Abstract
Evidence suggests over-representation of autism spectrum disorders (ASDs) and behavioral difficulties among people referred for gender issues, but rates of the wish to be the other gender (gender variance) among different neurodevelopmental disorders are unknown. This chart review study explored rates of gender variance as reported by parents on the Child Behavior Checklist (CBCL) in children with different neurodevelopmental disorders: ASD (N = 147, 24 females and 123 males), attention deficit hyperactivity disorder (ADHD; N = 126, 38 females and 88 males), or a medical neurodevelopmental disorder (N = 116, 57 females and 59 males), were compared with two non-referred groups [control sample (N = 165, 61 females and 104 males) and non-referred participants in the CBCL standardization sample (N = 1,605, 754 females and 851 males)]. Significantly greater proportions of participants with ASD (5.4 %) or ADHD (4.8 %) had parent reported gender variance than in the combined medical group (1.7 %) or non-referred comparison groups (0–0.7 %). As compared to non-referred comparisons, participants with ASD were 7.59 times more likely to express gender variance; participants with ADHD were 6.64 times more likely to express gender variance. The medical neurodevelopmental disorder group did not differ from non-referred samples in likelihood to express gender variance. Gender variance was related to elevated emotional symptoms in ADHD, but not in ASD. After accounting for sex ratio differences between the neurodevelopmental disorder and non-referred comparison groups, gender variance occurred equally in females and males.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gender variance in children and adolescents is an area of increased inquiry by both clinicians and researchers with the advent of gender identity clinics in several major academic medical centers as well as increased media coverage (Drescher & Byne, 2012). Terminology in the field of psychiatry is in flux for describing children and youth whose personal sense of gender identity does not conform with their outward biological body (e.g., a boy who wishes to be a girl or vice versa). The term “gender variance” is used in a range of contexts, but in this article we use the term to refer specifically to a child’s wish to be the other gender. There are various approaches for managing the challenges resulting from gender variance, with some clinics working to foster the adaptation and adjustment of the child by providing family support and helping a family problem-solve the complexities of daily life, especially school (Menvielle, 2012). Another approach suggests that because many gender variant children will not choose to transition gender later in life or identify as transgendered, a focus of treatment should be on helping these children become comfortable with their current bodies, if this is possible (as described in Dreger, 2009). Most approaches follow a child over a period of years to monitor gender identity development. When gender variance persists over an extended period of time and reaches clinical levels in which a child experiences significant dysphoria regarding his/her birth gender and a persistent wish to transition to the other gender, medical support for gender transition or puberty suspension may occur through use of hormones and/or hormone blockers (de Vries & Cohen-Kettenis, 2012). The diagnostic terms used to describe this condition are gender identity disorder (GID) (American Psychiatric Association, 2000) or gender dysphoria (American Psychiatric Association, 2013).
Navigating a child’s gender variance is often complex for children and families and the presence of neurodevelopmental disorders makes diagnostics, coping, and adaptation more challenging (Menvielle, 2012). Clinical observations suggest an over-representation of gender variant clients with comorbid autism spectrum disorders (ASD) (Edwards-Leeper & Spack, 2012). de Vries, Noens, Cohen-Kettenis, Van Berckelaer-Onnes, and Doreleijers (2010) reported seven separately published case studies (Gallucci, Hackerman, & Schmidt, 2005; Kraemer, Delsignore, Gundelfinger, Schnyder, & Hepp, 2005; Landen & Rasmussen, 1997; Mukaddes, 2002; Perera, Gadambanathan, & Weerasiri, 2003; Tateno, Tateno, & Saito, 2008; Williams, Allard, & Sears, 1996) representing nine individuals with comorbid gender variance and ASD, and a range of ages and nationalities. Another study indicates increased autistic mannerisms among a sample of gender dysphoric children, as measured by the Social Responsiveness Scale (Constantino & Gruber, 2005) (Wood, 2011, as reported in Zucker, Wood, & VanderLaan, 2014). Increased obsessive interests in gender variant children are also reported in a separate study from the same research group (VanderLaan et al., 2014).
In their own Dutch sample, de Vries et al. (2010) found a significant over-representation of ASD diagnoses among children and adolescents referred for GID/gender dysphoria: 7.8 % of their child and adolescent gender clients met full criteria for an ASD according to DSM IV-TR diagnostics (American Psychiatric Association, 2000). The incidence was higher among adolescents, with 9.4 % of their adolescent gender identity referrals meeting criteria for an ASD. It was noted that such an incidence of comorbid GID/gender dysphoria-related issues and ASD would be unlikely to occur by chance, as the presence of ASD alone among children in the general population is about 0.6–1 % (Baird et al., 2006; Fombonne, 2005). It was also suggested that the actual incidence of ASD in their gender identity clinic sample was probably higher than 7.8 %, noting that some gender client referrals did not complete their ASD diagnostics because of severe behavioral symptoms and that strict adherence to autism cut-offs for diagnostic instruments caused some children with apparent higher functioning ASD to be labeled non-autistic. The comorbidity of GID/gender dysphoria-related issues and ASD occurs in both males and females, as of the eight case studies cited by de Vries et al. (2010) and in their own sample, one-third was female. The proportion of males to females should be considered in the context of ASD gender ratios, where there is an over-representation of males (Center for Disease Control and Prevention [CDC], 2012).
