Abstract
Anoikis, an apoptosis triggered by loss of cell anchorage, has been shown to be a principal mechanism of inhibition of tumor metastasis. Recently, anti-apoptotic Bcl-2 and Cav-1 proteins have been demonstrated to be highly associated with tumor metastasis and apoptosis resistance. Curcumin, a major active component of turmeric, Curcuma longa, has been shown to inhibit neoplastic evolution and tumor progression; however, the underlying mechanisms are unclear. In this study, we investigated the effect of curcumin on cell anoikis as a possible mechanism of anti-tumorigenic action of curcumin, and evaluated the potential role of Bcl-2 and Cav-1 in this process. Our results showed that ectopic expression of either Bcl-2 or Cav-1 induced anoikis resistance of lung carcinoma H460 cells. Curcumin downregulated Bcl-2 protein during anoikis and sensitized the cells to detachment-induced apoptosis, whereas it had no significant effect on Cav-1 protein expression. Bcl-2 down-regulation as well as anoikis enhancement by curcumin were inhibited by superoxide anion scavenger, Mn(III)tetrakis(4-benzoic acid) porphyrin chloride, but were unaffected by other ROS scavengers including catalase and deferoxamine, suggesting that superoxide anion is a key player in the downregulation of Bcl-2 by curcumin. Furthermore, we provided evidence that curcumin decreased Bcl-2 level through ubiquitin-proteasomal degradation which sensitized cells to detachment-induced apoptosis. These findings indicate a novel pathway for curcumin regulation of Bcl-2 and provide a key mechanism of anoikis regulation that may be exploited for metastatic cancer treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Curcumin, a major active component of the turmeric (Curcuma longa), has been reported to possess a variety of pharmacological actions against cancers, including oncogene suppression, inhibition of cancer cell proliferation, and induction of cancer cell apoptosis both in in vitro and in vivo models [1–5]. Accumulating evidence also indicate that the mechanism by which curcumin induces apoptosis is associated with its pro-oxidant effect [6–8].
Anoikis or detachment-induced apoptosis plays an important role in cancer cell survival during their migration and establishment of secondary tumors. Resistance to anoikis is associated with a high degree of tumor metastasis and advanced stage of cancers [9–12]. Several signaling pathways including c-Jun amino-terminal kinase (JNK) [13], phosphatidylinositol-3 kinase (PI3 K)/Akt [14], focal adhesion kinase (FAK) [15], and extracellular signal-regulated protein kinase (ERK) [16, 17] have been implicated in anoikis regulation. Moreover, increasing evidence suggest the importance of apoptosis-regulatory proteins in the Bcl-2 family in cell survival after detachment [18]. Anoikis is initiated by the upregulation of pro-apoptotic Bcl-2 proteins such as Bim, Bmf, Bax, and Bid and/or downregulation of the anti-apoptotic Bcl-2 and Bcl-XL proteins [17–23]. Such dysregulation disrupts mitochondrial function, causing the release of cytochrome c from the mitochondrial intermembrane space and subsequent activation of caspase cascades [24, 25]. An upregulation of Bcl-2 has been shown to suppress anoikis of cancer cells [18, 26]. The expression of Bcl-2 is tightly regulated by different mechanisms, including transcription, heterodimerization, post-translational modifications and degradation. Among these, Bcl-2 degradation has been shown to be a key mechanism of Bcl-2 regulation during cell apoptosis [27, 28]. Bcl-2 degradation is mediated primarily through the ubiquitin–proteasome pathway [27, 28], which promotes apoptosis induced by various pathological stimuli and chemotherapeutic agents [8, 28–31].
Caveolin-1 (Cav-1), a 21–24 kDa structural protein of caveolae in plasma membrane, has garnered increasing attention in cancer research. It has been implicated in cancer cell proliferation, transformation and metastasis [32, 33]. Previous studies have also shown that overexpression of Cav-1 promotes survival and suppresses anoikis of cancer cells [34–36]. Therefore, Cav-1 could be involved in the regulation of cell anoikis induced by curcumin. The specific objectives of this study are to test (1) whether curcumin can induce anoikis of lung cancer cells, (2) whether this effect is mediated by ROS, and if so, what is the major ROS involved, and (3) whether Bcl-2 and Cav-1 play a role in the anoikis regulation.
Materials and methods
Cell culture and reagents
Non-small cell lung carcinoma H460, bronchial epithelial BEAS-2B, and melanoma G361 cells were obtained from American Type Culture Collection (Manassas, VA). H460 cells were cultured in RPMI medium, while BEAS-2B and G361 cells were cultured in DMEM medium. All media were supplemented with 10% of bovine fetal serum (FBS), 2 mmol/l L-glutamine, and 100 units/ml penicillin/streptomycin. Curcumin, Mn(III)tetrakis(4-benzoic acid)porphyrin chloride (MnTBAP), 2,3-Bis(2-methoxy-4-nitro-5-sulfophenyl)-2H-tetrazolium-5 carboxanilide inner salt (XTT), dihydroethidium (DHE), deferoxamine, catalase, cisplatin, and paclitaxel were obtained from Sigma Chemical, Inc. (St. Louis, MO). Propidium iodide (PI), dihydrodichlorofluorescein diacetate (H2DCF-DA), and Hoechst 33342 were obtained from Molecular Probes, Inc. (Eugene, OR). PromoFectin transfecting agent was obtained from PRomoKine (Heidelberg, Germany). Rabbit anti-Bcl-2 antibody and peroxidase-conjugated anti-rabbit secondary antibody were purchased from Abcam (Cambridge, MA). Protein A-conjugated Sepharose, mouse anti-Cav-1 and mouse anti-beta actin were purchased from Santa Cruz Biotechnology (Santa Cruz, CA). Rabbit anti-Mcl-1 antibody and rabbit anti-Bax antibody were purchased from Cell Signaling (Danvers, MA). Other biochemical reagents were obtained from Sigma Chemical, Inc.
