Abstract
This study examines general hospitals’ adjustments in psychiatric bed utilization practices in response to increases in psychiatric inpatient admissions. Using panel data from 439 hospitals, monthly observations (N = 7,831) between 2007 and 2010 on psychiatric admissions, psychiatric bed occupancy rates, and average length-of-stay were created for psychiatric inpatients. In fixed-effects regressions, an increase in psychiatric admissions was associated with an increase in the probability of psychiatric bed use exceeding 100 % occupancy and with a reduction of mean length-of-stay. These results were confirmed in instrumental variables models. General hospitals may dynamically adjust bed utilization practices in response to changing psychiatric bed needs. An implication of this dynamic adjustment model is that bed shortages are likely to be local, transitory events.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Over the past decade, reports of nationwide psychiatric bed shortages have drawn the attention of both the media and public officials (Alakeson et al. 2010; American College of Emergency Physicians 2008; Baraff et al. 2006; Sharfstein and Dickerson 2009). Some observers have warned of serious harm resulting from not having enough psychiatric beds (e.g., Torrey et al. 2008), such as increased homelessness and incarceration of persons with serious mental illnesses and increased risks of physical harm to psychiatric patients or members of the public. The number of psychiatric beds per capita did decrease sharply during 1990s and early 2000s (National Center for Health Statistics 2012), a trend that has often been cited in reports of potential shortages. However, shortages may be difficult to quantify and may be constantly in flux, both because psychiatric bed use is constantly changing and because hospitals potentially can adjust dynamically to changes in bed availability.
The term “bed shortage” seemingly implies that not enough beds are available for the people who need them, and that consequently many acutely ill, psychiatric patients are inappropriately denied access to an inpatient bed. However, to accommodate additional inpatients despite high psychiatric bed occupancy, some hospitals may place psychiatric inpatients in unoccupied general medical beds or “scatter beds” (Mark et al. 2010) rather than in beds located within distinct psychiatric care units, or may reduce average psychiatric length-of-stay by accelerating the discharge planning process. Shorter lengths-of-stay would allow the number of admissions to increase, as the total number of bed days is the product of length-of-stay and number of admissions. Although very little research has been done on these types of hospital adjustments in response to changes in psychiatric bed need, evidence found in one recent study of psychiatric bed closures in a large urban hospital (Shumway et al. 2012) suggests that some hospitals do accelerate discharge planning to increase spare bed capacity.
Whether or not general hospitals adjust their use of scatter beds or length-of-stay in response to fluctuations in psychiatric bed need may affect one’s interpretation of the term bed shortage. Observers often ascribe the existence of a bed shortage to a decline in the number of specialized psychiatric beds (e.g., Lamb and Weinberger 2005). This perspective assumes that the number of psychiatric beds needed to accommodate a given population is a fixed constant. However, if hospitals can adjust scatter bed use or length-of-stay, the number of psychiatric beds needed in a population may change dynamically over time. Thus, a decrease in the number of psychiatric beds would result in adjustment to a new equilibrium between length-of-stay, scatter bed use, and inpatient volume. This dynamic model of hospital adjustment would imply that “shortages” are transitory dis-equilibrium phenomena whose existence and resolution depends on local area factors, such as local population growth and local bed capacity, as well as on hospital-specific adjustments to changes in bed needs.
The “great recession” that officially began in December 2007 and ended in June 2009 offers an unusual opportunity to examine how U.S. general hospitals adjust in the short-run to increases in psychiatric bed need. Recessions are associated with increases in psychiatric inpatient admissions, a relationship that has been repeatedly demonstrated in various time periods and geographic areas of the U.S. and in several foreign countries (Catalano and Hartig 2004). Job losses and other income losses during recessions may result in greater levels of psychological distress, and consequently in greater help seeking at hospitals (Brenner 1967); financial and other in-kind or intangible supports for community living among disabled persons with serious mental illnesses may also contract during recessions, and, consequently, hospitalizations may increase (Brenner 1967). Whichever mechanisms are involved, the dramatic doubling of unemployment that occurred during the great recession provides a natural experiment that can be exploited to understand how increases in psychiatric inpatient admissions may affect hospitals’ bed utilization practices.
