support the alternative interpretation that an HIV diagnosis may lead to, for example, increased stress, fear, stigma, and other outcomes which then foster syndemic onset, such as depression, substance use, etc. Further research using longitudinal methods, as seen in a recent study of U.S. MSM (Mimiaga et al., 2015), will need to be conducted with MSM in this region of the world in order to make a more conclusive interpretation.
These findings may offer further support for the need for HIV prevention interventions to adopt holistic approaches that simultaneously address multiple co-occurring psychosocial conditions (Blashill, Perry & Safren, 2011; Safren, Blashill & O’Cleirigh, 2011; Safren et al., 2010). Public health programs or policies to prevent excess burden of risk for HIV among MSM should address each of these conditions, and, ideally, the social, political, and economic factors that contribute to the conditions and tie them together (Singer & Clair, 2003). The original syndemic theory considered the clustering of conditions, such as urbanicity and poverty, as contributing to HIV risk (Singer, 1994). Although this sample overwhelmingly reported being in the middle class, there may be other structural factors that behave in a similar way to enhance syndemic conditions. For example, these men could be socially marginalized in their countries of origin, which could exacerbate the syndemic condition in a similar fashion to the marginalizing effects of poverty. While homophobia, discrimination, and violence may vary across the countries included in this analysis (De Boni, Veloso, & Grinsztein, 2014), these factors likely still influence the impact of co-occurring psychosocial problems. Future research should measure and consider the context in which MSM live, including experiences of discrimination, and how this affects syndemics, to better understand how structural interventions, such as policy changes, may alter and ultimately improve this relationship.
In addition to potentiating HIV risk behaviors, the high prevalence of co-occurring psychosocial conditions among MSM in the United States may result in reduced efficacy of traditional HIV prevention interventions (Safren et al., 2010), and even extrapolate to other cultural contexts. It is likely that the syndemic conditions that influence sexual risk taking among MSM could also interact to moderate the effects of HIV prevention interventions over time (Halkitis, Wolitski, & Millet, 2013). Some evidence of this was provided by findings from Project EXPLORE, a behavioral intervention study to prevent HIV among high-risk MSM in six U.S. cities (Koblin, Chesney, & Coates, 2004): those reporting childhood sexual abuse were less likely to benefit from the intervention and were more likely to acquire HIV (Mimiaga et al., 2009).
While recent evidence has shown that early initiation of antiretroviral therapy (ART) reduces onward transmission of HIV, poor adherence to ART reduces efficacy. Psychosocial factors, such as depression and substance use, have been shown to be associated with reduced adherence to ART (Gonzalez, Batchelder, Psaros, & Safren, 2011). Moreover, pre-exposure prophylaxis (PrEP), a once-daily pill taken by HIV-uninfected individuals to prevent HIV infection, has been shown to be efficacious against HIV acquisition among MSM (Grant et al., 2010). However, as with ART, adherence is essential for the intervention to remain efficacious. As with adherence to ART, adherence to PrEP is affected by psychosocial factors, such as substance use—as evidenced by a large PrEP trial in East Africa (Haberer et al., 2013). It is likely that multiple co-occurring psychosocial conditions further impair adherence, which would reduce the benefits of these biomedical prevention modalities. These factors could therefore contribute to increased HIV incidence and prevalence among individuals with multiple syndemic conditions. Future research should consider the impact of syndemic factors on biomedical efficacy, and HIV prevention interventions should consider multifaceted approaches to address these factors.
The results of this study must be considered in the context of some limitations. This study was cross-sectional, and it is not possible to know if individuals acquired their HIV infection prior to onset of some of the psychosocial conditions, such as depression or substance use. The study was an online survey, and data were collected via self-report. The data are therefore subject to biases, such as the ability to recall some events. It is possible that individuals did not feel comfortable disclosing their HIV status. HIV status could also be underreported if individuals had not undergone HIV testing recently. Participants were recruited for this study though an online social and sexual networking website for MSM, and thus represent a unique population. Individuals may be at differential HIV risk compared to MSM who are not members of this site, and may have considerably different characteristics compared to non-members. As has been seen in previous online studies, there was some missing data and attrition over the course of the survey; however, levels of missing data were comparable to those of other online surveys of MSM (Rosenberger et al., 2011; Sullivan et al., 2011). Some of the measures used, such as childhood sexual abuse and IPV, have not been validated in the Latin American context and, therefore, may result in measurement error. Finally, this is a very heterogeneous sample. Respondents were pooled from vastly different countries, which may be problematic. Our analysis accounted for correlations within countries, and although further research is needed into how syndemics operate within the different cultural contexts in which study participants reside, our findings suggest that syndemics may be detrimental to the health of MSM in many contexts. Despite these limitations, this is the first study of syndemics on a large, multi-country scale in Latin America and used a novel data collection method, paving the way for future research among MSM using the Internet for social networking purposes.