Plasmid and stable transfection
Bcl-2 plasmid was generously provided by Dr. Christian Stehlik (Northwestern University, Chicago, IL). Cav-1 plasmid was obtained from American Type Culture Collection. Authenticity of the constructs was verified by DNA sequencing. Stable transfection was performed using PromoFectin® reagent according to manufacturer’s instruction. Briefly, H460 cells were cultured on 24-well plates until they reached 50–60% confluence. One microgram of Bcl-2, Cav-1 or pcDNA3 plasmid and 2 μl of Promofectin solution were mixed and incubated at room temperature for 30 min, then added to the cells in the absence of serum. After 24 h, the medium was replaced with culture medium containing 10% FBS. For stable transfection, H460 cells were maintained in medium containing 50 μg/ml of neomycin which gradually increased to 1,000 μg/ml for a month. Stable transfectants were identified by Western blot analysis. Bcl-2 overexpressing cells and Cav-1 overexpressing cells were cultured in normal growth medium without neomycin for 2 weeks before experiments were carried out.
Anoikis assay
Tissue culture six-well plates were coated with 6 mg/ml poly(2-hydroxyethyl-methacrylate (poly-HEMA) (Sigma–Aldrich, St. Louis, MO) in 95% ethanol and incubated at 37°C for drying. Cells were plated in poly-HEMA-coated plates in RPMI medium at a density of 20,000 cells/well for 24 h. Cell anoikis was determined by XTT assay. Briefly, XTT reagent (0.3 mg/ml) was added to each well, followed by incubation for 4 h at 37°C. The intensity of formazan product was determined at 450 nm using a microplate reader. Relative cell viability is calculated by dividing the OD reading of the sample by that of the control.
Apoptosis assay
Apoptosis was determined by Hoechst 33342/propidium iodide (PI) staining and by flow cytometric assays. Cells were incubated with 10 μg/ml of Hoechst 33342 or 5 μg/ml of PI, and apoptotic nuclei were visualized under a fluorescence microscope (Olympus IX51 with DP70). Apoptotic DNA fragmentation was determined by cell cycle analysis of sub G0 fraction using PI. Cells were incubated with 0.05% Triton X for 15 min, stained with 5 μg/ml of PI, and immediately analyzed for fluorescence intensity by FACScan flow cytometer (Beckton Dickinson, Rutheford, NJ) using a 488-nm excitation beam and a 630-nm band-pass filter with CellQuest software (Beckton Dickinson).
Caspase activity assay
Caspase-3 activity was measured by using APO LOGIX carboxyfluoroscein caspase detection kit (Cell Technologies, Minneapolis, MN), according to the manufacturer’s instructions. After treatment with various concentrations of curcumin for 6 h, detached H460 cells were incubated with 10 μl of 30× FAM-DEVD-FMK for 2 h at 37°C in dark. Media were then aspirated gently and cells were washed with 1× Working Dilution Wash Buffer which was supplied with the kit. The fluorescence signals were measured using a fluorescence microplate reader at the excitation and emission wavelengths of 488 and 520 nm, respectively, Caspase activity was expressed as the ratio of fluorescence signal from treated and control samples.
ROS detection
Intracellular ROS were determined by flow cytometry using dihydrodichloro-fluorescein diacetate (H2DCF-DA) as a fluorescent probe. Briefly, cells were incubated with 10 μmol/l of H2DCF-DA for 30 min at 37°C, after which they were washed, resuspended in phosphate-buffered saline (PBS), and immediately analyzed for fluorescence intensity by FACScan flow cytometer (Beckton Dickinson, Rutheford, NJ) using a 488-nm excitation beam and a 538-nm band-pass filter. Intracellular superoxide anion was similarly determined but using dihydroethidium (DHE) as a probe. The fluorescence intensity was analyzed on the FACScan flow cytometer using a 488-nm excitation beam and a 610-nm band-pass filter. Median fluorescence intensity was quantified by CellQuest software (Becton–Dickinson) analysis of the recorded histograms.
Western blot analysis
After specific treatments, cells were incubated with lysis buffer containing 2% Triton X-100, 1% sodium dodecyl sulfate (SDS), 100 mmol/l NaCl, 10 mmol/l Tris–HCl (pH 7.5), 1 mmol/l EDTA, and Complete Mini cocktail protease inhibitors (Roche Molecular Biochemicals) for 30 min on ice. After insoluble debris was pelleted by centrifuged at 14,000×g for 15 min at 4°C, the supernatant was collected and determined for protein content using Bradford method (Bio-Rad Laboratories, Hercules, CA). Proteins (40 μg) were resolved on 10% SDS–polyacrylamide gel electrophoresis (SDS–PAGE) and then transferred onto nitrocellulose membranes (Bio-Rad) using standard procedures. The membranes were blocked in 5% skim milk in TBST (25 mmol/l Tris–HCl, pH 7.4, 125 mmol/l NaCl, 0.1% Tween 20) for 1 h, followed by incubation with appropriate primary antibodies at 4°C overnight. Membranes were washed three times with TBST for 10 min, followed by incubation with horseradish peroxidase-conjugated secondary antibodies for 2 h at room temperature. The immune complexes were detected by chemiluminescence (Supersignal West Pico; Pierce, Rockford, IL) and quantified by imaging densitometry using analyst/PC densitometry software (Bio-Rad). Mean densitometry data from independent experiments were normalized with β-actin protein. The data were represented as the mean ± SD and analyzed by Student’s t test.
Immunoprecipitation
Cells were washed with ice-cold PBS and lysed in lysis buffer at 4°C for 20 min. After centrifugation at 14,000×g for 15 min, the supernatants were collected and determined for protein content using Bradford method (Bio-Rad Laboratories, Hercules, CA). Lysates were normalized and 60 μg proteins were incubated with anti-Bcl-2 antibodies for 14 h at 4°C, followed by incubation with protein A-conjugated Sepharose. Then immune complexes were washed with 20 volumes of lysis buffer, resuspended in 2× Laemmli sample buffer, and boiled at 95°C for 5 min. The immune complexes were resolved in 10% SDS–PAGE and analyzed by Western blotting as described.
