Abstract
The molecular determinants which dictate survival and apoptosis/anoikis in human intestinal crypt cells remain to be fully understood. To this effect, the roles of β1 integrin/Fak/Src signaling to the PI3-K/Akt-1, MEK/Erk, and p38 pathways, were investigated. The regulation of six Bcl-2 homologs (Bcl-2, Mcl-1, Bcl-XL, Bax, Bak, Bad) was likewise analyzed. We report that: (1) Anoikis causes a down-activation of Fak, Src, Akt-1 and Erk1/2, a loss of Fak–Src association, and a sustained/enhanced activation of p38β, which is required as apoptosis/anoikis driver; (2) PI3-K/Akt-1 up-regulates the expression of Bcl-XL and Mcl-1, down-regulates Bax and Bak, drives Bad phosphorylation (both serine112/136 residues) and antagonizes p38β activation; (3) MEK/Erk up-regulates Bcl-2, drives Bad phosphorylation (serine112 residue), but does not antagonize p38β activation; (4) PI3-K/Akt-1 is required for survival, whereas MEK/Erk is not; (5) Src acts as a cornerstone in the engagement of both pathways by β1 integrins/Fak, and is crucial for survival; and (6) β1 integrins/Fak and/or Src regulate Bcl-2 homologs as both PI3-K/Atk-1 and MEK/Erk combined. Hence, β1 integrin/Fak/Src signaling translates into integrated mediating functions of p38β activation and regulation of Bcl-2 homologs by PI3-K/Akt-1 and MEK/Erk, consequently determining their requirement (or not) for survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Programmed cell death (or apoptosis) is a highly regulated process which performs critical roles in development, tissue homeostasis and repair, as well as in the pathogenesis of numerous diseases [1–3]. The Bcl-2 family of proteins constitutes a critical decisional checkpoint in cell survival and death [2, 3]. At least 20 family members have been identified so far in mammalian cells, functioning either as anti-apoptotics/suppressors (e.g. Bcl-2, Mcl-1, Bcl-X L ), pro-apoptotics/activators (e.g. Bax, Bak) or pro-apoptotics/sensitizers (e.g. Bad). Bcl-2 homologs are well known to interact among themselves, allowing for the titration of pro- and anti-apoptotic functions [2, 3]. The suppression or induction of apoptosis in different cell types does not necessarily depend on the activity of single Bcl-2 homologs, but usually on a balance of anti- and pro-apoptotic activities from multiple homologs. Such a balance of anti- and pro-apoptotic functions can be altered by modulation of expression and/or by post-translational modifications (e.g. phosphorylation) [1–3].
Consequently, incoming extracellular signals determine in large part if a cell lives or dies through signaling events that affect the expression and/or functions of multiple anti- and pro-apoptotic Bcl-2 homologs [2–8]. Such signals are provided by various cues, including cell adhesion. To this effect, the disruption, or loss, of integrin-mediated cell adhesion induces apoptosis by a process that is termed anoikis [4–8]. In epithelial cells, those integrins belonging to the β1 subfamily are not only largely responsible for the establishment of a physical link between the extracellular matrix (ECM) and the cytoskeleton, but as well for the cell adhesion-mediated activation of signaling pathways [5–10]. Hence, signaling originating from β1 integrins to promote cell survival often implicate Fak (p125Fak), Src (p60Src), the MEK-1, -2/Erk-1, -2 (p42Erk2/p44Erk1 MAPK) pathway and/or the PI3-K/Akt (p57Akt) pathway, depending on the tissue and cellular context [5–17]. It is well established that integrin/Fak/Src signaling can stimulate the PI3-K/Akt and MEK/Erk pathways, either individually or in combination, depending on the cell type analyzed [5–9, 14–17]. In this respect, MEK/Erk and PI3-K/Akt are known for their implication in the regulation of the expression of Bcl-2 homologs, as well as the inhibitory phosphorylation of Bad on its serine112 and/or serine136 residues [3, 6–8, 11–14, 18]. Conversely, signaling pathways can also be responsible for driving apoptosis/anoikis [4, 6, 8, 13, 18, 19]. Stress-activated MAPKs (SAPKs), such as those of the p38SAPK pathway, have been identified to this effect [8, 13, 18, 19]––however, their implication in apoptosis/anoikis has been shown to depend on the specific p38 isoform involved, as well as depending on the cell type studied [8, 13, 18, 19].
Much remains to be known of the molecular determinants which dictate life and death for intestinal epithelial cells (IECs), including their roles in the development of disorders associated with the gut. The continuous renewal of the human intestinal epithelium consists essentially in the production of enterocytes in the crypts, which differentiate and then migrate toward the apex of villi in order to enter anoikis [20–22]. In addition, crypt cells may enter “spontaneous” apoptosis, a less frequent process which serves to remove defective or injured progeny cells [20–23]. With respect to such “duality of fate” between crypt and villus cells, it is now well established that human enterocytic cell survival and death are subjected to differentiation state-specific control mechanisms [8, 20, 21, 24–29]. However, the specific signaling events in the regulation of survival and apoptosis/anoikis in normal human intestinal epithelial crypt (HIEC) cells remain poorly understood. Such comprehension is of direct relevance to the physiopathology of the gut, especially when considering that crypt alterations and epithelial apoptosis are commonly observed in inflammatory bowel disease, and that the persistence of aberrant crypt cells can lead to cancer [20–23]. To this effect, the question remains as to how cell adhesion-mediated signaling regulates Bcl-2 homologs within the specific context of HIEC cell survival and death.
In the present study, we investigated the roles of β1 integrin/Fak/Src survival signaling to the PI3-K/Akt-1, MEK/Erk and p38 pathways in HIEC cells, especially with regards to their roles in modulating the expression/activity of Bcl-2 homologs. Herein, we report that β1 integrins/Fak/Src signaling translates into integrated, complex regulatory functions by PI3-K/Akt-1 and MEK/Erk in the expression/activity of Bcl-2 homologs, as well as in the specific activation of the pro-apoptotic p38β SAPK isoform, therefore determining their own requirement (or not) in the suppression of HIEC apoptosis/anoikis.
