Abstract
As researchers and community-based providers continue to encourage latex condom use as a chief strategy to prevent HIV transmission among men who have sex with men, research is needed to better explore the intersecting associations among penis size (length and circumference), condom feel, ease of finding condoms, recent experience of condom failure (breakage and slippage), and unprotected anal sex. Data were taken from a 2010 community-based survey of self-identified gay and bisexual men in New York City (n = 463). More than half (51.4 %) reported penile length as 6–8 in. long (15–20 cm) and 31.5 % reported penile circumference as 4–6 in. around (10–15 cm). Variation in self-reported penile dimensions was significantly associated with men’s attitudes toward the typical/average condom, difficulty finding condoms that fit, and the experience of condom breakage. Men who had engaged in recent unprotected insertive anal intercourse reported significantly higher values for both penile length and circumference, and these men were significantly more likely to report that the average/typical condom was “too tight.” Most men had measured their length (86.2 %) and/or circumference (68.9 %), suggesting that penile measurement might be a common and acceptable practice among gay and bisexual men. As HIV and STI prevention providers continue to serve as leading distributers of free condoms, these findings further highlight the need for condom availability to be in a variety of sizes. Improving condom fit and attitudes toward condoms may also improve condom use and minimize condom slippage and breakage.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The U.S. Centers for Disease Control and Prevention recommends the male latex condom as the best physical barrier one can use for preventing HIV and STI transmission (CDC, 2010a). In tandem, public health departments and other community-based providers include the distribution of free condoms as part of their comprehensive strategy to prevent the further transmission of HIV and STIs. For example, the New York City (NYC) Department of Health and Mental Hygiene (DOHMH) is the largest distributor of free condoms in the city (Burke et al., 2009, 2011). In 2007, the DOHMH distributed more than 36 million “standard” Lifestyles ® condoms (personal communication with the Condoms and Materials Distribution Unit, NYC DOHMH, 2010). These condoms are 7.07 in. (18.0 cm) long and 2.13 in. (5.4 cm) across. Recognizing the need to offer a variety of condoms, in 2009 the DOHMH expanded their distribution to include seven additional types of male condoms in a limited set of locations. Of the seven additional types of condoms offered, only two (Durex XXL and Durex Enhanced Pleasure) were tailored to accommodate variation in penile dimensions—Durex XXL is a larger sized condom and Durex Enhanced Pleasure has a contoured shape for better (more snug) fit.
Men who have sex with men (MSM) remain disproportionately affected by HIV/AIDS. In 2009, MSM accounted for 61 % of all new diagnoses of HIV infection, and 75 % of all diagnosed HIV infections among males (CDC, 2010b; Prejean et al., 2011). It is no surprise that health and community service providers place substantial emphasis on correct and consistent condom use for MSM. Much of the existing research on MSM’s attitudes toward condoms centers on perceptions that condoms are a barrier to physical intimacy and pleasure (Bauermeister, Carballo-Dieguez, Ventuneac, & Dolezal, 2009; Golub, Starks, Payton, & Parsons, 2011). Substantially less research has focused on perceptions of condom fit and feel, particularly among MSM. Researchers have argued that penis size can impact correct and consistent condom use and HIV/STI transmission (Reece et al., 2007, 2008). Herbenick and Reece (2006) have highlighted how there are only a limited range of condom sizes available, with a majority of manufacturers producing condoms to fit an “average” penis. Others suggested that experiences with the fit and feel of condoms (Crosby, Yarber, Sanders, & Graham, 2005; Grady, Klepinger, Billy, & Tanfer, 1993; Jadack, Fresia, Rompalo, & Zenilman, 1997) and condom breakage and slippage (Crosby et al., 2007, 2008; Herbenick & Reece, 2006; Rosenberg & Waugh, 1997) reduce consistent use by some men. As a result, this has been hypothesized to inadvertently lead to greater incidence of HIV and STIs (Herbenick & Reece, 2006; Reece et al., 2007, 2008).
There is limited research on condom fit and feel among MSM. Reece, Briggs, Dodge, Herbenick, and Glover (2010) reported on a sample of 215 HIV positive men (59 % were gay and 22 % bisexual) in which participants reported specific characteristics of condoms that challenged fit and feel, including 21 % endorsing that condoms felt too tight, 16 % that condoms were too short, and 19 % indicating that it was difficult to find size appropriate condoms. A second study of 178 African American MSM found 21 % reported that condoms felt too tight, 18 % reported that condoms felt too short, 10 % reported that condoms felt too loose, and 7 % reported that condoms felt too long (Reece et al., 2007). This study found that those who experienced slippage and/or breakage were more likely to indicate that condoms feel too tight.
