Abstract
Youth life satisfaction is a component of subjective well-being, an important part of a strengths-based approach to treatment. This study establishes the psychometric properties of the Brief Multidimensional Students’ Life Satisfaction Scale—PTPB Version (BMSLSS-PTPB). The BMSLSS-PTPB showed evidence of construct validity with significant correlations as expected to measures of youth hope and youth symptom severity, and no relationship as expected to youth treatment outcome expectations. A longitudinal analysis was conducted examining the relationship between youth-reported life satisfaction and mental health symptom severity (youth-, caregiver-, and clinician-report) for 334 youth (aged 11–18 years) receiving in-home treatment. Results indicated that life satisfaction consistently increased over the course of treatment but increased faster in youth whose symptom severity, as rated by all reporters, decreased over the course of treatment. Implications, future directions, and limitations of the study are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Over the last decade, there has been an increased focus on the importance of assessing life satisfaction in children and adolescents receiving mental health treatment. This emphasis supports efforts aimed at improving quality of life for youth served in several settings and balances a deficit or symptom-based approach by focusing on building optimal functioning for youth. Global life satisfaction has been defined as a cognitive aspect of subjective well-being consisting of “a global evaluation by the person of the quality of his or her life” (Pavot et al. 1991 p. 150). In addition to global life satisfaction, specific domains of life satisfaction can be assessed (e.g., satisfaction with family life or school) to provide a multi-contextual profile of well-being (Seligson et al. 2003). Notably, it is theorized that life satisfaction is considered to be more than a byproduct of life experiences or events, with some evidence that internal mechanisms (e.g., perceptions) have greater influence on life satisfaction than objective conditions (e.g., parents’ marital status, socioeconomic level) and demographic variables (e.g., age and gender; Gilman and Huebner 2003). Life satisfaction is hypothesized as a crucial factor that influences positive functioning in a cycle that is reciprocal and mutually reinforcing (Fredrickson 2001; Huebner 2004).
Recent reviews of child and adolescent research (Gilman and Huebner 2003; Huebner 2004; Proctor et al. 2009; Suldo et al. 2006) indicate that youth life satisfaction is not only linked with physical and mental health status but also relates to broader measures of well-being such as school engagement and academic achievement. For example, a recent longitudinal study of middle school-aged youth found a bidirectional relationship between life satisfaction and school engagement (Lewis et al. 2011). Specifically, higher life satisfaction predicted a greater belief that school is important to one’s future at five months and similarly, greater belief that school is important predicted higher life satisfaction in the same time period.
Further, it has been suggested that high life satisfaction is necessary, but not sufficient, for positive mental health (Diener et al. 1999). Cross-sectional studies of both subjective well-being (which includes life satisfaction) and emotional or behavioral problems in youth have found that both are correlated with various indicators of positive functioning such as physical health, social functioning, and academic adjustment (Greenspoon and Saklofske 2001; Suldo and Shaffer 2008). A recent longitudinal study found that subjective well-being may serve as a protective factor even in the face of high levels of psychopathology. While youth with low subjective well-being and high psychopathology had poorer academic outcomes at follow-up one year later, those with high levels of both subjective well-being and psychopathology demonstrated similar grade point averages over time to youth without high psychopathology (Suldo et al. 2011). Although psychopathology and life satisfaction are related, life satisfaction has been distinguished from psychopathology as measuring a different construct (Huebner 2004).
Such findings provide support for the growing trend to incorporate a strengths-based approach in youth mental health treatment by incorporating assessment and intervention aimed both at reducing symptoms and at building strengths, such as life satisfaction (Maddux 2005; Seligman and Csikszentmihalyi 2000). The present longitudinal study explores the relationship between youth life satisfaction and change in severity of symptoms over time for youth receiving home-based treatment. It was hypothesized that improvement in youth life satisfaction would correspond to improvement in symptom severity over time. In addition to youth symptom severity, analytic models in the current study examine several objective correlates of youth life satisfaction, including spirituality-related attributes (e.g., Sawatzky et al. 2009), youth substance use (e.g., Becker et al. 2009; Farhat et al. 2011), youth age and gender, caregiver marital status (e.g., Kwan 2010; Piko and Hamvai 2010), and caregiver emotional stress (Powdthavee and Vignoles 2008).
In addition to the longitudinal study, a psychometric evaluation of the Brief Multidimensional Students’ Life Satisfaction Scale—PTPB Version (BMSLSS-PTPB) was conducted. The BMSLSS-PTPB is a brief youth self-report instrument that is included in the Peabody Treatment Progress Battery (PTPB; Bickman et al. 2010) as an indicator of treatment progress. Of note, the BMSLSS-PTPB is intended for frequent use throughout the course of treatment to inform clinicians about youth’s current life satisfaction, as well as any changes that occur throughout treatment. This information may be important to incorporate into treatment.