Materials and methods
Materials
Specific antibodies directed against p125Fak, the phosphotyrosine397 activated form of p125Fak (pY397p125Fak), the Src-phosphorylated tyrosine 576 and 577 residues of p125Fak (pY576/577p125Fak), p57Akt-1, the phosphoserine473 activated form of p57Akt-1 (pS473p57Akt-1), p42Erk2/p44Erk1, the doubly phosphorylated (phosphothreonine202 and phosphotyrosine204) and activated forms of p42Erk2/p44Erk1 (p(T202,Y204)p42Erk2/p44Erk1), p60Src, the phosphotyrosine418 activated form of p60Src (pY418p60Src), p38SAPK, the doubly phosphorylated (phosphothreonine180 and phosphotyrosine182) and activated forms of p38SAPK (p(T180,Y192)p38), p38α, the p85 (α/β) regulatory subunit of PI3-K, Bcl-2, Bcl-XL, Mcl-1, Bax, Bak, Bad, the phosphoserine112 form of Bad (pS112Bad), the phosphoserine136 form of Bad (pS136Bad), and cytokeratin 18 (K18), were used as described previously [24–31] and were purchased from Calbiochem (San Diego, CA), Cell Signaling Technology (Beverly, MA), New England Biolabs (Mississauga, ON), Santa Cruz Biotechnology (Santa Cruz, CA), Sigma (Oakville, ON, Canada), Transductions Laboratories (Lexington, KY), and/or Upstate Biotechnology (Lake Placid, NY). Antibodies raised against p38β [29] were a kind gift of J. Landry (Centre de Recherche en Cancérologie de l’Université Laval, C.H.U.L., QC, Canada).
Cell culture
HIEC (Human Intestinal Epithelial Crypt) cells have been characterized elsewhere [32] and were cultured as already described [25, 28, 29]. Cells were maintained 0–24 h in medium without serum (controls) or with (1) 1 μM cytochalasin D (CD; Sigma), which has been shown to inhibit Fak at this concentration range without affecting actin filament polymerization [33]; (2) 100 μg/ml of the monoclonal antibody P4C10 (a kind gift of E. Ruoslahti, The Burnham Institute, LaJolla, CA), which inhibits the binding activity of the β1 integrin subunit [25–30]; (3) 100 μg/ml non-immune mouse IgG’s (Sigma), as control for experiments using the P4C10 antibody; (4) 30 μM Ly294002 (Calbiochem), for the inhibition of PI3-K; (5) 20 μM PD98059 (Calbiochem), for the inhibition of MEK-1/-2; (6) 20 μM PP2 (Calbiochem) or 10 μM herbimycin A (HA; Calbiochem), for the inhibition of Src; and/or (7) with 20 μM SB203580 or SB202190 (Calbiochem), for the inhibition of p38α/β. Cells were also kept in suspension in poly-2-hydroxyethyl methacrylate (polyHEMA)-coated dishes, as already described [25–29].
Western blotting (WB) and protein expression analyses
Cell cultures were lysed in sample buffer and processed as described previously [25–29]. Proteins were resolved by SDS-PAGE, electrotransferred and probed as already described [25–29]. Immunoreactive bands were visualized by the enhanced chemiluminescence (ECL) method (Amersham/Pharmacia, Baie D’UrFé, QC, Canada), according to the manufacturer’s instructions. Band intensities were scanned and semi-quantified with Scion Image (Scion, Frederick, MD), as previously described [25–31]. Typically, immunoreactive bands were semiquantified and the relative expression levels of proteins were established with the ratios protein/K18, which in turn were compared to those of control cultures, X100 (expressed as “% of control”).
Immunoprecipitation (IP) and relative kinase activation assays
Cell cultures were lysed in cold IP buffer and processed for IP as already described [25–29]. Immunoprecipitates were solubilized in sample buffer, resolved by SDS-PAGE and probed by WB (see above). Relative kinase activation analyses were performed as described previously [25–29, 31]. Typically, immunoreactive bands were semiquantified and the relative activated levels of kinases were established with the ratios phosphorylated kinase/total kinase, which in turn were compared to those of control cultures, X100 (expressed as “% of control”). Relative phosphorylated levels of proteins were similarly established.
Kinase autophosphorylation assays
Src was IP (see above) and immunoprecipitates were washed in IP buffer and kinase buffer as described already [26]. Assays and their analyses were performed as previously described [26].
Caspase-activated DNAse (CAD)-mediated DNA laddering assays
DNA was isolated and the visualization of CAD-mediated internucleosomal DNA fragmentation (DNA laddering) was performed as already described [25–29, 31].
In situ terminal deoxynucleotidyl transferase (TdT)-mediated dUTP nick-end labeling (ISEL) assays
Coverslip-grown cells were processed and ISEL was then carried out as already described [24–30]. Evaluation of ISEL-positive cells was performed as described previously [25–30]. Typically, apoptotic indices were compared to those of control cultures, X100 (expressed as “% of control”).
Transfections and cDNA constructs
Coverslip-grown cell cultures were transfected transiently and then processed for ISEL assays, as already described [26–31]. The cDNA constructs used were as follows: Fak WT, coding for wild type Fak; FakY397F, coding for a non-activable, dominant-negative mutant of Fak; FRNK (p45FRNK), coding for the dominant-negative, kinase domain-lacking isoform of Fak; Akt-1 WT, coding for wild type Akt-1; Akt-1DN, coding for a dominant-negative, kinase-dead mutant of Akt-1; Src WT, coding for wild type Src (Upstate Biotechnology); SrcK297R, coding for a dominant-negative, kinase-dead mutant of Src (Upstate Biotechnology); and Bcl-2 WT, coding for wild type Bcl-2. All constructs have been used previously as described [26–31]. Fak and Bcl-2 constructs were generous gifts from J.T. Parsons (Health Science Center, University of Virginia, Charlottesville, VA) and J.C. Reed (The Burnham Institute, LaJolla, CA), respectively.
Data processing
Results and values shown represent mean ± SEM for at least three (n ≥ 3) separate experiments and/or cultures. Statistically significant differences were determined with the Student t test. Data were compiled, analyzed and processed with Excel (Microsoft, Redmond, WA) and Cricket Graph (Computer Associates, Islandia, NY). Except otherwise specified, images from blots, gels and scans were processed with Vistascan (Umax), Photoshop (Adobe, San Jose, CA) and PowerPoint (Microsoft).
Results
HIEC cell anoikis is linked with a down-activation of Fak, Erk1/Erk2 and Akt-1
As shown in Fig. 1a, abundant CAD-mediated internucleosomal DNA degradation was observed in HIEC cultures that were maintained 24 h in suspension on polyHEMA (Fig. 1a, Susp.), as well as in cultures where β1 integrin binding activity was inhibited by blockade with the P4C10 antibody (Fig. 1a, P4C10), in contrast to control (adhering) cultures (Fig. 1a) and/or those exposed to non-immune IgG’s (Fig. 1a, IgG’s). The relative activation levels of Fak, Erk1/Erk2 and Akt-1 were then analyzed following anoikis induction. The activation of Fak (Fig. 2a and b, Susp.), of Akt-1 (Fig. 2a and c, Susp.) and of Erk2 (Fig. 2a and d, Susp.) were found significantly lowered in HIEC cultures undergoing anoikis.