Results
Curcumin sensitizes lung carcinoma H460 cells to detachment-induced cell death
To study the effect of curcumin on cell anoikis, we first determined detachment-induced cell death in H460 cells. Cells were detached and incubated in attachment-resistant poly-HEMA-coated plates for various times and analyzed for cell viability by XTT assay. Figure 1a shows that cell detachment induced a gradual decrease in cell viability. At 3 h post-detachment, approximately 70% of the cells were viable, and by 24 h only about 30% of the cells remained viable. Control experiments using attached cells in normal tissue culture plates show no significant change in cell viability during this time period (data not shown). To determine whether the observed reduction in cell viability was due to apoptotic cell death, we analyzed sub G0 fraction by flow cytometry, DNA condensation by Hoechst 33342 assay, and cell membrane integrity by PI exclusion assay. Flow cytometry data show that the sub G0 fraction was substantially increased after cell detachment (Fig. 1b), which is indicative of cell apoptosis. Likewise, Hoechst assay shows an increase in nuclear fluorescence and chromatin condensation of the detached cells over time (Fig. 1c). In contrast, no detectable changes in nuclear PI fluorescence, which is indicative of necrosis, were observed during the time period after cell detachment (Fig. 1c). These results indicate that apoptosis is the primary mode of cell death induced by detachment in H460 cells.
Anoikis response of non small cell lung carcinoma H460 cells. a H460 cells were cultured in poly-HEMA coated plates for various times after detachment. At the indicated time points, cell viability was determined by XTT assay. b Anoikis cells were determined from sub G0 fraction of cell cycle analysis. c Morphology of anoikis nuclei stained with Hoechst 33342 dye and propidium iodide. Values are means ± SD (n = 3). * p < 0.05 versus control at 0 h
To study the effect of curcumin on cell anoikis, attached and detached H460 cells were treated with various concentrations of curcumin (0.25–5 μmol/l) and analyzed for cell viability by XTT assay. Figure 2a shows that treatment of the cells with curcumin significantly decreased cell viability of the detached cells as compared to non-treated control. However, such treatment had minimal effect on the viability of attached cells. Cell cycle analysis of the detached cells shows a significant increase in sub G0 fraction in response to curcumin treatment (Fig. 2b). Hoechst assay also shows an increase in nuclear fluorescence and condensation, whereas PI exclusion assay shows no appreciable change in the fluorescence pattern (Fig. 2c). To further clarify the mechanism by which curcumin sensitizes detachment-induced apoptosis, the activity of caspase-3, a key executor in apoptotic cell death, was evaluated. Figure 2d shows that curcumin induced caspase-3 activation in a dose-dependent manner and that this activation is closely correlated with the cell death pattern observed in the nuclear condensation and sub G0 cell cycle assays. These results suggest that curcumin decreased viability of the detached cells by inducing apoptosis through a caspase-dependent mechanism.
Anoikis-sensitizing effect of curcumin. a Attached and detached H460 cells were treated with various concentrations of curcumin for 6 h, and cell viability was determined by XTT assay. b H460 cells were detached and then immediately treated with various concentrations of curcumin for 6 h. DNA fragmentation was measured as sub G0 fraction by flow cytometry using propidium iodide as a DNA labeling probe. c Morphology of anoikis nuclei in cells treated with curcumin. Treated cells were stained with Hoechst 33342 and propidium iodide, and examined under a fluorescence microscope. d Caspase-3 activation in response to curcumin treatment. After treatment with various concentrations of curcumin for 6 h, detached cells were incubated with carboxyfluorescein FAM-DEVD-FMK for 2 h. Caspase-3 activity was determined using a fluorescence microplate reader as described in the Materials and methods section. e Detached H460 cells were treated with 1 μmol/l of curcumin, cisplatin, or paclitaxel for 6 h, and cell viability was determined by XTT assay. Values are means ± SD (n = 3). * p < 0.05 versus non-treated control; # p < 0.05 versus curcumin-treated control
We also compared the anoikis-sensitizing effect of curcumin to established anticancer drugs for non-small cell lung cancer, paclitaxel and cisplatin [37, 38]. The results shown in Fig. 2e indicate that these drugs when treated at an equimolar concentration of 1 μmol/l were less effective in sensitizing H460 cells than curcumin, suggesting the high potency of curcumin in cancer cell anoikis.
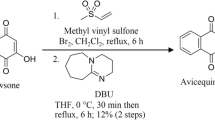
Bcl-2 and Cav-1 attenuate detachment-induced cell death in H460 cells
Bcl-2 and Cav-1 have been implicated in anoikis resistance of various cancer cell types [17, 26, 34–36]. To investigate whether Bcl-2 and Cav-1 could attenuate anoikis in H460 cells, the cells were stably transfected with Bcl-2 or Cav-1 plasmid and analyzed for the respective protein expression by Western blotting. Figure 3a shows that Bcl-2-transfected H460 cells (H460/Bcl-2) expressed a high level of Bcl-2 protein, and likewise Cav-1-transfected cells (H460/Cav-1) expressed an elevated level of Cav-1 protein, as compared to vector-transfected controls. To investigate the role of Bcl-2 and Cav-1 in anoikis resistance, H460/Bcl-2 and H460/Cav-1 cells were detached and analyzed for cell viability by XTT assay. Figure 3b shows that H460/Bcl-2 and H460/Cav-1 cells were more resistant to detachment-induced cell death as compared to control-transfected cells. In control cells, a significant decrease in cell viability was observed as early as 3 h after detachment, whereas in H460/Bcl-2 and H460/Cav-1 cells, a significant decrease in cell viability was not observed until 24 h. These results indicate that Bcl-2 and Cav-1 play a suppressive role in anoikis of H460 cells.
Bcl-2 and Cav-1 overexpression induces anoikis resistance in H460 cells. a H460 cells were transfected with Bcl-2, Cav-1, or control plasmid to generate H460/Bcl-2, H460/Cav-1, and H460/Con cells. Bcl-2 and Cav-1 protein expression was determined by Western blotting. b Anoikis response of the transfected cells was determined at the indicated times after cell detachment. Values are means ± SD (n = 3). * p < 0.05 versus indicated detachment time of control-transfected cells
Curcumin downregulates Bcl-2 but not Cav-1 expression during H460 cell anoikis
Having demonstrated the role of Bcl-2 and Cav-1 in anoikis regulation of H460 cells, we further investigated the effect of curcumin on Bcl-2 and Cav-1 expression in these cells. The cells were detached and incubated in attachment-resistant poly-HEMA-coated plates for various times (0–24 h) in the presence or absence of curcumin (1 μmol/l). Bcl-2 and Cav-1 protein expression was then determined by Western blotting. Figure 4a shows that curcumin significantly decreased Bcl-2 level which could be detected as early as 3 h after cell detachment, whereas curcumin had minimal effect on Cav-1 level. Endogenous levels of Bcl-2 and Cav-1 were relatively unchanged during detachment-induced apoptosis in the absence of curcumin (Fig. 4b). These results support the anoikis-sensitizing effect of curcumin through a Bcl-2-dependent pathway.