This study examines how changes between calendar years 2007 and 2010 in psychiatric inpatient admissions affected length-of-stay and over-capacity use of specialized psychiatric beds, using panel data for a sample of U.S. general hospitals drawn from the nationwide inpatient sample (NIS) (Agency for Healthcare Research and Quality 2013a). A psychiatric bed occupancy rate, defined as the ratio a hospital’s total psychiatric inpatient days in a month to the hospital’s total potential number of specialized psychiatric care beds days in a month, was used to define psychiatric bed occupancy greater than 100 %. This measure of over-capacity bed use was interpreted as a proxy indicator of scatter bed use. Scatter bed use is not directly identified in NIS databases and is rarely identified in other national databases, a data limitation that has impeded research on access to psychiatric beds. The study hypotheses were that increases in psychiatric admissions resulted in lower average length-of-stay and a greater probability that the psychiatric bed occupancy rate exceeded one.
Hypothesis test statistics were estimated using fixed effects (FE) and fixed effects instrumental variables (FE-IV) models. FE models were used to remove the cross-sectional variation in hospitals’ length of stay and bed occupancy levels, which may be spuriously correlated with total admissions. In the FE-IV models, the change in the state unemployment rate was used as an instrumental variable for the change in hospitals’ psychiatric admissions. This approach exploits exogenous unemployment shocks to estimate the impacts of increased psychiatric admissions on psychiatric length-of-stay and bed occupancy.
Methods
Modeling Approach
The basic model of psychiatric inpatient length-of-stay and bed occupancy was:
where y it indicates values of the dependent variable for hospital i at month t, x is a set time-invariant characteristics applicable to hospital i (e.g., size, geographic region, urban/rural location, managed care involvement), A it indicates the number of admissions, c i captures unmeasured time-invariant hospital heterogeneity, u it indicates a mean-zero error term, and b1, b2, and δ1 are parameters to be estimated.
c i in Eq. 1 may be correlated with A, and, consequently, regression estimation of Eq. 1 may result in biased estimates of b2. To remove this source of bias, a mean-transformed version of Eq. 1 was estimated:
where is the μy(i) is the mean of y i with respect to t; μ A(i) is the mean of A i with respect to t; and all other variables and parameters are the same as in Eq. 1. Equation 2 is the fixed effects (FE) “within” estimation model (Wooldridge 2002). The within estimator is implemented by replacing the two means μy(i) and μ A(i) with their sample analogs, \(\overline{{y_{\text{i}} }}\) and \(\overline{{A_{\text{i}} }}\). The chief advantage of Eq. 2 compared to Eq. 1 is that Eq. 2 does not contain c i.
Estimates of b2 obtained from regression estimation of Eq. 2 may still be biased if A it − \(\overline{{A_{\text{i}} }}\)is correlated with unmeasured determinants of y it − \(\overline{{y_{\text{i}} }}\) (i.e., if changes in admissions are “endogenous”). For example, hospitals’ decisions about increases in admissions could be affected by trends in occupancy levels or length-of-stay. As a result, Eq. 2 was also estimated using a fixed-effects instrumental variables (FE-IV) regression approach, in which A it − \(\overline{{A_{\text{i}} }}\) was treated as an endogenous right-hand-side variable. To implement the FE-IV model, an equation for A it − \(\overline{{A_{\text{i}} }}\) was specified as:
where N it is the unemployment rate in hospital i’s state at time t; \(\overline{{N_{\text{i}} }}\) is the mean of the unemployment rate with respect to t; and π 0 and π 1 are parameters to be estimated. In Eq. 3, the change in the unemployment rate was used as an instrumental variable for the change in admissions (A it − \(\overline{{A_{\text{i}} }}\)). Change in the unemployment rate may be considered an exogenous influence on changes in admissions, because increases in unemployment during this period were being driven by recessionary factors.