Method
Participants
Participants were drawn from a larger longitudinal cluster randomized experiment evaluating the effects of a measurement feedback system (Contextualized Feedback Systemstm) on mental health outcomes for youth receiving "treatment as usual" from a large national provider of home-based mental health services (Bickman et al. 2011 ). For the longitudinal study, criteria for inclusion of youth from the larger evaluation sample consisted of youth beginning treatment during the two-and-a-half year data collection period and having at least one valid (defined as having at least 85% non-missing data) BMSLSS-PTPB measure. This resulted in a sample of 334 youths aged 11–18 years (M = 14.7, SD = 2.6) that was 51% male. The racial breakdown was as follows: 55% Caucasian, 26% African American, 12% more than one race, and 17% other (e.g. Asian, American Indian, Native Hawaiian, etc.). Data for the psychometric evaluation were gathered from an additional 360 youths from the same large mental health provider who participated in an earlier study conducted to establish the psychometric properties of the measures used for the evaluation. This resulted in a total of 694 youth aged 11–18 (M = 14.7, SD = 2.6), 52% of which were male. Within the psychometric sample, 53% of youth were Caucasian, 27% African American, 12% more than one race, and 8% other (e.g. Asian, American Indian, Native Hawaiian, etc.). For youth in the psychometric sample with more than one completed BMSLSS-PTPB measure, only the first was used. All study procedures were approved by the Institutional Review Board of Vanderbilt University. For more information concerning the participants and the difference between these two samples, please see Riemer et al. (2012) in this issue.
Due to the nature of the larger evaluation study, which was conducted in real-world treatment settings, the number of completed BMSLSS-PTPB measures for each youth in the longitudinal sample varied. This was due to differences in treatment session frequency, invalid measures (less than 85% complete), and missing measures (incomplete for a variety of reasons, such as youth refusing to complete, youth not being present at a session, clinician failing to provide the measure to youth for completion, etc.). Of the total sample of 344 youths, 39% completed only one BMSLSS-PTPB measure, 28% completed two, and 32% completed three or more. All data were included in the longitudinal analysis. Youth in the longitudinal sample were in treatment for an average of 3.84 months (SD = 3.05) from their baseline assessment to their last measurement point.
Measures
Youth Life Satisfaction
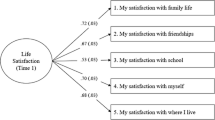
Youth satisfaction with life was assessed with the Brief Multidimensional Students’ Life Satisfaction Scale—PTPB Version (BMSLSS-PTPB). This measure represents a revision of the BMSLSS (Seligson et al. 2003) in which the original seven-point Likert-type response scale (ranging from ‘Terrible’ to ‘Delighted’) was changed. Item response theory (IRT) analysis from a previous psychometric study (Bickman et al. 2007) indicated that some response alternatives were not distinct. As a result, responses on the BMSLSS-PTPB are given on a five-point likert-type scale (ranging from ‘Very dissatisfied’ to ‘Very satisfied’). In addition, some questions and item stems from the original version were modified for clarity. The BMSLSS-PTPB measures life satisfaction using six youth-appropriate items, one of which measures overall life satisfaction. The other five items measure satisfaction in specific life domains: family life, friendships, school experience, self, and where the youth lives. The BMSLSS-PTPB has previously demonstrated sound psychometric qualities (Bickman et al. 2007). Items are averaged together resulting in a BMSLSS-PTPB Total Score, that represents overall life satisfaction. BMSLSS-PTPB Total Scores range from 1 to 5, with higher scores indicating greater life satisfaction. Suggested administration is at baseline and every 2 weeks, or at least once per month during treatment so that changes in a specific domain or overall life satisfaction can be reliably assessed.
Youth Mental Health Symptoms and Functioning
The Symptoms and Functioning Severity Scale (SFSS: Bickman et al. 2010) is completed by the youth, caregiver, and clinician. Composed of 26 five-point Likert-type items (27 for the clinician version), it yields a Total Score representing global symptom severity as well as subscale scores for internalizing and externalizing symptom severity. The SFSS has demonstrated sound psychometric qualities for all three respondent forms including internal consistency (range: α = 0.93–0.94), test–retest reliability (range: r = 0.68–0.87), construct validity, and convergent and discriminant validity. For this study, only the SFSS Total Scores for each respondent were used. See Athay et al. (2012) in this issue for more information on the SFSS.
Youth Hope
Youth hopefulness was measured using the Children’s Hope Scale—PTPB Edition (CHS-PTPB). The CHS-PTPB is composed of six items and assesses the youth’s beliefs in his or her ability to achieve goals and sustain movement toward these goals. The CHS-PTPB demonstrates adequate psychometric properties including internal consistency of α = 0.84. For more information on the CHS-PTPB, see Dew-Reeves et al. (2012) in this issue.