The results of this study support growing evidence that multiple syndemic psychosocial factors, working in concert with each other, negatively impact HIV risk above and beyond that of individual psychosocial factors, suggesting that HIV prevention interventions for MSM in Latin America may be most efficacious if they consider and simultaneously address co-occurring psychosocial conditions. In the Latin American context, in which homosexuality remains stigmatized, additional work needs to be done to develop comprehensive prevention interventions, which may mitigate the effect of syndemic conditions on HIV sexual risk.
References
Andresen, E. M., Malmgren, J. A., Carter, W. B., & Patrick, D. L. (1994). Screening for depression in well older adults: Evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). American Journal of Preventive Medicine, 10, 77–84.
Ayala, G., Makofane, K., Santos, G.M., Beck, J., Do, T. D., Herbert, P., et al. (2013). Access to basic HIV-related services and PrEP acceptability among men who have sex with men worldwide: Barriers, facilitators, and implications for combination prevention. Journal of Sexually Transmitted Diseases. doi:10.1155/2013/953123.
Ballester-Arnal, R., Gomez-Martinez, S., Llario, M. D., & Salmeron-Sanchez, P. (2013). Sexual compulsivity scale: Adaptation and validation in the Spanish population. Journal of Sex and Marital Therapy, 39, 526–540.
Berlan, E. D., Corliss, H. L., Field, A. E., Goodman, E., & Austin, S. B. (2010). Sexual orientation and bullying among adolescents in the Growing Up Today Study. Journal of Adolescent Health, 46, 366–371.
Beyrer, C., Baral, S. D., van Griensven, F., Goodreau, S. M., Chariyalertsak, S., Wirtz, A. L., & Brookmeyer, R. (2012). Global epidemiology of HIV infection in men who have sex with men. Lancet, 380, 367–377.
Biello, K., Colby, C., Closson, E., & Mimiaga, M. J. (2014a). The syndemic condition of psychosocial problems and HIV risk among male sex workers in Ho Chi Minh City, Vietnam. AIDS and Behavior, 18, 1267–1271.
Biello, K., Rosenberger, J., Novak, D., Robertson, A., Mayer, K., & Mimiaga, M. (2014b). Epidemiology of sexual health in the virtual environment: A multinational online survey of Spanish- and Portuguese-speaking men who use an internet sexual networking site. AIDS and Behavior, 18, 1675–1685.
Blashill, A. J., Perry, N., & Safren, S. A. (2011). Mental health: A focus on stress, coping, and mental illness as it relates to treatment retention, adherence, and other health outcomes. Current HIV/AIDS Reports, 8, 215–222.
Brennan, J., Kuhns, L. M., Johnson, A. K., Belzer, M., Wilson, E. C., Garofalo, R., & Adolescent Medicine Trials Network for HIV/AIDS Interventions. (2012). Syndemic theory and HIV-related risk among young transgender women: The role of multiple, co-occurring health problems and social marginalization. American Journal of Public Health, 102, 1751–1757.
Chesney, M. A., Koblin, B. A., Barresi, P. J., Husnik, M. J., Celum, C. L., Colfax, G., et al. (2003). An individually tailored intervention for HIV prevention: Baseline data from the EXPLORE Study. American Journal of Public Health, 93, 933–938.
Chiasson, M. A., Parsons, J. T., Tesoriero, J. M., Carballo-Dieguez, A., Hirshfield, S., & Remien, R. H. (2006). HIV behavioral research online. Journal of Urban Health, 8, 73–85.
Cochran, S. D., Ackerman, D., Mays, V. M., & Ross, M. W. (2004). Prevalence of non-medical drug use and dependence among homosexually active men and women in the US population. Addiction, 99, 989–998.
Cochran, S. D., & Mays, V. M. (2000). Lifetime prevalence of suicide symptoms and affective disorders among men reporting same-sex sexual partners: Results from NHANES III. American Journal of Public Health, 90, 573–578.
Cochran, S. D., Mays, V. M., & Sullivan, J. G. (2003). Prevalence of mental disorders, psychological distress, and mental health services use among lesbian, gay, and bisexual adults in the United States. Journal of Consulting and Clinical Psychology, 71, 53–61.