For the FE-IV model, Eqs. 2 and 3 were estimated jointly using mixed effects instrumental variables regression, which allowed for a common covariance across observations for the same hospital. Although the FE estimates are biased and inconsistent if admissions are endogenous to bed occupancy while FE-IV estimates are always consistent, FE estimates are more efficient than FE-IV estimates. Consequently, when the two methods produce similar estimates, the more efficient FE estimates are preferred and when the two methods produce different estimates, the consistent FE-IV estimates are preferred. A Hausman test was used to test the hypothesis of no differences between FE and FE-IV estimates. A rejection of this hypothesis indicated preference for the FE-IV estimates (Hausman, 1978). All models were estimated using Stata.
Data and Sample
Hospital-level data on psychiatric inpatient utilization at community hospitals with specialized psychiatric beds were developed from the 2007–2010 nationwide inpatient sample (NIS) database (Agency for Healthcare Research and Quality 2013a). NIS data are fully de-identified, and the study was determined not human subjects research (NHSR) by [the authors’ university] Institutional Review Board. The NIS includes censuses of essentially all hospital stays for a representative sample of hospitals in 37 states. HCUP databases have been extensively checked for consistency, and uniform data fields are created to facilitate analysis of data spanning multiple states and years. Data on hospitals’ numbers of specialized psychiatric beds (i.e., beds in distinct part psychiatric units), which were needed to operationally define psychiatric bed occupancy, were obtained from a separate database provided by the American Hospital Association (AHA), and then matched to NIS data using AHA ID numbers.
Of the 1,051 hospitals represented in the NIS data, 437 had no AHA ID. Of the remaining 614 hospitals, 595 were identified as general hospitals. Of these, 439 had specialized psychiatric beds. Compared to other hospitals in the NIS sample, these hospitals were more likely to be large (55 % versus 27 % among excluded hospitals; p < .001), urban (79 % vs. 55 % among excluded hospitals; p < .001), teaching hospitals (44 % vs. 13 % among excluded hospitals; p < .001), and they were more likely to be located in the Northeast census region (39 % vs. 10 % among excluded hospitals; p < .001). These hospitals yielded a panel of (N = 7,381) monthly observations.
Measures
Hospital-level monthly measures included total psychiatric inpatient admissions, psychiatric length-of-stay, psychiatric bed occupancy, and psychiatric bed occupancy greater than 1. Psychiatric inpatient admissions were identified as inpatient records with a principal discharge diagnosis corresponding to a mental health or substance use condition. NIS uses the clinical classification software (CCS) to classify International Classification of Disease Version 9 (IC9-9) codes into categories corresponding to mental health and substance abuse conditions (Agency for Healthcare Research and Quality, 2013b). The CCS mental health and substance abuse categories (CCS 601-670) encompass all ICD-9 codes 290-319 plus additional codes for other miscellaneous mental disorders and problems (648.4, V40.2, V40.3, V40.9, V67.3), delirium, dementia and other cognitive limitations (331.0, 331.1, 331.2, 331.8, 797), other developmental problems (V40.0, V40.1), screening and history of mental health and substance abuse problems (333.92, 357.5, 425.5, 535.3, 571.0-571.3, 790.3, V11.0-V15.8, V62.85, V66.3, V70.1, V70.2, V71.09, V79.0-V79.3, V79.8, V79.9), other alcohol- and drug-related disorders (648.3-648.4, 655.5, 760.7, 779.5, 965.5, 980.0, V65.42), and suicidal behaviors, suicide attempts, and intentional self-inflicted injuries (E950-E959, V628). Psychiatric length-of-stay in days was obtained directly from the NIS.
