Abstract
The aim of this study was to discuss the effect of autogenic training (AT) on patients with functional somatic syndrome (FSS) using salivary amylase, the skin temperature of the finger, subjective severity of symptoms, and psychological characteristics as measures. We assessed 20 patients with FSS and 23 healthy controls before and after AT. Baseline levels of salivary amylase prior to an AT session were significantly higher in the FSS group than in the control group. However, this difference was not significant after AT. The skin temperature of the finger increased after AT in both the FSS and control groups. AT contributed to the improvement of somatic symptoms in patients with FSS. Our results regarding psychological characteristics suggest that mood disturbances are deeply involved in the pathology of FSS. Individuals with FSS exhibited elevated levels of sympathetic activity compared with healthy controls. Our data indicates that AT eased dysregulation of the autonomic nervous system in patients with FSS. Thus, salivary amylase may be a useful index of change induced by AT in patients with FSS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Functional somatic syndrome (FSS) encompasses a group of syndromes that have a medically unknown origin (Barsky and Borus 1999; Wessely et al. 1999). According to Barsky and Borus, “Functional somatic syndrome (FSS) refers to several related syndromes that are characterized more by symptoms, suffering, and disability than by disease-specific, demonstrable abnormalities of structure or function” (Barsky and Borus 1999). Presently, there is no objective criterion for defining FSS (Henningsen et al. 2007).
Although FSS includes a range of diseases such as irritable bowel syndrome (IBS), functional dyspepsia (FD), fibromyalgia (FMS), and chronic fatigue syndrome (CFS), there is considerable overlap among the symptoms characteristic of each disorder (Nimnuan et al. 2001).
Patients with FSS often undergo repeated investigation and treatment in the hospital. Thus, FSS is associated with substantial costs to patients and the health system. FSS constitutes a large, clinically important, and costly health-care issue that urgently requires better understanding and improved management (Wessely et al. 1999). However, the pathology of FSS is poorly understood.
Dysregulation of the autonomic nervous system is an important component of FSS (Tak and Rosmalen 2010) that is strongly related to psychosocial factors (Barsky and Borus 1999). Previously, we examined dysregulation of the autonomic nervous system in patients with FSS via psychophysiological evaluation. We found that patients with FSS had a hypo-reactive psychophysiological acute stress response compared with healthy controls (Kanbara et al. 2004). Similarly, dysregulation of the autonomic nervous system has been reported in patients with FMS (Okifuji and Turk 2002). In another previous study, we reported that the physiological response in patients with FSS was lower than that in controls, but we found two sub-groups among individuals with FSS, who differed in terms of autonomic lability (i.e., low- and high-lability) (Kanbara et al. 2007). These studies suggest that evaluation of the autonomic nervous system is important when considering the pathology of FSS.
The somatic symptoms of FSS are maintained, prolonged chronically, and deteriorated by mood disturbances, such as anxiety or depression (Henningsen et al. 2003). Moreover, difficulty identifying or describing feelings (termed alexithymia) and a reduction of awareness of bodily feelings appear to be symptoms of FSS (Barsky and Borus 1999; Kanbara and Fukunaga 2009). In our previous study, we indicated that the relationship between autonomic function and alexithymia showed an inverse correlations between FSS patients and healthy controls (Kiba et al. 2013).
Considering the above, it seems necessary to examine the pathological elements of FSS from multiple perspectives, for instance, objective, subjective, and psychological evaluations.
Active behavioral interventions, such as biofeedback and hypnosis, have been effective in the management of FSS (Henningsen et al. 2007).
Autogenic training (AT), which is based on the study of hypnosis (Kasai 2012), is one approach to adjusting autonomic nervous system activity (Oka et al. 1994). In addition, AT is effective for relieving physical symptoms associated with anxiety or depression (Matsuoka 2012). AT decreases cardiac sympathetic nervous system activity and increases cardiac parasympathetic nervous system activity (Mitani et al. 2006). AT increases peripheral skin temperature (Oka and Koyama 2012), making the skin temperature of the finger (TEMP) a useful objective index for measuring changes induced by AT.
The clinical efficacy of AT can be evaluated via meta-analysis (Stetter and Kupper 2002). AT is thought to be effective for improving mood and cognitive performance. Moreover, AT has been found to be efficacious in treating tension headaches/migraines, mild-to-moderate essential hypertension, and coronary heart disease as well.
Several studies have investigated the influence of AT on types of FSS, such as IBS (Shinozaki et al. 2010), FMS (Keel et al. 1998), and tension headache (Collet et al. 1986; Van Dyck et al. 1991; Zitman et al. 1992; Spinhoven et al. 1992; Zsombok et al. 2003; Blanchard and Kim 2005; Kanji et al. 2006). In these studies, AT improved the physical symptoms and quality of life of patients. However, to the best of our knowledge, no studies have addressed the effect of AT on the full spectrum of FSS disorders.