Effect of curcumin treatment on Bcl-2 and Cav-1 protein expression in H460 cells after detachment. a Cells were detached and then immediately incubated with 1 μmol/l of curcumin for various times in poly-HEMA coated plates. Bcl-2 and Cav-1 protein expressions were determined by Western blotting. Plots show relative values over controls at 0 h. b Cells were cultured in poly-HEMA coated plates for various times after detachment. At each time point, Bcl-2 and Cav-1 levels were determined by Western blotting. Blots were reprobed with β-actin antibody to confirm equal loading of the samples. c Detached H460 cells were treated with various concentrations of curcumin for 6 h, and Bcl-2, Mcl-1, and Bax protein expressions were determined by Western blotting. Blots were reprobed with β-actin antibody to confirm equal loading of samples. Values are means ± SD (n = 3). * p < 0.05 versus curcumin-treated control at 0 h
We also determined the effect of curcumin on Mcl-1 and Bax, two key apoptosis regulatory proteins in the Bcl-2 family. Figure 4c shows curcumin had no appreciable effect on the two proteins under the same treatment condition that induced substantial downregulation of Bcl-2. These results suggest Bcl-2 as a major target for curcumin-induced anoikis.
Curcumin sensitizes H460 cell anoikis through superoxide anion generation
Previous studies have demonstrated the prooxidant activity of curcumin in a wide variety of cells. Furthermore, we and others have shown that superoxide anion is a principal ROS generated in response to curcumin treatment [8, 39, 40]. To test whether curcumin-induced superoxide anion might play a role in anoikis sensitization of H460 cells, we examined the effect of curcumin treatment on superoxide anion generation in these cells. Flow cytometric analysis of ROS generation using H2DCF-DA as a general oxidative probe shows that curcumin was able to induce ROS generation in a dose-dependent manner (Fig. 5a). To determine specific ROS induced by curcumin, cells were treated with the test agent in the presence or absence of various known specific inhibitors of ROS, including MnTBAP (a superoxide dismutase mimetic and superoxide anion scavenger), catalase (hydrogen peroxide scavenger), deferoxamine (inhibitor of Fenton-mediated hydroxyl radical), and analyzed for ROS generation as described. The results show that MnTBAP was able to inhibit curcumin-induced ROS generation, whereas other antioxidants had no significant effect (Fig. 5c), suggesting that superoxide anion is a major ROS induced by curcumin in the treated cells. The induction of superoxide anion by curcumin was also confirmed by flow cytometric analysis using dihydroethidium (DHE) as a specific fluorescent probe for superoxide anion (Fig. 5b).
Effect of ROS scavengers on curcumin-induced ROS generation. After detachment, H460 cells were immediately treated with various concentrations of curcumin for 1 h. Intracellular ROS and superoxide anion levels were then measured by flow cytometry using a H2DCF-DA and b DHE as fluorescent probes, respectively. Values are means ± SD (n = 4). * p < 0.05 versus non-treated control. c After detachment, cells were pretreated with 100 μmol/l of MnTBAP, 1,000 units/ml of catalase (Cat), or 20 mmol/l of deferoxamine (Def) for 30 min and then treated with 1 μmol/l of curcumin for 1 h. Intracellular ROS level was then determined by flow cytometry using H2DCF-DA as a probe. Values are means ± SD (n = 4). # p < 0.05 versus curcumin-treated control. d Effect of curcumin on cell viability in the presence or absence of ROS scavengers described above after 6 h. Values are means ± SD (n = 4). # p < 0.05 versus curcumin-treated control
To determine whether curcumin-induced superoxide anion generation is responsible for the anoikis-sensitizing effect of curcumin, cells were treated with curcumin in the presence or absence of MnTBAP pretreatment, and analyzed for cell viability after detachment. Parallel studies were also performed using other antioxidants to test the role of other ROS in curcumin sensitization of cell anoikis. The results show that MnTBAP was able to inhibit curcumin-induced cell death, whereas other antioxidants were ineffective (Fig. 5d), supporting the role of superoxide anion in curcumin sensitization of cell anoikis.
Curcumin induces Bcl-2 downregulation through superoxide anion-mediated ubiquitination
Since cell anoikis was earlier shown to be dependent on Bcl-2 expression and was promoted by curcumin treatment, we tested whether such treatment could attenuate Bcl-2 through superoxide anion. Cells were treated with curcumin in the presence or absence of ROS modulators and analyzed for Bcl-2 protein level by Western blotting. The results show that curcumin treatment induced Bcl-2 downregulation, the effect that can be completely inhibited by pretreatment of the cells with MnTBAP but not other antioxidants, catalase and deferoxamine (Fig. 6a). Control experiments using ROS modulators alone in the absence of curcumin show no significant effect on Bcl-2 expression under the same condition (data not shown). These results indicate that superoxide anion is a key mediator of curcumin-induced Bcl-2 downregulation, which could be a key mechanism of anoikis sensitization by curcumin.