Although Reece et al. provided insight into the experiences of African American MSM and HIV-positive men, such information among MSM more generally is unavailable. Furthermore, it is unclear how negative experiences with, and perceptions about, condoms are associated with condom use behavior among MSM. Finally, although there is some information on the attitudes of MSM toward condoms, there is limited knowledge as to how these factors are related directly to men’s own penile dimensions (length and circumference).
Addressing these limitations, the present study reports on 463 gay and bisexual men. We compared responses on questions of penis size (length and circumference), condom feel, ease of finding condoms, and recent condom failure (breakage and slippage). Next, we compared men who had never measured their penile length and/or circumference with those who had measured on condom feel, ease of finding condoms, and recent condom failure (breakage and slippage). Finally, we compared men who had engaged in recent (<3 months) unprotected insertive anal intercourse with a casual male partner (to those who had not) on penile length, circumference, condom feel, ease of finding condoms, and recent condom failure (breakage and slippage). Analyses were focused to the participant’s use of condoms on his own penis—we were unable to investigate condom use for receptive anal sex because we did not have data on the dimensions of participants’ partner’s penis.
Method
Participants
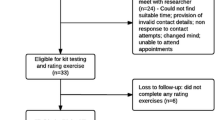
In spring 2010, a cross-sectional, street-intercept method (Miller, Wilder, Stillman, & Becker, 1997) was adapted to survey 463 gay and bisexual men at a series of gay, lesbian, and bisexual (GLB) community events in NYC through the Sex and Love Study v8.0 (Grov, Parsons, & Bimbi, 2010; Pantalone, Bimbi, Holder, Golub, & Parsons, 2010). This approach to collecting data has been used in numerous studies (Carey, Braaten, Jaworski, Durant, & Forsyth, 1999; Chen, Kodagoda, Lawrence, & Kerndt, 2002; Kalichman & Simbaya, 2004; Rotheram-Borus et al., 2001), including those focused on GLB persons (Benotsch, Kalichman, & Cage, 2002; Kalichman et al., 2001), and has been shown to provide data that are comparable to those obtained from other more methodologically rigorous approaches (Halkitis & Parsons, 2002), such as time–space sampling.
At each community event, the research team hosted a booth, and a member of the research team actively approached each person who passed the booth. The response rate was high, with 76 % of those approached consenting. The self-reported paper-and-pencil survey required 15–20 min to complete, and participants were handed the survey on a clipboard so that they could step away from others to complete the questionnaire privately. Adjacent to our booth, and cordoned off by a curtain, we provided participants a separate seating area, including spaced apart chairs, such that participants could complete the survey in added privacy. When handing participants surveys, project staff emphasized the importance of confidentiality and instructed participants to keep their responses private. Once completed, participants deposited their own completed survey into a secure box at the booth. As an incentive, participants were given a voucher for free admission to a movie. Survey data were entered into an SPSS database and checked/verified by project staff for accuracy. All procedures were reviewed and approved by the sponsoring center’s Institutional Review Board.
Measures
Participant Characteristics
Participants reported their age (in years), sexual identity, education, HIV status, STI history, and race and ethnicity. Response options are shown in Table 1.
Penis Length and Circumference
Men were asked to indicate, “When erect (hard), what is the length of your penis?” and presented with six ordinal categories that included lengths in inches and centimeters. To facilitate precision, surveys included a drawing depicting an erect penis with an adjacent ruler demonstrating the measurement starting (i.e., penis base) and end point (i.e., tip of the glans penis). Penis circumference was assessed by asking men, “When erect (hard), what is the girth (circumference around) of your penis?” Men were presented with five ordinal categories that included circumference in inches and centimeters. Similar to length, men were shown a drawing depicting an erect penis with a measuring tape circumnavigating the penis shaft. Men were also given the option to indicate if they had never measured their penile length and/or circumference. Response options and the images are shown in Table 1.
