Abstract
This mixed methods study aimed to examine partner and relationship characteristics associated with HIV risk among young men who have sex with men (YMSM). A sub-sample of YMSM (18–25 years) who were involved in serious relationships with other men were recruited from two on-going longitudinal studies, Project Q2 and Crew450 (N = 20 couples). The mean age of the dyadic sample was 22.5 years (SD = 5.33, range 18–46 years) and participants were racially and ethnically diverse, with the largest percentage of the sample identifying as African American (47.5 %), followed by Hispanic (20 %). Participants completed individual self-report measures using computer-assisted self-interview technology and engaged in couples-based interviews. Mixed methods analyses indicated three global reasons for unprotected sex among YMSM in serious relationships: (1) the desire to achieve emotional intimacy; (2) the perception of being in a monogamous relationship; and (3) the difficulties associated with accessing and/or using condoms. Couples’ decision-making processes, including decisions made “in the heat of the moment,” have implications for HIV prevention interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
From 2007 through 2010, the percentage of HIV diagnoses among adolescents and adults exposed through male-to-male sexual contact increased from 55 to 61 % (CDC, 2012a). Among 20- to 24-year olds in 2009, there were more than four times as many HIV infections among young men who have sex with men (YMSM) than among young women across all risk categories (CDC, 2012b). In light of these data, increased attention has focused on characteristics that place YMSM at higher risk for HIV infection (Mustanski, Newcomb, DuBois, Garcia, & Grov, 2011c). Recently, Sullivan, Salazar, Buchbinder, and Sanchez (2009) modeled HIV transmission data from MSM in five U.S. cities and estimated that the majority of transmissions (68 %) were from “main partners,” with the proportion of transmissions being significantly higher among YMSM ages 18–24 (79 %). They attributed these findings to how younger men define main partners, their shorter relationship lengths, and their higher proportion of unrecognized infections. In contrast, Goodreau et al. (2012) used dynamic, stochastic network models informed by data from several large HIV behavioral risk surveys to estimate the proportion of infection among MSM. These model-based estimates suggested a lower proportion of transmissions due to main partnerships (~39 % in the U.S.), but no age-stratified results were reported.
Individual, Partner, and Relationships Factors Associated with Unprotected Sex
With a large proportion of new infections among MSM occurring in main partnerships, there is a need for research that explores the influence of relationship factors on HIV risk, particularly within dyads. There are obvious emotional and health benefits that can come with being in a romantic relationship (Misovich, Fisher, & Fisher, 1997; Robles & Kiecolt-Glaser, 2003) and it is not surprising that most YMSM desire to be in a relationship (D’Augelli, Rendina, Sinclair, & Grossman, 2008; DeHaan, Kuper, Magee, Bigelow, & Mustanski, 2013), particularly as same sex relationships may buffer against prejudice and discrimination (Peplau & Fingerhut, 2007). Among male couples, risk for HIV transmission has been examined in relation to individual and partner characteristics, relationship characteristics, as well as negotiated safety within relationships. Given the dearth of relationship-oriented research on YMSM, we reviewed studies with adult MSM and highlighted findings with YMSM where appropriate.
Individual and Partner Characteristics
Relationship research among samples of MSM has examined the relation between HIV risk behaviors and partner characteristics, including age (Bingham et al., 2003; Bruce, Harper, Fernandez, Jamil, & Adolescent Medicine Trials Network for HIV/AIDS Interventions, 2012; Morris, Zavisca, & Dean, 1995; Mustanski, Newcomb, & Clerkin, 2011b), familiarity (Boulton, McLean, Fitzpatrick, & Hart, 1995; McNeal, 1997; Newcomb & Mustanski, 2013), sexual history (Boulton et al., 1995; McLean et al., 1994; Misovich et al., 1997), and HIV status (Davidovich, de Wit, & Stroebe, 2004; Elford, Bolding, Maguire, & Sherr, 1999; Remien, Wagner, Dolezal, & Carballo-Diéguez, 2002). Among YMSM, Sullivan et al. (2009) identified important developmental considerations in reference to HIV risk in relationships, including undiagnosed HIV infections among YMSM, cognitive differences in definitions of serious relationships, and relationship trajectories. In longitudinal research with young men in “boyfriend” relationships, Hays, Kegeles, and Coates (1997) found that over 40 % of the participants who reported having unprotected sex were not aware of their own HIV status or the status of their partner. Factors associated with unprotected sex were poor sexual communication skills, increased involvement in the relationship, and a lack of knowledge of HIV risk.
Additional risk factors relevant to YMSM include partner age and income differentials. Research on the association between sexual partner age and HIV risk in young MSM consistently points to a positive association (Bingham et al., 2003; Morris et al., 1995; Mustanski et al., 2011b; Newcomb & Mustanski, 2013). For example, a study of predictors of HIV infection among Black and White YMSM (ages 23–29 years) found that having older partners (by 5 years or more) nearly quadrupled the odds of being HIV positive (Bingham et al., 2003). There has been limited research on economic dependencies and HIV risk within young male partnerships, but a large survey of YMSM found that 11 % reported exchanging sex in the last 6 months for “things you or they needed” (Harawa et al., 2004).
Relationship Characteristics
Research that has examined HIV risk by relationship type indicates that one of the strongest and most consistent predictors of unprotected sex among YMSM is their characterization of their relationship as “serious,” “steady,” or “main” (Bingham et al., 2003; Elford et al., 1999; Hart, Peterson, & The Community Intervention Trial for Youth Study Team, 2004; Hays et al., 1997; Hoff, Coates, Barrett, Collette, & Ekstrand, 1996; Mustanski et al., 2011b; Stueve, O’Donnell, Duran, San Doval, & Geier, 2002; Wong, Schrager, Chou, Weiss, & Kipke, 2013). Higher rates of unprotected sex in serious relationships may be attributed to negotiated safety (e.g., agreements about sexual practices in and outside the relationship and sexual practices based on HIV seroconcordance). For example, couples may agree to practice unprotected sex with each other, but must only have protected sex with partners outside the relationship. However, even after correcting for negotiated safety, rates of unprotected intercourse are higher among steady partners than casual partners, supporting the assumption that serious relationships provide a context that facilitates sexual risk-taking behaviors (Davidovich, de Wit, & Stroebe, 2000).
Preliminary research suggests there is an association between relationship length and HIV risk. Two longitudinal studies of YMSM have found increased HIV risk behaviors associated with relationship length. That is, romantic partnerships lasting more than 6 months and incrementally serious relationships (i.e., from one night stands to casual dating) were predictive of unprotected sex in relationships among YMSM (Mustanski et al., 2011b; Newcomb, Ryan, Garofalo, & Mustanski, 2013). In addition, Mustanski et al. reported that young men were likely to classify a relationship as serious in less than 6 months of sexual contact and reported multiple serious relationships within 18 months, putting these men at greater risk for engaging in unprotected sex acts with multiple partners. Research is needed that explains the interplay between relationship length, seriousness, and HIV risk. One study with a sample of young heterosexual women suggested that decreases in condom use in “established” relationships may be attributed to increased knowledge about the partner and the perception of decreased risk if there are no observable signs of STIs (Fortenberry, Tu, Harezlak, Katz, & Orr, 2002).
Although research has examined associations between HIV risk behaviors and relationship factors, such as satisfaction, commitment, and investment among male couples, the findings are mixed and generally lacking among samples of YMSM. Some studies have found that MSM engage in unprotected sex to display trust, intimacy, and love in their relationships (Appleby, Miller, & Rothspan, 1999; Blais, 2006; Carballo-Diéguez & Dolezal, 1996; Davidovich et al., 2004; Golub, Starks, Payton, & Parsons, 2012; Remien, Carballo-Dieguez, & Wagner, 1995; Theodore, Duran, Antoni, & Fernandez, 2004). Similarly, other research has found that MSM have unprotected sex with steady partners in an attempt to strengthen relationship commitment and satisfaction (de Vroome, Stroebe, Sandfort, De Wit, & Van Griensven, 2000; McLean et al., 1994; McNeal, 1997; Worth, Reid, & McMillan, 2002). In contrast to these findings, Davidovich, de Wit, and Stroebe (2006) found that relationship satisfaction was associated with safer-sex behaviors. That is, participants who perceived high levels of satisfaction within their relationship were more likely to use condoms or engage in negotiated safety with their primary partners.