The Child Behavior Checklist (CBCL) (Achenbach & Rescorla, 2001), one of the most commonly used behavioral report inventories for children, has item-level data assessing gender variance. Two major international gender identity clinics have found strong correlations between clinical gender identity diagnosis and endorsement of gender variance-related CBCL items (Cohen-Kettenis, Owen, Kaijser, Bradley, & Zucker, 2003). In 130 children from the Utrecht Gender Clinic in The Netherlands and 358 children from the Toronto Child and Adolescent Gender Identity Clinic, Cohen-Kettenis et al. reported that CBCL gender variance item-level data were sensitive and specific to those children who had been diagnosed with GID by rigorous interview and history taking. Notably, there was a relationship between the raw scores on the gender variance-related CBCL item-level data and the intensity of GID symptoms, with highest raw scores on the CBCL associated with children who met complete criteria for GID and lower CBCL raw scores for children who met partial GID criteria.
Gender variance-related CBCL item-level data have also been utilized in a large twin study examining genetic and environmental influences on cross-gender behaviors (behaviors typical of the other gender). Among approximately 22,500 7 and 10 year-old twins in The Netherlands (Van Beijsterveldt, Hudziak, & Boomsma, 2006), elevations in gender variance-related CBCL data were found to be highly heritable, with significantly greater concordance of these CBCL items in monozygotic twin pairs than in dizygotic twins. It was also noted that there were relationships between gender variance and increased CBCL internalizing and externalizing problems.
Other studies have found that young people with gender variance have increased anxiety (Wallien, Swaab, & Cohen-Kettenis, 2007; Wallien, van Goozen, & Cohen-Kettenis, 2007) as well as other psychiatric and behavioral difficulties (e.g., Coates & Peterson, 1985; Lai, Chiu, Gadow, Gau, & Hwu, 2010; Zucker et al., 2012; Zucker, Owen, Bradley, & Ameeriar, 2002), which has been attributed by some to stress over the lack of congruity between gender identity and body (de Vries, Doreleijers, Steensma, & Cohen-Kettenis, 2011), as well as social pressures against gender nonconformity (Cohen-Kettenis et al., 2003). Issues are more complex in children with comorbid gender variance and ASD, as children with ASD are less aware of social information (American Psychiatric Association, 2000). We have observed clinically that many children who have comorbid ASD and gender variance are less aware of the social prejudice and societal pressures against expression of gender nonconformity. Clinically, they often appear less anxious and dysphoric about their gender variance, at least from the perspective of how others might judge them.
Whereas previous reports have focused on the presence of ASD among child and adolescent gender identity clinic referrals, this study explored rates of gender variance among children with different neurodevelopmental disorders, as well as non-referred comparison groups. Bedard, Zhang, and Zucker (2010) showed high rates of gender identity issues among a small sample of mixed developmental disorders (12.5 %), but sample size limited the opportunity to compare rates among different developmental disabilities. The current study proceeds from the following hypotheses:
-
1.
In agreement with prior findings (de Vries et al., 2010; Gallucci et al., 2005; Kraemer et al., 2005; Landen & Rasmussen, 1997; Mukaddes, 2002; Perera et al., 2003; Tateno et al., 2008; Williams et al., 1996), we expected to find elevated rates of gender variance among children with a confirmed diagnosis of ASD, but not among clinical comparison groups of participants with attention deficit hyperactivity disorder (ADHD), medical neurodevelopmental conditions, or typically developing control children.
-
2.
Given evidence that children and adolescents with gender variance have increased emotional symptoms (e.g., Wallien et al., 2007a), we predicted that, among the participants with neurodevelopmental disorders, rates of emotional symptoms would be elevated for those with gender variance when compared to those without gender variance.
-
3.
The relationship between gender variance and increased anxiety will be less pronounced among children with ASDs compared to those with other neurodevelopmental disorders or typically developing control children.
-
4.
Previous findings have suggested similar ratios of males and females with comorbid GID/gender dysphoria-related issues and ASD (e.g., de Vries et al., 2010) after accounting for underlying over-representation of male gender in ASD. We predicted that, after accounting for underlying sex ratios in the different comparison groups, the ratio of boys to girls with gender variance between the groups of neurodevelopmental disorders and controls will be similar.