A variety of methods have been employed with the goal of quantitatively measuring the psychophysiological status of patients with FSS. For instance, studies have evaluated autonomic nervous system activity using heart rate variability, surface electromyography, skin conductance, and so on (Kanbara et al. 2004, 2007; Tak and Rosmalen 2010). When evaluating the autonomic nervous system, biomarkers are required in addition to psychophysiological measures (Yamaguchi 2007). Therefore, cortisol is often used to evaluate the pathology of FSS (Mutsuura et al. 2009; Tak and Rosmalen 2010; Tak et al. 2011). However, using cortisol as an endocrine marker has certain limitations. For instance, secretion of cortisol is usually delayed by 20–30 min after stress stimulation in a stress test (Yamaguchi et al. 2007).
In contrast, salivary amylase (SAMY) can be used as an index of the sympathetic nervous system with the following advantages: it is instantaneousness, convenient, and non-invasive (Speirs et al. 1974; Bosch et al. 2002; Yamaguchi et al. 2006, 2007; Yamaguchi 2007). Some studies using SAMY have reported that it increases in response to heightened psychophysiological stress and is positively correlated with states of anxiety (Bosch et al. 1996; Mizuno et al. 2001; Bosch et al. 2003; Noto et al. 2005; Grillon et al. 2007; Shigeno et al. 2009; Murakami et al. 2009). However, these studies assessed healthy controls only. In addition, to the best of our knowledge, no studies have used SAMY to measure changes in autonomic nervous system activity induced by AT. Further, few studies have used SAMY to assess FSS pathology. Previously, we examined the relationship between SAMY levels and the psychological characteristics of patients with FSS (Kiba et al. 2013). We found that the pre-stress SAMY levels of patients with FSS were significantly higher than those of healthy controls, and that SAMY levels were closely correlated with tension, anxiety, and persistent depression.
Thus, the aim of this study was to use SAMY, TEMP, subjective severity of symptoms, and psychological characteristics to evaluate changes induced by AT in patients with FSS. We sought to test the following hypotheses: (1) SAMY is a useful index for measuring changes induced by AT in patients with FSS; (2) The pattern of SAMY change induced by AT in patients with FSS will differ from that in healthy controls.
Methods
Participants
Twenty patients (13 females and 7 males: age range = 22–71 years; mean ± standard deviation (SD) = 40.50 ± 13.57 years) comprised the participant group. All individuals were diagnosed with FSS according to the steps described below.
For study eligibility, we selected patients for whom physicians specializing in psychosomatic medicine (members of the Japanese Society of Psychosomatic Medicine) predicted AT would be effective as per a psychophysiological assessment. All participants gave written informed consent.
The diagnoses of 20 patients were as follows: IBS (n = 7), FD (n = 9), FMS (n = 3), CFS (n = 1), tension headache (n = 4), premenstrual syndrome (n = 2), chronic low back pain (n = 1), globus syndrome (n = 1). The physicians made diagnoses according to each criterion of each syndrome. FD and IBS were diagnosed using the ROME III (Tack et al. 2006; Longstreth et al. 2006), FMS using the American College of Rheumatology 1990 Criteria (Wolfe et al. 1990), CFS using the criteria of the International Chronic Fatigue Syndrome Study Group (Fukuda et al. 1994), tension headache using the International Classification of Headache Disorders 2nd Edition (Subcommittee of International Headache Society 2004), premenstrual syndrome using the criteria of the ACOG practice bulletin (2001), chronic low back pain using the criteria described by Last and Hulbert (2009), and globus syndrome using the criteria described by Koike et al. (1979).
We asked participants to maintain doses of existing medications prior to the examination, when possible, and they reported complying with this request. Five of the patients drank alcohol on a regular basis.
Twenty-three healthy participants (13 females and 10 males: age range = 16–65 years; mean ± SD = 37.83 ± 10.87 years) participated as controls. They were recruited through a public announcement that asked people to participate in a study that examining changes in autonomic activity induced by AT. Individuals who were regularly receiving medical care or had somatic symptoms were excluded. The controls were paid 3000 yen each for their participation. Ten of the healthy subjects drank alcohol regularly. We found no significant differences between the FSS group and healthy controls with respect to age (T test; p = .181, d = 0.220), the male/female ratio (χ2 test, χ2 = 0.065, p = .799, φ = −0.086), or the alcohol drinkers/non-drinkers ratio (χ2 test, χ2 = 0.897, p = .343, φ = 0.193).
This study was approved by the ethics committee of Kansai Medical University.
Autogenic Training
The form of AT used in this study was based on the style developed by Schulz (Schulz 1932; Schultz and Luthe 1969; Luthe and Schultz 1969). In this study, AT consisted of two standard exercises that took place after the participant stated the following formula: “I am at peace”. The first exercise encourages muscular relaxation via repetition of the formula: “My arms are heavy”. The next exercise encourages patients to feel warm via repetition of the following formula: “My arms are warm”. AT was performed in a sitting posture, using a tape recording.
The AT session was conducted individually in an examination room.
Biochemical and Psychophysiological Measurements
We measured SAMY using a hand-held type of salivary amylase monitor (Amylase monitor, Nipro Co., Ltd, Osaka, Japan.).