Sexual Agreements
The agreements that couples make about sexual behavior within and outside of their partnership are another important factor relevant to understanding HIV risk in relationships (Davidovich et al., 2000; Hoff & Beougher, 2010; Hoff, Beougher, Chakravarty, Darbes, & Neilands, 2010; Hoff et al., 2009; Kippax et al., 1997, 2003; Mitchell, Harvey, Champeau, Moskowitz, & Seal, 2012; Neilands, Chakravarty, Darbes, Beougher, & Hoff, 2010; Parsons, Starks, DuBois, Grov, & Golub, 2011; Parsons, Starks, Gamarel, & Grov, 2012; Prestage et al., 2008). Negotiated safety is one form of a sexual agreement in which concordant HIV negative couples engage in unprotected anal intercourse and both partners agree to practice safe sex with outside partners. The research results are mixed on the effectiveness of sexual agreements as an HIV prevention strategy (Davidovich et al., 2000; Hoff & Beougher, 2010; Kippax et al., 1997, 2003). Contextual factors, such as drug and alcohol use, have been found to negate the effective enactment of sexual agreements (Parsons et al., 2005; Wilkerson, Smolenski, Morgan, & Rosser, 2012). Additionally, among HIV serodiscordant couples, Hoff et al. (2009) found that, while serostatus differences were related to the quality of sexual agreements, there were no significant differences in the occurrences of faulted agreements or in reasons for breaking agreements based on the couples’ HIV status.
Sexual Decision-Making
Sexual decision-making is a process involving individual and dyadic input that cuts across partner and relationship characteristics associated with HIV risk. In particular, the concept of decisional balance to act on a behavior (Janis & Mann, 1977) has been examined in sexual risk research with MSM (Bauermeister, Carballo-Diéguez, Ventuneac, & Dolezal, 2009; Halkitis & Parsons, 2003; Janis & Mann, 1977). According to this framework, a behavioral decision is influenced by the practical gains and losses for the individual and their partner. For MSM in sexual relationships, decisional balance considers the reality of negotiating sexual encounters in which men may know that condoms protect against HIV but forego using them if they recognize the gains of engaging in unprotected sex (e.g., increased intimacy with a partner, enhanced pleasure) (Halkitis & Parsons, 2003). The concept of decisional balance is illustrated in research with HIV-positive and HIV-negative MSM. While both groups report pleasure and emotional gains associated with unprotected sex, HIV-positive men also reported having unprotected sex as a way of coping with social stressors (Bauermeister et al., 2009).
Decisional balance has also been examined among YMSM. The HIV prevention strategy of taking estimated risks balances cultural norms for safer sex with individual sexual desires (Eisenberg, Bauermeister, Pingel, Johns, & Santana, 2011). In their qualitative research, Eisenberg et al. reported that young men engaged in negotiated safety instead of strictly adhering to conventional prevention strategies (e.g., abstinence, consistent condom use). They also found that estimates of sexual risk were shaped by relationship expectations. That is, the young men described how engaging in anal sex promoted intimacy with, and communicated trust to, their romantic partners. In the decisional balance framework, YMSM weighed the potential gains (e.g., intimacy, pleasure) against the losses (e.g., partner mistrust, putting oneself at risk) of not using condoms during sexual encounters.
The Current Study
Our previous longitudinal research with racially and ethnically diverse YMSM found that labeling a relationship as “serious” was the biggest predictor of HIV risk, increasing the rate of unprotected sex in a given relationship by nearly eight times (Mustanski et al., 2011b). Additional factors that increased the rate of unprotected sex included being in a relationship lasting 6 months or longer, having older partners, having a history of violence or forced sex in the relationship, and using drugs prior to sex. To build on this prior quantitative research, we adopted a mixed methods approach to achieve a better understanding of these associations. This design takes advantage of the strengths of both quantitative and qualitative methodologies (Axinn & Pearce, 2006) and has been used successfully in our previous research (DeHaan et al., 2013; Magee, Bigelow, Dehaan, & Mustanski, 2012; Mustanski, Lyons, & Garcia, 2011a). This study aimed to: (1) fill a gap in the research literature by collecting descriptive quantitative survey data on the individual, partner, and relationship characteristics of YMSM in serious relationships and (2) explore relationship characteristics associated with unprotected sex among YMSM by conducting dyadic interviews with male couples. This examination was a shift from strictly individual-level factors to a multi-faceted analysis of partner- and relationship-level phenomena among a high-risk and understudied group of YMSM in serious relationships.
Method
Participants
We recruited 23 male-born couples from two ongoing longitudinal cohort studies of LGBT youth, Project Q2 and Crew450 (for further description of these studies, see Mustanski, Garofalo, & Emerson, 2010; Mustanski, Johnson, Garofalo, Ryan, & Birkett, 2012). Of those couples, project staff determined that two dyads had falsely reported being in relationships. These false couples were identified based on discrepancies between the quantitative data (e.g., partner drinking habits, sexual agreements, condom use) and interactions during the in-person interviews. One additional couple was excluded from analysis due to a large age discrepancy (>30 years) and lack of a sexual relationship (i.e., no oral or anal sex within the last year). Thus, the final analytic sample was comprised of 20 couples (14 couples were recruited from Project Q2 and six couples from Crew 450) which were composed of at least one YMSM (18–25 years of age) and their serious romantic partner.
The mean age of the sample was 22.5 years (SD = 5.33, range 18–46). As shown in Table 1, participants were racially and ethnically diverse, with the largest percentage of the sample identifying as African American (47.5 %), followed by Hispanic (20 %). Over three quarters of the sample identified as gay, with a subset identifying as bisexual. In terms of relationship length, approximately 75 % of the couples had been in their current relationship 3 years or less. For HIV status, four (20 %) of the couples identified as serodiscordant; the remaining couples were concordant HIV negative. Differences between participants based on recruitment source were minimal: the Crew450 sample was younger (M age = 21.08 years, SD = 5.49 vs. 23.14 years, SD = 5.24) and contained a smaller proportion of African Americans (25 vs. 57.1 %) compared to the Project Q2 sample.
Procedure
Research staff contacted potential participants if they indicated they were in a relationship at their last study visit with Project Q2 or Crew 450. When contacted, prospective participants were provided with a brief overview of the study and given time to ask their partner whether he would like to participate. New couples were recruited until data had reached saturation (i.e., no new themes emerged in the interviews). The point of saturation was identified through comparison of detailed couple interview summaries which were discussed at weekly team meetings.
Study procedures included quantitative and qualitative data collection. Upon arrival to the study site, both members of the couple met together with two trained interviewers who provided an overview of the research. The couple was then split and participants were taken into separate offices. Each individual provided informed consent to participate in the research and completed self-report measures using computer-assisted self-interview (CASI) technology. Following survey completion, interviewers reviewed alerts by the CASI flagging system if either partner indicated that physical abuse was occurring within the relationship. In these cases, interviewers individually met with the participant reporting the abuse to collect more information to ensure that the participant was not in current danger. Interviewers also assessed whether the participant wanted to continue with the qualitative interview of the couple. After completion of the individual CASIs, members of the couple were brought together and participated in the qualitative interview with the two interviewers.
Each interview followed a semi-structured format. Questions central to the study aims were included in the interview guide; however, interviewers were able to ask follow-up questions to gain more information regarding each couple’s responses to these questions. The interview guide addressed three main areas: (1) the couple’s relationship history and general functioning (e.g., how they met, how long they have been dating) and views regarding relationship labels and milestones (e.g., what language they use to refer to each other, views on living together); (2) the couple’s history of safe sex practices (e.g., getting tested for HIV, using condoms) and discussions within the relationship (e.g., how they have talked about monogamy); and (3) the couple’s history in previous HIV or couples-based interventions, as well as participants’ suggestions for the development of future interventions. At the end of each interview, participants were provided with a list of local, LGBT-friendly, couples-based resources and services (e.g., couples-based HIV testing). The interviews were approximately 90-min long and participants were each paid $30 for their time.
Measures
Dating Assessment
This assessment contained items drawn from previous research measuring dating history and relationship patterns (Furman, 1994; Harris et al., 2009; Kuttler & La Greca, 2004), as well as from our research assessing partner characteristics and sexual risk behaviors (Mustanski et al., 2010). Dating history items assess lifetime (e.g., “How old were you when you first started dating”), 12 month (e.g., “How many people have you dated in the past 12 months?”), and current dating experiences. Relationship patterns were assessed with the following item: “What are your usual dating patterns?” Response options ranged from (1) “I have never dated” to (4) “I am usually involved in an exclusive relationship with someone.” Partner characteristics questions assessed age, race/ethnicity, and gender. With regard to sexual risk behaviors, a sample item included, “Thinking back to the first time you had anal or vaginal sex with your first serious dating partner, did you or your partner use a condom?”
Relationship Satisfaction
Relationship satisfaction was measured using the 7-item Relationship Assessment Scale (RAS) (Hendrick, 1988). Participants used a 5-point Likert scale, with specific anchors varying across items. This measure demonstrated adequate internal consistency in the current sample (Cronbach’s α = 0.72). A total score was computed as the mean of all items (e.g., “How good is your relationship compared to most?”). Two items were reverse scored so that higher scores indicated greater relationship satisfaction.