Determinants of HIEC cell survival. (a) Representative CAD-mediated DNA laddering assays from HIEC cell control cultures (control; lanes 1, 8) and with the addition of CD (lane 2), Ly294002 (lane 3), PD98059 (lane 4), HA (lane 5), non-immune mouse IgG’s (lane 6), the β1 integrin-blocking antibody P4C10 (lane 7), or kept in suspension in polyHEMA-coated dishes (Susp.; lane 9). L, 100-bp DNA size markers. (b) HIEC cell cultures were maintained as in (a), and with PP2 as well. ISEL was then performed. (c) HIEC cells were transfected transiently with wild type Fak (Fak WT), FRNK (p45FRNK); FakY397F, wild type Akt-1 (Akt-1 WT), Akt-1 DN, wild type Src (Src WT), or SrcK297R. Sham-transfected (empty expression vectors) cells were used as controls. ISEL was then performed as in (b). (b and c) Statistically significant (0.001 ≤ P ≤ 0.01) differences between treated and control cultures are indicated by (*)
Cell adhesion-mediated engagement of Fak, PI3-K/Akt-1 and MEK/Erk in HIEC cell survival. (a) Representative WB analyses of Fak, Erk1/Erk2 and Akt-1 IPs from HIEC cell control cultures (control; lanes 1, 3, 5) and with the addition of non-immune mouse IgG’s (lane 2), P4C10 (lane 4), or kept in polyHEMA-coated dishes (Susp.; lane 6). Specific antibodies for pY397p125Fak, p(T202,Y204)p42Erk2/p44Erk1 and pS473p57Akt-1, as well as for respective total protein forms, were used. (b – d) Same as in (a), except that the relative activated levels of Fak (b), Akt-1 (c) and Erk2 (d) were established, then compared to controls. (b – d) Statistically significant (0.001 ≤ P ≤ 0.01) differences with control cultures are indicated by (*)
We then verified that such down-activations resulted directly from the loss of β1 integrin/Fak-mediated survival signaling. First, the antibody blockade of β1 integrins caused a significant down-activation of Fak (Fig. 2a and b, P4C10), of Akt-1 (Fig. 2a and c, P4C10) and of Erk2 (Fig. 2a and d, P4C10). Second, the inhibition of Fak with CD caused HIEC anoikis (Fig. 1a and b, CD) and its own down-activation (Fig. 2b, CD). In addition, the forced expression of p45FRNK and of FakY397F induced significant anoikis (Fig. 1c, p45FRNK, FakY397F vs. Fak WT). Third, the inhibition of Fak likewise caused a significant down-activation of Akt-1 (Fig. 2c, CD) and Erk2 (Fig. 2d, CD).
Implication of Src in β1 integrin/Fak-mediated HIEC cell survival
To verify whether Src participates in the suppression of HIEC cell anoikis mediated by β1 integrin/Fak signaling, we first analyzed the requirement of Src for the survival of HIEC cells. The inhibition of Src catalytic activity with HA or PP2 induced CAD-mediated DNA laddering (Fig. 1a, HA). These results were supported by ISEL (Fig. 1b, HA, PP2), as well as by significant reductions of Src activation (Fig. 3a and b, HA, PP2) and activity (Fig. 3c), following treatments. In addition, the forced expression of SrcK297R induced significant apoptosis/anoikis (Fig. 1c, SrcK297R vs. Src WT).
β1 integrin/Fak-mediated engagement of Src in HIEC cell survival. (a) Representative WB analyses of Src IPs from HIEC cell control cultures (control; lane 1) and with the addition of CD (lane 2), non-immune mouse IgG’s (lane 4), P4C10 (lane 5), PP2 (lane 6), or kept in polyHEMA-coated dishes (Susp.; lane 3). Specific antibodies for pY418p60Src, as well as for its total protein form (p60Src), were used. (b) Same as in (a), except that cells were also exposed to HA. In addition, the relative activated levels of Src were established. Statistically significant (0.001 ≤ P ≤ 0.01) differences with control cultures are indicated by (*). (c) Representative Src autophosphorylation kinase assays (32P-p60Src) and WB analyses (p60Src) from HIEC cell control cultures (control; lanes 1) and with HA (lanes 2). Ab, antibody used to IP Src
The relative activation levels of Src were then analyzed following anoikis induction in HIEC cells. The activation of Src was found significantly lowered in cultures undergoing anoikis (Fig. 3a and b, Susp.). That such down-activation of Src was caused largely from the loss of β1 integrin/Fak-mediated suppression of anoikis was thereafter verified. First, the blockade of β1 integrins resulted in significant reductions of Src activation (Fig. 3a and b, P4C10), in contrast to cultures exposed to IgG’s (Fig. 3a and b, IgG’s). Second, the inhibition of Fak likewise caused a significant down-activation of Src (Fig. 3a and b, CD). Third, the inhibition of Src (Fig. 4a, PP2) or Fak (not shown), as well as the induction of anoikis proper (Fig. 4a, Susp.), resulted in drastic reductions of Src-mediated Y576/577 phosphorylation of Fak. Such phosphorylation of Fak is not only indicative of Src catalytic activity, but also of Fak–Src interactions [14–17]. These results were corroborated with follow-up co-IP analyses, showing that anoikis and/or blockade of β1 integrin binding cause indeed a loss of Src association with Fak signaling cassettes (Fig. 4b).
Src acts as a cornerstone for the engagement of PI3-K/Akt-1 and MEK/Erk by β1 integrin/Fak survival signaling in HIEC cells. (a) Representative WB analyses of Fak IPs from HIEC cell control cultures (control; lanes 1, 3) and with the addition of PP2 (lane 2), or kept in polyHEMA-coated dishes (Susp.; lane 4). Specific antibodies for Src-mediated pY576/577p125Fak, as well as for its total protein form (p125Fak), were used. (b) Representative WB analyses of Fak IPs from HIEC cell cultures with the addition of non-immune mouse IgG’s (control; lane 1), P4C10 (lane 3), or kept in polyHEMA-coated dishes (Susp.; lane 2). Specific antibodies for Src (p60Src) and Fak (p125Fak) were used. (c) Representative WB analyses of Akt-1 and Erk1/Erk2 IPs from HIEC cell control cultures (control; lane 1) and with the addition of PP2 (lane 2). Specific antibodies for pS473p57Akt-1 and p(T202,Y204)p42Erk2/p44Erk1, as well as for respective total protein forms, were used. (d) Representative WB analyses of Fak IPs from HIEC cell control cultures (control; lane 1) and with the addition of non-immune mouse IgG’s (lane 2), P4C10 (lane 3), or HA (lane 4). Specific antibodies for p85PI3-K and p125Fak were used
We then analyzed the functions of Src in the cell adhesion/Fak-mediated engagement of the PI3-K/Akt-1 and MEK/Erk pathways (see above) in HIEC cells. The inhibition of Src resulted in a reduction of both Akt-1 (Fig. 4c, PP2) and Erk2 (Fig. 4c, PP2) activation. In addition, the inhibition of Src caused in a drastic loss of association of p85PI3-K with Fak signaling complexes (Fig. 4d, HA), as in the case when β1 integrin binding activity is blocked (Fig. 4d, P4C10).