We measured body temperature (TEMP) using a non-contact thermometer (Human Ful Thermometer, Mistal Co., Ltd, Sendai, Japan.) because we were able to gain more detailed information about TEMP via infrared rays (Ioannou et al. 2014). We measured the skin temperature of the tip of the middle finger of both hands, and used the mean for analysis.
Subjective Measurements
We used the VAS to evaluate the subjective severity of symptoms in the FSS patients: scores ranged from 0 (absent) to 100 (most severe).
Mood Measurements
To evaluate the psychological characteristics of the participants, we administered the Japanese edition of the Profile of Mood States (POMS) scale (Yokoyama et al. 1990), the Japanese version of the Hospital Anxiety and Depression Scale (HADS) (Hatta et al. 1998), the Japanese version of the Somatosensory Amplification Scale (SSAS) (Nakao et al. 2001), and the Japanese version of the Toronto Alexithymia Scale-20 (TAS-20) (Komai et al. 2003) during each session.
POMS is a 65-item scale that assesses six temporal affective mood dimensions. The subscale consists of tension-anxiety (T–A; range of T-score: 31–85), depression-dejection (D; range of T-score: 40–85), anger-hostility (A–H; range of T-score: 37–85), vigor (V; range of T-score: 27–80), fatigue (F; range of T-score: 35–85), and confusion (C; range of T-score: 32–85). HADS is a 14-item scale that assesses anxiety (A; range: 0–21) and depression (D; range: 0–21). SSAS (range: 10–50) is a 10-item scale that assesses somatosensory function. TAS-20 (range: 20–100) is a 20-item scale that assesses alexithymia. It has a subscale that measures difficulty identifying feelings (dif; range: 7–35), difficulty describing feelings (ddf; range: 5–25), and externally oriented thinking (eot; range: 8–40). The reliability and validity of POMS (Yokoyama et al. 1990), HADS (Hatta et al. 1998), SSAS (Nakao et al. 2001) and TAS-20 (Komai et al. 2003) have been confirmed previously.
Procedure
This study was conducted at the Department of Psychosomatic Medicine of the Kansai Medical University Hospital in Osaka, Japan between July 2012 and August 2013.
A patient was diagnosed as having FSS if he/she met the following four conditions, which were based on the diagnostic criteria from our previous study (Kanbara et al. 2007) and that in Henningsen’s study (Henningsen et al. 2007): (1) chief complaints were somatic symptoms that could not be explained medically or by a psychiatric disorder; (2) the subjective symptom rating score, based on a visual analogue scale (VAS) (Wewers and Lowe 1990), was ≥3 and the duration of the symptoms was ≥6 months; (3) the patient had disabilities that affected social or daily activity owing to the symptoms (The Global Assessment of Functioning Scale (American Psychiatric Association 2000) was ≤80); (4) the patient was diagnosed as having one of the diseases for which the review number in Henningsen’s study (Henningsen et al. 2007) was ≥2. We began with 30 potential participants. According to these conditions, five patients were excluded from the study [owing to the FSS criteria (4)]. Two patients were excluded because they were receiving β-adrenergic blockers, which are known to reduce levels of SAMY (Speirs et al. 1974). One patient was excluded because she was receiving a tricyclic antidepressant, which is known to increase SAMY levels (Veen et al. 2013). Two patients dropped out during the AT procedure. Finally, the remaining 20 patients were entered into the analyses portion of the study.
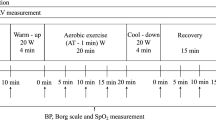
The session protocol is shown in Fig. 1. Mood measurements were collected at home on the day of each session. Biochemical, psychophysiological, and subjective measurements were collected in a hospital examination room. The room temperature was kept constant at 25 °C. Before starting the experiment, the participants received an explanation about the effects and method of AT both in writing and on a video. They were first instructed to relax and make themselves comfortable for 2 min, and then to engage in AT for 3 min. After an interval of 2 min, they repeated AT. We collected SAMY, TEMP, and subjective symptom score measurements both before and after AT. In consideration of circadian variations in SAMY levels (Nater et al. 2007), the examination was scheduled to take place between 15:30 and 16:30.
Statistical Methods
To compare changes in SAMY and TEMP levels, we conducted a two-way repeated measures analysis of variance (ANOVA) with “pre/post” (two levels: baseline and after AT) as the within-subjects factor and “group” (two levels: control and FSS groups) as the between-subjects factor.
To assess changes in the subjective symptom score in patients with FSS between baseline and after AT, we conducted a T-test.
To compare the psychological test results between patients with FSS and healthy controls, we conducted a T-test. If the ANOVA was significant, we used the Bonferroni correction to evaluate the significance of the individual differences.
Statistical analyses were performed using PASW statistics 18.0 for WindowsTM (SPSS Inc., Chicago, IL, USA). The α level was fixed at 0.05.