Relationship Investment
Relationship investment was measured using a modified version of the 5-item Investment Model Scale (Lehmiller & Agnew, 2006; Rusbult, Martz, & Agnew, 1998). With higher scores reflecting greater relationship investment, participants used a 9-point Likert scale (1 “do not agree at all” to 9 “agree completely”) to respond to study items (e.g., “Many aspects of my life have become linked to my partner”). A total score was computed as the mean of all items. This measure demonstrated low internal consistency in the current sample (Cronbach’s α = 0.51).
Sexual Agreements
Information about sexual agreements was assessed using a series of items developed by Hoff et al. (2010) for their qualitative research with male couples. Participants categorized their sexual agreement into one of the following options: (1) “We cannot have sex with an outside partner,” (2) “We can have sex with outside partners but with some restrictions,” (3) “We can have sex with outside partners without any restrictions,” or (4) “We do not have an agreement.” Participants who selected one of the first three responses were asked additional questions, including whether the agreement had been discussed explicitly, what restrictions were placed on sexual behaviors, and reasons the agreement was made.
Condom Use
Participants responded to a series of items on condom use in relationships that was developed for the present study. To establish frequency of condom use, participants were asked to categorize how often they used condoms with their romantic partner in the last 6 months based on five options ranging from “none of the time” to “every time.” Participants were then presented with a list of 12 reasons for not using condoms (or why they might stop using condoms) that was created from prior literature on condom use in relationships (e.g., “You and your partner wanted to express trust to each other”). Participants were also asked if a condom had been used during the first anal sex act with their current partner.
Analytic Approach
Quantitative survey data were examined both within and across dyads to provide descriptive information about YMSM in serious relationships and to provide additional context for the qualitative interviews. Concordance for relationship characteristics was determined by taking the difference between scale scores (i.e., relationship assessment and investment scales) or directly comparing participant item responses (i.e., condom use, sexual agreements) within the couple. Concordance on reasons couples did not use condoms was determined by comparing participant response options (e.g., express trust, HIV negative) within each couple. A dyad was found to be concordant if both individuals either (1) selected the same response option or (2) both did not select a response option (thereby agreeing that the reason was not a factor in their condom use).
The qualitative interviews of the couples were audio-recorded, transcribed, and uploaded into Dedoose (2012), a qualitative and mixed methods analysis program. During the first round of coding, a team of four coders independently open-coded a selection of transcripts and met weekly to develop an initial codebook. Between meetings, coders continued to code additional transcripts to revise existing codes and develop new codes. Codes reflected key interview topics (e.g., safe sex definition) as well as themes relevant to all three sections of the interview (e.g., relationship milestones, reasons for unprotected sex, intervention preferences). Once a comprehensive codebook was established, coders completed several rounds of reliability training where they applied codes to designated excerpts, which were then compared to the codes applied by the lead coder. For the initial reliability test using 52 excerpts from four interviews, the pooled kappa scores (De Vries, Elliott, Kanouse, & Teleki, 2008) ranged from 0.74 to 0.77, representing substantial inter-coder reliability (Cicchetti, 1994; Landis & Koch, 1977). Midway through coding, a second reliability test was administered to check for coding drift using 49 excerpts from four interviews. These kappas ranged from 0.80 to 0.87, indicating excellent agreement.
In the next phase of coding, codes relating to sexual health were isolated and further analyzed using grounded theory (Glaser & Strauss, 1967). First, a process of open-coding was conducted within each sexual health code. Next, these open-codes were grouped into axial codes that reflected sub-themes, processes, or components of the larger code. For this study, the primary code of interest was “reasons for unprotected sex.” Safe sex was defined as using protection or barrier methods to protect against HIV or STIs, in addition to minimizing or avoiding sexual contact. The code was applied to any discussion of reasons why the couple had (or currently has) unprotected sex and hypothetical reasons why couples may choose not to use condoms (e.g., they both tested negative for HIV).
After all transcripts were coded, the qualitative data were analyzed thematically (Miles & Huberman, 1994); that is, we explored thematic differences in reasons for unprotected sex among male couples. These data were merged with data from the demographic scales and quantitative relationship measures using mixed methods approaches (Axinn & Pearce, 2006; Boardman et al., 2011) that we have used successfully in prior studies (DeHaan et al., 2013; Magee et al., 2012; Mustanski et al., 2011a). Informed by our previous quantitative research on relationship characteristics and sexual risks among YMSM (Mustanski et al., 2011b; Newcomb et al., 2013), the present mixed methods analyses explored relationship length as a risk factor for unprotected sex among YMSM in serious relationships.
Results
Quantitative Findings
Demographic Characteristics
The demographic and relationship characteristics for the 20 couples are shown in Table 2. In eight (40 %) of these couples, there was an age difference of 1 year or less between partners; in another eight (40 %) couples, there was an age difference of 2–4 years, and in the remaining four (20 %) couples, there was an age difference of 5 years or more. In terms of racial and ethnic backgrounds, the couples were generally concordant, with 13 (65 %) having the same racial or ethnic backgrounds. Regarding sexual orientation, in 15 (75 %) partnerships, both members of the couple identified as gay. In the remaining five couples, at least one member of the dyad identified as bisexual and their partners identified as gay (n = 3), heterosexual (n = 1), and transgender (male-to-female) (n = 1).
Relationship Characteristics
Thirty-five percent of couples (n = 7) were in relationships lasting less than 1 year, 40 % (n = 8) were in 1–3 year relationships, and 25 % (n = 5) were in relationships lasting more than 3 years. Based on the quantitative survey, couples rated their relationships favorably, with mean scores of 4.23 (SD = 0.49) on the RAS (Likert scale range 1–5) and 7.3 (SD = 0.98) on the relationship investment scale (Likert scale range 1–9). Examination of single scale items also yielded high scores on seriousness, trust, love, commitment, and satisfaction (see Table 2). Absolute difference scores were computed at the dyadic-level to assess agreement or disagreement on relationship characteristics. These analyses indicated high agreement in couples’ evaluation of their partner and relationship. In addition, matches between couples’ scores (i.e., ±1 point on the Likert scale responses) were 85 % or higher across the relationship items.
Sexual Relationship Characteristics
Per the study eligibility criteria, all participants reported being sexually active with their romantic partner. At least one member in six of the 20 couples (30 % of all couples) did not know or were unsure of their partner’s HIV status. Analysis of reports within couples indicated that at least one partner from seven of the 20 couples (35 % of all couples) reported no condom use during their first anal sex act as a couple. Conversely, for 65 % of the couples, both partners reported condom use at their first anal intercourse. Regarding condom use in the past 6 months, 60 % (n = 12) of the couples were concordant in their reports of condom use. Of these 12 couples, one reported using condoms every time and five reported using condoms none of the time.
Table 3 presents reasons participants reported for not using condoms within their partnership, separated by the overall frequency of condom use in the relationship during the past 6 months (for those who always used condoms, the item asked about reasons the couple might stop using condoms). For participants who reported never or sometimes using condoms, expressing love, trust, and commitment were the most frequently cited reasons for having unprotected sex (62.5, 75, and 62.5 % respectively). Having a negative HIV status (50 %) and being in a monogamous relationship (37.5 %) were also highly cited reasons for not using condoms. Nearly one-third of participants (31.3 %) indicated that not using condoms was an unplanned event that became routinized in their sexual repertoire. Compared to their counterparts, participants who sometimes used condoms were less likely to endorse a reason for not using condoms across most items.
To assess whether or not couples were concordant in their reasons for not using condoms, the 12 survey response options were collapsed into seven factors: (1) condoms irritated the skin and/or did not fit; (2) the couple wanted to express intimacy (e.g., express love, trust, commitment); (3) the couple tested together and/or both were HIV negative; (4) the couple was monogamous; (5) sex outside the relationship was protected; (6) there was a belief that their partner did not want to use condoms; and (7) unprotected sex became routine after an unplanned event. Table 4 presents concordance of couples’ reasons for not using condoms in their relationships. Across all couples and items, the average concordance rate was 74 % with agreement across couples ranging from 57 to 100 % (includes agreements as to whether each factor was mutually selected or not selected as a reason for unprotected sex). Wanting to express intimacy was the most agreed upon reason for having unprotected sex (52.9 %). The most disagreed upon reason was that unprotected sex became routine after an unplanned event (41.2 %).