Method
Participants
The children and adolescents (ages 6–18 years) who participated in this study were either typically developing controls (N = 165, 61 females and 104 males) or had one of four neurodevelopmental disorders: an ASD (N = 147, 24 females and 123 males), ADHD (N = 126, 38 females and 88 males), or a medical neurodevelopmental disorder [epilepsy (N = 62, 28 females and 34 males) or neurofibromatosis 1 (N = 54, 29 females and 25 males)]. Our clinical samples were obtained from a comprehensive chart review. All available clinical charts from our hospital-based pediatric neuropsychology program database were reviewed by faculty-level clinical neuropsychologists and children and adolescents who met diagnostic criteria for one of the conditions were included in the study. Our hospital serves a broad range of children and families in the Washington, DC metro area. The criteria for inclusion in the study were: (1) initial diagnosis made by the clinical pediatric neuropsychologist (ASD or ADHD) or neurologist (epilepsy or NF1) at the time of the child’s evaluation based on parent and child interview, review of history, gold-standard neuropsychological/diagnostic measures (see below), and DSM-IV-TR (ASD and ADHD) or ICD 9 (epilepsy and NF 1) diagnostic criteria and (2) review of initial clinical diagnosis and diagnostic measure cut-offs by a clinical pediatric neuropsychologist during chart review for this study (e.g., ADOS and ADI scores for ASD and DSM-IV-TR symptom reports for ADHD). All assessments occurred at the time of the original evaluation. No IQ limits were set for exclusion in this study. Children referred by the hospital’s gender identity clinic were not included.
Participants with an ASD were diagnosed based on expert clinical impression using the DSM-IV-TR. All ASD participants met criteria for a “broad ASD” on the Autism Diagnostic Interview (ADI) or Autism Diagnostic Interview-Revised (ADI-R) (Le Couteur et al., 1989; Lord, Rutter, & Le Couteur, 1994) and/or the Autism Diagnostic Observation Schedule (ADOS) (Lord, Rutter, DiLavore, & Risi, 2000) according to the criteria established by the National Institute of Child Health and Human Development (NICHD) and the National Institute on Deafness and Other Communication Disorders (NIDCD) Collaborative Programs for Excellence in Autism (Lainhart et al., 2006).
Participants with ADHD were diagnosed based on a comprehensive diagnostic assessment which included clinical neuropsychological evaluation, family interview, and teacher informant reports by an expert clinical neuropsychologist with 12 years of experience diagnosing ADHD (L.E.K). Participants with ASD or ADHD were excluded if they had a known genetic or neurological disorder. Children with epilepsy were diagnosed by a neurologist based on clinical features, neurologic examination, ictal video-EEG, and high resolution epilepsy protocol MRI. Children with neurofibromatosis 1 (NF1) were diagnosed by a neurologist according to the National Institute of Health (NIH) standard for diagnosing NFI (Gutmann et al., 1997; Wolkenstein, Freche, Zeller, & Revuz, 1996). This NIH NF1 diagnostic standard requires that a child have two or more of the following features: (1) six or more café au lait macules (over 5 mm in greatest diameter in prepubertal individuals and over 15 mm in greatest diameter in postpubertal individuals); (2) two or more neurofibromas of any type or one plexiform neurofibroma; (3) freckling in the axillary or inguinal regions; (4) optic glioma; (5) two or more Lisch nodules; (6) a distinctive osseous lesion such as sphenoid dysplasia or thinning of long bone cortex with or without pseudoarthrosis; (7) a first-degree relative (parent or sibling) with NF1 by the above criteria.
Controls were recruited from the community through announcements in local periodicals and outreach to local children’s programs. They were screened for the presence of neurodevelopmental, psychiatric, learning, and neurologic disorders and none were taking psychiatric medication. Data were obtained as part of an IRB approved protocol and informed consent and/or assent (depending on age) were obtained for all participants. For minors (under 18), parents provided consent, while for adults (age 18), consent was obtained from the participant. In addition to our group of controls, we obtained normative data from the non-referred standardization sample of the CBCL (N = 1,605), including item-level data and basic demographics (Achenbach & Rescorla, 2001). Participant characteristics are shown in Table 1. Compared to controls and the non-referred CBCL group, participants with Epilepsy/NF1 or ADHD were younger (ts > 4.65, ps < .001 and ts > 5.75, p < .001). Compared to local controls and the non-referred CBCL group, there were significantly more males in the ASD group (χ2s > 16.43, p < .001). Similarly, there were more males in the ADHD group than the CBCL non-referred group. There were more females in the Epilepsy/NF1 group than in the local control group (χ2 = 14.30, p < .001). Compared to local controls, all neurodevelopmental groups had lower mean Full Scale IQ (ts > 4.59, ps < .001).
Measures
Cognitive Abilities
Measures of general intellectual functioning were included in this study to provide characterization of the sample, including differences between the groups. Intellectual functioning (Full Scale IQ) was measured with the Wechsler Intelligence Scale for Children-Third Edition, Wechsler Intelligence Scale for Children-Fourth Edition, Wechsler Adult Intelligence Scale–Third Edition, Wechsler Adult Intelligence Scale-Fourth Edition, Wechsler Preschool and Primary Scale of Intelligence-Third Edition, Wechsler Abbreviated Scale of Intelligence, the Differential Ability Scales-Second Edition, or the Reynolds Intellectual Assessment Scales, depending on the age and time period in which the child was assessed. A total of 460 of 554 study participants received IQ measures, representing 83 % of the sample.