p38β drives HIEC cell apoptosis/anoikis
We have previously reported that apoptosis/anoikis is driven selectively by the p38β isoform of the p38SAPK pathway in undifferentiated human enterocytes [28, 29]. As shown by complementary/supportive analyses herein, the induction of anoikis is paralleled by time-course (0–24 h) sustained/enhanced relative levels of p38SAPK activation (p(T180,Y182)p38/p38) which peak at 4 h (Fig. 5a, Suspension), in sharp contrast to control cultures (Fig. 5a, Control). The same is observed when Fak is inhibited [28, 29]. IP analyses at the 4 h time-point revealed that p38β is the isoform which is sustained in its activation, not p38α (Fig. 5b, Susp.). In addition, the inhibition of the catalytic activity of p38SAPK with SB203580 (or SB202190) significantly attenuated HIEC cell anoikis induced by keeping cells in suspension (Fig. 5c, Susp. vs. Susp. + SB203580), by the inhibition of Fak (Fig. 5d, CD vs. CD + SB202190) or by the inhibition of β1 integrins (Fig. 5d, P4C10 vs. P4C10 + SB202190), whereas such p38SAPK inhibition alone did not influence HIEC cell survival (Fig. 5c, SB203590; and Fig. 5d, SB202190). Subsequent transfection experiments further demonstrated this requirement for p38β in driving apoptosis/anoikis [28, 29].
β1 integrin/Fak/Src survival signaling antagonizes the activation of the apoptosis/anoikis-driver p38β SAPK isoform via PI3-K/Akt-1 in HIEC cells. (a) Relative activation levels of p38SAPK in HIEC cells maintained 0–24 h in serum-free medium (control; filled squares) and with the addition of Ly294002 (open squares), HA (open circles), PD98059 (filled lozenges), or kept in polyHEMA-coated dishes (filled circles). Specific antibodies for the detection of p(T180,Y182)p38 and p38 protein were used. The relative activation levels of p38 were established. (b) Representative WB analyses of p38α and p38β IPs from HIEC cell cultures which were maintained 4 h in serum-free medium (control) with the addition of HA, or kept in polyHEMA-coated dishes (Susp.). Specific antibodies for p(T180,Y182)p38 and p38 proteins were used. (c) Representative DNA laddering assays from HIEC cell control cultures (control; lane 1) and with the addition of SB203580 (lanes 2, 4, 6), HA (lanes 3, 4), or kept in polyHEMA-coated dishes (Susp.; lanes 5, 6). L, 100-bp DNA size markers. (d) Same as in (c), except that cells were also exposed to Ly294002, PD98059, non-immune mouse IgG’s, or P4C10, and SB202190 was used instead of SB203580. In addition, ISEL was then performed. Statistically significant (0.001 ≤ p ≤ 0.01) differences between treatments and controls, as well as between treatments and their counterparts with SB202190, are indicated by (*) and (**) respectively
To this effect, additional experiments herein show that the inhibition of Src likewise resulted in time-course sustained/enhanced levels of p38SAPK activation (Fig. 5a, HA). IP analyses at the 4 h time-point also revealed that it is p38β, not p38α, which has its activation thus enhanced/sustained (Fig. 5b, HA). Furthermore, the inhibition of p38SAPK likewise attenuated HIEC cell apoptosis/anoikis induced by the inhibition of Src (Fig. 5c, HA vs. HA + SB203580; and Fig. 5d, HA vs. HA + SB202190).
Selective roles of PI3-K/Akt-1 and MEK/Erk in HIEC cell survival
We then analyzed the roles of the PI3-K/Akt-1 and MEK/Erk pathways in promoting HIEC cell survival. The inhibition of MEK-1/-2 activity with PD98059 failed to affect the survival of HIEC cells (Fig. 1a and b, PD98059). Even doubling the concentration of PD98059 failed to elicit apoptosis (not shown). On the other hand, the inhibition of PI3-K activity with Ly294002 induced significant HIEC cell apoptosis (Fig. 1a and b, Ly294002). To confirm the efficiency of the treatments, the relative activation levels of Akt-1 and Erk2 were analyzed. The inhibition of PI3-K resulted in a significant down-activation of Akt-1 (Fig. 2c, Ly294002). In contrast, neither Fak (Fig. 2b, Ly294002), Erk2 (Fig. 2d, Ly294002) or Src (not shown) activation were affected. In turn, the inhibition of MEK-1/-2 resulted in a significant reduction of Erk2 activation (Fig. 2d, PD98059), whereas the activation of Fak (Fig. 2b, PD98059), Akt-1 (Fig. 2c, PD98059) or Src (not shown) was not affected.
The results on the selective roles of PI3-K/Akt-1 and MEK/Erk in HIEC cell survival were then further demonstrated. First, the forced expression of Akt-1DN induced significant apoptosis (Fig. 1c, Akt-1 DN vs. Akt-1 WT). A dominant negative mutant of MEK-1 (or -2) was not available at the time these studies were performed––incidentally, the overexpression of a constitutive active MEK-1 mutant fails to confer anchorage-independent growth in HIEC cells [34]. Second, the inhibition of PI3-K resulted in time-course sustained/enhanced levels of p38SAPK activation (Fig. 5a, Ly294002) and, more specifically, that of p38β alone (not shown; see refs. 39–40). In contrast, the inhibition of MEK-1/-2 failed to enact such time-course sustained/enhanced levels of p38SAPK activation (Fig. 5a, PD98059) and, accordingly, did not result in the sustained/enhanced activation of p38β specifically (not shown; see ref. 28). Third, the inhibition of p38SAPK attenuated HIEC cell apoptosis/anoikis induced by the inhibition of PI3-K (Fig. 5d, Ly294002 vs. Ly294002 + SB202190), whereas such p38SAPK inhibition had no effect on the failure of MEK-1/-2 inhibition to influence HIEC cell survival (Fig. 5d, PD98059 vs. PD98059 + SB202190).
