Abstract
Ischemia reperfusion (IR) injury (IRI) is associated with poor prognoses in the settings of both cardiac surgery and ischemic heart disease and causes mitochondrial oxidative stress and cell death. Silent information regulator 1 (SIRT1), a member of the histone deacetylase family, exerts anti-IRI effects. Bakuchiol (BAK), an analog of resveratrol and a monoterpene phenol isolated from the seeds of Psoralea corylifolia (Leguminosae), protects tissues from injury. This study was designed to investigate the protective effects of BAK treatment in the setting of myocardial IRI and to elucidate the potential mechanism of those effects. Prior to induction of IR, isolated rat hearts or cardiomyocytes were exposed to BAK in either the absence or presence of the SIRT1 inhibitors Sirtinol and SIRT1 siRNA. BAK exerted cardioprotective effects, as evidenced by the improvements noted in cardiac function following ischemia, attenuated myocardial apoptosis, and changes in several biochemical parameters (including increases in the level of the anti-apoptotic protein Bcl2, decreases in the level of the pro-apoptotic protein Bax, and decreases in the cleaved Caspase 3 level). However, Sirtinol and SIRT1 siRNA each blocked BAK-induced cardioprotection by inhibiting SIRT1 signaling. Additionally, BAK significantly increased the activities of mitochondrial succinate dehydrogenase, cytochrome c oxidase, and mitochondrial superoxide dismutase and decreased the production of malondialdehyde. These findings suggested that BAK significantly attenuated IR-induced mitochondrial oxidative damage. However, Sirtinol and SIRT1 siRNA abolished BAK-dependent mitochondrial function. In summary, our results demonstrate that BAK treatment attenuates IRI by attenuating IR-induced mitochondrial oxidative damage via the activation of SIRT1/PGC-1α signaling.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ischemic heart disease, also known as coronary atherosclerotic heart disease, has become a leading cause of death worldwide, accounting for 7.4 million deaths in 2012 (http://www.who.int/mediacentre/factsheets/fs310/en/); its prevalence continues to increase in developing countries [1]. Previous evidence has indicated that not only ischemia itself but also reperfusion contributes to the tissue injury sustained following myocardial ischemia, a phenomenon known as ischemia/reperfusion (IR) injury (IRI) [2]. Mitochondria play an important role in IRI [3]. The calcium overload and increased levels of oxidative stress that occur in the setting of IRI result in damage to the mitochondrial membrane and electron transport chain, the opening of mitochondrial permeability transition pores and the uncoupling of mitochondrial oxidative phosphorylation; these changes subsequently trigger the deterioration of mitochondrial structure and function, resulting in diminished cellular metabolism. The consequent low ATP levels and altered ion homeostasis result in the rupture of the plasma membrane and cell death in the myocardium. Therefore, mitochondria appear to be a key factor in cardiomyocyte death, and protecting mitochondria from oxidative stress and maintaining mitochondrial function may represent a means of ameliorating myocardial IRI [3]. Preconditioning the heart with multiple brief episodes of nonlethal ischemia episodes in combination with alternating periods of reflow has been shown to reduce the size of infarcts caused by subsequent ischemic insults, a phenomenon known as myocardial ischemic preconditioning (IPC) [4]. However, the classic IPC procedure requires that interventions be applied directly to the heart, which may potentiate additional injuries to target tissues and arteries and limit its clinical applicability; alternative methods of mimicking the cardioprotective effects of classic ischemic conditioning have been investigated, including both pharmacologic conditioning and remote conditioning [5].
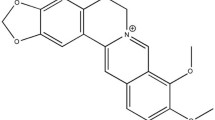
Bakuchiol (BAK), a monoterpene phenol isolated from the seeds of Psoralea corylifolia (Leguminosae) [6], exerts organic protective effects in both the liver [7, 8] and the skin [9]. Recent studies have demonstrated that BAK exerts a wide spectrum of pharmacologic effects, including anti-oxidative [10, 11], anti-inflammatory [12], anti-aging [9, 10], and anti-diabetic [13] effects. However, oxidative stress, inflammation and diabetes are the primary elements of myocardial IRI [14–16], which suggests that BAK may play a promising role in attenuating IRI.
Silent information regulator 1 (SIRT1) is a histone deacetylase that depends on nicotinamide adenine dinucleotide (NAD+) [17] and plays a key role in the longevity effects of calorie restriction; its cardioprotective effects are also well known [17, 18]. The activation of SIRT1 by IPC and resveratrol, a natural phenolic phytoalexin [19], reportedly attenuates myocardial IRI [20, 21]. Previous studies have demonstrated that resveratrol exerts cardioprotective effects by protecting cardiomyocytes from oxidative stress and improving mitochondrial function via the SIRT1 signaling pathway [22, 23]. Additionally, SIRT1 activates peroxisome proliferator-activated receptor-γ co-activator-1α (PGC-1α), which attenuates oxidative damage. Previous studies have indicated that the up-regulation of PGC-1α depends on SIRT1 and protects tissues in both cerebral ischemia [24, 25] and renal IRI [26]. Mitochondrial dysfunction is a pathological consequence of IRI; maintaining mitochondrial function following ischemia may preserve organ function; SIRT1/PGC-1α activation following IRI accelerates mitochondrial biogenesis and dynamics and ameliorates mitochondrial damage, which contributes to the recovery of mitochondrial protein expression and function [26, 27]. BAK is an analogue of resveratrol and has a resveratrol-like structure [28]. Thus, BAK likely attenuates myocardial IRI by maintaining mitochondrial function via SIRT1. However, the definitive role of SIRT1/PGC-1α signaling and its relationship with the cardioprotective effects of BAK in the setting of IRI have not been investigated.
Therefore, this study was designed to evaluate the protective effects of BAK in the setting of myocardial IRI and to investigate its potential effects on both myocardial mitochondrial redox states and mitochondrial function. The involvement of SIRT1/PGC-1α signaling in the maintenance of mitochondrial function was also evaluated.