Gender Variance
The wish to be the other gender was assessed with the CBCL for ages 6–18 years (Achenbach & Rescorla, 2001). The CBCL is a standardized parent report questionnaire of child/adolescent behavioral and emotional functioning. Gender variance was assessed using CBCL gender variance-related item-level data, a method established in two studies of GID/gender dysphoria in children and adolescents (Cohen-Kettenis et al., 2003; Van Beijsterveldt et al., 2006; Zucker et al., 2012). CBCL item 110, “Wishes to be the opposite sex” was reported by the parents with levels of “never,” “sometimes,” and “often.” Two groups were formed for the analyses: those with no wish to be the other gender (“never”) and those who “sometimes” or “often” wished to be the other gender.
Emotional Symptoms
Emotional symptoms were assessed with the CBCL domain scores, including the Anxious/ Depressed and the Withdrawn/Depressed scales (Achenbach & Rescorla, 2001). Scores are presented as standardized T scores (M = 50, SD = 10), with cutoffs for the borderline clinical range (64 < T < 70) and clinical range (T ≥ 70). Higher scores are indicative of greater problems.
Autism Diagnostics
Autism symptoms were assessed through the ADI/ADI-R and the ADOS. The ADI/ADI-R (Le Couteur et al., 1989; Lord et al., 1994) is a detailed parent or primary caregiver interview of developmental history and autism symptoms. Scores are aggregated into symptom clusters that correspond to DSM-IV-TR criteria for a diagnosis of autism. The ADOS (Lord et al., 2000) is a structured play and conversational interview that includes a series of social demands and other opportunities to elicit symptoms of an ASD. Scores for each domain are tallied and presented as non-standardized raw scores. Higher scores are indicative of more autism symptoms. The ADOS is the most widely-used gold-standard measure of in vivo autism symptomatology.
Data Analysis
To test Hypothesis 1, which examined rates of gender variance among groups, we calculated the percent endorsement of gender variance, as measured by the CBCL, as well as the odds ratios for the presence of gender variance in each neurodevelopmental disorder group as compared to the controls and non-referred subjects in the CBCL standardization sample. We calculated the confidence intervals for these odds ratios, as well as the p-values, indicating the level of significance of the odds ratio differences (Bland & Altman, 2000).
To test Hypothesis 2, two-tailed t-tests were employed to evaluate differences in mean Anxious/Depressed and Withdrawn/Depressed CBCL T-scores between neurodevelopmental disorder participants with and without gender variance. To test Hypothesis 3, which predicted that children with concurrent gender variance and ASD would have fewer reported emotional symptoms than children with gender variance and a non-ASD neurodevelopmental disorder, we conducted a regression with ASD status (ASD or no ASD) and gender variance status (gender variance or no gender variance) as predictors of CBCL anxious/depressed ratings. We included the interaction term of ASD status X gender variance status to explore the possible different relationships with anxiety/depression between the groups. Post-hoc two-tailed t-tests were used to evaluate differences in mean anxious/depressed scores between ASD children with and without gender variance and non-ASD children with neurodevelopmental disorders with and without gender variance.
Hypothesis 4 sought to examine sex ratios of participants with gender variance. As would be expected given the higher incidence of males to females in ASD (CDC, 2012) and ADHD (Arnold, 1996), there were significant differences in overall sex ratios between our groups. In order to be able to compare the sex ratios (percent male to female) of participants with gender variance between the neurodevelopmental disorder and CBCL non-referred groups, we equalized the sex ratios in the CBCL non-referred group to match those of the ASD and ADHD groups. This was accomplished by randomly removing female subjects from the CBCL non-referred group until the sex ratio matched that of our neurodevelopmental disorder groups. Due to the small number of epilepsy and NF1 participants with gender variance (N = 2), they were not included in the analyses. The sex ratios of participants with ADHD were then compared to those of the CBCL non-referred group (with equalized sex ratio) using a two-tailed Lancaster’s mid-p test [a robust method for use with small numbers of subjects (Biddle & Morris, 2011)]. The same test was used to compare the sex ratios of participants with ASD and the CBCL non-referred sample.
Results
Hypothesis 1: Rates of Gender Variance Among Groups
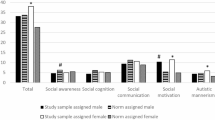
Percentages of endorsement of gender variance among the five groups are shown in Fig. 1. Gender variance was endorsed by parents in 0 % of local control participants, 0.7 % of non-referred control participants from the CBCL standardization sample, 1.7 % of participants with a medical neurodevelopmental condition (epilepsy or NF1), 4.8 % of participants with ADHD, and 5.4 % of participants with an ASD. As compared to CBCL non-referred controls, participants with an ASD were 7.59 times more likely to have gender variance, which was a statistically significant difference (see Table 2). Contrary to our hypothesis, ADHD participants also showed statistically significant elevation of gender variance compared to non-referred controls, with gender variance 6.64 times more likely among children with ADHD than CBCL non-referred controls. Participants with a medical neurodevelopmental disorder (i.e., epilepsy and NF1) did not show greater endorsement of gender variance compared to controls.