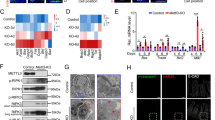
HIEC cell adhesion-mediated complex modulations of Bcl-2 homologs
To better understand the selective nature of the roles of the PI3-K/Akt-1 and MEK/Erk pathways in HIEC cell survival, we investigated the expression levels of five Bcl-2 homologs (anti-apoptotics: Bcl-2, Bcl-XL and Mcl-1; pro-apoptotics: Bax, Bak). As we have shown previously [28], and further supported by complementary/additional analyses herein, the PI3-K/Akt-1 and MEK/Erk pathways perform clearly distinct functions in regulating the expression of Bcl-2 homologs in HIEC cells (Fig. 6). On the one hand, the inhibition of PI3-K/Akt-1 caused a significant down-regulation of the expression of Bcl-XL and Mcl-1 without affecting Bcl-2 (Fig. 6a and b, Ly294002), while at the same time causing a significant up-regulation of Bax and Bak (Fig. 6a and c, Ly294002). On the other hand, the inhibition of MEK/Erk significantly down-regulated the expression of Bcl-2 (Fig. 6a and b, PD98059), without significantly affecting the other four homologs analyzed (Fig. 6a and c, PD98059). Incidentally, our further analyses herein show that anoikis proper resulted in a down-regulation of Bcl-2, Bcl-XL and Mcl-1 expression (Fig. 6a and b, Susp.), while at the same time causing an up-regulation of Bax and Bak (Fig. 6a and c, Susp.), which corresponds to the combined effects of the inhibition of PI3-K/Akt-1 and MEK/Erk. Likewise, the inhibition of Fak [28] or Src (Fig. 6a and c, HA) resulted in similar, if not closely related, modulations of all five Bcl-2 homologs analyzed.
β1 integrin/Fak/Src, PI3-K/Akt-1 and MEK/Erk regulation of Bcl-2 homologs in HIEC cells. (a) Representative WB analyses of the expression of Bcl-2 homologs from HIEC cell control cultures (control; lanes 1, 5) and with the addition of HA (lane 2), Ly294002 (lane 3), PD98059 (lane 4), or kept in polyHEMA-coated dishes (Susp.; lane 6). Specific antibodies for Bcl-2, Bcl-XL, Mcl-1, Bax and Bak were used. K18 was also detected as reference protein. (b and c) Same as in (a), except the relative expression levels of Bcl-2 homologs were established with the ratios (b) Bcl-2/K18 (open columns), Bcl-XL/K18 (filled columns) and Mcl-1/K18 (grey columns), or (c) Bax/K18 (open columns) and Bak/K18 (filled columns). Statistically significant (0.001 ≤ p ≤ 0.01) differences with control cultures are indicated by (*)
We thereafter investigated the inhibitory phosphorylation state of the pro-apoptotic homolog Bad, at its serine112 and 136 residues. Our analyses show that anoikis proper resulted in a drastic loss of Bad inhibitory phosphorylation at both residues (Fig. 7a and b, Susp.), and that the inhibition of Src likewise caused such a sharp loss of pS112Bad and pS136Bad (Fig. 7a and b, HA). Interestingly, the inhibition of PI3-K/Akt-1 not only resulted in a drastic reduction of pS136Bad, but also caused a significant reduction of pS112Bad (Fig. 7a and b, Ly294002). Conversely, the inhibition of the MEK/Erk pathway resulted in a significant reduction of pS112Bad, without affecting phosphorylation at the S136 residue (Fig. 7a and b, PD98059).
(a, b) Roles of PI3-K/Akt-1 and MEK/Erk on the inhibitory phosphorylation of Bad in HIEC cells. (a) Representative WB analyses of the phosphorylation of Bad from HIEC cell control cultures (control; lanes 1, 5) and with the addition of Ly294002 (lane 2), PD98059 (lane 3), HA (lane 4), or kept in polyHEMA-coated dishes (Susp.; lane 6). Specific antibodies for pS112Bad and pS136Bad, as well as for total Bad protein, were used. (b) Same as in (a), except that the relative phosphorylated levels of Bad were established with the ratios pS112Bad/Bad (filled columns) and pS136Bad/Bad (open columns), which were in turn compared controls. Statistically significant (0.001 ≤ p ≤ 0.01) differences with control cultures are indicated by (*). (c) Overexpression of Bcl-2 is sufficient to attenuate HIEC cell anoikis. WB analyses for the detection of Bcl-2 (upper panel) and DNA laddering assays (lower panel) of HIEC cells transfected transiently with either an empty expression vector (control; lanes 1, 2) or with wild type Bcl-2 (Bcl-2 WT; lanes 3, 4), and thereafter kept in serum-free medium for 24 h (lanes 1, 3) or in polyHEMA-coated dishes (Susp.; lanes 2, 4). L, 100-bp DNA size markers
Lastly, we confirmed that the failure of the inhibition of the MEK/Erk pathway to hamper HIEC cell survival lies not only with its failure in causing the activation of p38β (see previous sections), but also with its marginal impact on the overall balance of expression and activities of anti- and pro-apoptotic Bcl-2 homologs. HIEC cells were transfected to transiently overexpress Bcl-2, the expression of which is modulated by MEK/Erk in HIEC cells (see above). In contrast to cells transfected with an empty vector and which readily underwent anoikis (Fig. 7c, Empty vector vs. Empty vector + Susp.), cells which overexpressed Bcl-2 exhibited attenuated anoikis under the same conditions (Fig. 7c, Bcl-2 WT vs. Bcl-2 WT + Susp.)––thus indicating that such overexpression of Bcl-2 alone was sufficient to delay the process of anoikis.
Discussion
In the present study, we investigated the molecular determinants which dictate survival and apoptosis/anoikis in normal HIEC cells, specifically with regards to the roles of β1 integrin/Fak/Src survival signaling to the PI3-K/Akt-1, MEK/Erk and p38SAPK pathways, as well as their roles in modulating the expression/activity of Bcl-2 homologs. Herein, we provide evidence that the promotion of HIEC cell survival and suppression of apoptosis/anoikis by β1 integrins is dependent on associated Fak signaling complexes, in which Src is recruited for the engagement of both the PI3-K/Akt-1 and MEK/Erk pathways. We also demonstrate that PI3-K/Akt-1 and MEK/Erk perform selective roles in HIEC cell survival, in the suppression of the activation of the enterocytic apoptosis/anoikis-driving p38β isoform, and in the regulation of the expression/activity of various Bcl-2 homologs. Furthermore, we show that β1 integrins/Fak and/or Src perform the same regulatory functions of Bcl-2 homolog expression/activity, and of p38β activation, as both PI3-K/Atk-1 and MEK/Erk combined. Hence, as summarized in Fig. 8, β1 integrin/Fak/Src signaling translates into complex, integrated mediating functions of p38β activation and regulation of Bcl-2 homologs by the PI3-K/Akt-1 and MEK/Erk pathways.