Condom Feel and Ease of Finding Fitting Condoms
Similar to others’ studies (Reece et al., 2007, 2010; Reece, Herbenick, & Dodge, 2009), men were presented with three semantic differential scales. First, they were asked, “For my penis length, the average/typical condom is,” with response ranging from “1-Too Short” to “5-Too Long.” Next, men were asked, “For my penis girth, the average/typical condom is,” with response choices ranging from “1-Too Tight” to “5-Too Loose.” Finally, men were asked, “Finding condoms that fit my penis is,” with choices ranging from “1-Easy” to “5-Difficult.”
Recent Condom Breakage, Slippage, and Condom Use
Similar to others’ studies (Herbenick & Reece, 2006; Reece et al., 2008), men were asked, “In the last 3 months, how often have you experienced condom breakage (on your penis),” and “In the last 3 months, how often have you experienced condom slippage (on your penis).” Responses ranged from “0-Never Happens” to “5-Always Happens.” Men were also given the option to indicate that they had not worn a condom on their penis in the last 3 months. Finally, men indicated if they had engaged in unprotected insertive anal intercourse (UIAI) with a casual male partner in the last 3 months. Responses were coded 0 = no, 1 = yes.
Analytic Plan
When expected cell counts permitted, we used Chi-square. In addition, we used Goodman and Kruskal’s Gamma and Spearman’s rho rank correlation coefficient. Both measures are ideal for ordinal variables, providing indices for strength and direction of an association (Healey, 2009). The magnitude for Spearman’s rho is interpreted similarly to a Pearson’s r correlation coefficient, and Gamma can be conceptually interpreted as indicating proportional reduction in prediction error (i.e., percent of variation explained when using one variable to “predict” the other) (Kviz, 1981).
Results
Demographic Characteristics
Table 1 shows the characteristics of the sample. Ages ranged from 18 to 83 years (M = 42.0, SD = 11.88), and 39 % were men of color. Most men (92.9 %) self-identified as gay and 4.5 % as bisexual. All men reported sex with other men. Most participants (74.5 %) were HIV negative, 19.9 % were HIV positive, and 5.6 % failed to report or were untested. The majority (63 %) of men had contracted at least one STI during their lifetime and 46 % were in a relationship with another man lasting 3 months or longer.
Penis Size, Condom Feel, and Condom Failure
A majority of men (51.4 %) reported their erect penis length as being between 6 and 8 in. long (15–20 cm). Mode response for penis circumference was 4–6 in. around (10–15 cm) (31.5 %). A vast majority of men (71.7 %) reported that the “average/typical” condom was “just right” for their penis length and most (61.3 %) found it “just right” for their circumference. Nevertheless, only 38.4 % of men reported that finding condoms to fit their penis was “easy.” Among the 322 men who reported using condoms on their own penis, 31.7 % reported condom breakage, and 42.2 % reported condom slippage in the last 3 months (see Table 1).
Associations between Penis Size, Condom Fit, and Condom Failure
Table 2 presents a matrix of associations between all measures of penis size, condom feel, ease of finding condoms, and experience of condom failure (breakage and slippage). In these analyses, men who reported that they had never measured themselves were not included. Penis length was positively associated with penis circumference, difficulty finding condoms that fit, and condom breakage. Both penis length and circumference were inversely associated with finding the average condom to be “too long” and “too loose.” There was a positive association between difficulty finding condoms that fit and condom breakage and slippage. Interpreting Gamma, 26 % of the variation in condom breakage was explained by men’s rating on the ease/difficulty of finding condoms that fit. Finally, there was a significant positive association between condom breakage and condom slippage (see Table 2 for all values).
Associations between Penis Measurement Experience, Condom Feel, and Condom Failure
Table 3 reports comparisons between men who had previously measured their length and/or circumference to those who had not. Having measured one’s length (or not) was not associated with ratings on the average condom’s length, ease/difficulty in finding condoms that fit, recent condom breakage, recent condom slippage, or UIAI. In contrast, having measured one’s circumference was related to several variables. Men who had measured their circumference were more likely to report the average/typical condom as being too tight. Men who had measured their circumference also reported more difficulty in finding condoms that fit, and were more likely to report recent condom breakage and condom slippage. Whether men had measured their circumference (or not) was unrelated to UIAI (see Table 3 for all values).