Hypothesis 2: Emotional Symptoms in Participants with Gender Variance
As hypothesized, children with comorbid neurodevelopmental disorders and gender variance showed increased rates of emotional symptoms as compared to children with neurodevelopmental disorders and no reported gender variance (see Table 3). Children with comorbid neurodevelopmental disorders and gender variance had borderline clinical range levels of parent reported anxiety and depression. They did not differ from other children with neurodevelopmental disorders and no comorbid gender variance in terms of age, or IQ, and no sex ratio differences were found between the groups.
Hypothesis 3: Fewer Emotional Symptoms Among Children with ASDs and Gender Variance
When testing the hypothesis that children with concurrent gender variance and ASD would have fewer reported emotional symptoms than children with gender variance and a non-ASD neurodevelopmental disorder, the overall model was significant, F(3, 382) = 5.97, p = .001. There was a main effect for gender variance status, F(1, 382) = 7.41, p = .007, as well as for the interaction (ASD status X gender variance status), F(1, 382) = 4.70, p = .031. Post-hoc tests showed no significant difference in anxious/depressed ratings between ASD children with and without gender variance (t < 1). Anxious/depressed ratings were higher among non-ASD children with neurodevelopmental issues and concurrent gender variance as compared to those with a non-ASD neurodevelopmental disorder and no gender variance (t = −3.66, p < .001). Mean anxious/depressed scores were at the high end of the borderline clinical range (T = 69) for participants with a comorbid non-ASD neurodevelopmental disorder and gender variance, while mean anxious/depressed scores fell in the non-clinical range for participants with comorbid ASD and gender variance (T = 61.63).
Hypothesis 4: Sex Ratios of Participants with Gender Variance
Given the unequal male to female ratio inherent in ASDs and ADHD, we needed to adjust the base rate sex ratios of the CBCL non-referred group in order make comparisons with the participants in these two groups. This was accomplished by taking the male to female ratios in the ASD and ADHD groups and creating a new CBCL sample by randomly removing females in the CBCL non-referred sample until the male to female ratio matched that of the ASD and ADHD samples. After equalizing these base rate sex ratios, we found no significant differences in sex ratios of participants with gender variance and ADHD as compared to the CBCL non-referred comparison sample subjects with gender variance. We also found no significant sex ratio differences between the participants with gender variance and ASD and the CBCL non-referred subjects with gender variance. This process was repeated three times with no change in outcome.
Discussion
In the first study to compare the occurrence of wishing to be the other gender (gender variance) among children and adolescents with different neurodevelopmental disorders relative to non-referred control groups, we found participants with ASD to have significantly elevated rates of gender variance. Gender variance was 7.59 times more common in participants with ASD than in a large non-referred comparison group. This extends previous reports of an over-representation of ASD among children and adolescents referred for GID/gender variance (de Vries et al., 2010; Edwards-Leeper & Spack, 2012) by examining the overlap between ASD and gender variance among a group of children with ASDs. Surprisingly, we also found a significant over-representation of gender variance among participants with ADHD, with gender variance occurring 6.64 times more frequently among participants with ADHD than a non-referred comparison group. This is the first report of an overlap between ADHD diagnosis and comorbid gender variance, though previous studies have shown increased levels of behavioral problems and/or disruptive disorders among young people with gender variance (Cohen-Kettenis et al., 2003; de Vries et al., 2011; Wallien et al., 2007a; Zucker et al., 2002; Zucker & Bradley, 1995; Zucker et al., 2014). Our mixed medically-based neurodevelopmental group of participants with epilepsy or NF1 was not different from non-referred controls in rates of gender variance. Although rates of gender variance were several times higher in the ASD and ADHD groups, only about 5 % of the participants in these groups had parent reported gender variance on the CBCL. It is important to note that endorsement of the CBCL gender variance item level data does not imply a diagnosis of GID/gender dysphoria.
Building on previous studies reporting increased emotional symptoms among children and adolescents with GID/gender variance-related issues (de Vries et al., 2011; Wallien et al., 2007b), we found elevated rates of anxiety and depression symptoms (with mean scores in the borderline clinical range) among participants with comorbid neurodevelopmental disorders and gender variance as compared to participants with a neurodevelopmental disorder and no reported gender variance. Importantly, when comparing between the neurodevelopmental groups with comorbid gender variance, increased emotional symptoms were observed in the non-ASD neurodevelopmental groups, but not among participants with ASD. This could be due to reduced awareness of the societal pressures against gender nonconformity among gender nonconforming individuals with ASD, as ASD is a disorder characterized by social cognitive impairments. There were no significant differences in the ratio of male participants with gender variance compared to female participants with gender variance when comparing between the different neurodevelopmental disorder groups. Comorbid gender variance and neurodevelopmental disorders occurred in both males and females.
