Abstract
Cortisol replacement in patients with adrenal insufficiency usually consists of hydrocortisone (HC) given orally during day time. Due to the short half-life of hydrocortisone, cortisol levels between midnight and early morning are very low in contrast to the physiological rise of cortisol serum levels during this time. We investigated whether short-term cortisol replacement during the night improves cognitive function and well-being in these patients. Fourteen patients with adrenal insufficiency were put on HC infusion between midnight and 8 a.m. They subsequently underwent neurocognitive testing to measure intellectual functioning, concentration, memory and fine motor skills. Quality of life and mood were also evaluated. All tests were repeated after 2–4 weeks during usual oral glucocorticoid replacement therapy. Blood samples were taken for cortisol, epinephrine and norepinephrine measurement. With the exception of the digit symbol test with better scoring in the oral group (p = 0.005) there were no significant differences in neurocognitive testing, vegetative functions and quality of life on the two occasions. However, a higher cortisol level was associated with a worse performance in short-term memory. Plasma epinephrine concentration was subnormal in both groups, but increased only after intravenous hydrocortisone replacement. Mimicking the physiological rise in cortisol secretion during the night in this pilot study did neither significantly affect quality of life nor cognitive performance and vegetative functions. There was no improvement in general well being. Hydrocortisone infusion during night time might improve adrenomedullary reserve in patients with adrenal insufficiency.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cortisol replacement therapy in patients with primary or secondary adrenal insufficiency usually consists of two or three hydrocortisone doses, the last dose being given at bedtime. Due to the short half-life of hydrocortisone, cortisol levels between midnight and early morning are invariably very low. This contrasts to the physiological rise in cortisol secretion during this time in healthy individuals. In addition, this regimen results in supraphysiological levels of cortisol two hours after hydrocortisone ingestion (Howlett 1997; De Vile & Stanhope 1997; Groves et al. 1988). The consequences of cortisol deficiency during night time as well as those of the temporary hypercortisolism following the ingestion of hydrocortisone are yet unknown. Possible serious side-effects are osteoporosis (Peacey et al. 1997; Wichers et al. 2000; Tauchmanová et al. 2007), diabetes (McConnell et al. 2001) and glaucoma (Li Voon Chon et al. 2001). Compared to the normal population, patients with secondary adrenal insufficiency are known to be at greater risk for cardiovascular and cerebrovascular diseases (Erfurth & Hagmar 2005; Krzyzanowska et al. 2005; Bülow et al. 1997). Moreover, hypopituitary adults on conventional replacement therapy have severe deficiency of the major circulating fuels, i.e., glucose, non-esterified fatty acids (NEFA) and 3-hydroxybutyrate, throughout most of the night. This might be due to the absence of the physiological rise in cortisol secretion which is important in the regulation of substrate availability in normal humans (Al-Shoumer et al. 1996, 1997).
Cortisol has been shown to be a major determiner of neuropsychological function. Several studies have shown that conditions in which glucocorticoids are significantly decreased or increased are associated with impairment in hippocampal dependent forms of memory (Lupien et al. 2005). It is known that additional stress doses of HC can be effective on mental and physical health (Flemming & Kristensen 1999). Studies on the behaviour of adrenalectomized animals showed that the detrimental effects of adrenalectomy were acutely reversed by administration of glucocorticoids (Micco et al. 1979, Mitchell & Meaney 1991). Moreover, Lupien et al. found that acute modulation of cortisol levels by inhibition of cortisol production in a subgroup of healthy elderly subjects impaired memory, whereas this pattern was completely reversed by subsequent administration of hydrocortisone (Lupien et al. 2005).
Al-Shoumer et al. (1997) showed an increase in circulating night time concentrations of NEFA by reproducing the physiological diurnal cortisol rhythm for the short-term in hypopituitary adults. In conclusion, current evidence suggest that even short-term cortisol substitution might have positive effects. Because cortisol replacement therapy is required lifelong, optimization is of great importance to avoid additional problems due to inadequate endocrine treatment.