Analyses for sexual agreements were conducted at the individual- and dyadic-level. Examination of individual responses on whether or not the couple had established a sexual agreement revealed that 32 (80 %) participants reported having an agreement with their romantic partner. Of these participants, 78.1 % (25 of 32 participants) classified their agreement as monogamous (i.e., cannot have sex with outside partners), 18.8 % (6 of 32 participants) reported an agreement in which they could have sex with outside partners with restrictions (e.g., limits on sexual behaviors, use of condoms, degree of intimacy, etc.), and one participant noted an agreement in which he could have sex with outside partners without restrictions.
Examination of the dyadic data showed that two couples reported not having a sexual agreement (100 % concordant partner responses). Of the remaining 18 dyads, the partners in 11 (61.1 %) couples were concordant in their sexual agreement reports and 7 (38.9 %) couples were discordant. In five of these seven discordant couples, there were disagreements about monogamy. That is, one partner believed their relationship to be monogamous while the other indicated there was no agreement (in three couples) or that they could have sex with outside partners with some restrictions (in two couples).
Among the 32 participants who reported having a sexual agreement with their romantic partner, the most frequently endorsed reasons for making the agreement included to protect both individuals from HIV and STIs (68.8 and 81.3 %, respectively), to protect and strengthen the relationship (78.1 %), and to be honest in the relationship (71.9 %). Among all possible response options, to prevent boredom, to be more sexually adventurous, and to have satisfying sex were the least endorsed reasons (12.5, 18.8, and 25 %, respectively).
Qualitative and Mixed Methods Findings
The qualitative data were merged with the quantitative data in Dedoose and analyzed thematically (Miles & Huberman, 1994). High dyadic agreement on the quantitative relationship scales yielded limited variability across couples, thus prohibiting a meaningful analytic grouping of couples based on relationship characteristics (e.g., satisfaction, investment). As such, we divided the couples into three groups based on their relationship length for the mixed methods analyses: (1) less than 1 year (n = 7 couples; 29 excerpts); (2) 1–3 years (n = 8 couples; 27 excerpts); and (3) greater than 3 years (n = 5 couples; 16 excerpts). This analytic decision was based on our previous research identifying relationship length as a risk factor for unprotected sex among YMSM (Mustanski et al., 2011b; Newcomb et al., 2013).
Across the 20 transcripts of interviews with male couples, the code “reasons for unprotected sex” was applied 349 times. Sub-codes, developed through grounded theory analysis, included being in the heat of the moment (18 applications), making a connection with their partner (13 applications), lacking motivation to practice safe sex (10 applications), having a negative impact on pleasure (10 applications), and having technical or access issues with condoms (6 applications). In addition, the most frequent co-occurring codes applied to the same excerpts coded as reasons for unprotected sex were condoms (64 applications), getting tested or knowing each other’s HIV status (28 applications), and having trust and faith in their partner (30 applications). Since condom use and HIV testing were included in the code definition for reasons for unprotected sex, only the trust/faith code was further analyzed. This code was defined as any explicit mention of trust, faith, or a metaphor for trust/faith, including how trust/faith may develop over time. This code also captured fear and reservations as they relate to opening up to and trusting a partner, in addition to reports of having difficulty trusting other people.
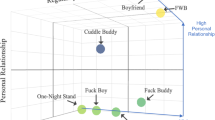
Dedoose software was used to analyze code application (i.e., reasons for unprotected sex) by descriptor (i.e., relationship length). Figure 1 presents the percentage of excerpts that were associated with a particular code separately for each group. These data were normalized because there were unequal numbers of cases in each group. The normalization function operates by assigning a weight of “1” to the group with the largest number of members (basis group) and then assigns weights to the other groups as a function of the numeric relation between the number of members in the group to that of the number of members in the “basis” group (Dedoose, 2012). These weights were then used to adjust the number of raw counts to accomplish ratio equivalence across group and the weighted percentage was calculated based on these adjusted counts. This normalization is necessary because the graphical representation for code application frequency by group is relatively meaningless if there are unequal numbers of individual cases across each sub-group.
As shown in Fig. 1, among couples whose relationship length was less than 1 year, codes for condom access/technical difficulties (four excerpts), being in the heat of the moment (seven excerpts), and trust/faith (12 excerpts) were applied more frequently as compared to the other two groups. For example, the code for condom access/technical difficulties was applied in over 85.7 % of the excerpts from relationships lasting less than 1 year and in 14.3 % of the excerpts from the 1 to 3 year relationships. This code was never applied in the longer-term relationship group as a reason for unprotected sex. In the following quotation, the couple described the feeling of having unprotected sex in the heat of the moment with condoms not being readily accessible. They convey the excitement and feeling of wanting to have sex under time and resource constraints:
-
Participant A (A): Just like the spur of the moment, just like… “We got 15 min, let’s make it,” you know? (laughter)
-
Interviewer (I): Make it happen. So, condoms were available, not available?
-
A: Like not accessible.
-
I: It was heat of the moment, like not expected?
-
A: Yeah, it was like, like right, it wasn’t expected like, it wasn’t like planned or nothing.
-
Participant B(B): Let’s just freak right now!
-
(Couple 38: both 18 years old; relationship length, less than 1 year)
In the following quotation, both partners discussed issues with condoms breaking and the futility of continuing condom use:
-
A: …Like we’re using condoms and stuff like that in the beginning, um, but they just kept breaking (laughter). And, or, like it was a time when he kept putting on condoms in the same night and they just kept popping and popping and popping, and I was like, “Well, if it’s gonna keep popping, you might as well just continue doing what you was doing.” I mean…so.
-
B: Naw, that ain’t what you said. We had another one. I threw that one on the floor, across my shoulder (both laugh).
-
(Couple 1: ages 22 and 21 years old; relationship length, less than 1 year)
Couples in relationships lasting over 3 years discussed a different set of reasons for unprotected sex compared to groups with shorter relationships. Among these participants, lack of motivation (four excerpts), connection with partner (four excerpts), and negative impact on sexual pleasure (three excerpts) were the most frequently applied codes. In the following quotation, the couple described having unprotected sex as a form of intimacy to demonstrate dedication to each other. One of the partners also clarified that testing negative for HIV and being monogamous contributed to their decision to have unprotected sex:
-
A: Um, that was, I think, it is a trust and love like kind of thing because you want to prove to your partner you’re dedicated and monogamous at that point, and you’re like willing to be more intimate with them.
-
B: Yeah, I mean I think, right, it goes back to the communication as well. We’re not sleeping with anyone else and we haven’t for like a long period of time. Um, and we’ve both been tested so we both know that we’re negative and don’t have any other like, I don’t know, issues. Um, so it just kinda made sense, at that point, when there wasn’t any outstanding reason.
-
(Couple 12: ages 23 and 26 years old; relationship length, greater than 3 years)
Across the three groups, codes for trust/faith and connection with partner were commonly applied as reasons for unprotected sex. In the following quotation from a serodiscordant couple that reported consistent condom use, one participant responded to the interviewer’s question, “When is it ok, if ever, for couples to stop using condoms?”:
-
B: Umm…to me, it’s…I think that’s something like much older in life, when they’re like married, like kids, and there’s like you know that there’s complete, absolute, like pure trust. Um, and as far as like somebody like, like us, where there is one positive and one negative, like never…
-
(Couple 36: both 20 years old; relationship length, less than 1 year)
The next quote describes monogamy, commitment, and trust as reasons for not using condoms from a couple dating between 1 and 3 years. The participants revealed that they did not discuss their decision to have unprotected sex in their relationship.
-
B: Well, um, we’re monogamous. And uh…we’re in a committed relationship so, um, and we’ve, we’ve been tested and we trust each other so, um, we haven’t…
-
I: Have you ever [used condoms]?
-
B: No.
-
I: Ok. And what are the reasons that you don’t use condoms?
-
A: We never really discussed it. Really. We just…
-
B: Well, I’m comfortable with him, so you know.
-
A: Yeah.
-
(Couple 19: 20 and 23 years old; relationship length, 1–3 years)
Discussion
This study aimed to describe relational characteristics of young male couples, as well as to examine HIV risk among YMSM in serious relationships. With regard to relationship factors, couples’ agreement scores were generally high and favorable on measures of satisfaction, investment, trust, love, and commitment. These findings were consistent with previous research which has shown positive relationship characteristics among gay and lesbian couples (Kurdek, 2005). With regard to HIV risk, YMSM in this study reported infection risks based on individual-level (i.e., lack of awareness of their own or their serious partner’s HIV status) and dyadic-level variables (i.e., inconsistent use of condoms, discrepancies in their sexual agreements pertaining to monogamy). Below, we discuss each of these areas in the context of the quantitative and qualitative findings in this mixed methods study.