Materials and methods
Materials
BAK, 4′,6-diamino-2-phenylindole (DAPI), 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT), dimethylsulfoxide (DMSO), and a protease inhibitor cocktail were purchased from Sigma-Aldrich (St. Louis, MO, USA). The SIRT1 siRNA and antibodies against PGC-1α, Bcl2, Bax, and β-actin were purchased from Cell Signaling Technology (Beverly, MA, USA). Sirtinol and the antibodies against Caspase 3 and SIRT1 were obtained from Santa Cruz Biotechnology (Santa Cruz, CA, USA). The kits used to measure the hydrogen peroxide (H2O2), glutathione (GSH), oxidized glutathione (GSSG), lactate dehydrogenase (LDH), creatine kinase-MB (CK-MB), superoxide dismutase (SOD), and malondialdehyde (MDA) levels were purchased from the Institute of Jiancheng Bioengineering (Nanjing, Jiangsu, China). The terminal deoxynucleotidyl transferase dUTP nick-end labeling (TUNEL) kits were purchased from Roche (Mannheim, Germany). The rabbit anti-goat, goat anti-rabbit, and goat anti-mouse secondary antibodies were purchased from the Zhongshan Company (Beijing, China).
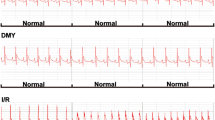
Preparation of the perfused isolated rat hearts and BAK treatment
The present study was performed in accordance with the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (National Institutes of Health Publication No. 85-23, revised in 1996) and approved by the Ethics Committee of the Fourth Military Medical University. Healthy adult male Sprague–Dawley (SD) rats (weighing between 220 and 250 g) and newborn SD rats (1–2 days old) were obtained from the animal center of the Fourth Military Medical University. As described in a previous study [29], the SD rats were intraperitoneally anesthetized with sodium pentobarbital (50 mg/kg). Twenty minutes following an intraperitoneal injection of 500 U/kg of heparin sodium, the chest was opened. The heart was quickly removed and retrogradely perfused through the aorta with a non-circulating Langendorff apparatus (Radnoti Glass Technology Inc., USA) at a constant pressure of 80 mmHg. The perfusate was Krebs–Henseleit buffer (KHB) containing (in mM) 118 NaCl, 4.7 KCl, 1.2 MgSO4, 1.2 KH2PO4, 1.25 CaCl2, 25 NaHCO3, and 11 glucose (pH 7.4, 37 °C), which was continuously gassed with 95 % O2 and 5 % CO2. The left ventricular developed pressure (LVDP) and heart rate (HR) were each monitored using a transducer (Model 100 BP-Biopac System Inc., USA) connected to a water-filled latex balloon inserted into the left ventricle via the left atrium. The BAK was dissolved in DMSO as stock solution and used in 3 days. At the beginning of the experiment, the left ventricular end-diastolic pressure (LVEDP) was adjusted to approximately 5 mmHg by inflating the balloon. The isolated heart was surrounded by a homoeothermic glass cover (37 °C) to maintain a constant temperature. All data were recorded and stored using the AcqKnowledge 3.8.1 software package and a Biopac Data Acquisition System (Model 100 BP-Biopac System Inc., Goleta, CA, USA). To establish the IRI model, the isolated perfused rat hearts were subjected to 45 min of ischemia, followed by 60 min of reperfusion. The various concentrations of BAK (0.25 μM, 0.5 μM, and 1 μM) were administrated for 5 min before the IR injury. After different treatments, the heart rate (HR), left ventricular developed pressure (LVDP) and rate of change of pressure development (+dP/dt max) were monitored. The coronary flow (CF) was calculated and collected during reperfusion for biochemical assays. The experimental protocols are included in Fig. 1a–c.
Cell culture, ischemia reperfusion (IR) treatment, and siRNA transfection
The primary cultures of neonatal rat cardiomyocytes from 1- to 2-day-old Sprague–Dawley rats were prepared using a previously reported method [30]. The cells were cultured in Dulbecco’s modified Eagle’s medium from Gibco (Invitrogen, Life Technologies, Ghent, Belgium), which was supplemented with 10 % fetal bovine serum (FBS) (Biochrom GmbH, Germany), 2 mM l-glutamine, 30 mg/l endothelial cell growth factor supplement (EGCS), 100 IU/ml penicillin, and 100 mg/ml streptomycin at 37 °C and 5 % CO2. The cells were transiently transfected with control siRNA or SIRT1 siRNA at 50 pM for 24 h using Lipofectamine RNAiMAX reagent (Invitrogen, Carlsbad, CA, USA) in DMEM [31]. After transfection with SIRT1 siRNA for 24 h, IR was then induced in the cardiomyocytes pre-treated with or without BAK for additional 2 h [32]. Then, the cells were harvested for further analysis.
Myocardial apoptosis analyses
A portion of the myocardium from the mid-left ventricle and treated cardiomyocytes were fixed in 4 % formalin. The level of cardiomyocyte apoptosis was analyzed via TUNEL staining. The TUNEL-positive cells that exhibited green nuclear staining, as well as the cells exhibiting blue nuclear DAPI staining, were counted within 5 randomly chosen fields under high-power magnification. The index of apoptosis was expressed as the ratio of positively stained apoptotic myocytes or cardiomyocytes to the total number of myocytes or cardiomyocytes counted × 100 %.
Myocardial necrosis analyses
Myocardial necrosis was estimated based on the levels of both LDH and CK-MB in the coronary effluent and cell lysis buffer. Respectively, the samples were added the substrate buffer and nicotinamide adenine dinucleotide to analyze the LDH. After incubation in 37 °C for 15 min, 2,4-dinitrophenylhydrazine (DNPH) was mixed and incubated for additional 15 min. At last, the 0.4 M NaOH was added at room temperature; the mixture was measured using an FLX 800 fluorescence microplate reader (Biotech Instruments, Inc., USA) at 440 nm. Moreover, the contents of CK-MB were analyzed using creatine kinase MB isoenzyme colorimetric assay kit in accordance with the manufacturer’s instructions.