β1 integrin/Fak/Src survival signaling in HIEC cells translates into complex, integrated mediating functions of p38β activation and regulation of Bcl-2 homologs by the PI3-K/Akt-1 and MEK/Erk pathways. Schematic drawing which summarizes the results of the present study and which illustrates how β1 integrin/Fak-mediated HIEC cell adhesion signaling recruits Src in order to engage both the PI3-K/Akt-1 and MEK/Erk pathways in the promotion of cell survival
Cell-ECM interactions perform critical functions in the control of adhesion, migration, restitution, proliferation, polarization and differentiation of the gut epithelium [21, 35, 36]. It is therefore not surprising that such interactions, mediated largely through integrins, likewise perform crucial roles in the promotion and maintenance of the survival of IECs [8, 21]. The microenvironment of the typical intestinal crypt is defined in good part by specific components in its basement membrane, thus distinguishing it from that of the villus [21, 23, 35]. Concordantly, the expression profile of integrins in crypt cells is clearly distinct from that of villus cells, thus enabling selective roles of specific integrin-ECM component interactions in the regulation of crypt and villus cell processes within the context of the maintenance and dynamic renewal of the gut epithelium [21, 35, 36]. One example of such distinctions is the α6β4 integrin, which is required for the survival of differentiated/villus enterocytes [25] but not of undifferentiated/crypt ones [25, 28]. Much remains to be understood and/or characterized of the crypt-villus specific integrin-ECM component interactions and their precise functions in enterocytic processes, as well as the signaling pathways they engage, including in the suppression of apoptosis/anoikis.
As a cytoplasmic, non-receptor tyrosine kinase, Src has been found to perform diverse functions in the cell adhesion-mediated control of cellular processes such as cell proliferation, adhesion, spreading and migration, depending on the cell type studied [14–17]. With regards to IEC survival, Src has been shown to play a role in the suppression of anoikis in rodent and human undifferentiated enterocytes [26, 37–39], as well as in differentiated human colonocytes [40] and enterocytes [26]. In addition, elevated Src expression and/or activity may contribute to the resistance to anoikis that is observed in transformed rodent enterocytes [37, 38] and highly tumorigenic, dedifferentiated colon cancer cells [41, 42]. However, much remains to be understood of the roles of Src in IEC survival, as well as its specific contributions in cell adhesion-mediated suppression of anoikis. In this respect, the present study not only provides evidence that Src is required for the survival of normal, non-transformed and non-immortalized HIEC cells, but furthermore identifies Src as a crucial effector of the specific β1 integrin/Fak-mediated suppression of anoikis in these same cells. In addition, we show for the first time that such an effector role by Src in HIEC cells is to act, in good part, as a cornerstone in the engagement of both the PI3-K/Akt-1 and MEK/Erk pathways by β1 integrin/Fak signaling (Fig. 8). Consequently, this explains why the effects of the upstream inhibition of β1 integrins, Fak and/or Src on the activation of the p38β SAPK isoform, as well as on the regulation of expression/activity of Bcl-2 homologs, correspond largely to the combined effects of the downstream inhibition of PI3-K/Akt-1 and MEK/Erk on these same survival determinants (Fig. 8).
Although β1 integrin/Fak signaling in HIEC cells engages both PI3-K/Akt-1 and MEK/Erk via Src, the present study furthermore demonstrates that these two pathways nonetheless perform distinctive roles in HIEC cell survival (Fig. 8). PI3-K/Akt and MEK/Erk are recognized as crucial effectors of survival for numerous cell types, in addition to a plethora of roles in various other cellular processes [5–10, 18, 21, 36]. However, much remains to be elucidated with regards to the roles of MEK/Erk and PI3-K/Akt in enterocytic survival. To this effect, the engagement and/or specific functions of these two pathways vary greatly depending on the tissue and cell contexts [5–10, 18, 21, 36]. In the specific case of HIEC cells, the present study provides evidence that PI3-K/Akt-1 is crucial for survival by virtue of its extensive roles in (i) antagonizing the activation of p38β; (ii) prominently influencing the balance of expression of anti- (Mcl-1, Bcl-XL) and pro- (Bax, Bak) apoptotic Bcl-2 homologs; and (iii) driving the inhibitory phosphorylation of the pro-apoptotic homolog Bad on both its S112 and S136 residues (Fig. 8). By contrast, and as we reported previously [25, 26, 28], MEK/Erk is not required for the survival of HIEC cells. As shown herein, such a lack of requirement is due to (i) its non-involvement in regulating the activation of p38β; (ii) its apparent marginal role in influencing the overall balance of Bcl-2 homolog expression (affecting Bcl-2 only); and (iii) its driving of the phosphorylation of Bad on the S112 residue only (Fig. 8). Hence, these findings bring novel insights into the roles of the PI3-K/Akt-1 and MEK/Erk pathways in the regulation of HIEC cell survival, especially that driven by β1 integrin/Fak/Src signaling. In addition, the present study provides tentative molecular bases as to why MEK/Erk is not required for the survival of human undifferentiated/crypt IECs.
It is noteworthy that our findings highlight differentiation state-related distinctions in the regulatory mechanisms of enterocytic cell survival and apoptosis/anoikis. For instance, PI3-K/Akt-1 contributes in the promotion of apoptosis/anoikis suppression in differentiated/villus human enterocytes [25–27, 29], as in the case of their undifferentiated/crypt counterparts; however, this pathway in differentiated cells similarly up-regulates Bcl-XL and Mcl-1 as in undifferentiated/crypt cells, but only down-regulates Bax [25]. In addition, PI3-K/Akt-1 antagonizes the activation of p38δ which drives apoptosis/anoikis in differentiated human enterocytes [29], instead of p38β. Correspondingly, MEK/Erk is required for the survival of human differentiated/villus enterocytes [25, 26], in sharp opposition to undifferentiated/crypt ones. Furthermore, MEK/Erk in differentiated human IECs up-regulates Bcl-2 and Bcl-XL while down-regulating Bak [25], thus influencing significantly the balance of Bcl-2 homolog expression within this context of enterocytic differentiated state. Moreover, our recent studies in human differentiated IECs have demonstrated that Src contributes selectively in the β1 integrin/Fak-mediated engagement of MEK/Erk only, whereas PI3-K/Akt-1 is Src-independent while remaining β1 integrin/Fak-dependent within this context [26]. Hence, these data altogether further emphasize the principle that differentiation state-distinct mechanisms prevail in the regulation of cell survival and apoptosis/anoikis in the gut epithelium [8, 21], and that crypt cells must be considered separately from villus cells in this respect.