Curcumin downregulates Bcl-2 via superoxide-dependent ubiquitination. a After detachment, H460 cells were pretreated with 100 μmol/l of MnTBAP, 1,000 units/ml of catalase (Cat), or 20 mmol/l of deferoxamine (Def) for 30 min and then treated with 1 μmol/l of curcumin for 6 h. Bcl-2 levels were determined by Western blotting and normalized to β-actin. Plots represent relative values over non-treated control at 6 h. Values are means ± SD (n = 4). * p < 0.05 versus non-treated control; # p < 0.05 versus curcumin-treated control. b After detachment, H460 cells were treated with the indicated concentrations of curcumin for 6 h in the presence or absence of 100 μmol/l of MnTBAP. Cell lysates were prepared and immunoprecipitated with anti-Bcl-2 antibody. The immune complex was then analyzed for Bcl-2 ubiquitination by Western blotting using anti-ubiquitin antibody. Values are means ± SD (n = 3). * p < 0.05 versus non-treated control; # p < 0.05 versus curcumin (1 μmol/l)-treated control
Bcl-2 has been shown to be downregulated under diverse apoptosis conditions through a non-transcriptional proteasomal degradation-dependent mechanism [8, 27, 41]. This process involves ubiquitination of the protein and its subsequent degradation by the proteasome. We therefore tested whether curcumin could induce Bcl-2 ubiquitination and whether or not this process is mediated by superoxide anion. Cells were detached and treated with curcumin in the presence or absence of MnTBAP as earlier described. Cell lysates were prepared, immunoprecipitated with anti-Bcl-2 antibody, and the resulting immune complexes were analyzed for ubiquitin by Western blotting. The results show that curcumin induced Bcl-2 ubiquitination in a dose-dependent manner and that this effect was inhibited by MnTBAP (Fig. 6b). These results support the role of superoxide anion as a key mediator of curcumin-induced Bcl-2 ubiquitination and its subsequent degradation during cell anoikis.
Curcumin sensitizes Bcl-2-overexpressing cells to anoikis
Bcl-2 overexpression was earlier shown to protect cells from anoikis (Fig. 3). Since curcumin is hypothesized to exert its anoikis-sensitizing effect through Bcl-2 down-regulation, we tested whether curcumin could reverse the protective effect of Bcl-2 and whether or not such reversal is associated with the downregulation of Bcl-2 by curcumin. To do this, we treated Bcl-2 overexpressing (H460/Bcl-2) cells with various concentrations of curcumin and analyzed for cell viability and Bcl-2 expression by XTT and Western blot assays. Cell viability assay shows that curcumin decreased the survival of detached H460/Bcl-2 cells in a dose-dependent manner (Fig. 7a). Western blot analysis of Bcl-2 expression also shows a parallel downregulation of the protein by the curcumin treatment (Fig. 7b). These results support the role of Bcl-2 downregulation as a key mechanism of anoikis sensitization by curcumin.
Curcumin downregulates Bcl-2 in H460/Bcl-2 cells and sensitizes them to anoikis. Bcl-2-overexpressing H460/Bcl-2 cells were detached and immediately treated with various concentrations of curcumin for 6 h. The cells were then determined for a cell viability by XTT assay, and b Bcl-2 expression by Western blotting. Values are means ± SD (n = 3). * p < 0.05 versus non-treated control
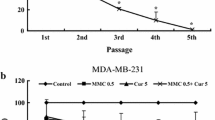
Curcumin also sensitizes other cells to anoikis through superoxide and Bcl-2 dependent mechanisms
To test the generality of the effect of curcumin on cell anoikis, we examined the effect of curcumin treatment on anoikis in two other cell systems, namely melanoma G361 cells and lung epithelial BEAS-2B cells. We also tested whether this effect is mediated by superoxide anion and Bcl-2. Cells were detached and incubated with curcumin in the presence or absence of superoxide anion scavenger MnTBAP. Cell viability and Bcl-2 expression were then determined. The results show that curcumin promoted detachment-induced cell death of both G361 and BEAS-2B cells in a dose-dependent manner, and that MnTBAP was able to inhibit this enhancement (Figs. 8a and b). Bcl-2 expression in the two cell systems was similarly downregulated by the curcumin treatment, the effect that could be inhibited MnTBAP (Fig. 8c and d). These results support the general role of superoxide anion in curcumin-induced Bcl-2 downregulation and anoikis sensitization in the test cell systems.
Effects of curcumin and MnTBAP on Bcl-2 expression and anoikis response in other cell systems. Melanoma G361 cells and bronchial epithelial BEAS-2B cells were detached and immediately incubated with various concentrations of curcumin in the presence or absence of 100 μmol/l of MnTBAP. a and b Viability of G361 and BEAS-2B cells determined by XTT assay. c and d Bcl-2 expression of G361 and BEAS-2B cells determined by Western blotting. Blots were reprobed with β-actin antibody to confirm equal loading of samples. Values are means ± SD (n = 3). * p < 0.05 versus non-treated control; # p < 0.05 versus curcumin-treated control
Discussion
Resistance to anoikis has been established as one of the key mechanisms of tumor cell metastasis. In this study, we demonstrated for the first time that curcumin can sensitize lung cancer H460 cells to anoikis. The mechanism underlying this anoikis sensitization was shown to involve intracellular superoxide anion generation and Bcl-2 downregulation. Curcumin has previously been shown to induce apoptosis and inhibit metastasis of various cancer cells including lung cancer cells both in vitro and in vivo [5, 8, 42], and has been proposed for use as a chemoadjuvant or direct treatment of cancers. The sensitizing effect of curcumin on cancer cell apoptosis has been reported for a variety of chemotherapeutic agents [43–45]. Several mechanisms of apoptosis potentiation by curcumin have also been proposed [43–47], including inactivation of NF-κB, modulation of Akt and p38, and upregulation of death receptor 5, depending on the chemotherapeutic agents. The results of this study further suggest that in addition to its apoptosis-sensitizing effect, curcumin also exhibits an anoikis-sensitizing effect that could potentially be exploited for the treatment of metastatic cancers.
There are several possible mechanisms that may be responsible for the anoikis-sensitizing effect of curcumin. We focused our efforts on two proteins that are known to be important in anoikis resistance of tumor cells, Bcl-2 [17, 18] and Cav-1 [34–36]. We found that overexpression of either of these proteins by stable gene transfection resulted in an increase in anoikis resistance of lung cancer H460 cells, as evidenced by their increased survival after cell detachment compared to control-transfected cells (Fig. 3). In osteosarcoma cells, Lin et al. recently reported an upregulation of Bcl-2 and increased resistance to anoikis [26], supporting our finding and the positive regulatory role of Bcl-2 in anoikis resistance. The role of Cav-1 in anoikis resistance and metastasis has been reported but remains controversial. While some studies indicated that Cav-1 inhibited cancer cell anoikis and promoted metastasis [34–36], others showed that it inhibited cancer cell growth and metastasis [48–50]. It is likely that different cell types and metastatic stages of cancer cells used in these studies contribute to the observed discrepancies, and further studies are needed to clarify the role of this protein in anoikis and metastasis. Our results in human lung cancer H460 cells support the inhibitory role of Cav-1 in anoikis, consistent with a previous report in human breast cancer MCF and HT-29-MDR cells [36].