Mitochondria isolation and oxidative damage analyses
The myocardial mitochondrial and cytosolic samples were prepared via differential centrifugation [33]. Briefly, frozen myocardial samples and cell lysis buffer were homogenized in 10 volumes of buffer A (250 mM sucrose; 10 mM Tris–HCl, pH 7.4; 1 mM EDTA, pH 7–8; 1 mM orthovanadate; 1 mM NaF; 0.3 mM phenylmethylsulfonyl fluoride (PMSF); and 5 μg/ml each of leupeptin, aprotinin and pepstatin A) and subjected to serial centrifugations at 1000, 10,000 and 100,000×g. The 1000 g pellet (nuclear fraction) was discarded, whereas the 10,000 g pellet (mitochondrial fraction) was washed in buffer A and re-centrifuged. The resulting pellet was re-suspended in buffer B (150 mM NaCl; 20 mM Tris–HCl, pH 7.4; 10 mM EDTA, pH 7–8; 1 mM orthovanadate; 1 mM NaF; 0.3 mM PMSF; 0.5 μg/ml pepstatin A; 5 μg/ml each of leupeptin and aprotinin; and 1 % NP-40) and subjected to centrifugation at 21,000×g for 10 min. The resulting supernatant was defined as the mitochondrial fraction. The 100,000 g supernatant was defined as the cytosolic fraction. All isolated mitochondrial and cytosolic samples were kept on ice and used within 3 h of isolation. As indicators of mitochondrial oxidative stress, the activity level of SOD and the levels of H2O2, GSH, GSSG, and MDA in the mitochondrial fraction were determined using commercially available kits. After mixed the different reagents with mitochondrial fraction in each kit, the SOD level was measured using an FLX 800 fluorescence microplate reader at 550 nm; while, H2O2 level was analyzed at 405 nm. The values of GSH and GSSG were calculated based on the mitochondrial redox potential (E h ) using the Nernst equation, as described previously [33]. Furthermore, the activity levels of succinate dehydrogenase (SDH, complex II) and cytochrome c oxidase (COX, complex IV) were also spectrophotometrically measured in the left ventricle tissue homogenates as previously described [34].
Western blot analyses
The myocardial and cardiomyocyte samples were homogenized in lysis buffer (Beyotime Biotechnology, Haimeng, Jiangsu, China) using a 1 % protease inhibitor cocktail. The lysates were centrifuged for 15 min at 12,000×g, and the resulting supernatant was transferred to a new tube and stored at −70 °C. The protein concentrations were determined using a Bradford protein assay kit, and the proteins were separated via electrophoresis and transferred to nitrocellulose membranes. The membranes were blocked for 1 h in Tris-buffered saline and Tween 20 (TBST, pH 7.6) containing 5 % non-fat dry milk before being incubated overnight at 4 °C with antibodies against SIRT1, PGC-1α (1:500 dilutions), Bcl2, Bax, Caspase 3, and β-actin (1:1000 dilution). The membranes were then washed with TBST and subsequently probed with the appropriate secondary antibodies (1:5000 dilution) at room temperature for 90 min. The membranes were washed again in TBST, and the protein bands on the membranes were detected using a Bio-Rad imaging system (Bio-Rad, Hercules, CA, USA) and quantified using the Quantity One software package (West Berkeley, CA, USA).
Statistical analysis
The results are expressed as the means ± standard deviations (SDs). Significance was determined using a two-tailed Student’s t test and one-way ANOVA, followed by the Tukey post hoc test, using statistical software (Prism 5.0 GraphPad Software, Inc., La Jolla, CA, USA); P < 0.05 was considered to indicate significant differences.
Results
The effects of BAK on LVDP, LDH release, CK-MB release, and SIRT1 expression in normal rat hearts
Following 110 min of perfusion, BAK (0.25, 0.5, or 1 µM) treatment did not affect the LVDP (P > 0.05 vs. the control group, Fig. 2a). Additionally, BAK treatment did not affect the LDH (Fig. 2b) or CK-MB (Fig. 2c) release in the coronary effluent (P > 0.05 vs. the control group). Interestingly, BAK significantly increased the levels of SIRT1 and PGC-1α expression in the normal hearts in a dose-dependent manner (Fig. 2d).
The effects of BAK on LVDP, LDH release, CK-MB release, and SIRT1 and PGC-1α expression in the normal rat hearts. a A representative line graph of the LVDP curves. b The level of LDH was normalized to the net heart weight and is expressed in IU/g. c The level of CK-MB was normalized to the net heart weight and is expressed in IU/g. d A representative image of the SIRT1 and PGC-1α Western blot results is depicted. The results are expressed as the means ± SDs, n = 8, aP < 0.05 versus the control group, bP < 0.05 versus the IR group, cP < 0.05 vsersu the 0.25 µM BAK + IR group, dP < 0.0 versus the 0.5 µM BAK + IR group. BAK bakuchiol, LVDP left ventricular peak developing pressure
The effects of BAK on cardiac function, apoptotic index, LDH release, and CK-MB release in IR-injured hearts
Following the IR procedure, the absolute values of LVDP, +dP/dt max, CF, and HR decreased significantly compared with their baseline values (P < 0.05). BAK treatment (0.25, 0.5, or 1 µM) significantly increased the functional recovery of post-ischemic hearts, as demonstrated by dose-dependent increases in the LVDP, +dP/dt max, CF, and HR values throughout the reperfusion period (P < 0.05 vs. the IR group, Fig. 3a–d). The apoptotic index in IR hearts was 59.80 ± 4.73 %, and BAK treatment (0.25, 0.5, or 1 µM) facilitated significant dose-dependent reductions in the apoptotic index to 39.10 ± 4.26, 29.55 ± 3.41, and 16.48 ± 3.49 % (P < 0.05 vs. the IR group), respectively (Fig. 4a). The total amounts of released LDH and CK-MB in the IR group were 131.79 ± 7.50 (Fig. 4b) and 62.44 ± 4.59 IU/L/g of wet weight, respectively (Fig. 4c). BAK treatment (0.25, 0.5, or 1 µM) also significantly reduced LDH release to 99.17 ± 5.42, 82.29 ± 4.66, and 69.17 ± 4.40 IU/L/g of wet weight (P < 0.05 vs. the IR group), respectively, and reduced CK-MB release to 55.18 ± 4.18, 40.03 ± 3.94, and 33.15 ± 3.50 IU/L/g of wet weight (P < 0.05 vs. the IR group), respectively. These changes were most significant in response to 1 μM BAK; therefore, this value was selected for pre-treatment in subsequent experiments.