Results
Salivary Amylase
Figure 2 shows the changes in SAMY levels for AT session in the FSS and control groups. The two-way ANOVA indicated that the pre/post-group interaction was significant (F(1,41) = 11.02, p = .002, \(\eta_{p}^{2}\) = 212).
The simple main effects test revealed that in the FSS group, the levels of SAMY after the AT session were significantly lower than those measured at baseline (F(1,41) = 15.15, p = .001).
In the control group, the level of SAMY after AT was significantly lower than the baseline level (F(1,22) = 7.56, p = .012, \(\eta_{p}^{2}\) = 0.256).
With respect to the difference in SAMY levels between the groups, the baseline levels in the AT session in the FSS group were significantly higher than those in the control group (F(1,41) = 11.69, p = .001).
Skin Temperature of the Finger
Figure 3 shows the changes in TEMP for both AT sessions in the FSS and control groups. The two-way ANOVA indicated that the pre/post effect was significant (F(1,41) = 5.946, p = .019, \(\eta_{p}^{2}\) = 127), but the pre/post-group interaction (F(1,41) = 3.592, p = .065, \(\eta_{p}^{2}\) = 0.081) and the group effect (F(1,41) = 2.733, p = .106, \(\eta_{p}^{2}\) = 0.063) were not significant.
In summary, we observed an increase in TEMP in both the FSS and the control group.
Psychological Test Results
Table 1 shows the psychological characteristics recorded in the FSS and healthy control groups. As indicated by the T-test, patients with FSS exhibited significantly lower POMS-V, while all other psychological test scores were significantly higher (scores on the POMS-A-H, TAS-20-ddf, and TAS-20-eot were higher but this effect did not reach significance) than those obtained by healthy controls.
Subjective Symptom Score
Figure 4 shows the changes in subjective symptom scores in the AT sessions in the FSS group. The T-test showed that the subjective symptom scores in the FSS group decreased between baseline and after AT (p = .001, d = 0.059).
Discussion
In the present study, we explored whether SAMY was efficacious as an index for measuring changes induced by AT in patients with FSS.
We found that baseline levels of SAMY in the FSS group were significantly higher than those in the control group. This indicates that the sympathetic nervous system is strained in patients with FSS. In our previous study, we suggested that pre-stress SAMY levels in patients with FSS were significantly higher than those in healthy controls (Kiba et al. 2013), which is in agreement with our present findings. Moreover, patients with FSS exhibit reduced cardiac vagal activity (Tak and Rosmalen 2010). Considering the above, a highly-strained sympathetic nervous system, as reflected by elevated SAMY levels at rest, may be associated with FSS pathology.
In the FSS group, SAMY levels decreased in the AT session. This result is in agreement with previous findings showing that AT decreases sympathetic nervous system activity (Oka and Koyama 2012; Mitani et al. 2006). Based on this results, we conclude that the performance of AT improves autonomic nervous system dysregulation in patients with FSS.
It is possible that the decrease in SAMY levels during the AT session in the FSS group was influenced by the highly-strained sympathetic nervous system at baseline. However, because it is known that the sympathetic nervous system is more active in patients with FSS, this may be thought of as a characteristic of patients with FSS. The dysregulation of the autonomic nervous system in patients with FSS may be unequal (Giesecke et al. 2003; Kanbara and Fukunaga 2009). Although we are unable to address this in the present study because our sample size was too small, patients with FSS may be classified according to levels of SAMY (i.e, low- and high-strain), considering the findings of our previous study (Kanbara et al. 2007). Thus, while the performance of AT appears to decrease sympathetic nervous system activity in patients with FSS, AT may be particularly effective for patients with FSS who suffer from especially high levels of sympathetic nervous system activity. Whether individuals with FSS can be classified into two groups based on SAMY levels as a biochemical index remains to be established.
We also observed a decrease in the levels of SAMY during the AT sessions in the control group. AT is thought to be helpful for healthy people as a form of stress management and promotion of health (Kasai 2012; Oka and Koyama 2012). The current study suggests that AT is helpful for healthy people as a method of relaxation.
We observed an increase in TEMP in the AT session in both the FSS and the control group.
With respect to stress, TEMP is an index of variability in autonomic activity (Palanisamy et al. 2012), and it decreases if the sympathetic nervous system is strained (Yamashiro et al. 1991). In addition, TEMP is thought to be affected by both sympathetic activity and parasympathetic activity because increases in skin temperature can be induced by stimulating parasympathetic activity (Ichinose 2010). This data suggests that AT induces stimulation of parasympathetic activity. In general, changes in TEMP induced by AT are rarely observed in the first session (e.g., Oka et al. 1993). However, several researchers have observed an increase in TEMP after the first AT session (Irie et al. 1996; Fukunaga et al. 1997). Moreover, skin temperature is known to be affected by metabolism and diaphoresis (Ichinose 2010). Therefore, there is room for debate regarding the relationship between changes in TEMP induced by AT and autonomic activity.