Recent Unprotected Insertive Anal Intercourse with a Casual Male Partner
Table 4 reports comparisons between men who had engaged in recent UIAI with a casual male partner (21.6 %, n = 100) and those who had not. Those who had engaged in recent UIAI reported significantly higher values for both penile length and circumference. Similarly, those who had engaged in UIAI were more likely to report that the average condom was “too tight.” There was a marginally significant (p < .10) positive association between UIAI and condom breakage. UIAI was not associated with ratings on the average condom’s length, ease of finding condoms that fit or recent experienced condom slippage.
Finally, we entered items from Table 4 that were significant at p < .10 into a logistic regression to identify factors associated with UIAI (1 = yes, 0 = no). When controlling for other effects, penile circumference was associated with ascending odds ratios for UIAI (AORCircumference 2–4 in. = 1.71, CI95 % = 1.11–1.32; AORCircumference 4–6 in. = 2.92, CI95 % = 1.11–2.64; AORCircumference 6–8 in. = 4.99, CI95 % = 1.35–18.45; AORCircumference 8+ in. = 8.53, CI95 % = 1.49–48.75). Other variables were not significant in the model.
Discussion
Although most men indicated their penis length was between 6 and 8 in. long (15–20 cm), there was a lot of variation self-reported length and circumference. This variation was significantly associated with men’s attitudes toward the typical/average condom, difficulty finding condoms that fit, and the experience of condom breakage, which is consistent with prior research (Herbenick & Reece, 2006; Reece et al., 2009). Men who had engaged in recent UIAI reported significantly higher values for both penile length and circumference—and these men were significantly more likely to report that the average/typical condom was “too tight.”
The extent to which men reported difficult experiences with condoms was similar to those identified by others (Reece et al., 2007, 2010) and, collectively, these findings provide further evidence of the large proportion of gay, bisexual, and other MSM who report problems with condom fit. As researchers and health providers continue to encourage condom use as a chief strategy to prevent HIV transmission among MSM, these results highlight the need to better explore the intersecting roles among penis size, condom feel, ease of finding comfortably fitting condoms, the experience of condom failure, and unprotected anal sex.
We identified a significant association between prior experience measuring oneself and a variety of outcomes. Although prior experience with measuring length was largely unrelated to other variables, prior experience with measuring circumference was associated with multiple outcomes. In all, it seemed men who had never measured their circumference fared better—they were less likely to experience condom breakage or condom slippage, and indicated it was easier to find condoms that fit. This is not to suggest that measuring one’s penile circumference somehow leads to negative outcomes. Instead, perhaps men who had difficulty using condoms felt it necessary to measure their own circumference in order to “diagnose” the problem.
Limitations
Though these findings are compelling, there are several limitations to consider. These data do not generalize to all gay and bisexual men, as this sample was limited to those who attended large-scale GLB events in NYC. As our analyses drew from cross-sectional data, causality should not be inferred nor do these analyses rule out the potential for confounding effects from other variables not assessed. Our sampling approach, however, may improve ecological validity for the types of individuals that attend large scale GLB events, and comprise a considerable (and accessible) portion of the gay, bisexual and MSM communities in NYC.
Our survey included a broad array of demographic and sexual health questions; however, it has its limitations. Consistent with the brief street-intercept survey method (Miller et al., 1997), many of the questions were quantitative and close-ended. For example, we did not gather detailed data on HIV or STI testing behavior. Among MSM, HIV is transmitted predominately via anal sex with male partners (CDC, 2008, 2010c). As such, our focus was on anal intercourse between men; we did not collect data with regard to female partners. In addition, some questions had less than ideal wording—condom slippage and condom breakage data might have been more useful were we to gather frequency responses. And, although efforts were taken to ensure confidentiality, there was potential for socially desirable responses in the reporting of sensitive information.
Given the wide availability and distribution of “standard” condoms in NYC, our analyses asked participants to rate the “average/typical” condom. NYC MSM encounter such “standard” condoms at a variety of gay bars/clubs, bookstores, adult video stores, bathhouses, sex clubs, private sex parties, and at large scale GLB events. These are also the type of condom predominantly distributed by community service organizations and care providers. Further, the NYC DOHMH also advertises its NYC-branded condom on billboards across the city, on radio, and TV. Our focus on the “average/typical” condom enabled us to understand how MSM view these condoms; nevertheless, we recognize participants’ own interpretation of this wording may not be universal nor does this measure capture the actual condoms participants may have used. Further, instead of men reflecting on condom use over a 3-month period, another approach to collecting data could be to use event-specific measures. Such alternate approaches carry inherent strengths and limitations. Our research questions focused on condom size as it related to length/width and slippage/breakage. Other factors to consider include condom texture, shape, lubrication, and flavor.