The coincidence of gender variance with ADHD and ASD could be understood vis-à-vis the influence of underlying symptoms of these neurodevelopmental disorders. In ADHD, difficulties inhibiting impulses are central to the disorder (American Psychiatric Association, 2000) and could result in difficulty keeping gender impulses “under wraps” in spite of internal and external pressures against cross-gender expression. In ASD, children and adolescents may be less aware of the social restrictions against expressions of gender variance and therefore less likely to avoid expressing these inclinations. It could also be theorized that excessively rigid or “black and white” thinking in ASD could result in a child with ASD rigidly interpreting mild or moderate gender nonconforming inclinations as more intense or absolute. However, this second idea is in contrast to a report from de Vries et al. (2010) that, after extended psychiatric evaluation, a substantial proportion of adolescents with ASD and concurrent GID/gender dypshoria showed persistent gender variance and were appropriate for gender transitioning.
Recent findings suggest a possible physiological correlate for the overlap between ASD and gender variance. Bejerot et al. (2012) studied adults with ASD and found that, compared to a non-ASD group, women with ASD had increased masculine physical characteristics: higher testosterone levels, less feminine facial features, and larger head circumference. Men with ASD, as compared to a non-ASD group, had less masculine characteristics overall, including less masculine body attributes, less masculine voice, and a ratio of second to fourth finger more similar to that in females. Nevertheless, it remains unclear how our findings fit with models, such as the extreme male brain theory (Baron-Cohen, 2002, 2009), that have paralleled ASD differences from typical development with those found in males versus females. There is also evidence showing reduced sex differences among adults with ASD in brain regions recruited to perform neuropsychological tasks (Beacher et al., 2012).
Though novel, our study had limitations. First, because this was not a population-based study, issues of clinical ascertainment bias may arise; however, this concern is mitigated in between group comparisons due to highly similar referral sources. Future studies should examine the coincidence of gender variance and neurodevelopmental disorders in the context of total population samples, extending beyond clinically-ascertained groups. Second, the field lacks well-tested instruments sensitive to gender variance. Although the CBCL gender identity-related item level data has been shown to be sensitive and specific to gender variance, future studies should employ more comprehensive assessments of gender identity, including self-reports from the children and adolescents themselves.
This study confirms the importance of examining gender variance in various neurodevelopmental disorders. Given our findings of elevated emotional symptoms among those children with comorbid neurodevelopmental disorders and gender variance, and our clinical experience that these children have particularly complex challenges managing gender variance in the presence of neurodevelopmental challenges, further inquiry into this comorbidity is important. Future directions should include research on the management of gender variance when there is a comorbid neurodevelopmental disorder. For example, how does a clinician best assess whether an adolescent with ASD who expresses a wish to transition to the other gender understands the “big picture” implications of such a decision, when it is known that ASD often results in problems with so-called “central coherence” and related “big picture” thinking skills (Happé & Frith, 2006; Jackson & Atance, 2008). Treatment related studies are also required, addressing such issues as how to help an adolescent with persistent gender variance and ASD manage gender transition, when deficits in social awareness, executive function (Kenworthy, Yerys, Anthony, & Wallace, 2008), and self-help skills (Kenworthy, Case, Harms, Martin, & Wallace, 2010; Rodrigue, Morgan, & Geffken, 1991) severely impact their ability to “pass” as the other gender.
References
Achenbach, T. M., & Rescorla, L. A. (2001). Manual for ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families.
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: Author.
Arnold, S. D. (1996). Sex differences in ADHD: Conference summary. Journal of Abnormal Child Psychology, 24, 555–569.
Baird, G., Simonoff, E., Pickles, A., Chandler, S., Loucas, T., Meldrum, D., et al. (2006). Prevalence of disorders of the autism spectrum in a population cohort of children in South Thames: The Special Needs and Autism Project (SNAP). Lancet, 368, 210–215.
Baron-Cohen, S. (2002). The extreme male brain theory of autism. Trends in Cognitive Sciences, 6, 248–254.
Baron-Cohen, S. (2009). Autism: The empathizing-systemizing (E-S) theory. Annals of the New York Academy of Sciences, 1156, 68–80.
Beacher, F. D. C. C., Radulescu, E., Minati, L., Baron-Cohen, S., Lombardo, M. V., Lai, M., et al. (2012). Sex differences and autism: Brain function during verbal fluency and mental rotation. PLoS ONE, 7. doi:10.1371/journal.pone.0038355.
Bedard, C., Zhang, H. L., & Zucker, K. J. (2010). Gender identity and sexual orientation in people with developmental disabilities. Sexuality and Disability, 28, 165–175.