Considering the above, it is possible that SAMY levels can be used as measure of autonomic nervous system dysregulation in patients with FSS. Moreover, this index may capture change in autonomic activity throughout an AT session that are difficult to capture using cortisol. Many studies have used psychophysiological measures such as heart rate, skin conductance and TEMP to measure changes in autonomic activity caused by AT (e.g., Yamashiro et al. 1991; Oka et al. 1993, 1994; Irie et al. 1996; Fukunaga et al. 1997; Sakano et al. 1997). However, we argue that the level of SAMY is also useful as an index of changes in autonomic nervous system activity. When evaluating SAMY in this study, we considered the following methodological concerns were indicated: (1) the contribution of the salivary flow rate; (2) the use of absorbent materials for saliva collection, and; (3) the stimulation of saliva secretion by chewing (Bosch et al. 2011). We addressed the second and third concerns by choosing to use a hand-held type of salivary amylase monitor. Although we controlled the age of the participants in both group, we were not able to directly resolve variations in salivary flow rate.
Our results regarding psychological characteristics agree with our previous studies (Mutsuura et al. 2009; Kiba et al. 2013). These findings suggest that for mood disturbances such as anxiety or depression, somatosensory sensibility and alexithymia is deeply involved with the pathology of FSS.
There is no objective criterion for defining FSS (Henningsen et al. 2007). In a recent study, the diagnosis of “bodily distress syndrome” was used as a new criterion for defining FSS (Christensen et al. 2015). Although bodily distress syndrome is defined by “three or more symptoms” (Fink et al. 2007), some reviewers also include individuals with single symptoms in the FSS group (Henningsen et al. 2007). Moreover, some of the patients with FSS may be classified as somatic symptom disorders in Diagnostic and Statistical Manual of Mental Disorders 5th edition (American Psychiatric Association 2013) from the viewpoint of psychiatry. However, the symptoms of many individuals with disorders such as IBS or FMS would not fulfill the requirements of Criterion B; excessive thoughts, feelings, or behaviors related to the somatic symptoms or associated health concerns, which is necessary to diagnose somatic symptom disorders (American Psychiatric Association 2013). Therefore, in this study, we made a diagnosis based on the criteria of FSS used in our previous study (Kanbara et al. 2007) and that used in Henningsen’s study (Henningsen et al. 2007).
The performance of AT contributed to the improvement of somatic symptoms in patients with FSS. Setter’s meta-analysis (Stetter and Kupper 2002) also showed that AT is effective in addressing somatic symptoms. Moreover, several studies have reported that AT is effective in treating patients with specific diseases encompassed by FSS, such as IBS (Shinozaki et al. 2010) and tension headache (Van Dyck et al. 1991; Zitman et al. 1992; Spinhoven et al. 1992; Zsombok et al. 2003; Blanchard and Kim 2005). The results of the present study do not contradict these findings. Our study cannot be conclusive because of the small sample size, but we believe that our findings demonstrate that AT contributes to the improvement of somatic symptoms in patients with FSS as a whole.
Limitations of this Study
Whether the observed change between the baseline and post-AT measurements in patients with FSS was a result of AT alone is debatable because we did not use a waiting-list control group of patients with FSS.
Moreover, our sample size was small and the diagnoses of patients were uneven. The pathology of FSS will become clearer via examination of larger populations.
In the present study, we selected patients for whom physicians specializing in psychosomatic medicine predicted that AT would be effective. Thus, our participant selection process was potentially biased.
In the present study, some of the patients had multiple diagnoses, given that FSS is a diverse syndrome. In addition, we could not exclude the influences of basic medical treatment involved in medication and confounding factors other than age, sex, and alcohol consumption.
Conclusion
Sympathetic activity is increased in patients with FSS compared with healthy controls. We found that AT contributed to reduced dysregulation of the autonomic nervous system in patients with FSS, especially when the sympathetic activity of the patients was heightened. We suggest that SAMY is useful as an index of change induced by AT in patients with FSS.
References
ACOG Practice Bulletin. (2001). Premenstrual syndrome. Intenational Journal of Gynecolgy & Obstetrics, 73, 183–191.
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders, 4th ed. Text revision. Washington, DC: American Psychiatric Press.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Publishing.
Barsky, A. J., & Borus, J. F. (1999). Functional somatic syndrome. Annals Internal Medicine, 130, 910–921.
Blanchard, E. B., & Kim, M. (2005). The effect of the definition of menstrually-related headache on the response to biofeedback treatment. Applied Psychophysiology and Biofeedback, 30(1), 53–63.
Bosch, J. A., Brand, H. S., Ligtenberg, T. J., Bermond, B., Hoogstraten, J., & Nieuw Amerongen, A. V. (1996). Psychological stress as a determinant of protein levels and salivary-induced aggregation of streptococcus gordonii in human whole saliva. Psychosomatic Medicine, 58(4), 374–382.
Bosch, J. A., de Geus, E. J., Veerman, E. C., Hoogstraten, J., & Nieuw Amerongen, A. V. (2003). Innate secretory immunity in response to laboratory stressors that evoke distinct patterns of cardiac autonomic activity. Psychosomatic Medicine, 65(2), 245–258.