Researchers have noted that gay and bisexual culture is filled with imagery emphasizing the size of one’s genitalia (Bergling, 2007; Drummond & Filiault, 2007; Grov et al., 2010; Moskowitz & Hart, 2011). Many men-seeking-men websites (the modal way in which gay and bisexual men find sex partners in the U.S.) (Chiasson et al., 2006) have incorporated penile dimensions as a prominent feature in members’ profiles (adjacent to characteristics like height, weight, race, and sexual position). Users can post and search for nude photos and websites often allow users to restrict their search based on penis sizes. Taken together, we believe an emphasis on penile dimensions is ingrained into many facets of gay culture and there are norms prompting gay and bisexual men to know their own dimensions. In support of this, we found that a majority of participants had experience measuring themselves and felt comfortable reporting these dimensions on our survey. Further, results from our study were similar to another in which gay men measured their partners and found penises to be an average length of 6.0 in. (15.3 cm) and average circumference of 4.9 in. (12.5 cm) (Harding & Golombok, 2002). Notably, Harding and Golombok followed up with participants 3 months later and found similar values for length (15.2 cm) and circumferences (12.6 cm). They found no association between measurement discrepancies and age, social class, education, ethnicity, or employment status. Similarly, Reece and Herbenick (personal communication, 2011), in their studies on penis size have asked participants to measure themselves using a Fit Kit and separately with a ruler. They too found a strong correlation between reports (~.80).
That being said, there are several noteworthy limitations in how we collected these data. For example, some research on penis size among gay and bisexual men used normative ratings (e.g., “above average,” “below average”) (e.g., Grov et al., 2010), and we believe that our use of a standard metric (inches and cm) was an improvement. Nevertheless, we could have allowed men to write in the actual length and circumference (rather than selecting from categories), but this may have resulted in additional missing and unusable data. Response options in our survey were in 2-in. increments (e.g., 4–6 in., 6–8 in.); however, future research might consider a finer array of categories (e.g., 1 in. increments). Yet, our use of a wider increment might have better accommodated measurement error (e.g., someone who mismeasured himself at 5.5 in, when he was actually 4.9 in, would have been captured in the same category: “4–6 in.”). In order to improve the accuracy of self-reported penile dimensions, our survey included two drawings depicting erect penises and adjacent rulers indicating measurement starting and endpoints. Nevertheless, there was no guarantee that the drawings we showed men reflected how they actually measured themselves. We also did not collect data on amount of time since most recent measurements. Given that our study was conducted at large scale community events, it was not feasible for participants to measure themselves, or the research team to perform measurements on site (which, in and of itself, could impact participation rates). Taken together, future researchers must weigh the costs and benefits of different data collection strategies and know that no one approach may result in “best” data.
Conclusion
These limitations notwithstanding, this study provided additional insight into MSM’s penis sizes as they relate to attitudes and experiences with condoms, an area with limited research. As HIV and STI prevention providers continue to serve as leading distributers of free condoms, these findings further highlight the need for condom availability to be in a variety of sizes—a “one size fits all” approach to condom distribution may not meet the needs of many MSM who fall outside the range of the “average” condom. Most men had measured both their length and circumference, suggesting that measuring oneself might be a common and acceptable practice—and this may be an opportunity for providers to initiate discussions with MSM about the match between condom size and penile dimensions.
In recent years, condom manufactures have responded to increased demand for product diversity by introducing an expanded range of condom sizes, shapes, colors, flavors, and textures. Some HIV prevention providers have begun to distribute a wider array of products, though often in limited supply. Given our current findings, we recommend HIV prevention providers and MSM themselves become more familiar with the range of new products that exist. By improving condom fit and attitudes toward condoms, we may effectively improve condom use while minimizing condom slippage and breakage.
References
Bauermeister, J. A., Carballo-Dieguez, A., Ventuneac, A., & Dolezal, C. (2009). Assessing motivations to engage in intentional condomless anal intercourse in HIV risk contexts (“bareback sex”) among men who have sex with men. AIDS Education and Prevention, 21, 156–168.
Benotsch, E. G., Kalichman, S. C., & Cage, M. (2002). Men who have met sex partners via the internet: Prevalence, predictors, and implications for HIV prevention. Archives of Sexual Behavior, 31, 177–183.