Approximately one-third of couples reported that they did not use condoms for their first anal intercourse together and a similar proportion indicated that they did not use condoms in the last 6 months. For the participants who reported no or irregular condom use in the past 6 months, expressing love, trust, and commitment were the most frequently cited reasons for not using condoms. These findings were consistent with previous research that suggests a desire for intimacy in romantic relationships is achieved through having unprotected sex (Carballo-Diéguez & Dolezal, 1996; Eisenberg et al., 2011; McLean et al., 1994; Remien et al., 1995). For example, in qualitative interviews with a sample of African-American MSM, Malebranche, Fields, Bryant, and Harper (2009) reported that the decision to forego condom use was viewed as an intimate act and trust was the most commonly cited factor influencing personal decisions to have unprotected sex. In research with YMSM, Eisenberg et al. (2011) also reported that young men’s sexual practices promoted intimacy with, and communicated trust to, sexual partners.
The qualitative analyses explored thematic differences in reasons for unprotected sex according to couples’ relationship length. Compared to couples in longer-term relationships, those dating for less than 1 year frequently described condom access/technical difficulties, being in the heat of the moment, and trust/faith as reasons for unprotected sex. While previous research has documented high levels of condom-related errors (e.g., using oil-based lubricant) and failures (e.g., breakage) among young, ethnically and racially diverse MSM (DuBois, Emerson, & Mustanski, 2011), the current study highlighted that problems with condom access were most common in shorter-term relationships. For YMSM in the formative stages of a romantic relationship, it is likely that norms have not yet been established for condom access and use. In contrast to shorter-term couples, it is likely that longer-term couples that consistently use condoms have developed behavioral routines to overcome condom access issues for their sexual activities. Notably, couples in relationships lasting longer than 3 years did not report condom difficulties and few indicated being in the heat of the moment as a reason for unprotected sex.
Differences in reasons for unprotected sex described by men in shorter- and longer-term relationships reflect issues associated with relationship maturation. Research suggests that, over the course of romantic relationships, decreases in condom use may be attributed to increased knowledge about the partner and the perception of decreased risk if there are no observable signs of STIs (Fortenberry et al., 2002). For the longer-term couples, unprotected sex was associated with a lack of motivation to use condoms and the desire to connect with their partner. While some couples reported decreased motivation to use condoms after testing negative for HIV and other STIs, other couples describing waning motivation for condom use after having unprotected sex. These men believed that resuming condom use was pointless, referring to the fact that condom failures would persist or that they may have already placed themselves at risk for infection. Additionally, previous research has indicated that motivations for sex change over time within relationships, with issues of trust and intimacy receiving greater priority in on-going relationships (Cooper, Shapiro, & Powers, 1998). In this study, it was somewhat surprising that there were no major differences in the themes of trust across relationship duration. However, discussions of trust/faith were prevalent among YMSM in shorter-term relationships, suggesting that trust may be associated with unprotected sex much earlier than the 1 year cut-off used in our analyses.
Along with emotional intimacy as a reason for unprotected sex, having a negative HIV status and being in a monogamous relationship were highly cited reasons for not using condoms among YMSM. However, in 30 % of the couples, one member of the partnership did not know or was unsure of his partner’s HIV status and nearly 40 % of couples were discordant in their understanding of their current sexual agreement. This high proportion of couple discordance among YMSM was similar to recent research with adult gay male couples in which less than half of the dyads were concordant about having a sexual agreement, type of agreement, and adherence to the agreement (Mitchell et al., 2012). However, other studies have found much lower rates of discordance in samples of adult male couples (Hoff & Beougher, 2010; Parsons et al., 2012).The divergent rates of discordance across studies may be attributed to differences in assessing and reporting types of sexual agreements. Within partnerships, however, discordance may reflect nuanced definitions of monogamy that couples adopt for themselves (Hoff & Beougher, 2010). For example, couples just beginning their relationships may be in the process of negotiating their agreements; as such, neither partner may fully understand what their sexual agreement is and how it has evolved over time (Hoff & Beougher, 2010). From a developmental perspective, discordant sexual agreements may reflect poor communication skills among YMSM on the topics of sexual exclusivity, condom use, and HIV serostatus (Hays et al., 1997; Trussler, Perchal, & Barker, 2000). This discordance in agreements may increase HIV transmission risk among YMSM in serious relationships (Davidovich et al., 2004; Hoff & Beougher, 2010; Parsons et al., 2012) and further research understanding sexual agreements is critical for the implementation of interventions that may or may not assume agreement among couples.
In consideration of partner and relationship characteristics associated with HIV risk in this study, some researchers have argued that the estimated risks of having unprotected sex represent rational sexual decision-making (Pinkerton & Abramson, 1992; Smith et al., 2012). Smith et al. posited that condom use is a socially constructed tool to protect against disease and that condoms are typically used in casual relationships. As such, continued condom use in relationships that are characterized as serious and committed may be perceived as irrational. Further, the decision not to use condoms may serve to reinforce the belief that the relationship is stable and enduring. Unfortunately, for YMSM who engage in multiple, short-term relationships perceived to be serious (Mustanski et al., 2011b), their desire to achieve lasting intimacy by having unprotected sex may increase their risk of exposure to HIV.
Limitations, Strengths, and Implications
Our results must be interpreted in the context of study limitations. First, findings from this convenience sample of racially and ethnically diverse YMSM in serious relationships with other men in the Midwest may not be generalizable to all young male couples. Second, the dyadic interview data were based on retrospective accounts of sexual activity, condom use behaviors, and perceptions of risk. As such, recollections of past relationship and sexual experiences may have been restructured over the course of the relationship due to fluctuating developmental perspectives. Third, low internal consistency of the Investment Model Scale (Lehmiller & Agnew, 2006; Rusbult et al., 1998) suggests that further research is needed to validate measures of relationship investment among YMSM. Fourth, the HIV serostatus of MSM in serious relationships adds complexity to the process of negotiating condom use and sexual agreements. Given the few serodiscordant couples in this study, further research is necessary with larger samples to examine the difficulty of negotiating sex with a discordant partner and the effects of stress on the couple’s physical and psychological health (Hoff et al., 2009). Lastly, the mixed methods analyses examining reasons for unprotected sex by relationship length were conducted with relatively small numbers of participants in each group; thus, we did not have the power to perform tests for statistical significance and only percentages were reported. Nevertheless, we believe describing these patterns is useful for the purposes of hypothesis generation for future larger-scale studies.
Acknowledging these limitations, this study had a number of strengths. First, our sample was racially and ethnically diverse and included relationships that varied by partner age, sexual orientation, and relationship length. Second, the use of both quantitative and qualitative dyadic data enabled a rich understanding of the relationship dynamics among YMSM in serious relationships. Couple-level analyses of partner and relationship characteristics underscore that sexual risk occurs in interpersonal contexts and that intervention must address these relational factors. Third, survey data were collected via computer, which may have increased participants’ comfort with reporting sensitive data (e.g., sexual concurrency). This information may not be disclosed otherwise in interviews of couples due to a participants’ reluctance to share sensitive information, such as infidelity, in front of their partners. Lastly, our coding team achieved excellent inter-rater agreement across the 20 dyadic interviews.
Several implications for future research and intervention stem from this study. The sexual decision-making processes described by YMSM in this research are consistent with health behavior theories that include an evaluation of the negative and positive aspects of a behavior, along with the expected outcome of the behavior (Noar & Zimmerman, 2005). Unfortunately, the major focus of these theories is on individuals and few account for variation across situations, contexts, or populations. Understanding this ecology is of particular importance for YMSM in serious relationships because many reported having unprotected sex “in the heat of the moment.” Examining emotional and situational states (i.e., “hot cognitions”) that inhibit decision making and safer sex practices are necessary for the sexual health of young male couples (Mustanski, 2007).
With a focus on relationships, the Information Motivation and Behavioral Skills (IMB) model is one of the few behavior change frameworks that has been adapted for HIV research in dyadic partnerships (Fisher & Fisher, 2002; Fisher, Fisher, Williams, & Malloy, 1994; Misovich et al., 1997). The IMB model draws on implicit personality theory in which HIV risk assessments are based on visible or inferred partner characteristics and includes HIV prevention heuristics about sexual risk (e.g., “Known partners are safe partners.”). The model also includes attitudes towards preventive behavior within relationships, perceived vulnerability, and self-efficacy to negotiate preventive behaviors (e.g., condom use, HIV testing). The IMB model has not been evaluated with young same sex couples, but has been tested with individual sexual minority youth (Fisher, 2012) and heterosexual couples (Harman & Amico). For example, Harman and Amico found that the Relationship-Oriented IMB model significantly predicted condom use behaviors in a sample of 75 heterosexual couples.