The aim of the present pilot study was to evaluate whether additional cortisol replacement from midnight to early morning that mimicks the circadian rhythm improves cognitive function and well-being in patients with primary or secondary adrenal insufficiency. Moreover, the influence of nocturnal cortisol replacement on the adrenomedullary hormones epinephrine and norepinephrine was examined, as adrenocortical dysfunction adversely affects adrenomedullary catecholamine synthesis (Bornstein et al. 1999).
Subjects and Methods
Patients
Fourteen patients (11 women, 3 men, age 29–70 years) with primary or secondary adrenal insufficiency were recruited from the endocrine out-patient clinic and gave informed written consent to participate in this study. ACTH deficiency was due to pituitary adenoma in six patients, craniopharyngeoma in two patients, and Sheehan′s syndrome in one case. Three patients suffered from primary adrenal insufficiency (Addison′s disease) and two patients had been adrenalectomised for Cushing′s disease. All patients were on maintenance oral replacement therapy with hydrocortisone or cortisone acetate at a daily dose of 10.0–37.5 mg. In addition, levothyroxine, somatotropin, gonadal hormones, or desmopressin were given if appropriate.
Protocol
The study protocol is depicted in Fig. 1. Patients were hospitalised overnight (a in Fig. 1). They had been advised to take their last oral dose of hydrocortisone at 03.00 p.m. An indwelling cannula was placed in an antecubital vein.
Subjects went to bed between 22.00 and 23.00, and fasted overnight. They were put on hydrocortisone infusion between midnight and 08.00 p.m. at a dose according to Al-Shoumer et al. (1996). Table 1 shows the hydrocortisone infusion rate.
At the end of infusion blood was drawn from the opposite arm for measurement of serum cortisol as well as plasma norepinephrine and plasma epinephrine concentration (A in Fig. 1). Thereafter patients took their usual glucocorticoid dose in order to prevent a cortisol deficit during the tests, and were allowed breakfast. For evaluation of well-being at the morning of the test patients had to answer a non-standardised questionnaire containing parts of the SF-36 (QoL, quality of life, part 1, Fig. 1). They were asked about the quality of sleep, well-being at the morning of the test, pep, calmness, energy, nervousness, being down in dumps, exhaustion, tiredness, and happiness.
The second blood sample for cortisol measurement was taken half an hour later before starting neuropsychological testing (B in Fig. 1). Patients subsequently underwent standardised cognitive testing to determine intellectual functioning (Wechsler Intelligence Scale, IQ, Tewes 1997), mental flexibility (digit symbol test, DST, Tewes 1997), focussed attention (d2 letter cancellation test [LCT], Brickenkamp 2000), vigilance (VIG, Zimmermann & Fimm 2002), short-term memory (digit span test, STM, Tewes 1997), and executive function (trail-making test, TMT-A, TMT-B, Spreen & Strauss 1991).
At the end of cognitive tests the third blood sample for measurement of cortisol, epinephrine and norepinephrine was taken (C in Fig. 1).
Finally, patients were asked to answer two questionnaires to assess quality of life, which was evaluated using the SF-36 assessment tool and the Beck Depression Inventory (QoL, part 2, Fig. 1; Ware 2000; Steer et al. 2001). All tests were repeated after 2–4 weeks with the patients being on their usual oral glucocorticoid replacement therapy (b in Fig. 1). This chronological order was chosen because any bias due to the inevitable learning effect would not falsely favour the nocturnal HC replacement. After basal blood samples for cortisol, epinephrine and norepinephrine measurement had been taken at 08.00 h (A), additional blood samples were taken at 08.30 h (B, cortisol only) and 11.30 h (C). Moreover, heart rate and blood pressure were recorded before, during and after the tests on both occasions. Blood pressure measurement was performed using non-invasive auscultatory method by stethoscope and sphygmomanometer. Heart rate was taken by palpation.
The study protocol was approved by the Ethics Committee of the University of Kiel, Germany.