Bergling, T. (2007). Chasing adonis: Gay men and the pursuit of perfection. New York: Harrington Park Press.
Burke, R. C., Wilson, J., Bernstein, K. T., Grosskopf, N., Murrill, C., Cutler, B., … Begier, E. M. (2009). The NYC condom: Use and acceptability of New York City’s branded condom. American Journal of Public Health, 99, 2178–2180.
Burke, R. C., Wilson, J., Kowalski, A., Murrill, C., Cutler, B., Sweeney, M., et al. (2011). NYC condom use and satisfaction and demand for alternative condom products in New York City sexually transmitted disease clinics. Journal of Urban Health, 88, 749–758.
Carey, M. P., Braaten, L. S., Jaworski, B. C., Durant, L. E., & Forsyth, A. D. (1999). HIV and AIDS relative to other health, social, and relationship concerns among low-income women: A brief report. Journal of Women’s Health and Gender Based Medicine, 8, 657–661.
CDC. (2008). Trends in HIV/AIDS diagnoses among men who have sex with men—33 States, 2001–2006. Morbidity and Mortality Weekly Report, 57, 681–686.
CDC. (2010a). Condoms and STDs: Fact sheet for public health personnel. Retrieved from http://www.cdc.gov/condomeffectiveness/latex.htm.
CDC. (2010b). Diagnoses of HIV infection and AIDS in the United States and dependent areas, 2009. HIV Surveillance Report. Atlanta: U.S. Department of Health and Human Services.
CDC. (2010c). HIV among gay, bisexual and other men who have sex with men (MSM) Retrieved from http://www.cdc.gov/hiv/topics/msm/pdf/msm.pdf.
Chen, J. L., Kodagoda, D., Lawrence, A. M., & Kerndt, P. R. (2002). Rapid public health interventions in response to an outbreak of syphilis in Los Angeles. Sexually Transmitted Diseases, 29, 285–287.
Chiasson, M. A., Parsons, J. T., Tesoriero, J. M., Carballo-Dieguez, A., Hirshfield, S., & Remien, R. H. (2006). HIV behavioral research online. Journal of Urban Health, 83, 73–85.
Crosby, R. A., Salazar, L. F., Yarber, W. L., Sanders, S. A., Graham, C. A., Head, S., & Arno, J. N. (2008). A theory-based approach to understanding condom errors and problems reported by men attending an STI clinic. AIDS and Behavior, 12, 412–418.
Crosby, R. A., Yarber, W. L., Sanders, S. A., & Graham, C. A. (2005). Condom discomfort and associated problems with their use among university students. Journal of American College Health, 54, 143–147.
Crosby, R. A., Yarber, W. L., Sanders, S. A., Graham, C. A., McBride, K., Milhausen, R. R., & Arno, J. N. (2007). Men with broken condoms: Who and why? Sexually Transmitted Infections, 83, 71–75.
Drummond, M. J. N., & Filiault, S. M. (2007). The long and short of it: Gay men’s preceptions of penis size. Gay and Lesbian Issues and Psychology Review, 3, 121–129.
Golub, S. A., Starks, T. J., Payton, G., & Parsons, J. T. (2011). The critical role of intimacy in the sexual risk behaviors of gay and bisexual men. AIDS and Behavior. doi:10.1007/s10461-011-9972-4.
Grady, W. R., Klepinger, D. H., Billy, J. O., & Tanfer, K. (1993). Condom characteristics: The perceptions and preferences of men in the United States. Family Planning Perspectives, 25, 67–73.
Grov, C., Parsons, J. T., & Bimbi, D. S. (2010). The association between penis size and sexual health among men who have sex with men. Archives of Sexual Behavior, 39, 788–797.
Halkitis, P. N., & Parsons, J. T. (2002). Recreational drug use and HIV-risk sexual behavior among men frequenting gay social venues. Journal of Gay and Lesbian Social Services, 14, 19–38.
Harding, R., & Golombok, S. E. (2002). Test-retest reliability of the measurement of penile dimensions in a sample of gay men. Archives of Sexual Behavior, 31, 351–357.
Healey, J. F. (2009). Statistics: A tool for social research (8th ed.). Florence, KY: Wadsworth.
Herbenick, D., & Reece, M. (2006). Penis length and circumference as contributors to condom breakage, slippage, and perceived discomfort. European Journal of Sexual Health, 15(S1), 35.