The present study also demonstrated that curcumin treatment of H460 cells resulted in a downregulation of Bcl-2 protein without significantly affecting some other proteins such as Cav-1, Mcl-1, and Bax (Fig. 4). These results suggest that curcumin may exert its anoikis-sensitizing effect primarily through Bcl-2 downregulation. Bcl-2 is a redox-sensitive anti-apoptotic protein. Since curcumin is a known pro-oxidant capable of inducing ROS generation in various cell types including cancer cells [39, 51, 52], we tested whether curcumin-induced ROS generation could be responsible for the downregulation of Bcl-2 and the sensitization of cells to anoikis. As expected, we found that ROS, particularly superoxide anion, indeed plays a role in both Bcl-2 downregulation and anoikis sensitization induced by curcumin (Figs. 5 and 6). These results also suggest the linkage between these two events.
We and others have previously reported that Bcl-2 is rapidly degraded through the ubiquitin–proteasome pathway in response to various apoptotic stimuli [8, 28, 29, 41, 53]. However, whether or not this mechanism is operative in anoikis cells treated with curcumin is not known. We found that curcumin induced ubiquitination of Bcl-2 in a dose-dependent manner and that this induction was inhibited by superoxide anion inhibitor, MnTBAP (Fig. 6). These results indicate the requirement of superoxide anion in curcumin-induced Bcl-2 ubiquitination and provide a mechanistic insight into the mechanism of Bcl-2 downregulation and anoikis sensitization by curcumin.
Finally, we provided evidence supporting the role of Bcl-2 and the potential utility of curcumin to overcome anoikis resistance in other cell systems. We found that curcumin can downregulate Bcl-2 and sensitize cells to anoikis in melanoma G361 cells and bronchial BEAS-2B cells (Fig. 8). These effects of curcumin can be inhibited by superoxide anion scavenging, supporting the above findings in H460 cells.
In conclusion, we reported a novel finding on the anoikis-sensitizing effect of curcumin and its regulatory mechanisms. The effect of curcumin on anoikis is mediated, at least in part, through superoxide anion-mediated Bcl-2 downregulation via the ubiquitin pathway. Since increased stability and expression of Bcl-2 has been associated with anoikis resistance in many cancer cell types and since such resistance has been attributed to cancer metastasis, the results of this study could be beneficial to the design of more effective strategies aimed at overcoming anoikis resistance and cancer metastasis.
Abbreviations
- XTT:
-
2,3-Bis(2-methoxy-4-nitro-5-sulfophenyl)-2H-tetrazolium-5 carboxanilide inner salt
- DHE:
-
Dihydroethidium
- H2DCF-DA:
-
Dihydrodichlorofluorescein diacetate
- MnTBAP:
-
Mn(III)tetrakis(4-benzoic acid) porphyrin chloride
- Def:
-
Deferoxamine
- Cat:
-
Catalase
- polyHEMA:
-
Poly(2-hydroxy ethylmethacrylate)
- Cav-1:
-
Caveolin-1
References
Han SS, Chung ST, Robertson DA, Ranjan D, Bondada S (1999) Curcumin causes the growth arrest and apoptosis of B cell lymphoma by downregulation of egr-1, c-myc, bcl-XL, NF-kappa B, and p53. Clin Immunol 93:152–161. doi:10.1006/clim.1999.4769
Simon A, Allais DP, Duroux JL, Basly JP, Durand-Fontanier S, Delage C (1998) Inhibitory effect of curcuminoids on MCF-7 cell proliferation and structure-activity relationships. Cancer Lett 129:111–116. doi:10.1016/S0304-3835(98)00092-5
Bush JA, Cheung KJJ, Li G (2001) Curcumin induces apoptosis in human melanoma cells through a Fas receptor/caspase-8 pathway independent of p53. Exp Cell Res 271:305–314. doi:10.1006/excr.2001.5381
Bachmeier B, Nerlich AG, Iancu CM, Cilli M, Schleicher E, Vené R, Dell’Eva R, Jochum M, Albini A, Pfeffer U (2007) The chemopreventive polyphenol curcumin prevents hematogenous breast cancer metastases in immunodeficient mice. Cell Physiol Biochem 19:137–152
Chen HW, Lee JY, Huang JY, Wang CC, Chen WJ, Su SF, Huang CW, Ho CC, Chen JJ, Tsai MF, Yu SL, Yang PC (2008) Curcumin inhibits lung cancer cell invasion and metastasis through the tumor suppressor HLJ1. Cancer Res 68:7428–7438. doi:10.1158/0008-5472.CAN-07-6734
Yoshino M, Haneda M, Naruse M, Htay HH, Tsubouchi R, Qiao SL, Li WH, Murakami K, Yokochi T (2004) Prooxidant activity of curcumin: copper-dependent formation of 8-hydroxy-2′-deoxyguanosine in DNA and induction of apoptotic cell death. Toxicol In Vitro 18:783–789. doi:10.1016/j.tiv.2004.03.009
Cao J, Jia L, Zhou HM, Liu Y, Zhong LF (2006) Mitochondrial and nuclear DNA damage induced by curcumin in human hepatoma G2 cells. Toxicol Sci 91:476–483. doi:10.1093/toxsci/kfj153
Chanvorachote P, Pongrakhananon V, Wannachaiyasit S, Luanpitpong S, Rojanasakul Y, Nimmanit U (2009) Curcumin sensitizes lung cancer cells to cisplatin-induced apoptosis through superoxide anion-mediated Bcl-2 degradation. Cancer Invest 26:624–635. doi:10.1080/07357900802653472
Grossmann J (2002) Molecular mechanisms of “detachment-induced apoptosis-anoikis”. Apoptosis 7:247–260. doi:10.1023/A:1015312119693