The effects of BAK on cardiac function in the IR-injured hearts. a A representative line graph of the LVDP curves. b A representative line graph of the +dP/dt curves. c A representative line graph of the CF curves. d A representative line graph of the HR curves. The results are expressed as the means ± SDs, n = 8, aP < 0.05 versus the control group, bP < 0.05 versus the IR group, cP < 0.05 versus the 0.25 µM BAK + IR group, dP < 0.0 versus the 0.5 µM BAK + IR group. BAK bakuchiol, LVDP left ventricular peak developing pressure, +dP/dt max the maximum rate of pressure change in the ventricle, CF coronary flow, HR heart rate
The effects of BAK on apoptotic index, LDH release, and CK-MB release in the IR-injured hearts. a Representative images of apoptotic cardiomyocytes are presented (×400). The apoptotic cells were detected using immunofluorescence staining with TUNEL (green), and the nuclei were labeled with DAPI (blue). b The level of LDH was normalized to the net heart weight and is expressed in IU/g. c The level of CK-MB was normalized to the net heart weight and is expressed in IU/g. The results are expressed as the means ± SDs, n = 8, aP < 0.05 versus the control group, bP < 0.05 versus the IR group, cP < 0.05 versus the 0.25 µM BAK + IR group, dP < 0.0 versus the 0.5 µM BAK + IR group. BAK bakuchiol (Color figure online)
The effects of BAK on the mitochondrial oxidative damage indicators of IR-injured hearts
The mitochondrial oxidative damage indicators underwent additional measurements. As expected, the mitochondrial SDH (Fig. 5a), COX (Fig. 5b), and SOD activities (Fig. 5c) and mitochondrial E h (Fig. 5f) were significantly decreased, whereas the MDA (Fig. 5d) and H2O2 (Fig. 5e) content was significantly increased, in the IR group (P < 0.05 vs. the control group). BAK treatment significantly increased the SDH, COX, SOD activities and mitochondrial E h , as well as decreased the MDA content and H2O2 formation (P < 0.05 vs. the IR group). These effects were most significant with 1 μM BAK, which increased the SDH, COX, SOD activities and mitochondrial E h to 6.30 ± 0.49 U/mg of protein, 67.08 ± 4.31 mM/min/mg of protein, 19.40 ± 1.53 U/mg of protein, and 191.24 ± 16.88 mV, respectively, and decreased the MDA content and H2O2 formation to 1.14 ± 0.19 nM/mg of protein and 91.32 ± 5.11 μM/mg protein, respectively.
The effects of BAK on the mitochondrial oxidative damage indicators of the IR-injured hearts. a SDH activity in the mitochondria. b COX activity in the mitochondria. c SOD activity in the mitochondria. d MDA production in the mitochondria. e H2O2 production in the mitochondria. f GSH and GSSG in mitochondria were calculated based on the redox potential (E h ). The results are expressed as the means ± SDs, n = 8, aP < 0.05 versus the control group, bP < 0.05 versus the IR group, cP < 0.05 versus the 0.25 µM BAK + IR group, dP < 0.0 versus the 0.5 µM BAK + IR group. BAK bakuchiol, SDH succinate dehydrogenase, COX cytochrome c oxidase, SOD superoxide dismutase, MDA malondialdehyde, E h mitochondrial redox potential
The effects of BAK on SIRT1, PGC-1α, Bcl2, Bax, and cleaved Caspase 3 expression in IR-injured hearts
As depicted in Fig. 6, the levels of SIRT1, PGC-1α, and Bcl2 expression significantly decreased, whereas Bax and cleaved Caspase 3 expression significantly increased, in the IR group (P < 0.05 vs. the control group). BAK treatment significantly increased the levels of SIRT1, PGC-1α, and Bcl2 expression and decreased the level of Bax and cleaved Caspase 3 expression (P < 0.05 vs. the IR group). These effects were most significant with 1 μM BAK, which increased the levels of SIRT1, PGC-1α, and Bcl2 expression to 61.08 ± 4.20, 67.30 ± 4.77, and 74.69 ± 4.46 %, respectively, and decreased the levels of Bax and cleaved Caspase 3 expression to 96.16 ± 4.75 and 166.91 ± 15.88 %, respectively.
The effects of BAK on SIRT1, PGC-1α, cleaved Caspase 3, Bcl2 and Bax expression in the IR-injured hearts. Representative images of the Western blot results are provided. The results are expressed as the means ± SDs, n = 8, aP < 0.05 versus the control group, bP < 0.05 versus the IR group, cP < 0.05 versus the 0.25 µM BAK + IR group, dP < 0.0 versus the 0.5 µM BAK + IR group. BAK bakuchiol
The effects of BAK and Sirtinol on LVDP, LDH release, and CK-MB release in IR-injured isolated hearts
Additional experiments were performed to determine the role of SIRT1/PGC-1α signaling in the myocardial protective effects of BAK. Sirtinol was used as an SIRT1 inhibitor. As depicted in Fig. 7a–c, BAK (1 μM) treatment significantly increased LVDP to 64.98 ± 7.25 mmHg following 60 min of reperfusion and decreased LDH and CK-MB release to 65.04 ± 4.37 and 35.69 ± 3.64 IU/L/g of wet weight (P < 0.05 vs. IR group), respectively. Sirtinol (3.75 μM), a specific inhibitor of SIRT1 based on our previous research [32], reversed the protective effects of BAK, decreased LVDP to 50.4 ± 6.6 mmHg, and increased LDH and CK-MB release to 107.12 ± 6.59 and 55.90 ± 4.50 IU/L/g of wet weight (P < 0.05 vs. BAK + IR group), respectively. Compared with the IR group, Sirtinol + IR treatment did not affect the LVDP, LDH release, and CK-MB release (P > 0.05). However, Sirtinol treatment alone did not affect the expressions of these targets.