The present findings likewise highlight differences in the regulatory mechanisms of cell survival between IECs of human and rodent (namely, rat) origin. For instance, PI3-K/Akt is crucial for the survival of undifferentiated rat enterocytes [38, 39, 43], as in the case of human ones - however, this pathway in rat cells does not influence the expression of Bcl-XL and only down-regulates Bak [37, 43]. Additionally, the MEK/Erk pathway has not only been shown to be a crucial determinant for the survival of rat undifferentiated/crypt IECs [34, 38, 44], in stark contrast to human ones (see above), but was also reported to up-regulate Bcl-2, Bcl-XL and Mcl-1 while down-regulating Bak [43, 44]. And although the p38SAPK pathway has been reported to drive apoptosis/anoikis in both rat [45–47] and human (this study; see also refs. 28–29) undifferentiated IECs, recent evidence indicate that it is p38α which is selectively involved in the rat cells [47] instead of p38β. Yet another example is the fact that the crypt-villus axis expression profile of Bcl-2 homologs in man has been shown to differ from that observed in rats [20, 21, 24]. Hence, it is now becoming clear that the regulation of IEC survival implicates non-negligible species-specific distinctions, which should be taken into account when extrapolating observations from rat IECs to human ones.
A better understanding of the regulation of IEC survival, apoptosis and anoikis is of significance to the physiopathology of the gut mucosa. For example, major alterations in epithelial integrity and composition of the basement membrane are observed in inflammatory bowel disease [20–22, 48, 49]. Nonetheless, much remains to be understood of the signaling pathways involved in this context, as well as the overall impact on the balance of Bcl-2 homolog expression/activity [49]. Likewise, alterations in basement membrane composition, as well as in the repertoire of integrins expressed, constitute landmarks of cancers - including those of the colon [20–22, 35, 36, 48, 50]. Incidentally, increased Bcl-XL expression, as well as a decrease and/or loss of Bax and Bak, constitute common features of colon cancers [20–22, 50]. The recent identifications of mutated, constitutive active forms of PI3-K and Akt-1 in some colon cancers [10–12, 50], as well as the reported requirement of MEK/Erk for the survival of colon cancer cells [21, 22, 34, 36, 50], further underlie the need for an improved comprehension of the regulatory mechanisms which dictate life and death of gut epithelial cells.
Conclusion
In conclusion, this study allows for a clearer picture of the molecular determinants that are involved in the regulation of HIEC cell survival (Fig. 8). Specifically, the present findings provide evidence that β1 integrins/Fak/Src signaling translates into integrated, complex regulatory functions by PI3-K/Akt-1 and MEK/Erk in the expression/activity of Bcl-2 homologs, as well as in the specific activation of the apoptosis/anoikis-driving p38β SAPK isoform, consequently determining their requirement (or not) in the maintenance of HIEC cell survival. Further studies, in addition to the present findings, should provide a greater understanding of the inherent complexities in the control of cell survival and apoptosis/anoikis not only within the normal context of the maintenance and renewal of the epithelium of the gut, but as well within the physiopathological context of gut disorders.
References
Jacobson MD, Weil M, Raff MC (1997) Programmed cell death in animal development. Cell 88:347–354
Reed JC (1998) Bcl-2 family proteins. Oncogene 17:3225–3236
Cory S, Huang DCS, Adams JM (2003) The Bcl-2 family: roles in cell survival and oncogenesis. Oncogene 22:8590–8607
Frisch SM, Screaton RA (2001) Anoikis mechanisms. Curr Opin Cell Biol 13:555–562
Stupack DG, Cheresh DA (2002) Get a ligand, get a life: integrins, signaling and cell survival. J Cell Sci 115:3729–3738
Martin SS, Vuori K (2004) Regulation of Bcl-2 proteins during anoikis and amorphosis. Biochim Biophys Acta 1692:145–157
Reddig PJ, Juliano RL (2005) Clinging to life: cell to matrix adhesion and cell survival. Cancer Metastasis Rev 24:425–439
Vachon PH (2006) Cell survival: differences and differentiation. Med Sci 22:423–429
Giancotti FG, Ruoslahti E (1999) Integrin signaling. Science 285:1028–1032
Damsky CH, Ilic D (2002) Integrin signaling: it’s where the action is. Curr Opin Cell Biol 14:594–602
Manning BD, Cantley LC (2007) AKT/PKB signaling: navigating downstream. Cell 129:1271–1274
Altomare DA, Testa JR (2005) Perturbations of the Akt signaling pathway in human cancer. Oncogene 24:7455–7464
Kyriakis JM, Avruch J (2001) Mammalian mitogen-activated protein kinase signal transduction pathways activated by stress and inflammation. Physiol Rev 81:807–869
Mitra SK, Schlaepfer DD (2006) Integrin-regulated FAK-Src signaling in normal and cancer cells. Curr Opin Cell Biol 18:516–523
Parsons JT (2003) Focal adhesion kinase: the first ten years. J Cell Sci 116:1409–1416
Frame MC (2004) Newest findings on the oldest oncogene; how activated src does it. J Cell Sci 117:989–998
Parsons SJ, Parsons JT (2004) Src family kinases, key regulators of signal transduction. Oncogene 23:7906–7909
Raman M, Chen W, Cobb MH (2007) Differential regulation and properties of MAPKs. Oncogene 26:3100–3112
Nagai H, Noguchi T, Takeda K, Ichijo H (2007) Pathophysiological roles of ASK1-MAP kinase signaling pathways. J Biochem Mol Biol 40:1–6
Potten CS (1997) Epithelial cell growth and differentiation II. Intestinal apoptosis. Am J Physiol 273:G253–G257
Ménard D, Beaulieu J-F, Boudreau F, Perreault N, Rivard N, Vachon PH (2005) Gastrointestinal tract. In: Unsicker K, Kriegelstein K (eds) Cell signaling and growth factors in development II. Verlag, Wiley-VCH, pp 755–790
Edelblum KL, Yan F, Yamaoka T, Polk DB (2006) Regulation of apoptosis during homeostasis and disease in the intestinal epithelium. Inflamm Bowel Dis 12:413–424