Curioso, W. H., Blas, M. M., Nodell, B., Alva, I. E., & Kurth, A. E. (2007). Opportunities for providing web-based interventions to prevent sexually transmitted infections in Peru. PLoS Medicine, 4, e11.
De Boni, R., Veloso, V. G., & Grinsztein, B. (2014). Epidemiology of HIV in Latin America and the Caribbean. Current Opinion in HIV and AIDS, 9, 192–198.
De Cock, K. M., Jaffe, H. W., & Curran, J. W. (2012). The evolving epidemiology of HIV/AIDS. AIDS, 26, 1205–1213.
Dyer, T. P., Shoptaw, S., Guadamuz, T. E., Plankey, M., Kao, U., Ostrow, D., et al. (2012). Application of syndemic theory to black men who have sex with men in the Multicenter AIDS Cohort Study. Journal of Urban Health, 89, 697–708.
Ewing, J. A. (1984). Detecting alcoholism: The CAGE questionnaire. Journal of the American Medical Association, 252, 1905–1907.
Farmer, P. (1999). Infections and inequality: The modern plagues. Berkeley, CA: University of California Press.
Ferlatte, O., Hottes, T. S., Trussler, T., & Marchand, R. (2014). Evidence of a syndemic among young Canadian gay and bisexual men: Uncovering the associations between anti-gay experiences, psychosocial issues, and HIV risk. AIDS and Behavior, 18, 1256–1263.
Fiellin, D. A., Reid, M. C., & O’Connor, P. G. (2000). Screening for alcohol problems in primary care: A systematic review. Archives of Internal Medicine, 160, 1977–1989.
Fitzmaurice, G. M., Laird, N. M., & Ware, J. H. (2004). Applied longitudinal analysis. Hoboken, NJ: Wiley.
Geibel, S., Tun, W., Tapsoba, P., & Kellerman, S. (2010). HIV vulnerability of men who have sex with men in developing countries: Horizons studies, 2001-2008. Public Health Reports, 125, 316–324.
Gilman, S. E., Cochran, S. D., Mays, V. M., Hughes, M., Ostrow, D., & Kessler, R. C. (2001). Risk of psychiatric disorders among individuals reporting same-sex sexual partners in the National Comorbidity Survey. American Journal of Public Health, 91, 933–939.
Gonzalez, J. S., Batchelder, A. W., Psaros, C., & Safren, S. A. (2011). Depression and HIV/AIDS treatment nonadherence: A review and meta-analysis. Journal of Acquired Immune Deficiency Syndrome, 58, 181–187.
Grant R. M., Lama, J. R., Anderson, P. L., McMahan, V., Liu, A.Y., Vargas, L., et al. (2010). Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. New England Journal of Medicine, 363, 2587–2599.
Greenwood, G. L., Relf, M. V., Huang, B., Pollack, L. M., Canchola, J. A., & Cantania, J. A. (2002). Battering victimization among a probability-based sample of men who have sex with men. American Journal of Public Health, 92, 1964–1969.
Haberer, J. E., Baeten, J. M., Campbell, J., Wangisi, J., Katabira, E., Ronald, A., et al. (2013). Adherence to antiretroviral prophylaxis for HIV prevention: A substudy cohort within a clinical trial of serodiscordant couples in East Africa. PLOS Medicine, 10, e1001511. doi:10.1371/journal.pmed.1001511.
Halkitis, P. N., Wolitski, R. J., & Millett, G. A. (2013). A holistic approach to addressing HIV infection disparities in gay, bisexual, and other men who have sex with men. American Psychologist, 68, 261–273.
Herrick, A. L., Lim, S. H., Plankey, M. W., Chmiel, J. S., Guadamuz, T. E., Kao, U., et al. (2013). Adversity and syndemic production among men participating in the Multicenter AIDS Cohort Study: A life-course approach. American Journal of Public Health, 103, 79–85.
Hirshfield, S., Remien, R. H., Humberstone, M., Walavalkar, I., & Chiasson, M. A. (2004). Substance use and high-risk sex among men who have sex with men: A national online study in the USA. AIDS Care, 16, 1036–1047.
Jie, W., Ciyong, L., Xueqing, D., Hui, W., & Lingyao, H. (2012). A syndemic of psychosocial problems places the MSM (men who have sex with men) population at greater risk of HIV infection. PLoS ONE, 7, e32312.
Kalichman, S. C., & Rompa, D. (1995). Sexual sensation seeking and sexual compulsivity scales: Validity, and predicting HIV risk behavior. Journal of Personality Assessment, 65, 586–601.