The effects of BAK and Sirtinol on LVDP, LDH release, CK-MB release, and the mitochondrial oxidative damage indicators of the IR-injured isolated hearts. a A representative line graph of the LVDP curves. b The level of LDH was normalized to the net heart weight and is expressed in IU/g. c The level of CK-MB was normalized to the net heart weight and is expressed in IU/g. d SDH activity in the mitochondria. e COX activity in the mitochondria. f SOD activity in the mitochondria. g MDA production in the mitochondria. h H2O2 production in the mitochondria. i GSH and GSSG in the mitochondria were calculated based on the redox potential (E h ). The results are expressed as the means ± SDs, n = 8, aP < 0.05 versus the IR group, bP < 0.05 versus the BAK + IR group, cP < 0.05 versus the BAK + Sirtinol + IR group. BAK bakuchiol, LVDP left ventricular peak developing pressure, SDH succinate dehydrogenase, COX cytochrome c oxidase, SOD superoxide dismutase, MDA malondialdehyde, E h mitochondrial redox potential
The effects of BAK and Sirtinol on the mitochondrial oxidative damage indicators of IR-injured hearts
As depicted in Fig. 7d–i, BAK treatment significantly increased the SDH, COX, and SOD activities and mitochondrial E h to 6.37 ± 0.48 U/mg of protein, 69.18 ± 4.60 mM/min/mg of protein, 18.93 ± 1.69 U/mg of protein, and 186.93 ± 15.48 mV, respectively, and decreased the MDA content and H2O2 formation to 1.09 ± 0.17 nM/mg of protein and 89.55 ± 5.01 μM/mg protein, respectively (P < 0.05 vs. IR group). Sirtinol reversed the mitochondrial protective effects of BAK and decreased the SDH, COX, and SOD activities and mitochondrial E h to 5.29 ± 0.41 U/mg of protein, 51.65 ± 3.77 mM/min/mg of protein, 13.17 ± 1.27 U/mg of protein, and 168.21 ± 16.42 mV, respectively. It also decreased MDA content and H2O2 formation to 1.78 ± 0.19 nM/mg of protein and 116.57 ± 5.98 μM/mg protein, respectively (P < 0.05 vs. BAK + IR group). Compared with the IR group, Sirtinol + IR treatment did not affect the SDH, COX, or SOD activities, mitochondrial E h , MDA content, or H2O2 formation (P > 0.05).
The effects of BAK and Sirtinol on SIRT1, PGC-1α, Bcl2, Bax, and cleaved Caspase 3 expression in IR-injured hearts
As depicted in Fig. 8, BAK treatment significantly increased the levels of SIRT1, PGC-1α, and Bcl2 expression to 294.03 ± 17.52, 279.20 ± 16.28, and 336.37 ± 19.29 %, respectively, and decreased the level of Bax and cleaved Caspase 3 expression to 19.78 ± 2.14 and 146.22 ± 14.61 %, respectively (P < 0.05 vs. IR group). Sirtinol not only effectively inhibited SIRT and PGC-1α expression (P < 0.05, shown in Supplementary Fig. 1) but also reversed the effect of BAK and decreased the levels of SIRT1, PGC-1α, and Bcl2 expression to 86.48 ± 4.61, 188.09 ± 10.64, and 77.16 ± 4.71 %, respectively, and increased the levels of Bax and cleaved Caspase 3 expression to 80.05 ± 4.83 and 206.21 ± 20.55 %, respectively (P < 0.05 vs. BAK + IR group). Compared with the IR group, Sirtinol + IR treatment effectively decreased the levels of SIRT1 and PGC-1α expression to 19.09 ± 2.35 and 25.64 ± 3.26 %, respectively (P < 0.05).
The effects of BAK and Sirtinol on SIRT1, PGC-1α, cleaved Caspase 3, Bcl2 and Bax expression in the IR-injured hearts. Representative images of the Western blot results are provided. The results are expressed as the means ± SDs, n = 8, aP < 0.05 versus the control group, bP < 0.05 versus the IR group, cP < 0.05 versus the BAK + IR group, dP < 0.05 versus the BAK + Sirtinol + IR group. BAK bakuchiol
The effects of BAK and SIRT1 siRNA pretreatment on the cell viability, apoptotic index, and mitochondrial oxidative damage indicators of IR-injured cardiomyocytes
The cardiomyocyte results were consistent with those that were obtained from the isolated rat. The cell viability was analyzed by the MTT assay. Pretreatment with BAK markedly increased cell viability following IR (vs. control siRNA + IR group, P < 0.05, Supplementary Fig. 2A). In addition, BAK pretreatment significantly decreased the apoptotic index (vs. control siRNA + IR group, P < 0.05, Supplementary Fig. 2B). However, the protective effect of BAK pretreatment was abolished by SIRT1 siRNA (vs. control siRNA + BAK + IR group, P < 0.05). Significantly reduced levels of LDH (Supplementary Fig. 2C) and MDA (Supplementary Fig. 2E) were observed in the control siRNA + BAK + IR group compared with the control siRNA + IR group (P < 0.05). In addition, BAK pretreatment significantly increased mitochondrial SOD (vs. control siRNA + IR group, P < 0.05, Supplementary Fig. 2D). However, SIRT1 siRNA pretreatment abolished most of the protective effect afforded by BAK pretreatment (P < 0.05). Compared with the control group, control siRNA had no effect on the cell viability, apoptotic index, and LDH, SOD, and MDA release.
The effects of BAK and SIRT1 siRNA pretreatment on SIRT1, PGC-1α, Bcl2, Bax, and cleaved Caspase 3 expression in IR-injured cardiomyocytes
As depicted in Supplementary Fig. 3, BAK pretreatment significantly increased SIRT1, PGC-1α, and Bcl2 and decreased Bax and cleaved Caspase 3 expression (vs. the control siRNA + IR group, P < 0.05). However, the effect of BAK pretreatment on the expression of these proteins was abolished by SIRT1 siRNA (vs. control siRNA + BAK + IR group, P < 0.05). As expected, SIRT1 siRNA + IR treatment significantly decreased SIRT1 expression (vs. IR group, P < 0.05).
Discussion
BAK, a monoterpene phenol isolated from the seeds of P. corylifolia (Leguminosae) [6], exerts many biological and pharmacological effects. Park et al. observed that BAK protects against the hepatocyte toxicants tert-butyl hydroperoxide and carbon tetrachloride and attenuates D-GalN-induced toxicity in the liver [8]. In another study, Park et al. suggested that BAK protects the liver from fibrosis and cirrhosis via caspase-3-dependent apoptosis by preventing the c-Jun NH2-terminal kinase-mediated mitochondrial translocation of Bax [7]. Additionally, Chaudhuri and Bojanowski observed that BAK, a retinol-like functional compound, significantly improves the lines and wrinkles, pigmentation, elasticity, firmness, and photo-damage of the skin [9]. Importantly, although the direct relationship between BAK and myocardial IRI has not been elucidated, BAK has been indicated to inhibit the pathogenesis of myocardial IRI, including oxidative stress, inflammation, and diabetes [14–16]. Seo et al. confirmed that BAK inhibits oxidative stress-induced ROS production and mitochondrial dysfunction [10]. Moreover, Choi et al. suggested that BAK is a potent anti-inflammatory compound [12], and Krenisky et al. observed the protective effects of BAK in the setting of diabetes [13]. Therefore, BAK likely plays a protective role in myocardial IRI. In this study, BAK pre-treatment protected isolated rat hearts, as demonstrated by improvements in the physiological, enzymologic, and cell survival indices, including improvements in the LDVP, dP/dt max, CF, heart rate, and LDH and CK-MB release, as well as decreased cardiomyocyte apoptosis.