Jadack, R. A., Fresia, A., Rompalo, A. M., & Zenilman, J. (1997). Reasons for not using condoms of clients at urban sexually transmitted diseases clinics. Sexually Transmitted Diseases, 24, 402–408.
Kalichman, S. C., Benotsch, E., Rompa, D., Gore-Felton, C., Austin, J., Luke, W., … Simpson, D. (2001). Unwanted sexual experiences and sexual risks in gay and bisexual men: Associations among revictimization, substance use, and psychiatric symptoms. Journal of Sex Research, 28, 1–9.
Kalichman, S. C., & Simbaya, L. (2004). Traditional beliefs about the cause of AIDS and AIDS-related stigma in South Africa. AIDS Care, 16, 572–580.
Kviz, F. J. (1981). Interpreting proportional reduction in error: Measures as percentage of variation explained. Sociological Quarterly, 22, 413–420.
Miller, K. W., Wilder, L. B., Stillman, F. A., & Becker, D. M. (1997). The feasibility of a street-intercept survey method in an African-American community. American Journal of Public Health, 87, 655–658.
Moskowitz, D. A., & Hart, T. A. (2011). The influence of physical body traits and masculinity on anal sex roles in gay and bisexual men. Archives of Sexual Behavior, 40, 835–841.
Pantalone, D. W., Bimbi, D. S., Holder, C. A., Golub, S. A., & Parsons, J. T. (2010). Consistency and change in club drug use by sexual minority men in New York City, 2002 to 2007. American Journal of Public Health, 100, 1892–1895.
Prejean, J., Song, R., Hernandez, A., Ziebell, R., Green, T., Walker, F., … Hall, H. I. (2011). Estimated HIV incidence in the United States, 2006–2009. PLoS ONE, 6, e17502.
Reece, M., Briggs, L., Dodge, B., Herbenick, D., & Glover, R. (2010). Perceptions of condom fit and feel among men living with HIV. AIDS Patient Care and STDs, 24, 435–440.
Reece, M., Dodge, B., Herbenick, D., Fisher, C., Alexander, A., & Satinsky, S. (2007). Experiences of condom fit and feel among African-American men who have sex with men. Sexually Transmitted Infections, 83, 454–457.
Reece, M., Herbenick, D., & Dodge, B. (2009). Penile dimensions and men’s perceptions of condom fit and feel. Sexually Transmitted Infections, 85, 127–131.
Reece, M., Herbenick, D., Monahan, P. O., Sanders, S. A., Temkit, M., & Yarber, W. L. (2008). Breakage, slippage, and acceptability outcomes of a condom fitted to penile dimensions. Sexually Transmitted Infections, 84, 143–149.
Rosenberg, M. J., & Waugh, M. S. (1997). Latex condom breakage and slippage in a controlled clinical trial. Contraception, 56, 17–21.
Rotheram-Borus, M. J., Lee, M., Zhou, S., O’Hara, P., Birnbaum, J. M., Swendeman, D., … Wight, R. G. (2001). Variation in health and risk behavior among youth living with HIV. AIDS Education and Prevention, 13, 42–54.
Acknowledgments
The Sex and Love Study v8.0 was supported by the Hunter College Center for HIV/AIDS Educational Studies and Training (CHEST), under the direction of Dr. Parsons. The authors acknowledge the contributions of other members of the Sex and Love v8.0 Team: Anthony Bamonte, Anthony Surace, Bill Kowalczyk, Bryant Porter, Catherine Holder, Corina Weinberger, David S. Bimbi, Hunter Kincaid, Jaye Walker, Gregory Payton, Jon Rendina, Jose Nanin, Julia Tomassilli, Kevin Robin, Monica Gonzalez, Kristi Gamarel, Sarit A. Golub, Mark Pawson, Michael Adams, and Tyrel Starks. We would also like to acknowledge the CHEST Recruitment Team, CHEST interns, and the Drag Initiative to Vanquish AIDS (DIVAs) for their contributions to Sex and Love v8.0.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Grov, C., Wells, B.E. & Parsons, J.T. Self-Reported Penis Size and Experiences with Condoms Among Gay and Bisexual Men. Arch Sex Behav 42, 313–322 (2013). https://doi.org/10.1007/s10508-012-9952-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10508-012-9952-4