There are two areas of interest for adapting this model for YMSM in serious relationships. First, as found in this study, MSM actively estimated sexual risk in their relationships; they acknowledged that condoms protect against HIV, but they often had other motivations to have unprotected sex. As such, adapting the IMB model for YMSM could target couples’ norms and attitudes about condom use to increase motivation and subsequent condom use behaviors. Second, associations between constructs in the IMB model may vary for individuals in different types of relationships (Harman & Amico, 2009). For YMSM, these relationships types may be defined by sexual agreements or couple serostatus, among other dyadic factors. Based on these relationship typologies, intervention content could be tailored to the specific needs of the couple.
HIV preventive interventions for YMSM must also focus on relationship formation and maintenance, in addition to delivering sexual health information. It is vital for young men to know what typical relationship trajectories are for young adults and to understand the long-term consequences of sexual decision-making in light of “hot cognitions” and the desire to achieve intimacy in romantic relationships. Because the dominant paradigm in public health recommends condom use at all stages in relationships, young men are left with little information about how to navigate decisions about when and how to stop using condoms in their long-term relationships. As relationships become more serious with increased desire for intimacy, the meanings of condom use in relationships may also shift. In casual relationships, condoms serve as a barrier to protect against HIV and STIs, however, in serious relationships, condoms may represent barriers to intimacy and trust (Carballo-Dieguez et al., 2011; Golub et al., 2012). Young MSM must be equipped with the knowledge and skills to navigate these changes in their relationships. It is an unrealistic expectation that condom use will persist over the life of the partnership for couples who are emotionally intimate, get regular HIV/STI testing, and have established sexual agreements to protect both partners in the relationship. To this end, couples-based intervention content should include skill development focused on improving communication within relationships, creating and adhering to sexual agreements, and introducing routine couples-based HIV testing (Stephenson et al., 2011) and other biomedical interventions (e.g., PrEP) (Underhill, Operario, Skeer, Mimiaga, & Mayer, 2010).
Conclusion
To our knowledge, this research was one of the first couples-based studies focusing on ethnically and racially diverse YMSM in serious relationships. Several findings from this study were consistent with previous research with YMSM and couples research with samples of older MSM. First, examination of relationship-level characteristics (e.g., length of relationship) underscored the influence of intimacy, monogamy, and condom related-problems on unprotected sex among young male couples. Second, this study found important discrepancies in sexual agreements between partners in the current sample of YMSM. And third, in most reports of unprotected sex, even in those described as being in the heat of the moment, couples often described a decision-making process in which the gains associated with unprotected sex (e.g., establishing trust) outweighed the risks for infection. Taken together, our mixed methods approach extends the scant social science and public health knowledge on the relationship characteristics that place YMSM at risk for HIV infection. As researchers and interventionists strengthen their efforts to reduce HIV risk behaviors in relationships through encouraging condom use and repeat HIV testing, innovative approaches are needed that focus on developmental, dyadic, and contextual variables. Interventions that focus on relationship formation, duration, and quality may improve overall health among YMSM, in addition to decreasing their risk for HIV infection.
References
Appleby, P. R., Miller, L. C., & Rothspan, S. (1999). The paradox of trust for male couples: When risking is a part of loving. Personal Relationships, 6, 81–93. doi:10.1111/j.1475-6811.1999.tb00212.x.
Axinn, W. G., & Pearce, L. D. (2006). Mixed method data collection strategies. Cambridge: Cambridge University Press.
Bauermeister, J. A., Carballo-Diéguez, A., Ventuneac, A., & Dolezal, C. (2009). Assessing motivations to engage in intentional condomless anal intercourse in HIV-risk contexts (“bareback sex”) among men who have sex with men. AIDS Education and Prevention, 21, 156–168. doi:10.1521/aeap.2009.21.2.156.
Bingham, T. A., Harawa, N. T., Johnson, D. F., Secura, G. M., MacKellar, D. A., & Valleroy, L. A. (2003). The effect of partner characteristics on HIV infection among African American men who have sex with men in the Young Men’s Survey, Los Angeles, 1999–2000. AIDS Education and Prevention, 15(Suppl. 1A), 39–52. doi:10.1521/aeap.15.1.5.39.23613.
Blais, M. (2006). Vulnerability to HIV among regular male partners and the social coding of intimacy in modern societies. Culture Health & Sexuality, 8, 31–44. doi:10.1080/13691050500391232.
Boardman, F., Griffiths, F., Kokanovic, R., Potiriadis, M., Dowrick, C., & Gunn, J. (2011). Resilience as a response to the stigma of depression: A mixed methods analysis. Journal of Affective Disorders, 135, 267–276. doi:10.1016/j.jad.2011.08.007.
Boulton, M., McLean, J., Fitzpatrick, R., & Hart, G. (1995). Gay men’s accounts of unsafe sex. AIDS Care, 7, 619–630. doi:10.1080/09540129550126263.
Bruce, D., Harper, G. W., Fernandez, M. I., Jamil, O. B., & Adolescent Medicine Trials Network for HIV/AIDS Interventions. (2012). Age-concordant and age-discordant sexual behavior among gay and bisexual male adolescents. Archives of Sexual Behavior, 41, 441–448. doi:10.1007/s10508-011-9730-8.
Carballo-Diéguez, A., & Dolezal, C. (1996). HIV risk behaviors and obstacles to condom use among Puerto Rican men in New York City who have sex with men. American Journal of Public Health, 86, 1619–1622. doi:10.2105/ajph.86.11.1619.
Carballo-Dieguez, A., Ventuneac, A., Dowsett, G. W., Balan, I., Bauermeister, J., Remien, R. H., … Mabragana, M. (2011). Sexual pleasure and intimacy among men who engage in “bareback sex”. AIDS and Behavior, 15(Suppl. 1), S57–S65. doi:10.1007/s10461-011-9900-7.
CDC. (2012a). Diagnoses of HIV infection and AIDS among adolescents and young adults in the United States and 5 U.S. dependent areas, 2006–2009. Retrieved July 24, 2013 from http://www.cdc.gov/hiv/topics/surveillance/resources/reports/.
CDC. (2012b). HIV surveillance-epidemiology of HIV infection (through 2011). Retrieved September 5, 2013 from http://www.cdc.gov/hiv/topics/surveillance/resources/slides/general/index.htm.
Cicchetti, D. V. (1994). Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychological Assessment, 6, 284–290. doi:10.1037/1040-3590.6.4.284.
Cooper, M. L., Shapiro, C. M., & Powers, A. M. (1998). Motivations for sex and risky sexual behavior among adolescents and young adults: A functional perspective. Journal of Personality and Social Psychology, 75, 1528–1558. doi:10.1037//0022-3514.75.6.1528.
D’Augelli, A., Rendina, H. J., Sinclair, K., & Grossman, A. (2008). Lesbian and gay youth’s aspirations for marriage and raising children. Journal of LGBT Issues in Counseling, 1, 77–98. doi:10.1300/J462v01n04_06.
Davidovich, U., de Wit, J. B., & Stroebe, W. (2000). Assessing sexual risk behaviour of young gay men in primary relationships: The incorporation of negotiated safety and negotiated safety compliance. AIDS, 14, 701–706.
Davidovich, U., de Wit, J. B., & Stroebe, W. (2004). Behavioral and cognitive barriers to safer sex between men in steady relationships: Implications for prevention strategies. AIDS Education and Prevention, 16, 304–314. doi:10.1521/aeap.16.4.304.40398.
Davidovich, U., de Wit, J. B., & Stroebe, W. (2006). Relationship characteristics and risk of HIV infection: Rusbult’s investment model and sexual risk behavior of gay men in steady relationships. Journal of Applied Social Psychology, 36, 22–40. doi:10.1111/j.0021-9029.2006.00002.x.
De Vries, H., Elliott, M. N., Kanouse, D. E., & Teleki, S. S. (2008). Using pooled kappa to summarize interrater agreement across many items. Field Methods, 20, 272–282. doi:10.1177/1525822x08317166.
de Vroome, E. M. M., Stroebe, W., Sandfort, T. G. M., De Wit, J., & Van Griensven, G. (2000). Safer sex in social context: Individualistic and relational determinants of AIDS-preventive behavior among gay men. Journal of Applied Social Psychology, 30, 2322–2340. doi:10.1111/j.1559-1816.2000.tb02439.x.
Dedoose. (2012). Web application for managing, analyzing, and presenting qualitative and mixed method data (Version 4.5.91). Los Angeles, CA: SocioCultural Research Consultants.
DeHaan, S., Kuper, L. E., Magee, J. C., Bigelow, L., & Mustanski, B. S. (2013). The interplay between online and offline explorations of identity, relationships, and sex: A mixed-methods study with LGBT youth. Journal of Sex Research, 50, 421–434. doi:10.1080/00224499.2012.661489.
DuBois, S. N., Emerson, E., & Mustanski, B. (2011). Condom-related problems among a racially diverse sample of young men who have sex with men. AIDS and Behavior, 15, 1342–1346. doi:10.1007/s10461-010-9862-1.