Mehlen P, Puisieux A (2006) Metastasis: a question of life or death. Nat Rev Cancer 6:449–458. doi:10.1038/nrc1886
Hanahan D, Weiberg RA (2000) The hallmarks of cancer. Cell 100:57–70. doi:10.1016/S0092-8674(00)81683-9
Frisch SM, Screaton RA (2001) Anoikis Mechanisms. Curr Opin Cell Biol 13:555–562. doi:10.1016/S0955-0674(00)00251-9
Chen Y, Kuo C, Tsai Y, Yu C, Wang G, Liao H (2008) Norcantharidin induces anoikis through Jun-N-terminal kinase activation in CT26 colorectal cancer cells. Anticancer Drugs 19:55–64. doi:10.1097/CAD.0b013e3282f18826
Dufour G, Demers MJ, Gagne D, Dydensborg AB, Teller IC, Bouchard V, Degongre I, Beaulieu JF, Cheng JQ, Fujita N, Tsuruo T, Vallee K, Vachon PH (2004) Human intestinal epithelial cell survival and anoikis: differentiation state distinct regulation and roles of protein kinase B/Akt isoforms. J Biol Chem 279:44113–44122. doi:10.1074/jbc.M405323200
Almeida EA, Ilic D, Han Q, Hauck CR, Jin F, Kawakatsu H, Schlaepfer DD, Damsky CH (2000) Matrix survival signaling: from fibronectin via focal adhesion kinase to c-Jun NH(2)-terminal kinase. J Cell Biol 149:741–754
Collins NL, Reginato MJ, Paulus JK, Sgroi DC, Joshua L, Brugge JS (2005) G1/S cell cycle arrest provides anoikis resistance through Erk-mediated Bim suppression. Mol Cell Biol 25:5282–5291. doi:10.1128/MCB.25.12.5282-5291.2005
Galante JM, Mortenson MM, Bowles TL, Virudachalam S, Bold RJ (2009) Erk/Bcl-2 pathway in the resistance of pancreatic cancer to anoikis. J Surg Res 152:18–25. doi:10.1016/j.jss.2008.05.017
Martin SS, Vuori K (2004) Regulation of Bcl-2 proteins during anoikis and amorphosis. Biochim Biophys Acta 1692:145–157. doi:10.1016/j.bbamcr.2004.02.008
Reginato MJ, Mills KR, Paulus JK, Lynch DK, Sgroi DC, Debnath J, Muthuswamy SK, Brugg JS (2003) Intergrins and EGFR coordinately regulate the pro-apoptotic protein Bim to prevent anoikis. Nat Cell Biol 35:733–740. doi:10.1038/ncb1026
Schmelzle T, Mailluex AA, Overholtzer M, Carroll JS, Solimini NL, Lightcap ES, Veiby OP, Brugge JS (2006) Functional role and oncogene-regulated expression of the BH3-only factor Bmf in mammary epithelial anoikis and morphogenesis. Proc Natl Acad Sci USA 104:3787–3792. doi:10.1073/pnas.0700115104
Valentijn AJ, Metcalfe AD, Kott J, Streuli CH, Gilmore AP (2003) Spatial and temporal change in Bax subcellular localization during anoikis. J Cell Biol 162:599–612. doi:10.1083/jcb.200302154
Valentijn AJ, Gilmore AP (2004) Translocation of full-length Bid to mitochondria during anoikis. J Biol Chem 279:32848–32857. doi:10.1074/jbc.M313375200
Frankel A, Rosen K, Filmus J, Kerbel RS (2001) Induction of anoikis and suppression of human ovarian tumor growth in vivo by down-regalation of Bcl-XL. Cancer Res 61:4837–4841
Scorrano L, Korsmeyer SJ (2003) Mechanisms of cytochrome c release by proapoptotic BCL-2 family members. Biochem Biophys Res Commun 304:437–444
Grossmann J, Walther K, Artinger M, Kiessling S, Scholmerich J (2001) Apoptotic signaling during initiation of detachment-induced apoptosis (‘Anoikis’) of primary human intestinal epithelial cells. Cell Growth Diff 12:147–155
Lin D, Feng J, Chen W (2008) Bcl-2 and caspase-8 related anoikis resistance in human osteosarcoma MG-63 cells. Cell Biol Int 32:1199–1206. doi:10.1016/j.cellbi.2008.07.002
Dimmeler S, Breitschopf K, Haendeler J, Zeiher AM (1999) Dephosphorylation targets Bcl-2 for ubiquitin-dependent degradation: a link between the apoptosome and the proteasome pathway. J Exp Med 189:1815–1822
Chanvorachote P, Nimmanit U, Stehlik C, Wang L, Jiang B, Ongpipatanakul B, Rojanasakul Y (2006) Nitric oxide regulates cell sensitivity to cisplatin-induced apoptosis through S-nitrosylation and inhibition of Bcl-2 ubiquitination. Cancer Res 66:6353–6360. doi:10.1158/0008-5472.CAN-05-4533
Haendeler J, Messmer UK, Brune B, Neugebauer E, Dimmeler S (1996) Endotoxic shock leads to apoptosis in vivo and reduces Bcl-2. Shock 6:405–409
Paradis E, Doulliard H, Koutroumanis M, Goodyer C, Leblanc A (1996) Amyloid beta peptide of alzheimer’s disease downregulates Bcl-2 and upregulates Bax expression in human neurons. J Neurosci 16:7533–7539
Yanamadala V, Negoro H, Gunaratnam L, Kong T, Denker BM (2007) Galpha12 stimulates apoptosis in epithelial cells through JNK1-mediated Bcl-2 degradation and up-regulation of IkappaBalpha. J Biol Chem 282:24352–24363. doi:10.1074/jbc.M702804200
Williams TM, Lisanti MP (2005) Caveolin-1 in oncogenic transformation, cancer, and metastasis. Am J Physiol Cell Physiol 288:C494–C506. doi:10.1152/ajpcell.00458.2004
Yang G, Truong LD, Timme TL, Ren C, Wheeler TM, Park SH, Nasu Y, Bangma CH, Kattan MW, Scardino PT, Thompson TC (1998) Elevated expression of caveolin is associated with prostate and breast cancer. Clin Cancer Res 4:1873–1880
Ravid D, Maor S, Werner H, Liscovitch M (2006) Caveolin-1 inhibits anoikis and promotes survival signaling in cancer cells. Adv Enzyme Regul 46:163–175. doi:10.1016/j.advenzreg.2006.01.022