King, M., Semlyen, J., Tai, S. S., Killaspy, H., Osborn, D., Popelyuk, D., & Nazarethm, I. (2008). A systematic review of mental disorder, suicide, and deliberate self harm in lesbian, gay and bisexual people. BMC Psychiatry, 8, 70.
Koblin, B. A., Chesney, M. A., & Coates, T. (2004). Effects of a behavioural intervention to reduce acquisition of HIV infection among men who have sex with men: The EXPLORE randomized controlled study. Lancet, 364, 41–50.
Koblin, B. A., Chesney, M. A., Husnik, M. J., Bozeman, S., Celum, C. L., Buchbinder, S., et al. (2003). High-risk behaviors among men who have sex with men in six US cities: Baseline data from the EXPLORE Study. American Journal of Public Health, 93, 926–932.
Liau, A., Millett, G., & Marks, G. (2006). Meta-analytic examination of online sex-seeking and sexual risk behavior among men who have sex with men. Sexually Transmitted Diseases, 33, 576–584.
Marcus, U., Hickson, F., Weatherburn, P., & Schmidt, A. J. (2012). Prevalence of HIV among MSM in Europe: Comparison of self-reported diagnoses from a large scale internet survey and existing national estimates. BMC Public Health, 12, 978.
Marcus, U., Schmidt, A. J., Hamouda, O., & Bochow, M. (2009). Estimating the regional distribution of men who have sex with men (MSM) based on Internet surveys. BMC Public Health, 9, 180.
Marshal, M. P., Friedman, M. S., Stall, R., King, K. M., Miles, J., Gold, M. A., et al. (2008). Sexual orientation and adolescent substance use: A meta-analysis and methodological review. Addiction, 103, 546–556.
Meyer, I. H. (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129, 674–697.
Mimiaga, M. J., Noonan, E., Donnell, D., Safren, S. A., Koenan, K. C., Gortmaker, S., et al. (2009). Childhood sexual abuse is highly associated with HIV risk-taking behavior and infection among MSM in the EXPLORE Study. Journal of Acquired Immune Deficiency Syndrome, 51, 340–348.
Mimiaga, M. J., O’Cleirigh, C., Biello, K.B., Robertson, A.M., Safren, S. A., Coates, T. J., et al. (2015). The effect of psychosocial syndemic production on 4-year HIV incidence and risk behavior in a large cohort of sexually active men who have sex with men. Journal of Acquired Immune Deficiency Syndrome, 68, 329–336.
Mustanski, B., Garofalo, R., Herrick, A., & Donenberg, G. (2007). Psychosocial health problems increase risk for HIV among urban young men who have sex with men: Preliminary evidence of a syndemic in need of attention. Annals of Behavioral Medicine, 34, 37–45.
Parsons, J. T., Grov, C., & Golub, S. A. (2012). Sexual compulsivity, co-occurring psychosocial health problems, and HIV risk among gay and bisexual men: Further evidence of a syndemic. American Journal of Public Health, 102, 156–162.
Reisner, S. L., Mimiaga, M. J., Skeer, M., Bright, D., Cranston, K., Isenberg, D., et al. (2009). Clinically significant depressive symptoms as a risk factor for HIV infection among black MSM in Massachusetts. AIDS and Behavior, 13, 798–810.
Rogers, G., Curry, M., Oddy, J., Pratt, N., Beilby, J., & Wilkinson, D. (2003). Depressive disorders and unprotected casual anal sex among Australian homosexually active men in primary care. HIV Medicine, 4, 271–275.
Rosenberger, J. G., Reece, M., Schick, V., Herbenick, D., Novak, D. S., Van Der Pol, B., & Fortenberry, J. D. (2011). Sexual behaviors and situational characteristics of most recent male-partnered sexual event among gay and bisexually identified men in the United States. Journal of Sexual Medicine, 8, 3040–3050.
Ruiz-Grosso, P., Loret de Mola, C., Vega-Dienstmaier, J. M., Arevalo, J. M., Chavez, K., Vilela, A., & Huapaya, J. (2012). Validation of the Spanish Center for Epidemiological Studies Depression and Zung Self-Rating Depression Scales: A comparative validation study. PLoS One, 7(10), e45413.
Safren, S. A., Blashill, A. J., & O’Cleirigh, C. M. (2011). Promoting the sexual health of MSM in the context of comorbid mental health problems. AIDS and Behavior, 15, S30–S34.
Safren, S. A., & Heimberg, R. G. (1999). Depression, hopelessness, suicidality, and related factors in sexual minority and heterosexual adolescents. Journal of Consulting and Clinical Psychology, 67, 859–866.