Yen TH, Wright NA (2006) The gastrointestinal tract stem cell niche. Stem Cell Rev 2:203–212
Vachon PH, Cardin É, Harnois C et al (2000) Early establishment of epithelial apoptosis in the developing human small intestine. Int J Dev Biol 44:891–898
Gauthier R, Harnois C, Drolet J-F et al (2001) Human intestinal epithelial cell survival; differentiation state-specific control mechanisms. Am J Physiol 280:C1540–C1554
Bouchard V, Demers M-J, Thibodeau S et al (2007) Fak/Src signaling in human intestinal epithelial cell survival and anoikis: differentiation state-specific uncoupling with the PI3-K/Akt-1 and MEK/Erk pathways. J Cell Physiol 212:717–728
Dufour G, Demers M-J, Gagné D et al (2004) Human intestinal epithelial cell survival and anoikis. Differentiation state-distinct regulation and roles of protein kinase B/Akt isoforms. J Biol Chem 279:44113–44122
Harnois C, Demers M-J, Bouchard V et al (2004) Human intestinal epithelial crypt cell survival and death: Complex modulations of Bcl-2 homologs by Fak, PI3-K/Akt-1, MEK/Erk, and p38 signaling pathways. J Cell Physiol 198:209–222
Vachon PH, Harnois C, Grenier A et al (2002) Differentiation state-selective roles of p38 isoforms in human intestinal epithelial cell anoikis. Gastroenterology 123:1980–1991
Vachon PH, Xu H, Liu L et al (1997) Integrins (α7β1) in muscle function and survival; disrupted expression in merosin-deficient congenital muscular dystrophy. J Clin Invest 100:1870–1881
Laprise P, Vallée K, Demers M-J et al (2003) Merosin (laminin-2/4)-driven survival signaling: complex modulations of Bcl-2 homologs. J Cell Biochem 89:1115–1125
Pageot L-P, Perreault N, Basora N et al (2000) Human cell models to study small intestinal functions: recapitulation of the crypt-villus axis. Microsc Res Tech 49:394–406
Wary KK, Dans M, Mariotti A, Giancotti FG (2005) Biochemical analysis of integrin-mediated Shc signaling. In: Howlett AR (ed) Methods in molecular biology, vol 129. Integrin protocols, Humana Press, Totowa, pp 35–49
Boucher MJ, Jean D, Vézina A, Rivard N (2004) Dual role of MEK/ERK signaling in senescence and transformation of intestinal epithelial cells. Am J Physiol 286: G736–G746
Lussier C, Basora N, Bouatrouss Y, Beaulieu JF (2000) Integrins as mediators of epithelial cell-matrix interactions in the human small intestinal mucosa. Microsc Res Tech 51:169–178
Basson MD (2003) Cell-matrix interactions in the gut epithelium. Surgery 133:263–267
Rosen K, Loza Coll M, Li A, Filmus J (2001) Transforming growth factor-alpha prevents detachment-induced inhibition of c-Src kinase activity, Bcl-XL down-regulation, and apoptosis of intestinal epithelial cells. J Biol Chem 276:37273–37279
Loza-Coll M, Perera S, Shi W, Filmus J (2005) A transient increase in the activity of Src-family kinases induced by cell detachment delays anoikis of intestinal epithelial cells. Oncogene 24:1727–1737
Bhattacharya S, Ray RM, Johnson LR (2006) Integrin beta3-mediated Src activation regulates apoptosis in IEC-6 cells via Akt and STAT3. Biochem J 397:437–447
Hofmann C, Obermeier F, Artinger M et al (2007) Cell-cell contacts prevent anoikis in primary human colonic epithelial cells. Gastroenterology 132:587–600
Windham TC, Parikh NU, Siwak DR et al (2002) Src activation regulates anoikis in human colon tumor cell lines. Oncogene 21:7797–7807
Golubovskaya VM, Gross S, Kaur AS et al (2003) Simultaneous inhibition of focal adhesion kinase and SRC enhances detachment and apoptosis in colon cancer cell lines. Mol Cancer Res 1:755–764
Rosen K, Rak J, Leung T et al (2000) Activated Ras prevents downregulation of Bcl-X(L) triggered by detachment from the extracellular matrix. A mechanism of Ras-induced resistance to anoikis in intestinal epithelial cells. J Cell Biol 149:447–456
Horikawa Y, Otaka M, Komatsu K et al (2007) MEK activation suppresses CPT11-induced apoptosis in rat intestinal epithelial cells through a COX-2-dependent mechanism. Dig Dis Sci 52:2757–2765
Rosen K, Shi W, Calabretta B, Filmus J (2002) Cell detachment triggers p38 mitogen-activated protein kinase-dependent over-expression of Fas ligand. J Biol Chem 277:46123–46130
Zhou Y, Wang Q, Evers MB, Chung DH (2006) Oxidative stress-induced intestinal epithelial cell apoptosis is mediated by p38 MAPK. Biochem Biophys Res Commun 350:860–865
Sheng G, Guo J, Warner BW (2007) Epidermal growth factor receptor signaling modulates apoptosis via p38alpha MAPK-dependent activation of Bax in intestinal epithelial cells. Am J Physiol 293: G599–G606
Teller IC, Beaulieu JF (2001) Interactions between laminin and epithelial cells in intestinal health and disease. Expert Rev Mol Med 3:1–18
Ruemmele FM, Seidman EG, Lentze MJ (2002) Regulation of intestinal epithelial cell apoptosis and the pathogenesis of inflammatory bowel disorders. J Pediatr Gastroenterol Nut 34:254–260
Watson AJM (2004) Apoptosis and colorectal cancer. Gut 53:1701–1709
Acknowledgements
The authors thank Drs. J. Landry (Centre de Recherche en Cancérologie de l’Université Laval, C.H.U.L., QC, Canada), J.T. Parsons (Health Science Center, University of Virginia, Charlottesville, VA, USA), J.C. Reed (The Burnham Institute, LaJolla, CA, USA) and E. Ruoslahti (The Burnham Institute, LaJolla, CA) for the kind gift of tools. Financial support: Canadian Institutes of Health Research (CIHR) and The Cancer Research Society Inc. P.H.V. is a Chercheur-Boursier Sénior du Fonds de la Recherche en Santé du Québec (FRSQ) and a Chercheur de la Fondation Canadienne pour l’Innovation (FCI/CFI).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bouchard, V., Harnois, C., Demers, MJ. et al. β1 integrin/Fak/Src signaling in intestinal epithelial crypt cell survival: integration of complex regulatory mechanisms. Apoptosis 13, 531–542 (2008). https://doi.org/10.1007/s10495-008-0192-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10495-008-0192-y