Youth Treatment Outcome Expectations
The Treatment Outcome Expectations Scale (TOES) is an eight-item measure that assesses caregiver and youth expectations about what will happen in the future as a result of youth counseling. Respondents use a three-point Likert-type scale ranging from one ('I do not expect this') to three ('I do expect this') to respond to items indicating possible positive consequences of participating in treatment. The TOES Total Score represents the mean of the responses across all eight items and is calculated for each informant. Both the youth and caregiver TOES display sound psychometric properties including adequate internal consistency (α = 0.91, 0.85 respectively).The youth version is utilized in the current study. For more information on the TOES, see Dew-Reeves and Athay (2012) in this issue.
Youth and Caregiver Characteristics
As part of the initial baseline assessment for the larger evaluation study, the youth, caregivers, and clinicians completed background questionnaires. The background form completed by youth consisted of 14 items about their demographic profile (e.g., gender, age, ethnicity), problems with school (e.g., suspensions), involvement with juvenile justice (e.g., arrests), and spirituality (e.g., religious preference, importance of religion or spirituality). The background form completed by caregivers consisted of 21 items about the youth’s and their own demographic profile (e.g., marital status, household income), their own spirituality, and their own mental health history. The baseline assessment completed by clinicians consists of 14 items pertinent to the youth’s presenting problems, treatment history, referral information, and whether a diagnosis was noted by the clinician in the baseline assessment. For this study, several individual items were used as covariates in the longitudinal analysis: youth importance of religion/spirituality for helping with thoughts, feelings, or behavior; caregiver current marital status; caregiver history of emotional, behavioral, alcohol, or drug use problem; and clinician indication of one or more diagnoses for youth and indication of youth use of drugs or alcohol.
Procedures
For the larger evaluation study, all measures were completed throughout the course of treatment as part of the larger battery of PTPB measures used to assess youth treatment progress (e.g., symptom severity) and treatment process (e.g., therapeutic alliance). Measures were administered using paper- and pencil-forms at the close of treatment sessions. The BMSLSS-PTPB was scheduled for administration at baseline, every other week throughout treatment, and at discharge. The SFSS was administered on the same schedule. However, the BMSLSS-PTPB and SFSS were on an alternating week schedule; thus, they were not administered at the same time. The CHS-PTPB was administered at baseline and once a month throughout treatment. The TOES was administered at baseline only. Completed measures were entered into the CFS application by administrative staff at the treatment sites.
For the longitudinal analyses, multiple imputations (MI) were used to treat missing data from the SFSS and background questionnaires. Following procedures suggested by McKnight et al. (2007), missing data across subjects and variables were inspected and no discernable patterns of missingness were found that would indicate that data were not missing at random (non-MAR). Established guidance is that five imputations are desirable for MI procedures (Rubin, 1987; von Hippel, 2005). Thus, missing data were treated as MAR and five imputed data sets were created to use separately for analyses. Averaged results are presented.
Analyses
Psychometric Analyses
The psychometric properties of the BMSLSS-PTPB were evaluated using methods from classical test theory (CTT), confirmatory factor analysis (CFA) and IRT. This approach yielded information about the psychometric qualities of individual items and the overall scale. CTT and CFA analyses were conducted with SAS® version 9.2 software, while IRT analyses utilized WINSTEPS 3.36.0 (Linacre 2007). For more detailed information about the approach to psychometric analysis, see Riemer et al. (2012) in this issue.
Within CTT, characteristics of each item were inspected to assess its distributional characteristics and the item’s relationship to the BMSLSS-PTPB Total Score. Summary statistics and the internal consistency reliability (i.e., Cronbach’s alpha) of the BMSLSS-PTPB Total Score were also examined. The correlations between each item and the BMSLSS-PTPB Total Score were examined to identify items that were unrelated to the overall measure.
The BMSLSS-PTPB was developed as a unidimensional scale to assess youth satisfaction with life. To confirm this factor structure, CFA was applied to the data to ensure that all items loaded onto a single latent variable. Fit indices including Bentler's Comparative Fit Index (CFI), Joreskog Goodness of Fit Index (GFI), and Standardized Root Mean Square Residual (SRMR) were used to determine how well data fit with this proposed model Indices were compared to commonly acceptable standards (i.e. > 0.90 for GFI and SRMR, < 0.05 for Bentler CFI).
The IRT Rating Scale Model (RSM: Andrich 1978) was used in the current paper. Application of the RSM yields item difficulty ratings and item fit statistics (infit and outfit). Using a logit scale, item difficulties indicate where an item most accurately estimates the level of life satisfaction. Fit statistics quantify how well each item fits with the proposed model. WINSTEPS 3.63.0 (Linacre 2007) also provides an estimate of item discrimination, that is each item’s ability to differentiate between youth with high and low life satisfaction.