Eisenberg, A., Bauermeister, J. A., Pingel, E., Johns, M. M., & Santana, M. L. (2011). Achieving safety safer sex, communication, and desire among young gay men. Journal of Adolescent Research, 26, 645–669. doi:10.1177/0743558411402342.
Elford, J., Bolding, G., Maguire, M., & Sherr, L. (1999). Sexual risk behaviour among gay men in a relationship. AIDS, 13, 1407–1411. doi:10.1097/00002030-199907300-00019.
Fisher, C. M. (2012). Adapting the Information–Motivation–Behavioral Skills model: Predicting HIV-related sexual risk among sexual minority youth. Health Education & Behavior, 39, 290–302. doi:10.1177/1090198111406537.
Fisher, J. D., & Fisher, W. A. (2002). The information-motivation-behavioral skills model. In R. J. DiClemente, R. A. Crosby, & M. C. Kegler (Eds.), Emerging theories in health promotion practice and research: Strategies for improving public health (pp. 40–70). San Francisco: Jossey-Bass.
Fisher, J. D., Fisher, W. A., Williams, S. S., & Malloy, T. E. (1994). Empirical tests of an Information–Motivation–Behavioral Skills model of AIDS-preventive behavior with gay men and heterosexual university students. Health Psychology, 13, 238–250. doi:10.1037/0278-6133.13.3.238.
Fortenberry, J. D., Tu, W. Z., Harezlak, J., Katz, B. P., & Orr, D. P. (2002). Condom use as a function of time in new and established adolescent sexual relationships. American Journal of Public Health, 92, 211–213. doi:10.2105/Ajph.92.2.211.
Furman, W. (1994). Dating history questionnaire. Unpublished measure, University of Denver, Denver, CO.
Glaser, B. G., & Strauss, A. L. (1967). The discovery of grounded theory; strategies for qualitative research. Chicago, IL: Aldine Publishing Co.
Golub, S. A., Starks, T. J., Payton, G., & Parsons, J. T. (2012). The critical role of intimacy in the sexual risk behaviors of gay and bisexual men. AIDS and Behavior, 16, 626–632. doi:10.1007/s10461-011-9972-4.
Goodreau, S. M., Carnegie, N. B., Vittinghoff, E., Lama, J. R., Sanchez, J., Grinsztejn, B., … Buchbinder, S. P. (2012). What drives the US and Peruvian HIV epidemics in men who have sex with men (MSM)? PLoS ONE, 7(11), e50522. doi:10.1371/journal.pone.0050522.
Halkitis, P. N., & Parsons, J. T. (2003). Intentional unsafe sex (barebacking) among HIV-positive gay men who seek sexual partners on the internet. AIDS Care, 15, 367–378. doi:10.1080/0954012031000105423.
Harawa, N. T., Greenland, S., Bingham, T. A., Johnson, D. F., Cochran, S. D., Cunningham, W. E., … Valleroy, L. A. (2004). Associations of race/ethnicity with HIV prevalence and HIV-related behaviors among young men who have sex with men in 7 urban centers in the United States. Journal of Acquired Immune Deficiency Syndromes, 35, 526–536. doi:10.1097/00126334-200404150-00011.
Harman, J. J., & Amico, K. R. (2009). The relationship-oriented Information–Motivation–Behavioral Skills model: A multilevel structural equation model among dyads. AIDS and Behavior, 13, 173–184. doi:10.1007/s10461-007-9350-4.
Harris, K. M., Halpern, C. T., Whitsel, E., Hussey, J., Tabor, J., Entzel, P., & Udry, J. R. (2009). The national longitudinal study of adolescent health: Research design. Retrieved October 4, 2012 from http://www.cpc.unc.edu/projects/addhealth/design.
Hart, T., Peterson, J. L., & The Community Intervention Trial for Youth Study Team. (2004). Predictors of risky sexual behavior among young African American men who have sex with men. American Journal of Public Health, 94, 1122–1124. doi:10.2105/AJPH.94.7.1122.
Hays, R. B., Kegeles, S. M., & Coates, T. J. (1997). Unprotected sex and HIV risk taking among young gay men within boyfriend relationships. AIDS Education and Prevention, 9, 314–329.
Hendrick, S. S. (1988). A generic measure of relationship satisfaction. Journal of Marriage and the Family, 50, 93–98. doi:10.2307/352430.
Hoff, C. C., & Beougher, S. C. (2010). Sexual agreements among gay male couples. Archives of Sexual Behavior, 39, 774–787. doi:10.1007/s10508-008-9393-2.
Hoff, C. C., Beougher, S. C., Chakravarty, D., Darbes, L. A., & Neilands, T. B. (2010). Relationship characteristics and motivations behind agreements among gay male couples: Differences by agreement type and couple serostatus. AIDS Care, 22, 827–835. doi:10.1080/09540120903443384.
Hoff, C. C., Chakravarty, D., Beougher, S. C., Darbes, L. A., Dadasovich, R., & Neilands, T. B. (2009). Serostatus differences and agreements about sex with outside partners among gay male couples. AIDS Education and Prevention, 21, 25–38. doi:10.1521/aeap.2009.21.1.25.
Hoff, C. C., Coates, T. J., Barrett, D. C., Collette, L., & Ekstrand, M. (1996). Differences between gay men in primary relationships and single men: Implications for prevention. AIDS Education and Prevention, 8, 546–559.
Janis, I. L., & Mann, L. (1977). Decision making: A psychological analysis of conflict, choice, and commitment. New York: Free Press.
Kippax, S., Noble, J., Prestage, G., Crawford, J. M., Campbell, D., Baxter, D., & Cooper, D. (1997). Sexual negotiation in the AIDS era: Negotiated safety revisited. AIDS, 11, 191–197.
Kippax, S., Slavin, S., Ellard, J., Hendry, O., Richters, J., Grulich, A., & Kaldor, J. (2003). Seroconversion in context. AIDS Care, 15, 839–852.
Kurdek, L. A. (2005). What do we know about gay and lesbian couples? Current Directions in Psychological Science, 14, 251–254. doi:10.1111/j.0963-7214.2005.00375.x.
Kuttler, A. F., & La Greca, A. M. (2004). Linkages among adolescent girls’ romantic relationships, best friendships, and peer networks. Journal of Adolescence, 27, 395–414. doi:10.1016/j.adolescence.2004.05.002.
Landis, J. R., & Koch, G. G. (1977). The measurement of observer agreement for categorical data. Biometrics, 33, 159–174. doi:10.2307/2529310.
Lehmiller, J. J., & Agnew, C. R. (2006). Marginalized relationships: The impact of social disapproval on romantic relationship commitment. Personality and Social Psychology Bulletin, 32, 40–51. doi:10.1177/0146167205278710.
Magee, J. C., Bigelow, L., Dehaan, S., & Mustanski, B. S. (2012). Sexual health information seeking online: A mixed-methods study among lesbian, gay, bisexual, and transgender young people. Health Education and Behavior, 39, 276–289. doi:10.1177/1090198111401384.
Malebranche, D. J., Fields, E. L., Bryant, L. O., & Harper, S. R. (2009). Masculine socialization and sexual risk behaviors among Black men who have sex with men: A qualitative exploration. Men and Masculinities, 12, 90–112. doi:10.1177/1097184x07309504.
McLean, J., Boulton, M., Brookes, M., Lakhani, D., Fitzpatrick, R., Dawson, J., … Hart, G. (1994). Regular partners and risky behaviour: Why do gay men have unprotected intercourse? AIDS Care, 6, 331–341.
McNeal, J. L. (1997). The association of idealization and intimacy factors with condom use in gay male couples. Journal of Clinical Psychology in Medical Settings, 4, 437–451. doi:10.1023/A:1026209603522.
Miles, M. B., & Huberman, A. M. (1994). Qualitative data analysis: An expanded sourcebook (2nd ed.). Thousand Oaks, CA: Sage.
Misovich, S. J., Fisher, J. D., & Fisher, W. A. (1997). Close relationships and elevated HIV risk behavior: Evidence and possible underlying psychological processes. Review of General Psychology, 1, 72–107. doi:10.1037/1089-2680.1.1.72.
Mitchell, J. W., Harvey, S. M., Champeau, D., Moskowitz, D. A., & Seal, D. W. (2012). Relationship factors associated with gay male couples’ concordance on aspects of their sexual agreements: Establishment, type, and adherence. AIDS and Behavior, 16, 1560–1569. doi:10.1007/s10461-011-0064-2.
Morris, M., Zavisca, J., & Dean, L. (1995). Social and sexual networks: Their role in the spread of HIV/AIDS among young gay men. AIDS Education and Prevention, 7(Suppl. 5), 24–35.