SIRT1 is a member of the class III group of histone deacetylases, which deacetylate many transcription factors and nuclear co-activators and are involved in the protection of many organs and tissues, including the heart and brain [17]. Zhang et al. observed that interferon regulatory factor 9 mediated myocardial IRI by negatively regulating the SIRT1-p53 axis in the setting of IR, both in vivo and in vitro. SIRT1 protects cardiomyocytes from myocardial IRI via deacetylase activity, which promotes the deacetylation of acetyl-p53 and downregulates a downstream apoptosis-related signaling cascade [35]. Lysine deacetylation occurs during IPC, and Nadtochiy et al. suggested that increased SIRT1 activity plays a role in this phenomenon. The inhibition of SIRT1, either directly or by restricting the availability of its substrate, NAD+, inhibits IPC. These data suggest a role for SIRT1-mediated lysine deacetylation in the mechanism underlying acute IPC [20]. Moreover, Hong et al. observed that resveratrol downregulates c-Myc and β-catenin via SIRT1 activation, mimicking the effects of IPC [21]. Additionally, Paschalaki et al. observed that SIRT1 upregulation attenuated DNA damage and the senescence of endothelial progenitor cells in smokers and patients with chronic obstructive pulmonary disease, exerting cardiovascular protective effects [36]. Furthermore, Li et al. demonstrated that resveratrol protects cardiomyocytes from oxidative stress via SIRT1 and mitochondrial biogenesis signaling pathways [22]. Similarly, Shalwala et al. suggested that SIRT1 activation mediates sildenafil- and resveratrol-induced cardioprotection against IRI in mice [37], and Sun et al. observed that resveratrol protects hypothermic preserved isolated rat hearts from injury via the upregulation of SIRT1 expression [38]. Importantly, previous studies have demonstrated that SIRT1 activates PGC-1α and plays a role in the attenuation of IRI. Zhu et al. suggested that icariin protects against IRI by enhancing SIRT1-dependent PGC-1α expression in the setting of cerebral ischemic stroke [25], and Fu et al. demonstrated that α-lipoic acid upregulates SIRT1 expression [24]. The overexpression of SIRT1 activates the transcriptional activity of PGC-1α and protects the brain against focal ischemia in mice [24]. BAK is an analog of resveratrol, which inhibits ROS generation in cardiomyocytes via SIRT1 [22]. Therefore, we hypothesized that BAK protected tissues from myocardial IRI by attenuating oxidative stress via the SIRT1/PGC-1α pathway. In this study, treating normal hearts with BAK induced a dose-dependent increase in SIRT1 and PGC-1α expression in the absence of significant differences in the LDVP and LDH levels and CK-MB release. IR significantly decreased both SIRT1 and PGC-1α expression in isolated hearts, whereas BAK pre-treatment significantly restored SIRT1 and PGC-1α expression in a dose-dependent manner. However, inhibiting SIRT1 with Sirtinol and SIRT1 siRNA abolished the BAK-mediated increases in the expression of SIRT1 and PGC-1α. Moreover, the SIRT1 upregulation induced by BAK treatment was also related to an increase in the level of the apoptosis-related factor cleaved Caspase 3 and anti-apoptotic factor Bcl2, as well as a reduction in the level of the pro-apoptotic factor Bax. Additionally, previous studies have demonstrated that SIRT1 inhibits apoptotic signals by inducing Bcl2 expression and reducing Bax expression [39]. Therefore, BAK pre-treatment protects cardiac tissue via SIRT1-dependent PGC-1α activation and the induction of downstream signals associated with anti-apoptotic effects in the heart.
Resveratrol treatment has been shown to improve mitochondrial biogenesis and function in the setting of IRI, while the inhibition of SIRT1 reversed these benefits [20, 23], indicating that SIRT1 activity reduces mitochondrial oxidative stress and maintains mitochondrial function. Additionally, Della-Morte et al. suggested that the resveratrol-mediated upregulation of SIRT1 inhibits mitochondrial uncoupling protein 2 (UCP2), which has been linked to mitochondrial dysfunction [40]. Das et al. also determined that the resveratrol-mediated upregulation of SIRT1 protects cardiac tissue by activating the Forkhead box, subgroup O (Foxo3a)/PTEN-induced kinase 1 (PINK1)/PARKIN signaling pathway, resulting in mitochondrial fission and mitophagy, as well as the attenuation of oxidative injury [41]. Mitochondrial oxidative stress is a significant pathological consequence of IRI and increases mitochondrial oxidative damage, which subsequently accelerates both the development and progression of oxidative stress. In this study, we investigated the redox status of mitochondria following ischemia in isolated hearts. The results of these experiments suggested that BAK pre-treatment maintained mitochondrial function, as evidenced by significant improvements in the mitochondrial SDH, COX, and SOD activities. Moreover, increased mitochondrial E h and decreased mitochondrial MDA content and H2O2 formation were also observed, which indicates that the mitochondrial oxidative damage caused by IRI was attenuated. However, Sirtinol and SIRT1 siRNA abolished the improvements in mitochondrial function secondary to BAK pre-treatment. Together, these findings indicate that BAK attenuates myocardial IRI-induced mitochondrial oxidative damage via SIRT1 activation.
Our findings suggest that BAK treatment exerts promising cardioprotective effects in the setting of IRI. These effects were primarily attributed to the activation of SIRT1/PGC-1α signaling and the attenuation of mitochondrial oxidative injury, as SIRT1/PGC-1α signaling attenuates the myocardial IRI-induced mitochondrial oxidative damage (Fig. 9). These results indicate that BAK may play a promising role in the treatment of myocardial IRI in the setting of cardiac surgery and ischemic heart disease.