Construct validity refers to the degree that we are measuring the construct we think we are measuring. Here, construct validity is assessed based on how well this measure correlates with variables known to be related or unrelated to youth life satisfaction. Reviews of the literature consistently find a relationship between life satisfaction and symptom severity (e.g., see Huebner 2004). Therefore, we expect to find a significant correlation between the BMSLSS-PTPB and the SFSS. A relationship between life satisfaction and youth hope was also reported in a recent review (Proctor et al. 2009). Given this, we also expect to find a significant correlation between the BMSLSS-PTPB and the CHS-PTPB. However, given that the SFSS and CHS-PTPB are not measuring the same construct as life satisfaction, we expect these correlations to be moderate. In addition, no research was found showing a relationship between life satisfaction and treatment outcome expectations. Therefore we expect to find a non-significant relationship between the BMSLSS-PTPB and the TOES.
Longitudinal Analyses
Longitudinal analyses employed hierarchical linear modeling (HLM) using HLM 6 computer software (Raudenbush et al. 2004). HLM is the most appropriate analytic technique for the current data for two primary reasons. First, multiple observations (i.e., multiple BMSLSS-PTPB data points) per youth were used. HLM avoids violating the assumption of independence by taking this data structure into account where there are multiple data points nested within individuals. In this way, hierarchical analyses describe variability in individual youth trajectories of life satisfaction and allow for simultaneously estimating the influence of variables from different levels (i.e., between- and within-youth effects) and the cross-level interactions of these variables on the dependent variable, youth symptom severity (Raudenbush and Bryk 2002). Second, HLM does not require an equal number or spacing of observations per youth, which accommodates the unequal number of BMSLSS-PTPB observations across youth.
The growth models used consist of two levels: a Level-1 model (within-youth) and a Level-2 model (between-youth). The within-youth model allows for the estimation of various parameters of growth, such as initial level of life satisfaction and rate of change in each youth. The between-youth model allows for the examination of mean rate of change for all youth as well as youth correlates of initial life satisfaction and change. To test the primary hypothesis that improvement in life satisfaction would correspond to the improvement of youth’s symptom severity, the recommendations of Singer and Willet (2003) were followed. Therefore, symptom severity was separated into two components: a time-invariant component (i.e., youth symptom severity at baseline: SFSSba) and a time-varying component (i.e., changes in symptom severity from baseline: SFSSch). Baseline severity was grand-mean centered so that information was obtained about individuals above or below the average youth symptom severity.
One group of models was conducted for each of the three respondents on the SFSS: the youth, caregiver, and clinician. An example of the within-youth model (Level 1) used for each youth in the sample is:
In Eq. 1, BMSLSSti represents the youth’s life satisfaction of youth i at time t, Timeti represents the time in months the youth had been in treatment, and SFSSchti indicates the change in youth’s symptom severity since baseline as rated by person i at time t. An example of the Level-2 model used is specified as follows:
Equation 2 captures the mean initial youth life satisfaction (β00), the average monthly rate of change in youth life satisfaction (β10), the initial relationship between youth’s baseline symptom severity and youth life satisfaction (β01), and the association between change in youth life satisfaction and change in youth symptom severity (β20).
In addition, the Level-2 model includes several binary predictors previously identified in the literature. The description and coding for these predictors are found in Table 1. Age was grand-mean centered. Of the 334 youth included in this analysis, approximately 51% were male, 77% had a diagnosis, 46% had used alcohol or drugs (as reported by the clinician on the background questionnaire at baseline), and 67% indicated that religion or spirituality is important in helping them with their problems (as reported by youth on the background questionnaire at baseline). Among the caregivers of these youth, 44% were married (or living as married) and 28% had a history of an emotional, behavior or substance problem (as reported by the caregiver on the background questionnaire at baseline).
The r0i and r1i in Eq. 2 are Level-2 residuals, which are also called as random effects. The r0i captures the deviation of a youth’s initial BMSLSS-PTPB from the mean, and r1i indicates a youth’s deviation from mean rate of BMSLSS-PTPB change. These residuals are assumed to be normally distributed with variance τ00 and τ11, respectively. A lack of degrees of freedom prohibited the investigation of the variance for change in symptom severity (π2i). Therefore, τ21 was fixed within all Level-2 models. Nested models were compared using deviance statistics to determine best fit to the data.