Mustanski, B. (2007). The influence of state and trait affect on HIV risk behaviors: A daily diary study of MSM. Health Psychology, 26, 618–626. doi:10.1037/0278-6133.26.5.618.
Mustanski, B., Garofalo, R., & Emerson, E. (2010). Mental health disorders, psychological distress, and suicidality in a diverse sample of lesbian, gay, bisexual, and transgender youths. American Journal of Public Health, 100, 2426–2432. doi:10.2105/AJPH.2009.178319.
Mustanski, B., Johnson, A., Garofalo, R., Ryan, D., & Birkett, M. (2012). Perceived likelihood of using HIV pre-exposure prophylaxis medications among young men who have sex with men. AIDS and Behavior, 17, 2173–2179. doi:10.1007/s10461-012-0359-y.
Mustanski, B., Lyons, T., & Garcia, S. C. (2011a). Internet use and sexual health of young men who have sex with men: A mixed-methods study. Archives of Sexual Behavior, 40, 289–300. doi:10.1007/s10508-009-9596-1.
Mustanski, B., Newcomb, M. E., & Clerkin, E. M. (2011b). Relationship characteristics and sexual risk-taking in young men who have sex with men. Health Psychology, 30, 597–605. doi:10.1037/a0023858.
Mustanski, B., Newcomb, M. E., DuBois, S. N., Garcia, S. C., & Grov, C. (2011c). HIV in young men who have sex with men: A review of epidemiology, risk and protective factors, and interventions. Journal of Sex Research, 48, 218–253. doi:10.1080/00224499.2011.558645.
Neilands, T. B., Chakravarty, D., Darbes, L. A., Beougher, S. C., & Hoff, C. C. (2010). Development and validation of the sexual agreement investment scale. Journal of Sex Research, 47, 24–37. doi:10.1080/00224490902916017.
Newcomb, M. E., & Mustanski, B. (2013). Racial differences in same-race partnering and the effects of sexual partnership characteristics on HIV risk in MSM: A prospective sexual diary study. Journal of Acquired Immune Deficiency Syndromes, 62, 329–333. doi:10.1097/QAI.0b013e31827e5f8c.
Newcomb, M. E., Ryan, D. T., Garofalo, R., & Mustanski, B. (2013). The effects of sexual partnership and relationship characteristics on three sexual risk variables in young men who have sex with men. Archives of Sexual Behavior. doi:10.1007/s10508-013-0207-9.
Noar, S. M., & Zimmerman, R. S. (2005). Health behavior theory and cumulative knowledge regarding health behaviors: Are we moving in the right direction? Health Education Research, 20, 275–290. doi:10.1093/her/cyg113.
Parsons, J. T., Schrimshaw, E. W., Bimbi, D. S., Wolitski, R. J., Gómez, C. A., & Halkitis, P. N. (2005). Consistent, inconsistent, and non-disclosure to casual sexual partners among HIV-seropositive gay and bisexual men. AIDS, 19, S87–S97. doi:10.1097/01.aids.0000167355.87041.63.
Parsons, J. T., Starks, T. J., DuBois, S., Grov, C., & Golub, S. A. (2011). Alternatives to monogamy among gay male couples in a community survey: Implications for mental health and sexual risk. Archives of Sexual Behavior, 42, 303–312. doi:10.1007/s10508-011-9885-3.
Parsons, J. T., Starks, T. J., Gamarel, K. E., & Grov, C. (2012). Non-monogamy and sexual relationship quality among same-sex male couples. Journal of Family Psychology, 26, 669–677. doi:10.1037/a0029561.
Peplau, L. A., & Fingerhut, A. W. (2007). The close relationships of lesbian and gay men. Annual Review of Psychology, 58, 405–424. doi:10.1146/annurev.psych.58.110405.085701.
Pinkerton, S. D., & Abramson, P. R. (1992). Is risky sex rational? Journal of Sex Research, 29, 561–568.
Prestage, G., Jin, F., Zablotska, I., Grulich, A., Imrie, J., Kaldor, J., … Kippax, S. (2008). Trends in agreements between regular partners among gay men in Sydney, Melbourne and Brisbane, Australia. AIDS and Behavior, 12, 513–520. doi:10.1007/s10461-007-9351-3.
Remien, R. H., Carballo-Dieguez, A., & Wagner, G. (1995). Intimacy and sexual risk behaviour in serodiscordant male couples. AIDS Care, 7, 429–438. doi:10.1080/09540129550126380.
Remien, R. H., Wagner, G., Dolezal, C., & Carballo-Diéguez, A. (2002). Factors associated with HIV sexual risk behavior in male couples of mixed HIV status. Journal of Psychology & Human Sexuality, 13(2), 31–48. doi:10.1300/J056v13n02_03.
Robles, T. F., & Kiecolt-Glaser, J. K. (2003). The physiology of marriage: Pathways to health. Physiology & Behavior, 79, 409–416. doi:10.1016/S0031-9384(03)00160-4.
Rusbult, C. E., Martz, J. M., & Agnew, C. R. (1998). The Investment Model Scale: Measuring commitment level, satisfaction level, quality of alternatives, and investment size. Personal Relationships, 5, 357–391. doi:10.1111/j.1475-6811.1998.tb00177.x.
Smith, J. L., Fenwick, J., Skinner, R., Hallet, J., Merriman, G., & Marshall, L. (2012). Sex, condoms and sexually transmissible infections: A qualitative study of sexual health in young Australian men. Archives of Sexual Behavior, 41, 487–495. doi:10.1007/s10508-010-9664-6.
Stephenson, R., Sullivan, P. S., Salazar, L. F., Gratzer, B., Allen, S., & Seelbach, E. (2011). Attitudes towards couples-based HIV testing among MSM in three US cities. AIDS and Behavior, 15, S80–S87. doi:10.1007/s10461-011-9893-2.
Stueve, A., O’Donnell, L., Duran, R., San Doval, A., & Geier, J. (2002). Being high and taking sexual risks: Findings from a multisite survey of urban young men who have sex with men. AIDS Education and Prevention, 14, 482–495. doi:10.1521/aeap.14.8.482.24108.
Sullivan, P. S., Salazar, L., Buchbinder, S., & Sanchez, T. H. (2009). Estimating the proportion of HIV transmissions from main sex partners among men who have sex with men in five US cities. AIDS, 23, 1153–1162. doi:10.1097/QAD.0b013e32832baa34.
Theodore, P. S., Duran, R. E., Antoni, M. H., & Fernandez, M. I. (2004). Intimacy and sexual behavior among HIV-positive men-who-have-sex-with-men in primary relationships. AIDS and Behavior, 8, 321–331. doi:10.1023/B:AIBE.0000044079.37158.a9.
Trussler, T., Perchal, P., & Barker, A. (2000). ‘Between what is said and what is done’: Cultural constructs and young gay men’s HIV vulnerability. Psychology, Health & Medicine, 5, 295–306. doi:10.1080/13548500050119350.
Underhill, K., Operario, D., Skeer, M., Mimiaga, M., & Mayer, K. (2010). Packaging PrEP to prevent HIV: An integrated framework to plan for pre-exposure prophylaxis implementation in clinical practice. Journal of Acquired Immune Deficiency Syndromes, 55, 8–13. doi:10.1097/QAI.0b013e3181e8efe4.
Wilkerson, J. M., Smolenski, D. J., Morgan, R., & Rosser, B. (2012). Sexual agreement classifications for gay and bisexual men and implications for harm reduction HIV prevention. Health Education & Behavior, 39, 303–314. doi:10.1177/1090198111413917.
Wong, C. F., Schrager, S. M., Chou, C. P., Weiss, G., & Kipke, M. D. (2013). Changes in developmental contexts as predictors of transitions in HIV-risk behaviors among young men who have sex with men (YMSM). American Journal of Community Psychology, 51, 439–450. doi:10.1007/s10464-012-9562-2.
Worth, H., Reid, A., & McMillan, K. (2002). Somewhere over the rainbow: Love, trust and monogamy in gay relationships. Journal of Sociology, 38, 237–253. doi:10.1177/144078302128756642.
Acknowledgments
This research was funded by a grant from the National Institute of Mental Health (1R21MH095413; PI: Mustanski). A small portion of the sample was also recruited through a cohort funded by the National Institute of Drug Abuse (R01DA025548; PIs: Mustanski and Garofalo). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Greene, G.J., Andrews, R., Kuper, L. et al. Intimacy, Monogamy, and Condom Problems Drive Unprotected Sex Among Young Men in Serious Relationships with Other Men: A Mixed Methods Dyadic Study. Arch Sex Behav 43, 73–87 (2014). https://doi.org/10.1007/s10508-013-0210-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10508-013-0210-1