The SIRT1-dependent mechanism of the cardioprotective effects against IRI afforded by BAK. BAK upregulated SIRT1, which subsequently triggered PGC-1α expression. The downstream effects included improvements in SDH, COX, and SOD activities; improvements in mitochondrial redox potential (E h ); and decreased MDA and H2O2 contents in the mitochondria. These changes resulted in an increase in the level of the anti-apoptotic factor Bcl2 and a decrease in the level of the pro-apoptotic factor cleaved Caspase 3 and Bax, resulting in cardioprotective effects against myocardial IRI. SIRT1 silent information regulator 1, IRI ischemia reperfusion injury, BAK bakuchiol, SDH succinate dehydrogenase, COX cyclooxygenase, SOD superoxide dismutase, MDA malondialdehyde
References
Zhu KF, Wang YM, Zhu JZ, Zhou QY, Wang NF (2015) National prevalence of coronary heart disease and its relationship with human development index: a systematic review. Eur J Prev Cardiol. doi:10.1177/2047487315587402
Buja LM (2013) The pathobiology of acute coronary syndromes: clinical implications and central role of the mitochondria. Tex Heart Inst J 40:221–228
Murphy E, Steenbergen C (2008) Mechanisms underlying acute protection from cardiac ischemia-reperfusion injury. Physiol Rev 88:581–609
Gill R, Kuriakose R, Gertz ZM, Salloum FN, Xi L, Kukreja RC (2015) Remote ischemic preconditioning for myocardial protection: update on mechanisms and clinical relevance. Mol Cell Biochem 402:41–49
Ferdinandy P, Hausenloy DJ, Heusch G, Baxter GF, Schulz R (2014) Interaction of risk factors, comorbidities, and comedications with ischemia/reperfusion injury and cardioprotection by preconditioning, postconditioning, and remote conditioning. Pharmacol Rev 66:1142–1174
Chopra B, Dhingra AK, Dhar KL (2013) Psoralea corylifolia L. (Buguchi)—folklore to modern evidence: review. Fitoterapia 90:44–56
Park EJ, Zhao YZ, Kim YC, Sohn DH (2007) Bakuchiol-induced caspase-3-dependent apoptosis occurs through c-Jun NH2-terminal kinase-mediated mitochondrial translocation of Bax in rat liver myofibroblasts. Eur J Pharmacol 559:115–123
Park EJ, Zhao YZ, Kim YC, Sohn DH (2005) Protective effect of (S)-bakuchiol from Psoralea corylifolia on rat liver injury in vitro and in vivo. Planta Med 71:508–513
Chaudhuri RK, Bojanowski K (2014) Bakuchiol: a retinol-like functional compound revealed by gene expression profiling and clinically proven to have anti-aging effects. Int J Cosmet Sci 36:221–230
Seo E, Oh YS, Kim D, Lee MY, Chae S, Jun HS (2013) Protective role of Psoralea corylifolia L. Seed extract against hepatic mitochondrial dysfunction induced by oxidative stress or aging. Evid Based Complement Alternat Med. 2013:678028
Kim KA, Shim SH, Ahn HR, Jung SH (2013) Protective effects of the compounds isolated from the seed of Psoralea corylifolia on oxidative stress-induced retinal damage. Toxicol Appl Pharmacol 269:109–120
Choi SY, Lee S, Choi WH, Lee Y, Jo YO, Ha TY (2010) Isolation and anti-inflammatory activity of Bakuchiol from Ulmus davidiana var. japonica. J Med Food 13:1019–1023
Krenisky JM, Luo J, Reed MJ, Carney JR (1999) Isolation and antihyperglycemic activity of bakuchiol from Otholobium pubescens (Fabaceae), a Peruvian medicinal plant used for the treatment of diabetes. Biol Pharm Bull 22:1137–1140
Pant R, Marok R, Klein LW (2014) Pathophysiology of coronary vascular remodeling: relationship with traditional risk factors for coronary artery disease. Cardiol Rev 22:13–16
Osipov RM, Bianchi C, Feng J et al (2009) Effect of hypercholesterolemia on myocardial necrosis and apoptosis in the setting of ischemia-reperfusion. Circulation 120:S22–S30
Holzmann MJ, Rathsman B, Eliasson B et al (2015) Long-term prognosis in patients with type 1 and 2 diabetes mellitus after coronary artery bypass grafting. J Am Coll Cardiol 65:1644–1652
Yang Y, Duan W, Li Y et al (2013) Novel role of silent information regulator 1 in myocardial ischemia. Circulation 128:2232–2240
Yang Y, Duan W, Li Y et al (2013) New role of silent information regulator 1 in cerebral ischemia. Neurobiol Aging 34:2879–2888
Holthoff JH, Woodling KA, Doerge DR, Burns ST, Hinson JA, Mayeux PR (2010) Resveratrol, a dietary polyphenolic phytoalexin, is a functional scavenger of peroxynitrite. Biochem Pharmacol 80:1260–1265
Nadtochiy SM, Redman E, Rahman I, Brookes PS (2011) Lysine deacetylation in ischaemic preconditioning: the role of SIRT1. Cardiovasc Res 89:643–649
Hong KS, Park JI, Kim MJ et al (2012) Involvement of SIRT1 in hypoxic down-regulation of c-Myc and beta-catenin and hypoxic preconditioning effect of polyphenols. Toxicol Appl Pharmacol 259:210–218
Li YG, Zhu W, Tao JP et al (2013) Resveratrol protects cardiomyocytes from oxidative stress through SIRT1 and mitochondrial biogenesis signaling pathways. Biochem Biophys Res Commun 438:270–276
Price NL, Gomes AP, Ling AJ et al (2012) SIRT1 is required for AMPK activation and the beneficial effects of resveratrol on mitochondrial function. Cell Metab 15:675–690
Fu B, Zhang J, Zhang X et al (2014) Alpha-lipoic acid upregulates SIRT1-dependent PGC-1alpha expression and protects mouse brain against focal ischemia. Neuroscience 281C:251–257
Zhu HR, Wang ZY, Zhu XL, Wu XX, Li EG, Xu Y (2010) Icariin protects against brain injury by enhancing SIRT1-dependent PGC-1alpha expression in experimental stroke. Neuropharmacology 59:70–76
Funk JA, Schnellmann RG (2013) Accelerated recovery of renal mitochondrial and tubule homeostasis with SIRT1/PGC-1alpha activation following ischemia-reperfusion injury. Toxicol Appl Pharmacol 273:345–354
Liu P, Zou D, Yi L et al (2015) Quercetin ameliorates hypobaric hypoxia-induced memory impairment through mitochondrial and neuron function adaptation via the PGC-1alpha pathway. Restor Neurol Neurosci 33:143–157