Bosch, J. A., Ring, C., De Geus, E. C., Veerman, E. C. I., & Amerongen, A. V. N. (2002). Stress and secretory immunity. International Review of Neurobiology, 52, 213–253.
Bosch, J. A., Veerman, E. C., de Geus, E. J., & Proctor, G. B. (2011). α-Amylase as a reliable and convenient measure of sympathetic activity: Don’t start salivating just yet! Psychoneuroendocrinology, 36, 449–453.
Christensen, S. S., Frostholm, L., Ørnbøl, E., & Schröder, A. (2015). Changes in illness perceptions mediated the effect of cognitive behavioural therapy in severe functional somatic syndromes. Journal of Psychosomatic Research, 78, 363–370.
Collet, L., Cottraux, J., & Juenet, C. (1986). GSR feedback and schultz relaxation in tension headaches: A comparative study. Pain, 25(2), 205–213.
Fink, P., Toft, T., Hansen, M. S., Ørnbøl, E., & Olesen, F. (2007). Symptoms and syndromes of bodily distress: An exploratory study of 978 internal medical, neurological, and primary care patients. Psychosomatic Research, 69, 30–39.
Fukuda, K., Staus, S. E., Hickie, I., Sharpe, M. C., Dobbins, J. G., & Komaroff, A. (1994). The chronic fatigue syndrome: A comprehensive approach to its definition and study. International chronic fatigue syndrome study group. Annals of Internal Medicine, 121(12), 953–959.
Fukunaga, M., Takebayashi, N., Fujita, M., & Nakai, Y. (1997). The effects of ten session of group autogenic training on the skin temperature. Japanese Journal of Psychosomatic Medicine, 37(7), 511–517.
Giesecke, T., Williams, D. A., Harris, R. E., Cupps, T. R., Tian, X., Tian, T. X., et al. (2003). Subgrouping of fibromyalgia patients on the basis of pressure-pain thresholds and psychological factors. Arthritis and Rheumatology, 48(10), 2916–2922.
Grillon, C., Duncko, R., Covington, M. F., Kopperman, L., & Kling, M. A. (2007). Acute stress potentates anxiety in humans. Biological Psychiatry, 62, 1183–1186.
Hatta, H., Higashi, A., Yashiro, H., Ozawa, K., Hayashi, K., Kiyota, K., et al. (1998). A validation of the Hospital Anxiety and Depression Scale. Japanese Journal of Psychosomatic Medicine, 38(5), 309–315.
Henningsen, P., Zimmermann, T., & Sattel, H. (2003). Medically unexplained physical symptoms, anxiety, and depression: A meta-analytic review. Psychosomatic Medicine, 65(4), 528–533.
Henningsen, P., Zipfel, S., & Herzog, W. (2007). Management of functional somatic syndromes. Lancet, 369, 946–955.
Ichinose, M. (2010). Physiological parameter in human and its evaluation. Japanese Journal of Biofeedback Research, 37(2), 109–115.
Ioannou, S., Gallese, V., & Merla, A. (2014). Thermal infrared imaging in psychophysiology: Potentialities and limits. Psychophysiology, 51, 951–963.
Irie, M., Mishima, N., & Nagata, S. (1996). Psychophysiological effect of first-time autogenic training on healthy beginners. Japanese Journal of Psychosomatic Medicine, 36(4), 299–305.
Kanbara, K., & Fukunaga, M. (2009). The pathology of functional somatic syndrome. Nippon Rinsho Japanese Journal of Clinical Medicine, 67(9), 1669–1675.
Kanbara, K., Fukunaga, M., Mutsuura, H., Takeuchi, H., Kitamura, K., & Nakai, Y. (2007). An exploratory study of subgrouping of patients with functional somatic syndrome based on the psychophysiological stress response: Its relationship with moods and subjective variables. Psychosomatic Medicine, 69, 158–165.
Kanbara, K., Mitani, Y., Fukunaga, M., Ishino, S., Takebayashi, N., & Nakai, Y. (2004). Paradoxical results of psychophysiological stress profile in functional somatic syndrome: Correlation between subjective tension score and objective stress response. Applied Psychophysiology and Biofeedback, 29(4), 255–268.
Kanji, N., White, A. R., & Ernst, E. (2006). Autogenic training for tension type headaches: A systematic review of controlled trials. Complement Therapies in Medicine, 14(2), 144–150.
Kasai, H. (2012). History and evolution of autogenic training. Japanese Journal of Psychosomatic Medicine, 52(1), 12–18.
Keel, P. J., Bodoky, C., Gerhard, U., & Müller, W. (1998). Comparison of integrated group therapy and group relaxation training for fibromyalgia. The Clinical Journal of Pain, 14(3), 232–238.
Kiba, T., Kanbara, K., Yamamoto, K., Ban, I., Oka, Y., Kato, F., et al. (2013). The relationship of pre-stress α-amylase levels to alexithymia in patients with functional somatic syndrome. Japanese Journal of Psychosomatic Medicine, 53(7), 670–681.