Bejerot, S., Eriksson, J. M., Bonde, S., Carlström, K., Humble, M. B., & Eriksson, E. (2012). The extreme male brain revisited: Gender coherence in adults with autism spectrum disorder. British Journal of Psychiatry, 201, 116–123.
Biddle, D. A., & Morris, S. B. (2011). Using Lancaster’s mid-P correction to the Fisher’s exact test for adverse impact analyses. Journal of Applied Psychology, 96, 956–965.
Bland, J. M., & Altman, D. G. (2000). Statistics notes: The odds ratio. British Medical Journal, 320, 1468.
Center for Disease Control and Prevention. (2012). Prevalence of autism spectrum disorders—autism and developmental disabilities monitoring network, fourteen sites, United States, 2008. Surveillance Summaries, 61, 1–19.
Coates, S., & Person, E. S. (1985). Extreme boyhood femininity: Isolated behavior or pervasive disorder? Journal of the American Academy of Child Psychiatry, 24, 702–709.
Cohen-Kettenis, P. T., Owen, A., Kaijser, V. G., Bradley, S. J., & Zucker, K. J. (2003). Demographic characteristics, social competence, and behavior problems in children with gender identity disorder: A cross-national, cross-clinic comparative analysis. Journal of Abnormal Child Psychology, 31, 41–53.
Constantino, J. N., & Gruber, C. P. (2005). Social Responsiveness Scale. Los Angeles, CA: Western Psychological Services.
de Vries, A. L. C., & Cohen-Kettenis, P. T. (2012). Clinical management of gender dysphoria in children and adolescents: The Dutch approach. Journal of Homosexuality, 59, 301–320.
de Vries, A. L. C., Doreleijers, T. A. H., Steensma, T. D., & Cohen-Kettenis, P. T. (2011). Psychiatric comorbidity in gender dysphoric adolescents. Journal of Child Psychology and Psychiatry, 52, 1195–1202.
de Vries, A. L. C., Noens, I. L., Cohen-Kettenis, P. T., Van Berckelaer-Onnes, I. A., & Doreleijers, T. A. (2010). Autism spectrum disorders in gender dysphoric children and adolescents. Journal of Autism and Developmental Disorders, 40, 930–936.
Dreger, A. (2009). Gender identity disorder in childhood: Inconclusive advice to parents. Hastings Center Report, 39, 26–29.
Drescher, J., & Byne, W. (2012). Introduction to the Special Issue on “The Treatment of Gender Dysphoric/Gender Variant Children and Adolescents.” Journal of Homosexuality, 59, 295–300.
Edwards-Leeper, L., & Spack, N. P. (2012). Psychological evaluation and medical treatment of transgender youth in an interdisciplinary “Gender Management Service” (GeMS) in a major pediatric center. Journal of Homosexuality, 59, 321–336.
Fombonne, E. (2005). Epidemiology of autistic disorder and other pervasive developmental disorders. Journal of Clinical Psychiatry, 66, 3–8.
Gallucci, G., Hackerman, F., & Schmidt, C. W. (2005). Gender identity disorder in an adult male with Asperger’s syndrome. Sexuality and Disability, 23, 35–40.
Gutmann, D. H., Aylsworth, A., Carey, J. C., Korf, B., Marks, J., Pyeritz, R. E., et al. (1997). The diagnostic evaluation and multidisciplinary management of neurofibromatosis 1 and neurofibromatosis 2. Journal of the American Medical Association, 278, 51–57.
Happé, F., & Frith, U. (2006). The weak coherence account: Detail-focused cognitive style in autism spectrum disorders. Journal of Autism and Developmental Disorders, 36, 5–25.
Jackson, L. K., & Atance, C. M. (2008). Future thinking in children with autism spectrum disorders: A pilot study. Journal on Developmental Disabilities, 14, 40–45.
Kenworthy, L., Case, L., Harms, M. B., Martin, A., & Wallace, G. L. (2010). Adaptive behavior ratings correlate with symptomatology and IQ among individuals with high-functioning autism spectrum disorders. Journal of Autism and Developmental Disorders, 40, 416–423.
Kenworthy, L., Yerys, B. E., Anthony, L. G., & Wallace, G. L. (2008). Understanding executive control in autism spectrum disorders in the lab and in the real world. Neuropsychology Review, 18, 320–338.
Kraemer, B., Delsignore, A., Gundelfinger, R., Schnyder, U., & Hepp, U. (2005). Comorbidity of asperger syndrome and gender identity disorder. European Child and Adolescent Psychiatry, 14, 292–296.
Lai, M., Chiu, Y., Gadow, K. D., Gau, S. S., & Hwu, H. (2010). Correlates of gender dysphoria in Taiwanese university students. Archives of Sexual Behavior, 39, 1415–1428.
Lainhart, J. E., Bigler, E. D., Bocian, M., Coon, H., Dinh, E., Dawson, G., et al. (2006). Head circumference and height in autism: A study by the Collaborative Program of Excellence in Autism. American Journal of Medical Genetics Part A, 140, 2257–2274.