NIS data do not delineate psychiatric admissions to scatter beds from psychiatric admissions to beds in specialized psychiatric units. Consequently, psychiatric admissions encompassed both types of beds. As noted earlier, the psychiatric bed occupancy rate for each hospital and month was defined as the ratio of total psychiatric inpatient days to the number of specialized psychiatric beds multiplied by 30. A psychiatric bed occupancy rate greater than one (i.e., psychiatric bed use exceeding full capacity) was interpreted as an indicator of scatter bed use. This indicator may underestimate actual scatter bed use (i.e., it may not be sensitive to changes) because it is based on the implicit assumption that hospitals only use scatter beds when their specialized psychiatric beds are more than 100 % full. In actuality, hospitals may use scatter beds even when their specialized psychiatric beds are less than full, in order to maintain spare psychiatric bed capacity for new admissions that require the level of security and monitoring that specialized psychiatric units provide.
FE-IV regression models required information on the state monthly unemployment rate. These data were obtained from the Bureau of Labor Statistics. FE and FE-IV regression models were also adjusted for calendar years in order to delineate any longer-term trend in length-of-stay or bed occupancy rates from the shorter-term impacts of unemployment shocks. All of these variables were demeaned prior to analysis, in accordance with the approach, as discussed above.
Results
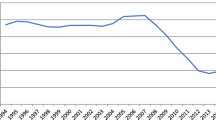
Table 1 shows sample means for key variables, and Fig. 1 shows monthly trends from 2007 to 2010. The monthly data in Fig. 1 were smoothed using a moving average filter, which averages the observations adjacent to the observation for each month. Trends for psychiatric admissions (Fig. 1a) and bed occupancy (Fig. 1b) appear to be positively associated with the unemployment rate, whereas the trend for length-of-stay appears to be negatively correlated with the unemployment rate. Over the four-year period, the fraction of hospitals with a psychiatric bed occupancy rate greater than one increased from approximately .22 to approximately .25. Meanwhile, mean length-of-stay decreased moderately from 6.97 days per stay to 6.89 days per stay.
Table 2 shows the 12-month average changes in hospitals’ psychiatric admissions, psychiatric bed occupancy rate, and average length-of-stay (LOS) stratified by their occupancy rate quintile at the baseline period. Hospitals with occupancy rates in the first quintile (i.e., those with occupancy rates less than .55) on average experienced increases in admissions (+3.3), occupancy rate (+.04), and mean length-of-stay (+.41 days), while hospitals with baseline occupancy rates in the fourth and fifth quintiles experienced decreases in admissions, occupancy rate, and mean length-of-stay. Hospitals in the second and third quintiles had mixed trends. The last row of the table shows the correlations (ρ) between starting occupancy rate and trends in admissions, occupancy, and length-of-stay. Greater starting occupancy rates were negatively correlated with the 12-month changes in admissions (ρ = −.24, p < .001), occupancy rate (ρ = −.39, p < .001), and mean length-of-stay (ρ = −.18, p < .001).
Table 3 shows regression estimates of Eq. 2 for the likelihood that hospitals had a psychiatric bed occupancy rate greater than one. The FE estimates indicate that an increase of 10 psychiatric admissions per month was associated with a .043 increase in the likelihood that a hospital had a bed occupancy rate greater than one.0 (z = 24.9, p < .001, 95 % CI .038–.046). The IV-FE estimate of coefficient on admissions was .053 (95 % CI .006–.101) and statistically significant (z = 2.2, p = .028). Year effects were not statistically significant in either model. A Hausman test of the hypothesis that the IV-FE coefficient estimates were the same as the FE estimates was not rejected (Χ2 (4) = .2, p = .995).
Both the FE and the FE-IV regression estimates for mean length-of-stay (Table 4) indicate that increases in admissions were associated with decreases in psychiatric length-of-stay. The FE estimates indicate that an increase of 10 psychiatric admissions per month was associated with a decrease in mean length-of-stay of .178 days (z = 16.0, p < .001, 95 % CI −.199, −.156). The IV-FE point estimate of this same coefficient was .332 (z = 2.1, p = .037, 95 % CI −.645, −.019). Year effects were not statistically significant in either model. The hypothesis that the IV-FE coefficient estimates differed from FE estimates was not rejected (Χ2 (4) = .9, p = .918).