Results
Psychometric Properties of the BMSLSS-PTPB
The results of the psychometric analyses for individual items and the BMSLSS-PTPB Total Score are presented in Table 2. The Total Score distribution was approximately normally distributed with a mean of 3.81 (SD = 0.85) indicating that generally youth reported high satisfaction with life. For individual items, where ratings could range from 1 to 5, two items (item 2 ‘Satisfaction with friendships’ and item 4 ‘Satisfaction with myself’) had means approaching the ceiling resulting in slightly skewed item score distributions. The BMSLSS-PTPB Total Score demonstrated a satisfactory degree of internal consistency (Standardized Chronbach’s α = 0.77). This is consistent with the range of values found in the psychometric evaluation of the original BMSLSS in normative (school) samples (Chronbach’s α = 0.76–0.85; Huebner, Seligson, Valois, and Suldo 2006). The item-total correlations of the BMSLSS-PTPB ranged from 0.40 to 0.78 and item difficulties ranged from −0.36 to 0.40 on a logit scale. Fit indices (infit and outfit) were adequate and all fell within the desirable range of 0.6–1.4 (Wright and Linacre 1994), indicating model fit. Generally, the items also displayed adequate discrimination (i.e., discrimination values close to 1). This means that items are able to discriminate between youth with low versus high life satisfaction. However, item 3 (‘Satisfaction with school’) may not discriminate as readily as other items.
Results of CFA indicated the proposed one-factor model fit the data (Bentler CFI = 0.93; Joreskog GFI = 0.97; SRMR = 0.05). Standardized factor loadings ranged from 0.46 to 0.78. Overall, results suggest the BMSLSS-PTPB is a psychometrically sound instrument for use in youth in home-based mental health services.
To aid interpretation, scores can be classified as high, medium, and low according to the 25th and 75th quartiles. For the BMSLSS-PTPB Total Score, a score greater than 4.5 is considered high, while a score less than 3.3 is considered low. Scores between 3.3 and 4.5 are considered medium or moderate scores. Based on standard error of measurement (SEM = 0.40) and the internal reliability of the measure, an index of minimum detectable change (MDC) was calculated. The MDC indicates with 75% confidence that a change of 0.66 points in the BMSLSS-PTPB Total Score from one administration to the next is not due to chance or measurement error and thus may be clinically meaningful.
As hypothesized, the BMSLSS-PTPB was significantly correlated with youth hope (CHS-PTPB; r = 0.40, p < 0.001) and youth-rated symptom severity (SFSS; r = −0.36, p < 0.001). Additionally, the BMSLSS-PTPB did not significantly relate to youth TOES (0.08, p = 0.17). This provides some evidence for the construct validity of the BMSLSS-PTPB in this sample.
Youth Life Satisfaction Predicts Change in Severity of Symptoms and Functioning
The longitudinal analyses focused on the relationship between youth life satisfaction and change in youth symptom severity over time. Table 3 presents descriptive statistics for life satisfaction (BMSLSS-PTPB Total Score) and symptom severity (SFSS Total Score) at baseline and the last time each was measured. In addition, Table 3 presents overall values for change (i.e., raw discrepancy scores) for each measure as well as the relationship between measures. These statistics for the first and last time points of each measure are included to provide an overall indication of change over time and should be interpreted with caution, given that they did not account for length of time in treatment. Youth received treatment for varying lengths of time and thus the time between the first and last measurement points varied by youth. For example, of the 204 youths with more than one completed BMSLSS-PTPB measure, the average length of time between first and last measurement point was 16.4 weeks (SD = 12.06), but this duration varied from approximately 2 weeks to 75 weeks.
Matched paired t tests showed that average youth life satisfaction increased and symptom severity (rated by the youth, caregiver, and clinician) decreased between baseline and the last time point. Additionally, correlations between youth life satisfaction and symptom severity ratings indicated a significant negative relationship between youth life satisfaction and youth- and clinician-rated symptom severity across both time points. Although the correlation between youth life satisfaction and caregiver-rated symptom severity was significant at baseline, it failed to reach significance at the final time point.
Results of fitting the final HLM models to the data are found in Table 4. Baseline models without Level-2 predictors were conducted prior to final models. However, based on deviance statistics, the final models provided a better fit to the data. Therefore, only final results are presented.
With one exception, results were similar across the three SFSS respondent models (youth, caregiver, and clinician). At baseline, average youth life satisfaction varied significantly by baseline symptom severity (β01) for all three respondents. The negative direction of these parameters indicates that lower baseline life satisfaction reported by youth was related to higher baseline symptom severity regardless of respondent, and vice versa. There was also a significant relationship between youth baseline life satisfaction and youth age (β03) in all three models. Given that age was grand-mean centered at 15 years, holding all else constant, average baseline life satisfaction was higher for youth aged 11–14 years as compared to older youth. Additionally, on average females had lower baseline life satisfaction compared to males (β02) in the caregiver and clinician models. There were no differences in any of the three models for the remaining fixed effects (clinician-reported youth diagnosis or substance use at baseline, youth self-report of the importance of religion/spirituality in helping with problems, and caregiver-report of marital status and their own history of emotional, behavioral, or substance use problems).
On average, youth satisfaction with life (β10) improved throughout treatment. Consistent with our hypothesis, average life satisfaction reported by the youth increased faster when there was a corresponding decrease in youth symptom severity (β20), regardless of which respondent was rating symptom severity. For example, holding all else constant, for every unit improvement in symptom severity according to the youth, average life satisfaction increased 0.02 units faster than a corresponding youth with no symptom improvement.