Safren, S. A., Reisner, S. L., Herrick, A., Mimiaga, M. J., & Stall, R. D. (2010). Mental health and HIV risk in men who have sex with men. Journal of Acquired Immune Deficiency Syndrome, 55(Suppl. 2), S74–S77.
Saitz, R., Lepore, M. F., Sullivan, L. M., Amaro, H., & Samet, J. H. (1999). Alcohol abuse and dependence in Latinos living in the United States: Validation of the CAGE (4M) questions. Archives of Internal Medicine, 159, 718–724.
Santos, G. M., Do, T., Beck, J., Makofane, K., Arreola, S., Pyun, T., et al. (2014). Syndemic conditions associated with increased HIV risk in a global sample of men who have sex with men. Sexually Transmitted Infections, 90, 250–253.
Singer, M. (1994). AIDS and the health crisis of the U.S. urban poor: The perspective of critical medical anthropology. Social Science and Medicine, 39, 931–948.
Singer, M., & Clair, S. (2003). Syndemics and public health: Reconceptualizing disease in bio-social context. Medical Anthropology Quarterly, 17, 423–441.
Singer, M. C., Erickson, P. I., Badiane, L., Diaz, R., Ortiz, D., Abraham, T., & Nicolaysen, A. M. (2006). Syndemics, sex and the city: Understanding sexually transmitted diseases in social and cultural context. Social Science and Medicine, 63, 2010–2021.
Stall, R., Friedman, M., & Catania, J. (2008). Interacting epidemics and gay men’s health: A theory of syndemic production among urban gay men. In R. J. Wolitski, R. Stall, & R. O. Valdiserri (Eds.), Unequal opportunity: Health disparities affecting gay and bisexual men in the United States (pp. 251–274). New York, NY: Oxford University Press.
Stall, R., Mills, T. C., Williamson, J., Hart, T., Greenwood, G., Paul, J., et al. (2003). Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. American Journal of Public Health, 93, 939–942.
Stall, R., Paul, J. P., Greenwood, G., Pollack, L. M., Bein, E., Crosby, G. M., et al. (2001). Alcohol use, drug use and alcohol-related problems among men who have sex with men: The Urban Men’s Health Study. Addiction, 96, 1589–1601.
Stupiansky, N. W., Rosenberger, J. G., Schick, V., Herbenick, D., Novak, D. S., & Reece, M. (2010). Factors associated with sexually transmitted infection testing among men who utilize an internet-based men who have sex with men community. AIDS Patient Care and STDS, 24, 713–717.
Sullivan, P. S., Hamouda, O., Delpech, V., Geduld, J. E., Prejean, J., Semaille, C., et al. (2009). Reemergence of the HIV epidemic among men who have sex with men in North America, Western Europe, and Australia, 1996-2005. Annals of Epidemiology, 19, 423–431.
Sullivan, P. S., Khosropour, C. M., Luisi, N., Amsden, M., Coggia, T., Wingood, G. M., & DiClemente, R. J. (2011). Bias in online recruitment and retention of racial and ethnic minority men who have sex with men. Journal of Medical Internet Research, 13, e38.
Swendeman, D., & Rotheram-Borus, M. J. (2010). Innovation in sexually transmitted disease and HIV prevention: Internet and mobile phone delivery vehicles for global diffusion. Current Opinion in Psychiatry, 23, 139–144.
Wang, L., Wang, L., Norris, J. L., Li, D. M., Guo, W., Ding, Z. W., & Wang, N. (2012). HIV prevalence and influencing factors analysis of sentinel surveillance among men who have sex with men in China, 2003–2011. Chinese Medical Journal, 125, 1857–1861.
Wim, V. B., Christiana, N., & Marie, L. (2014). Syndemic and other risk factors for unprotected anal intercourse among an online sample of Belgian HIV negative men who have sex with men. AIDS and Behavior, 18, 50–58.
Yu, F., Nehl, E. J., Zheng, T., He, N., Berg, C. J., Lemieux, A. F., et al. (2013). A syndemic including cigarette smoking and sexual risk behaviors among a sample of MSM in Shanghai, China. Drug and Alcohol Dependence, 132, 265–270.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mimiaga, M.J., Biello, K.B., Robertson, A.M. et al. High Prevalence of Multiple Syndemic Conditions Associated with Sexual Risk Behavior and HIV Infection Among a Large Sample of Spanish- and Portuguese-Speaking Men Who Have Sex with Men in Latin America. Arch Sex Behav 44, 1869–1878 (2015). https://doi.org/10.1007/s10508-015-0488-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10508-015-0488-2