Discussion
Use of scatter beds for psychiatric inpatient stays may have increased and length-of-stay may have decreased as a result of increased psychiatric admissions to general hospitals during the great recession. An increase of 10 psychiatric admissions per month, which represents approximately a 10 percent increase, was associated with a 4.3 percentage point increase in the probability of the proportion of hospitals with psychiatric inpatient units exceeding 100 % bed occupancy (z = 24.9, p < .001, 95 % CI .038–.046) and with a decrease in mean length-of-stay of .178 days (z = 16.0, p < .001, 95 % CI −.199, −.156). These results were confirmed in instrumental variables models that used only changes in the unemployment rate to identify the impacts of changes in psychiatric admissions. This suggests that changes in admissions had a causal influence, as there is no reason to expect that changes in the unemployment rate directly affect psychiatric bed occupancy or length-of-stay.
The study’s findings suggest that general hospitals may dynamically adjust scatter bed use and length-of-stay in response to changes in psychiatric bed capacity or bed need in their service area. More generally, this implies that a bed “shortage” (or a “surplus”) may be understood as a local area dis-equilibrium phenomenon that is resolved, for better or for worse, through adjustments in patient volume, psychiatric bed capacity, scatter bed use, and length-of-stay until a new equilibrium between these various factors is reached. This re-interpretation of shortages does not preclude the possibility of inpatient bed unavailability and attendant negative consequences (e.g., Lamb and Weinberger 2005). However, it implies that most local bed shortages are transitory unless hospitals cannot adjust due to other constraints, such as a regulatory mandate that imposes a minimum length-of-stay. Besides regulatory mandates, other potential constraints on adjustment could include an already high occupancy rate in general medical beds, a local area shortage of hospital psychiatric staff (e.g., social workers and psychiatric nurses), or delays in access to outpatient mental health services. Consequently, persistent shortages may be characterized by strained capacity on multiple fronts (e.g., staffing and local area hospital bed occupancy).
In addition to length-of-stay and scatter bed use, hospitals could respond to a local area psychiatric bed shortage by making their clinical inpatient admission criteria more stringent. Such a process change would tend to reduce the volume of psychiatric inpatient admissions, albeit with potentially negative consequences for patients. Whether hospitals in fact adjust admission criteria in response to bed shortages is unknown to us, and the data used in this study provide no information about admission criteria or their use. Moreover, previous research on the contextual factors that influence psychiatric inpatient admission decisions (e.g., Unick et al. 2011) does not directly address this issue. This would seem to be a significant question for future research.
This dynamic model of hospital adjustment is consistent with counter-intuitive findings from a recent study of an urban public-sector hospital that eliminated half its psychiatric beds (Shumway et al. 2012). Despite this drastic reduction, no evidence of anticipated adverse consequences, such as increased demand for psychiatric emergency services, decreased access to emergency or inpatient services, increased recidivism to inpatient care, or increased levels of inadequately treated mental illness in the community, was found. Moreover, this was not a case of underutilized capacity. The hospital’s psychiatric inpatient service had been operating at full capacity prior to the bed reductions. The authors conclude that “strategic efforts to reduce inpatient length of stay were a key factor” in preventing potential negative impacts of service changes (Shumway et al. 2012). Inpatient length-of-stay was reduced over the study period by almost one-third, making it possible to serve the same number of patients with fewer beds. A key strategy involved initiating collaborative discharge planning soon after patients were admitted rather than waiting until they were ready for discharge.