Comparing youth who are improving, worsening, or staying the same in terms of symptom severity may help better explain the relationship between symptom improvement and increased youth life satisfaction. Based on the psychometric study, an MDC was calculated for each respondent of the SFSS (see Athay et al. (2012) in this issue). The MDC value indicates with 75% certainty that a change in SFSS is not due to chance or measurement error. Therefore, a youth with continuous improvement in symptom severity here is defined as having a one MDC decrease in SFSS each month during treatment. Similarly, youth with worsening symptoms is defined as having an increase in symptom severity of one MDC each month. A youth with no change in symptom severity is defined as maintaining the same SFSS score throughout treatment. As reported previously, MDC’s for the SFSS Total Scores were 4.63 (youth respondent), 4.43 (clinician) and 4.07 (caregiver). Figure 1 depicts predicted life satisfaction trajectories based on these definitions for youth’s symptom change (as indicated by each of the three respondents). These are predicted scores for the average 15 year old.
Figure 1 illustrates the relationship between life satisfaction and symptom severity over time separately for males and females. In general, youth (both males and females) with continuous improvement in symptom severity also showed substantial improvement over time in life satisfaction; whereas life satisfaction only increased slightly or remained relatively stable over time for youth with no change in symptom severity. Youth with continuous worsening of symptom severity showed a slight decline in life satisfaction over time, with a substantial decline when the youth themselves reported their symptoms. As seen when comparing the male and female graphs in Fig. 1, a gender difference is apparent in the intercept where females, on average, had lower baseline life satisfaction compared to males.
Discussion
In the first portion of this paper, the psychometric properties of the BMSLSS-PTPB were evaluated with a sample of clinically-referred youth aged 11–18. This measure provides a global score of the youth’s life satisfaction. The use of multiple methods (CTT, CFA, and IRT) in this psychometric evaluation provided a greater understanding about how this measure and corresponding items function in this population. These methods also provided more evidence about the validity of the measure than a single method would have yielded.
Psychometric analyses indicated that overall, the BMSLSS-PTPB displays adequate psychometric properties for use with clinically-referred youth. BMSLSS-PTPB Total Scores and individual items were approximately normally distributed. The BMSLSS-PTPB had high internal consistency, adequate item-total correlations, and the proposed single-factor model was confirmed. Application of the RSM indicated the items fit the model and, thus, demonstrated sufficient measure characteristics. The BMSLSS-PTPB also showed evidence of construct validity with expected significant correlations to measures of youth hope and symptom severity, and an expected lack of relationship to youth treatment outcome expectations. However, further validation research is needed given that measure validation is a never-ending and circular process (Hubley and Zumbo 1996). Additionally, further analyses are needed to evaluate the predictive validity of the BMSLSS-PTPB as well as its sensitivity to change in this population.
This study also examined the relationship between youth life satisfaction and symptom severity over time. No other studies were indentified that investigated this relationship. The findings of the current longitudinal analysis indicated a clear pattern where greater increases in life satisfaction were found in the presence of corresponding decreases in symptom severity (and vice versa). For youth with relatively stable symptom severity over time, there was little change in life satisfaction. This held true regardless of whether the youth, the caregiver, or the clinician reported on youth symptoms. As recommended by others (e.g., Maddux 2005), such findings lend support for the integration of strengths-based assessment into the traditional measurement of psychopathology in youth mental health services. With frequent measurement, both life satisfaction and symptom severity serve as related but distinct indicators of treatment progress that clinicians can use to ‘stay the course’ when youths are improving, or adjust the focus of treatment if they observe a worsening in either life satisfaction or symptoms.
Given the findings of the present study, an interesting next step would be determining whether focusing on life satisfaction in treatment could serve to improve youth mental health symptoms and functioning, and vice versa. Current analyses indicate that life satisfaction and symptom severity are interrelated both at baseline and over the course of youth treatment. Unfortunately, the correlational nature of this study limits the ability to infer causality. It may be that changes in symptom severity cause changes in life satisfaction or it could be the reverse. Alternatively, a causal relationship between life satisfaction and symptom severity may be bidirectional, which would lend additional support to focusing on common factors and strengths throughout the course of treatment. Regardless of the specific causal nature of the relationship, the relationships between life satisfaction and youth self-report, caregiver- and clinician-rated youth symptom severity indicate that both symptom reduction and improvement in life satisfaction are important goals of treatment. Further research is needed on such a ‘dual factor model’ that incorporates both indicators of wellness and psychopathology in youth mental health treatment settings (e.g., Suldo et al. 2011).
Because no information was available on the specific types of treatment received by the youth or the therapeutic orientation of the clinicians in the present study, it is unclear whether the specific treatment or clinician-orientation may have contributed to the relationship between life satisfaction and symptom severity. It could be that the clinicians were already utilizing some strengths-based strategies in their routine clinical care, which may have impacted the relationship between youth life satisfaction and symptom severity in the present study. Additional research will be needed examining the possible impact of clinician and treatment characteristics on this relationship.