Fiucci G, Ravid D, Reich R, Liscovitch M (2002) Caveolin-1 inhibits anchorage-independent growth, anoikis and invasiveness in MCF-7 human breast cancer cells. Oncogene 21:2365–2375. doi:10.1038/sj/onc/1205300
Ravid D, Maor S, Werner H, Liscovitch M (2005) Caveolin-1 inhibits cell detachment-induced p53 activation and anoikis by upregulation of insulin-like growth factor-I receptors and signaling. Oncogene 24:1338–1347. doi:10.1038/sj.onc.1208337
Sandler AB, Nemunaitis J, Denham C, vonPawel J, Cormier Y, Gatzemeier U, Mattson K, Ch Manegold, Palmer MC, Gregor A, Nguyen B, Niyikiza C, Einhorn LH (2000) Phase III trial of gemcitabine plus cisplatin versus cisplatin alone in patients with locally advanced or metastatic non-small-cell lung cancer. J Clin Oncol 18:122–130
Gan PP, Pasquier E, Kavallaris M (2007) Class III B-tubulin mediates sensitivity to chemotherapeutic drugs in non-small cell lung cancer. Cancer Res 67:9356–9363. doi:10.1158/0008-5472.CAN-07-0509
Bhaumik S, Anjum R, Rangaraj N, Pardhasaradhi BVV, Khar A (1999) Curcumin mediated apoptosis in AK-5 tumor cells involves the production of reactive oxygen intermediates. FEBS Lett 456:311–314. doi:10.1016/S0014-5793(99)00969-2
Syng-ai C, Kumari A, Khar A (2004) Effect of curcumin on normal and tumor cells: role of glutathione and bcl-2. Mol Cancer Ther 3:1101–1108
Breitshopf K, Haendeler J, Malchow P, Zeiher AM, Dimmeler S (2000) Posttranslational modification of bcl-2 facilitates its proteasome-dependent degradation: molecular characterization of the involved signaling pathway. Mol Cell Biol 20:1886–1896
Pillai GR, Srivastava AS, Hassanein TI, Chauhan DP, Carrier E (2004) Induction of apoptosis in human lung cancer cells by curcumin. Cancer Lett 208:163–170. doi:10.1016/j.canlet.2004.01.008
Notarbartolo M, Poma P, Perri D, Dusonchet L, Cervello M, D’Alessandro N (2005) Antitumor effects of curcumin, alone or in combination with cisplatin or doxorubicin, on human hepatic cancer cells. Analysis of their possible relationship to changes in NF-kB activation levels and in IAP gene expression. Cancer Lett 244:53–65
Weir NM, Selvendiran K, Kutala VK, Tong L, Vishwanath S, Rajaram M, Tridandapani S, Anant S, Kuppusamy P (2007) Curcumin induced G2/M arrest and apoptosis in cisplatin-resistant human ovarian cancer cells by modulating Akt and p38 MAPK. Cancer Biol Ther 6:178–184
Du B, Jiang L, Xia Q, Zhong L (2006) Synergistic inhibitory effect of curcumin and 5-fluorouracil on the growth of the human colon cancer cell line HT-29. Chemotherapy 52:23–28. doi:10.1159/000090238
Deeb D, Jiang H, Gao X, Hafner MS, Wong H, Divine G, Chapman RA, Dulchavsky SA, Gautam SC (2004) Curcumin sensitizes prostate cancer cells to tumor necrosis factor-related apoptosis-inducing ligand/Apo2L by inhibiting nuclear factor-kappaB through suppression of IkappaB alpha phosphorelation. Mol Cancer Ther 3:803–812
Jung EM, Lim JH, Lee TJ, Park JW, Choi KS, Kwon TK (2005) Curcumin sensitizes tumor necrosis factor-related apoptosis-inducing ligand (TRAIL)-induced apoptosis through reactive oxygen species-mediated upregulation of death receptor 5 (DR5). Carcinogenesis 26:1905–1913. doi:10.1093/carcin/bgi167
Sloan EK, Stanley KL, Anderson RL (2004) Caveolin-1 inhibits breast cancer growth and metastasis. Oncogene 23:7893–7897. doi:10.1038/sj.onc.1208062
Cantiani L, Manara MC, Zucchini C, Sanctis PD, Zuntini M, Valvassori L, Serra M, Olivero M, Renzo MFD, Colombo MP, Picci P, Scotlandi K (2007) Caveolin-1 reduces osteosarcoma metastases by inhibiting c-Src activity and Met signaling. Cancer Res 67:7674–7685. doi:10.1158/0008-5472.CAN-06-4697
Gu D, Li H, Wang Z, Chen Q, Jiang J, Zhu H (2009) Caveolin-1 inhibits the growth of human laryngeal squamous cell carcinoma and down regulates EGFR-MAPKs signaling pathway. Laryngoscope 117:1782–1789. doi:10.1097/MLG.0b013e31811edd31
Thayyullathil F, Chathoth S, Hago A, Patel M, Galadari S (2008) Rapid reactive oxygen species (ROS) generation induced by curcumin leads to caspase-dependent and -independent apoptosis in L929 cells. Free Radic Biol Med 45:1403–1412. doi:10.1016/j.freeradbiomed.2008.08.014
Khar A, Ali AM, Pardhasaradhi BVV, Varalakshmi C, Anjum R, Kumari AL (2001) Induction of stress response renders human tumor cell lines resistant to curcumin-mediated apoptosis: role of reactive oxygen intermediates. Cell Stress Chaperones 6:368–376
Wang L, Chanvorachote P, Toledo D, Stehlik C, Mercer RR, Castranova V, Rojanasakul Y (2008) Peroxide is a key mediator of Bcl-2 down-regulation and apoptosis induction by cisplatin in human lung cancer cells. Mol Pharmacol 73:119–127. doi:10.1124/mol.107.040873
Acknowledgments
This work was supported by the Thailand Research Fund (MG5080134; Pithi Chanvorachote and RGJ 5.Q.CU/50/A.1).
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Pongrakhananon, V., Nimmannit, U., Luanpitpong, S. et al. Curcumin sensitizes non-small cell lung cancer cell anoikis through reactive oxygen species-mediated Bcl-2 downregulation. Apoptosis 15, 574–585 (2010). https://doi.org/10.1007/s10495-010-0461-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10495-010-0461-4