Hospital adjustments to increased admissions could also have contributed to the long-term decline in psychiatric inpatient length-of-stay that has continued since the 1990’s. Between 1997 and 2011, psychiatric inpatient length-of-stay has declined from 8.0 days per stay to 7.3 days per stay (HCUPnet, 2014). During this same period, general hospitals have experienced a substantial (23 %) increase in psychiatric inpatient admissions (HCUPnet, 2014) and a reduction in psychiatric beds (National Center for Health Statistics, 2012). These changes may have contributed to psychiatric bed shortages (Alakeson et al. 2010) and lengthy emergency department visit durations in some communities (Chang et al. 2012; Slade et al. 2010). However, results from previous research suggests that hospitals also may have accelerated discharges by beginning the discharge planning process soon after admission and by more proactively coordinating a discharge with outpatient programs (Shumway et al. 2012). Any future increases in psychiatric bed need would be expected to result in further changes in hospitals’ inpatient management practices, which may imply further reductions in psychiatric inpatient length-of-stay.
Several limitations of the study data may affect the interpretation and generalizability of this study’s results. A key limitation is that scatter bed use was not identifiable in the data. Although scatter bed use can be identified in some insurance claims databases, using revenue codes (Mark et al. 2010), such codes are generally not available in the NIS and in other national databases. As a result, the validity of the inference that scatter bed use increased in response to increased admissions depends on an unverified correspondence between having a psychiatric bed occupancy rate greater than one and scatter bed use. Whereas a psychiatric bed occupancy rate greater than one logically implies use of non-psychiatry beds, a rate less than one does not imply zero scatter bed use. Scatter beds may be used even when psychiatric units are less than 100 % full. Thus, scatter bed use may be underestimated in this study.
A second data limitation is that the study sample is not representative of U.S. hospitals. Compared to the full NIS sample, which is nationally representative, the hospitals included in the study sample were disproportionately large, urban, teaching hospitals, and hospitals in the Northeast census region. This in part reflects the characteristics of hospitals that have specialized psychiatric care units and that serve persons with serious and persistent mental illness living in and around cities. However, it also reflects missing AHA identifiers for some hospitals. As a result, these results may or may not generalize to smaller, rural, and non-teaching hospitals.
Another feature of the results that may affect their interpretation is that changes in bed occupancy and length-of-stay were small to moderate in magnitude. Over the four-year study period, the fraction of hospitals with a psychiatric bed occupancy rate greater than one increased from 22 to 25 % while mean length-of-stay decreased only .08 days (or 1 %), from 6.97 days per stay to 6.89 days per stay. These effects are averages across a sample of hospitals, only some of which had a high bed occupancy rate at the start of the period. Consequently, although marginal effects at particular hospitals could have been larger and more consequential, the average pattern suggests that hospitals’ adjustments to scatter-bed use and psychiatric length-of-stay were incremental.
A final consideration is that no information was available on care denials or other administrative barriers to inpatient admission. As discussed earlier, such administrative barriers could be used by hospitals to regulate admissions. Consequently, care denials could have insulated hospitals from even larger increases in admissions than they experienced and might be correlated with length-of-stay. This is addressed within the empirical framework through the use of the “within” estimator and the instrumental variables method. The within estimator removed unmeasured cross-sectional differences among hospitals, which might have reflected unmeasured differences in the rate of care denials, but did not address unmeasured changes in care denials over time. Such unmeasured changes were addressed by the instrumental variables estimates, which were identified solely by changes in the unemployment rate. Consequently, the study’s results are unlikely to have been influenced by omitted information on care denials.
Conclusions
This study found evidence that increases in psychiatric inpatient admissions resulted in moderate increases in the proportion of hospitals with psychiatric inpatient units exceeding 100 % bed occupancy, which may reflect an increase in the use of scatter beds. This study also found small reductions in psychiatric inpatient length-of-stay in response to increases in psychiatric inpatient admissions. These responses suggest that general hospitals dynamically adjust utilization of general medical and specialized psychiatric beds in response to changes in psychiatric bed capacity or bed need in their service area. More generally, this implies that a local bed shortage may be understood as a dis-equilibrium phenomenon that is resolved through adjustments in patient volume, psychiatric bed capacity, scatter bed use, and length-of-stay until a new equilibrium between these various factors is reached. Thus, shortages are likely to be local and transitory barring other constraints on hospital adjustment.