While younger age and male gender were associated with higher baseline life satisfaction, there were no differences in youth life satisfaction for any of the other baseline correlates including youth’s rating of the importance of spirituality or religion in helping with problems, youth substance abuse, presence of a clinician-reported mental health diagnosis at baseline, or caregivers’ marital status and history of emotional, behavioral, or substance use problems. It is possible that these factors, as measured in the current study, served as insufficient proxies for some of the correlates previously identified in the literature, such as youth substance use (e.g., Becker et al. 2009; Farhat et al. 2011), caregiver distress (e.g., Powdthavee and Vignoles, 2008), and youth spirituality-related attributes (e.g., Sawatzky et al. 2009).
The present study found the BMSLSS-PTPB to be a psychometrically sound measure. Additionally, the present results supported a relationship between youth life satisfaction and symptom severity over time. As a whole, the results of the present study suggest that, alongside measuring pathology, this brief measure of positive functioning changes over time and is coherently related to other clinical constructs.
References
Andrich, D. (1978). A rating formulation for ordered response categories. Psychometrika, 43, 561–573.
Athay, M.M., Riemer, M., & Bickman, L. (2012). The Symptoms and Functioning Severity Scale (SFSS): Psychometric evaluation and discrepancies among youth, caregiver, and clinician ratings over time. Administration and Policy in Mental Health and Mental Health Services Research. doi:10.1007/s10488-012-0403-2.
Becker, S. J., Curry, J. F., & Yang, C. (2009). Longitudinal association between frequency of substance use and quality of life among adolescents receiving a brief outpatient intervention. Psychology of Addictive Behaviors, 23, 482–490.
Bickman, L., Reimer, M., Lambert, E.W., Kelley, S.D., Breda, C., Dew., S., et al. (2007). Manual of the Peabody Treatment and Progress Battery (Electronic version). Nashville, TN: Vanderbilt University. http://peabody.vanderbilt.edu/ptpb/.
Bickman, L., Athay, M.M., Riemer, M., Lambert, E.W., Kelley, S.D., Breda, C., Tempesti, T., Dew-Reeves, S.E., Brannan, A.M., Vides de Andrade, A.R. (eds). (2010). Manual of the Peabody Treatment Progress Battery, 2nd ed. [Electronic version]. Nashville, TN: Vanderbilt University. http://peabody.vanderbilt.edu/ptpb\.
Bickman, L., Kelley, S., Breda, C., DeAndrade, A., & Riemer, M. (2011). Effects of routine feedback to clinicians on youth mental health outcomes: A randomized cluster design. Psychiatric Services, 62, 1423–1429.
Dew-Reeves, S.E., & Athay, M.M. (2012). Validation and use of the youth and caregiver Treatment Outcome Expectations Scale (TOES) to assess the relationship between expectations, pretreatment characteristics, and outcomes. Administration and Policy in Mental Health and Mental Health Services Research. doi:10.1007/s10488-012-0406-z.
Dew-Reeves, S.E., Athay, M.M., & Kelley, S.D. (2012). Validation and use of the Children's Hope Scale - Revised PTPB Edition (CHS-PTPB): High initial youth hope and elevated baseline symptomatology predict poor treatment outcomes. Administration and Policy in Mental Health and Mental Health Services Research. doi:10.1007/s10488-012-0411-2.
Diener, E., Suh, E. M., Lucas, R. E., & Smith, H. L. (1999). Subjective well-being: Three decades of progress. Psychological Bulletin, 125, 276–302.
Farhat, T., Simons-Morton, B., & Luk, J. W. (2011). Psychosocial correlates of adolescent marijuana use: Variations by status of marijuana use. Addictive Behaviors, 36, 404–407.
Fredrickson, B. L. (2001). The role of positive emotions in positive psychology: The broaden-and-build theory of positive emotions. American Psychologist, 56, 218–226.
Gilman, R., & Huebner, S. (2003). A review of life satisfaction research with children and adolescents. School Psychology Quarterly, 18, 192–205.
Greenspoon, P. J., & Saklofske, D. H. (2001). Toward an integration of subjective wellbeing and psychopathology. Social Indicators Research, 54, 81–108.
Hubley, A.M., & Zumbo, B.D. (1996). A dialectic on validity: where we have been and where we are going. Journal of General Psychology, 123, 207–215.
Huebner, E. S. (2004). Research on assessment of life satisfaction of children and adolescents. Social Indicators Research, 66, 3–33.
Huebner, E.S., Seligson, J.L., Valois, R.F., & Suldo, S.M. (2006). A review of the Brief Multidimensional Students' Life Satisfaction Scale. Social Indicators Research, 79, 477–484.