Dong DG, Zhang Y, Zhang SL et al (2014) Inhibition potential of UDP-glucuronosyltransferases (Ugts) 1A isoforms by the analogue of resveratrol, bakuchiol. Pharmazie 69:60–63
Yang Y, Duan W, Jin Z et al (2013) JAK2/STAT3 activation by melatonin attenuates the mitochondrial oxidative damage induced by myocardial ischemia/reperfusion injury. J Pineal Res 55:275–286
Gorbe A, Giricz Z, Szunyog A et al (2010) Role of cGMP-PKG signaling in the protection of neonatal rat cardiac myocytes subjected to simulated ischemia/reoxygenation. Basic Res Cardiol 105:643–650
Di S, Fan C, Yang Y et al (2015) Activation of endoplasmic reticulum stress is involved in the activity of icariin against human lung adenocarcinoma cells. Apoptosis. 20(9):1229–1241
Yang Y, Duan W, Lin Y et al (2013) SIRT1 activation by curcumin pretreatment attenuates mitochondrial oxidative damage induced by myocardial ischemia reperfusion injury. Free Radic Biol Med 65:667–679
Li T, Zhang P, Liu J et al (2010) Protective effects of hemoglobin-based oxygen carrier given to isolated heart during ischemia via attenuation of mitochondrial oxidative damage. Free Radic Biol Med 48:1079–1089
Jouihan HA, Cobine PA, Cooksey RC et al (2008) Iron-mediated inhibition of mitochondrial manganese uptake mediates mitochondrial dysfunction in a mouse model of hemochromatosis. Mol Med 14:98–108
Zhang Y, Liu X, She ZG et al (2014) Interferon regulatory factor 9 is an essential mediator of heart dysfunction and cell death following myocardial ischemia/reperfusion injury. Basic Res Cardiol 109:434
Paschalaki KE, Starke RD, Hu Y et al (2013) Dysfunction of endothelial progenitor cells from smokers and chronic obstructive pulmonary disease patients due to increased DNA damage and senescence. Stem Cells 31:2813–2826
Shalwala M, Zhu SG, Das A, Salloum FN, Xi L, Kukreja RC (2014) Sirtuin 1 (SIRT1) activation mediates sildenafil induced delayed cardioprotection against ischemia-reperfusion injury in mice. PLoS One 9:e86977
Sun WM, Zheng MZ, Ying L et al (2014) Protection of hypothermic preserved isolated rat hearts by resveratrol and its underlying mechanism. Zhongguo Ying Yong Sheng Li Xue Za Zhi 30:348–351 (in Chinese)
Yang Y, Jiang S, Dong Y et al (2015) Melatonin prevents cell death and mitochondrial dysfunction via a SIRT1-dependent mechanism during ischemic-stroke in mice. J Pineal Res 58:61–70
Della-Morte D, Dave KR, DeFazio RA, Bao YC, Raval AP, Perez-Pinzon MA (2009) Resveratrol pretreatment protects rat brain from cerebral ischemic damage via a sirtuin 1-uncoupling protein 2 pathway. Neuroscience 159:993–1002
Das S, Mitrovsky G, Vasanthi HR, Das DK (2014) Antiaging properties of a grape-derived antioxidant are regulated by mitochondrial balance of fusion and fission leading to mitophagy triggered by a signaling network of Sirt1-Sirt3-Foxo3-PINK1-PARKIN. Oxid Med Cell Longev 2014:345105
Acknowledgments
This study was supported by grants from the 12th National Five Years Supporting Project of China (2011BAI11B20), the National Natural Science Foundation of China (81500263, 81470415, 81270170, 81200151, 81470411), China Postdoctoral Science Foundation (2015M572681), the Social Development Project of Shaanxi Province (2015SF104 and 2012K15-02-01), the International Technology Cooperation and Communication Project of Shaanxi Province (2015KW-047), the Scientific Innovation Project of Shaanxi Province (2013KTCL03-01), the Natural Science Foundation of Shaanxi Province (2014JM4106), and the Academic Promotion Project of Xijing Hospital (XJZT14203, XJGX12C11, XJGX13LC15).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest in the studies described.
Additional information
Jianyu Feng, Yang Yang and Yajun Zhou have contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Fig. 1
Effect of Sirtinol treatment on the expression of SIRT1 and PGC-1α proteins in the IR-injured hearts. Representative images of the Western blot results are provided. The results are expressed as the means±SDs, n=8, aP<0.05 vs. the control group.. Supplementary material 1 (TIFF 302 kb)
Supplementary Fig. 2
The effects of BAK and SIRT1 siRNA on the cell viability, apoptotic index, LDH release, and mitochondrial oxidative damage indicators of the IR-injured cardiomyocytes. (A) Cardiomyocyte viability was assessed using the MTT assay. Cell viability is expressed as an OD value. (B) Representative images of apoptotic cardiomyocytes are presented (200×). The apoptotic cells were detected using immunofluorescence staining with TUNEL (green), and the nuclei were labeled with DAPI (blue). (C) The level of LDH was normalized to the net heart weight and is expressed in IU/g. (D) SOD activity in the mitochondria. (E) MDA production in the mitochondria. The results are expressed as the means±SDs, n=8, aP<0.05 vs. the control siRNA+IR group, bP<0.05 vs. the SIRT1 siRNA+IR group, cP<0.05 vs. the control siRNA+BAK+IR group. BAK, bakuchiol. Supplementary material 2 (TIFF 903 kb)
Supplementary Fig. 3
The effect of Cur and SIRT1 siRNA pretreatment on SIRT1, PGC-1α, cleaved Caspase 3, Bcl2 and Bax expression in SIR-injured cardiomyocytes. Representative images of the Western blot results are presented. The results are expressed as the means±SDs, n=8, aP<0.05 vs. the control siRNA+IR group, bP<0.05 vs. the SIRT1 siRNA+IR group, cP<0.05 vs. the control siRNA+BAK+IR group. BAK, bakuchiol. Supplementary material 3 (TIFF 921 kb)
Rights and permissions
About this article
Cite this article
Feng, J., Yang, Y., Zhou, Y. et al. Bakuchiol attenuates myocardial ischemia reperfusion injury by maintaining mitochondrial function: the role of silent information regulator 1. Apoptosis 21, 532–545 (2016). https://doi.org/10.1007/s10495-016-1225-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10495-016-1225-6