Landen, M., & Rasmussen, P. (1997). Gender identity disorder in a girl with autism: A case report. European Child and Adolescent Psychiatry, 6, 170–173.
Le Couteur, A., Rutter, M., Lord, C., Rios, P., Robertson, S., Holdgrafer, M., et al. (1989). Autism Diagnostic Interview: A standardized investigator-based instrument. Journal of Autism and Developmental Disorders, 19, 363–387.
Lord, C., Rutter, M., DiLavore, P. C., & Risi, S. (2000). Autism Diagnostic Observation Schedule (ADOS). Los Angeles: Western Psychological Services.
Lord, C., Rutter, M., & Le Couteur, A. (1994). Autism Diagnostic Interview-Revised: A revised version of the Autism Diagnostic Interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders, 24, 659–685.
Menvielle, E. (2012). A comprehensive program for children with gender variant behaviors and gender identity disorders. Journal of Homosexuality, 59, 357–368.
Mukaddes, N. M. (2002). Gender identity problems in autistic children. Child: Care. Health and Development, 28, 529–532.
Perera, H., Gadambanathan, T., & Weerasiri, S. (2003). Gender identity disorder presenting in a girl with Asperger’s disorder and obsessive compulsive disorder. Ceylon Medical Journal, 48, 57–58.
Rodrigue, J. R., Morgan, S. B., & Geffken, G. R. (1991). A comparative evaluation of adaptive behavior in children and adolescents with autism, Down syndrome, and normal development. Journal of Autism and Developmental Disorders, 21, 187–196.
Tateno, M., Tateno, Y., & Saito, T. (2008). Comorbid childhood gender identity disorder in a boy with Asperger syndrome. Psychiatry and Clinical Neurosciences, 62, 238.
Van Beijsterveldt, C. E. M., Hudziak, J. J., & Boomsma, D. I. (2006). Genetic and environmental influence on cross-gender behavior and relation to behavior problems: A study of Dutch twins at ages 7 and 10 years. Archives of Sexual Behavior, 35, 647–658.
VanderLaan, D. P., Postema, L., Wood, H., Singh, D., Fantus, S., Hyun, J., et al. (2014). Do children with gender dysphoria have intense/obsessional interests? Journal of Sex Research. doi:10.1080/00224499.2013.860073.
Wallien, M. S. C., Swaab, H., & Cohen-Kettenis, P. T. (2007a). Psychiatric comorbidity among children with gender identity disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 46, 1307–1314.
Wallien, M. S. C., van Goozen, S. H. M., & Cohen-Kettenis, P. T. (2007b). Physiological correlates of anxiety in children with gender identity disorder. European Child and Adolescent Psychiatry, 16, 309–315.
Williams, P. G., Allard, A. M., & Sears, L. (1996). Case study: Cross-gender preoccupations with two male children with autism. Journal of Autism and Developmental Disorders, 26, 635–642.
Wolkenstein, P., Freche, B., Zeller, J., & Revuz, J. (1996). Usefulness of screening investigations in neurofibromatosis type 1: A study of 152 patients. Archives of Dermatology, 132, 1333–1336.
Wood, H. (2011, October). The relationship between gender identity disorder and autism spectrum disorder. In K. J. Zucker (Chair), Gender identity disorder in children and adolescents: Theoretical and empirical advances. Symposium presented at the joint meeting of the American Academy of Child and Adolescent Psychiatry and the Canadian Academy of Child and Adolescent Psychiatry, Toronto.
Zucker, K. J., & Bradley, S. J. (1995). Gender identity disorder and psychosexual problems in children and adolescents. New York: Guildford Press.
Zucker, K. J., Bradley, S. J., Owen-Anderson, A., Kibblewhite, S. J., Wood, H., Singh, D., et al. (2012). Demographics, behavior problems, and psychosexual characteristics of adolescents with gender identity disorder or transvestic fetishism. Journal of Sex and Marital Therapy, 38, 151–189.
Zucker, K. J., Owen, A., Bradley, S. J., & Ameeriar, L. (2002). Gender-dysphoric children and adolescents: A comparative analysis of demographic characteristics and behavioral problems. Clinical Child Psychology and Psychiatry, 7, 398–411.
Zucker, K. J., Wood, H., & VanderLaan, D. P. (2014). Models of psychopathology in children and adolescents with gender dysphoria. In B. P. C. Kreukels, T. D. Steensma, & A. L. C. de Vries (Eds.), Gender dysphoria and disorders of sex development: Progress in care and knowledge (pp. 171–192). New York: Springer.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Strang, J.F., Kenworthy, L., Dominska, A. et al. Increased Gender Variance in Autism Spectrum Disorders and Attention Deficit Hyperactivity Disorder. Arch Sex Behav 43, 1525–1533 (2014). https://doi.org/10.1007/s10508-014-0285-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10508-014-0285-3