Kwan, Y. K. (2010). Life satisfaction and self-assessed health among adolescents in Hong Kong. Journal of Happiness Studies, 11, 383–393.
Lewis, A. D., Huebner, E. S., Malone, P. S., & Valois, R. F. (2011). Life satisfaction and student engagement in adolescents. Journal of Youth and Adolescence, 40, 249–262.
Linacre, J.M. (2007). WINSTEPS® 3.63.0 [Computer software]. Retrieved Jan 8, 2007, from http://www.winsteps.com/index.htm.
Maddux, J. E. (2005). Stopping the “madness:” Positive psychology and the deconstruction of the illness ideology and the DSM. In C. Snyder (Ed.), Handbook of positive psychology (pp. 13–25). Cary: Oxford University Press.
McKnight, P. E., McKnight, K. M., Sidani, S., & Figueredo, A. J. (2007). Missing data: A gentle introduction. New York: Guilford Press.
Pavot, W. G., Diener, E., Colvin, C. R., & Sandvik, E. (1991). Further validation of the satisfaction with life scale: Evidence for the cross-method convergence of well-being measures. Journal of Personality Assessment, 57, 149–161.
Piko, B. F., & Hamvai, C. (2010). Parent, school, and peer-related correlates of adolescents’ life satisfaction. Children and Youth Services Review, 32, 1479–1482.
Powdthavee, N., & Vignoles, A. (2008). Mental health of parents and life satisfaction of children: A within-family analysis of intergenerational transmission of well-being. Social Indicators Research, 88, 397–422.
Proctor, C. L., Linley, P. A., & Maltby, J. (2009). Youth life satisfaction: A review of the literature. Journal of Happiness Studies, 10, 583–630.
Proctor, C., Linley, P. A., & Maltby, J. (2010). Very happy youths: Benefits of very high life satisfaction among adolescents. Social Indicators Research, 98, 519–532.
Raudenbush, S. W., & Bryk, A. S. (2002). Hierarchical Linear Models: Applications and data analysis methods. Thousand Oaks: Sage Publishing.
Raudenbush, S. W., Bryk, A. S., & Congdon, R. (2004). HLM 6 for Windows [Computer software]. Lincolnwood, IL: Scientific Software International, Inc.
Riemer, M., Athay, M.M., Bickman, L., Breda, C., Kelley, S.D., & Vides de Andrade (2012). The Peabody Treatment Progress Battery: History and methods for developing a comprehensive measurement battery for youth mental health. Administration and Policy in Mental Health and Mental Health Services Research. doi:10.1007/s10488-012-0404-1.
Rubin, D. B. (1987). Multiple imputation for nonresponse in Surveys. New York: Wiley.
Sawatzky, R., Gadermann, A., & Pesut, B. (2009). An investigation of the relationship between spirituality, health status and quality of life in adolescents. Applied Research Quality Life, 4, 5–22.
Seligman, M. E. P., & Csikszentmihalyi, M. (2000). Positive psychology: An introduction. American Psychologist, 55, 5–14.
Seligson, J., Huebner, E. S., & Valois, R. F. (2003). Preliminary validation of the brief multidimensional students’ life satisfaction scale (BMSLSS). Social Indicators Research, 61, 121–145.
Singer, J. D., & Willet, J. B. (2003). Applied longitudinal data analysis: Modeling change and event occurrence. New York: Oxford University Press.
Suldo, S. M., & Shaffer, E. J. (2008). Looking beyond psychopathology: The dual-factor model of mental health in youth. School Psychology Review, 37, 52–68.
Suldo, S. M., Riley, K., & Shaffer, E. S. (2006). Academic correlates of children and adolescents’ life satisfaction. School Psychology International, 27, 567–582.
Suldo, S., Thalji, A., & Ferron, J. (2011). Longitudinal academic outcomes predicted by early adolescents’ subjective well-being, psychopathology, and mental health status yielded from a dual factor model. The Journal of Positive Psychology, 6, 17–30.
Von Hippel, P. T. (2005). How many imputations are needed? A comment on Hershberger and Fisher (2003). Structural Equation Modeling, 12, 334–335.
Wright, B.D., & Linacre, J.M. (1994). Reasonable mean-square fit values. Rasch Measurement Transactions, 8, 370. Retrieved March 10, 2011 from www.rasch.org/rmt/rmt83b.htm.
Acknowledgments
This research was supported by NIMH grants R01-MH068589 and 4264600201 awarded to Leonard Bickman.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Michele Athay, M., Kelley, S.D. & Dew-Reeves, S.E. Brief Multidimensional Students’ Life Satisfaction Scale—PTPB Version (BMSLSS-PTPB): Psychometric Properties and Relationship with Mental Health Symptom Severity Over Time. Adm Policy Ment Health 39, 30–40 (2012). https://doi.org/10.1007/s10488-011-0385-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10488-011-0385-5