Koike, Y., Monju, T., Toda, M., & Ohta, F. (1979). Diagnosis “ex juvantibus” for patients of foreign-body sensation in the throat. The Oto-rhino-and Laryngological Clinic, 72(11), 1499–1506.
Komai, G., Maeda, M., Arimura, T., Nakata, A., Shinoda, H., Ogata, I., et al. (2003). The reliability and factorial validity the Japanese version of the 20-item Toronto Alexithymia Scale (TAS-20). Japanese Journal of Psychosomatic Medicine, 43(12), 839–846.
Last, A. R., & Hulbert, K. (2009). Chronic low back pain: Evaluation and management. American Family Physician, 79(12), 1067–1074.
Longstreth, G. F., Thompson, W. G., Chey, W. D., Houghton, L. A., Mearin, F., & Spiller, R. C. (2006). Functional bowel disorders. C1. Irritable bowel syndrome. Ganstoenteolory, 130, 1480–1481.
Luthe, W., & Schultz, J. H. (1969). Autogenic therapy 2. New York: Grune and Stratton Inc.
Matsuoka, Y. (2012). Application of autogenic training in psychosomatic disease. Japanese Journal of Psychosomatic Medicine, 52(1), 32–37.
Mitani, S., Fujita, M., Sakamoto, S., & Shirakawa, T. (2006). Effect of autogenic training on cardiac autonomic nervous activity in high-risk fire service worker for posttraumatic stress disorder. Journal of Psychosomatic Research, 60(5), 439–444.
Mizuno, Y., Yamaguchi, M., & Yoshida, H. (2001). Is saliva an index for stress level? Japanese Journal of Medical Electronics and Biological Engineering, 39(3), 234–239.
Murakami, M., Tahara, Y., Takeda, K., & Yamaguchi, M. (2009). Psychosomatic stress and salivary amylase activity in junior high school student. Transaction of Japanese Society for Medical and Biological Engineering, 47(2), 166–171.
Mutsuura, H., Kanbara, K., Fukunaga, M., Yamamoto, K., Ban, I., Kitamura, K., et al. (2009). Depression and anxiety correlate differently with salivary free cortisol in the morning in patients with functional somatic syndrome. Applied Psychophysiology and Biofeedback, 34(4), 291–298.
Nakao, M., Kumano, H., Kuboki, T., & Barsky, A. J. (2001). Reliability and validity of the Japanese version of Somatosensory Amplification Scale: Clinical application to psychosomatic illness. Japanese Journal of Psychosomatic Medicine, 41(7), 539–547.
Nater, U. M., Rohleder, N., Schlotz, W., Ehlert, U., & Kirschbaum, C. (2007). Determinants of the diurnal course of salivary alpha-amylase. Psychoneuroendocrinology, 32(4), 392–401.
Nimnuan, C., Rabe-Hesketh, S., Wessely, S., & Hotopf, M. (2001). How many functional somatic syndromes? Journal of Psychosomatic Research, 51(4), 549–557.
Noto, Y., Sato, T., Kudo, M., Kurata, K., & Hirota, K. (2005). The relationship between salivary biomarker and state-trait anxiety inventory score under mental arithmetic stress: a pilot study. Anesthesia and Analgesia, 101(6), 1873–1876.
Oka, T., Handa, M., Matsuoka, Y., & Nakagawa, T. (1994). The effect of autogenic training on vagal nervous function. Japanese Journal of Autogenic Therapy, 14(1–2), 1–9.
Oka, T., & Koyama, H. (2012). Psychophysiological effects of autogenic training and its effectiveness for stress-related psychosomatic diseases. Japanese Journal of Psychosomatic Medicine, 52(1), 25–31.
Oka, T., Matsuoka, Y., Mishima, N., & Nakagawa, T. (1993). The effect of autogenic training on the autonomic nervous function: An analysis of CVR-R, Microvibration and CVWH100. Japanese Journal of Psychosomatic Medicine, 33(4), 293–300.
Okifuji, A., & Turk, D. C. (2002). Stress and psychophysiological dysregulation in patients with fibromyalgia syndrome. Applied Psychophysiology and Biofeedback, 27(2), 129–141.
Palanisamy, K., Murugappan, M., & Yaacob, S. (2012). Descriptive analysis of skin temperature variability of sympathetic nervous system activity in stress. Journal of Physical Therapy Science, 24(12), 1341–1344.
Sakano, Y., Sato, K., & Nishizaki, T. (1997). Fluctuation of autogenic responses and characteristics of psychological changes through autogenic training. Japanese Journal of Autogenic Therapy, 16(2), 34–45.
Schultz, J. H., & Luthe, W. (1969). Autogenic therapy 1. New York: Grune and Stratton Inc.
Schulz, J. H. (1932). Das autogene training: Konzentrative Selbstentspannung. Stuttgart: Thieme Verlag.
Shigeno, K., Fukusaki, C., Ohtani, M., & Kobayashi, K. (2009). Effects of hyperoxic inhalation on psychological stress-induce salivary biomarkers. Biomedical Research, 30(4), 245–249.