References
Agency for Healthcare Research and Quality (2013a). Overview of the nationwide inpatient sample (NIS), healthcare cost and utilization project (HCUP). from www.hcup-us.ahrq.gov/nisoverview.jsp. Retrieved 11 Nov 2013.
Agency for Healthcare Research and Quality (2013b). HCUP clinical classifications software (CCS) for ICD-9-CM, healthcare cost and utilization project (HCUP). from www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. Retrieved 11 Nov 2013.
Alakeson, V., Pande, N., & Ludwig, M. (2010). A plan to reduce emergency room ‘boarding’ of psychiatric patients. Health Affairs, 29(9), 1637–1642.
American College of Emergency Physicians (2008). ACEP psychiatric and substance abuse survey 2008. from http://www.acep.org/uploadedFiles/ACEP/Advocacy/federal_issues/PsychiatricBoardingSummary.pdf. Retrieved 1 May 2009.
Baraff, L. J., Janowicz, N., & Asarnow, J. R. (2006). Survey of California emergency departments about practices for management of suicidal patients and resources available for their care. Annals of Emergency Medicine, 48(4), 452–458.
Brenner, M. H. (1967). Economic change and mental hospitalization: New York State, 1910–1960. Social Psychiatry, 2(4), 180–188.
Catalano, R., & Hartig, T. (2004). Economic predictors of admissions to inpatient psychiatric treatment in sweden. Social Psychiatry and Psychiatric Epidemiology, 39(4), 305–310.
Chang, G., Weiss, A. P., Orav, E. J., Smallwood, J. A., Gonzalez, S., Kosowsky, J. M., et al. (2012). Bottlenecks in the Emergency Department: the psychiatric clinicians’ perspective. General Hospital Psychiatry, 34, 403–409.
Hausman, J. A. (1978). Specification tests in econometrics. Econometrica, 46, 1251–1271.
Lamb, H. R., & Weinberger, L. E. (2005). The shift of psychiatric inpatient care from hospitals to jails and prisons. Journal of the American Academy of Psychiatry Law, 33, 529–534.
Mark, T., Vandivort-Warren, R., Owens, P., Buck, J., Levit, K., Coffey, R., et al. (2010). Psychiatric discharges in community hospitals with and without psychiatric units: How many and for whom?. Psychiatric Services, 61(6), 562–568.
National Center for Health Statistics (2012) Health, United States, 2011: Table 117. Mental health organizations and beds for 24-hour hospital and residential treatment, by type of organization. Hyattsville, MD. http://www.cdc.gov/nchs/hus/contents2011.htm#117. Accessed 4 Sept 2013.
Sharfstein, S. S., & Dickerson, F. B. (2009). Hospital psychiatry for the twenty-first century. Health Affairs, 28(3), 685–688.
Shumway, M., Alvidrez, J., Leary, M., Sherwood, D., Woodard, E., Lee, E. K., et al. (2012). Impact of capacity reductions in acute public-sector inpatient psychiatric services. Psychiatric Services, 63(2), 135–141.
Slade, E. P., Dixon, L. B., & Semmel, S. (2010). Trends in the duration of emergency department visits, 2001–2006. Psychiatric Services, 61(9), 878.
Torrey, E. F., Entsminger, K., Geller, J., Stanley, J., & Jaffe, D. J. (2008). The shortage of public hospital beds for mentally ill persons. Arlington, VA: Treatment Advocacy Center.
Unick, G. J., Kessell, E., Woodard, E. K., Leary, M., Dilley, J. W., & Shumway, M. (2011). Factors affecting psychiatric inpatient hospitalization from a psychiatric emergency service. General Hospital Psychiatry, 33(6), 618–625.
Wooldridge, J. M. (2002). Econometric analysis of cross section and panel data. Cambridge, MA: The MIT Press.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Slade, E.P., Goldman, H.H. The Dynamics of Psychiatric Bed Use in General Hospitals. Adm Policy Ment Health 42, 139–146 (2015). https://doi.org/10.1007/s10488-014-0554-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10488-014-0554-4