Shinozaki, M., Kanazawa, M., Kano, M., Endo, Y., Nakaya, N., Hongo, M., et al. (2010). Effect of autogenic training on general improvement in patients with irritable bowel syndrome: A randomized controlled trial. Applied Psychophysiology and Biofeedback, 35(3), 189–198.
Speirs, R. L., Herring, J., Cooper, W. D., Hardy, C. C., & Hind, C. R. K. (1974). The influence of sympathetic activity and isoprenaline on the secretion of amylase from the human parotid gland. Archives Oral Biology, 19, 747–752.
Spinhoven, P., Linssen, A. C., Van Dyck, R., & Zitman, F. G. (1992). Autogenic training and self-hypnosis in the control of tension headache. General Hospital Psychiatry, 14(6), 408–415.
Stetter, F., & Kupper, S. (2002). Autogenic training: A meta-analysis of clinical outcome studies. Applied Psychophysiology and Biofeedback, 27(1), 45–98.
Subcommittee of International Headache Society. (2004). The international classification of headache disorders (2nd ed). Cephalalgia, 24(1), 9–160.
Tack, J., Talley, N. J., Camilleri, M., Holtmann, G., Pinjin, H. U., Malagelada, J. M., et al. (2006). Functional gastroduodenal disorders. B1. Functional dyspepsia. Ganstoenteolory, 130, 1466–1468.
Tak, L. M., Cleare, A. J., Ormel, J., Manoharan, A., Kok, I. C., Wessely, S., et al. (2011). Meta-analysis and meta-regression of hypothalamic-pituitary-adrenal axis activity in functional somatic disorders. Biological Psychology, 87(2), 183–194.
Tak, L. M., & Rosmalen, J. G. (2010). Dysfunction of stress responsive systems as a risk factor for functional somatic syndromes. Journal of Psychosomatic Research, 68(5), 461–468.
Van Dyck, R., Zitman, F. G., Linssen, A. C., & Spinhoven, P. (1991). Autogenic training and future oriented hypnotic imagery in the treatment of tension headache: Outcome and process. The International Journal of Clinical and Experiental Hypnosis, 39(1), 6–23.
Veen, G., Giltay, E. J., Licht, C. M., Vreeburg, S. A., Cobbaert, C. M., Penninx, B. W., et al. (2013). Evening salivary alpha-amylase, major depressive disorder, and antidepressant use in the Netherlands Study of Depression and Anxiety (NESDA). Psychiatry Research, 208, 41–46.
Wessely, S., Nimnuan, C., & Sharpe, M. (1999). Functional somatic syndrome: One or many? Lancet, 354, 936–939.
Wewers, M. E., & Lowe, N. K. (1990). A critical review of visual analogue scales in the measurement of clinical phenomena. Research in Nursing & Health, 13(4), 227–236.
Wolfe, F., Smythe, H. A., Yunas, M. B., Bennett, R. M., Bombardier, C., Golednberg, D. L., et al. (1990). The American college of rheumatology 1990 criteria for the classification of fibromyalgia. Report of the multicenter criteria committee. Arthritis and Rheumatology, 33(2), 160–172.
Yamaguchi, M. (2007). Stress evaluation using a biomarker in saliva. The Japanese Journal of Pharmacology, 129(2), 80–84.
Yamaguchi, M., Deguchi, M., & Miyazaki, Y. (2006). The effects of exercise in forest and urban environments on sympathetic nervous activity of normal young adults. Journal of International Medical Research, 34(2), 152–159.
Yamaguchi, M., Hanawa, N., & Yoshida, H. (2007). Evaluation of novel monitor for the sympathetic nervous system using salivary amylase activity. Transactions of the Japanese Society for Medical and Biological Engineering, 45(2), 161–168.
Yamashiro, I., Shirakawa, N., & Nakajima, S. (1991). Relation between changes in body temperature and therapeutic effects with autogenic training. Japanese Journal of Autogenic Therapy, 12(1–2), 25–34.
Yokoyama, K., Araki, S., Kawakami, N., & Takeshita, T. (1990). Production of the Japanese edition of profile of mood states (POMS): Assessment of reliability and validity. Nihon Koshu Eisei Zasshi, 37(11), 913–918.
Zitman, F. G., Van Dyck, R., Spinhoven, P., & Linssen, A. C. (1992). Hypnosis and autogenic training in the treatment of tension headaches: A two-phase constructive design study with follow-up. Jounal of Psychosomatic Research, 36(3), 219–228.
Zsombok, T., Juhasz, G., Budavari, A., Vitrai, J., & Bagdy, G. (2003). Effect of autogenic training on drug consumption in patients with primary headache: an 8-month follow-up study. Headache, 43(3), 251–257.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kiba, T., Kanbara, K., Ban, I. et al. Saliva Amylase as a Measure of Sympathetic Change Elicited by Autogenic Training in Patients with Functional Somatic Syndromes. Appl Psychophysiol Biofeedback 40, 339–347 (2015). https://doi.org/10.1007/s10484-015-9303-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10484-015-9303-z