Laboratory Methods
Blood samples were transferred on ice immediately, centrifuged at 2500×g at 4°C for 10 min and the supernatants were stored at −20°C until analysis. Cortisol was analysed by chemiluminescence immunoassay (Immulite®, DPC Biermann, Bad Nauheim, Germany). The intra-assay precision (CV, coefficient of variation) for cortisol was 8.8% at a mean concentration of 2.7 μg/dl, 7.8% at 11.3 μg/dl, and 6.2% at 29.1 μg/dl. The corresponding values for the inter-assay CV were 10, 7.7 and 7.6%, respectively. Epinephrine and norepinephrine in plasma were analysed using high performance liquid chromatography with electrochemical detection after extraction with alumina.
The intra-assay CV for epinephrine was 11.4% at a mean concentration of 129 ng/l and 2.7% at a mean concentration of 1,053 ng/l. The inter-assay CV was 14.5% at a mean value of 86.0 ng/l and 2.9% at 488 ng/l. For norepinephrine the intra-assay CV was 8.1% at a mean concentration of 237 ng/l and 2.0% at 1,117 ng/l; the inter-assay CV was 10.5% at a mean value of 292 ng/l and 3.2% at 1,733 ng/l.
Statistical Analysis
Data are expressed as mean ± standard deviation or as median where appropriate.
Results obtained on the two occasions were compared using Student′s paired t-test in case of normally distributed data. In all other cases results were compared using the non-parametric Wilcoxon signed-ranks test. A p-value of less than 0.05 was considered significant.
Results
Biochemical Parameters
Serum Cortisol Concentrations (Fig. 2)
At the end of hydrocortisone infusion (A in Fig. 2) mean serum cortisol concentration was 18.5 ± 8.3 μg/dl and was thus within the normal range for healthy subjects. However, two patients showed supraphysiological cortisol levels (40.3 and 29.5 μg/dl, respectively). As expected, serum cortisol levels were very low in the early morning in patients on conventional oral glucocorticoid replacement therapy (2.0 ± 2.6 μg/dl, p < 0.001). One patient with Addison′s disease had a cortisol level within the normal range (11.2 μg/dl). Following oral hydrocortisone ingestion (B in Fig. 2) both groups demonstrated the expected rise in serum cortisol concentration (34.7 ± 14.6 and 21.7 ± 19.4 μg/dl, respectively, p < 0.02). At the end of the test (C in Fig. 2), serum cortisol levels were 21.9 ± 8.5 and 21.5 ± 8.5 μg/dl, respectively (not significant).
Plasma Catecholamines (Fig. 3)
Epinephrine concentrations in plasma (left panel in Fig. 3) were subnormal on both occasions and at any time of the protocol. After i. v. hydrocortisone replacement during night time, epinephrine concentrations in the early morning were not different from those found after oral therapy (7.42 vs. 8.92 ng/l, A in Fig. 3, n. s.). However, after the neurocognitive tests they increased significantly to 11.78 ± 7.61 ng/l after nocturnal hydrocortisone infusion (C in Fig. 3, p < 0.001). No such increase was seen after oral glucocorticoid replacement therapy (9.92 ± 7.73 ng/l, n. s.).
Epinephrine (left panel) and norepinephrine (right panel) plasma concentrations after hydrocortisone infusion (white columns) and on usual oral glucocorticoid replacement therapy (grey columns) before (A) and after (C) neurocognitive tests. Arrows indicate normal range for epinephrine (left) and norepinephrine (right), respectively. ** p < 0.001, * p < 0.05. Note logarithmic scale
In contrast, plasma norepinephrine concentrations (right panel in Fig. 3) were in the normal range at any time point and increased significantly from 172.14 ± 101.07 to 318.92 ± 165.84 ng/l after i. v. hydrocortisone replacement, whereas no increase was seen after oral glucocorticoid replacement therapy (from 250.07 ± 139.69 to 249.00 ± 194.35 ng/l, n. s.).
Hemodynamic Parameters
Heart rate and blood pressure showed no significant differences on both occasions, so they are not reported here.
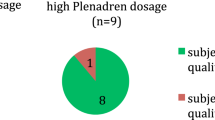
Cognitive Tests
With the exception of the digit symbol test with better scoring in the oral group (p < 0.005), results of cognitive tests were not different on the two occasions (Fig. 4).
Results of neurocognitive tests after hydrocortisone infusion (white columns) and on usual glucocorticoid replacement therapy (grey columns). IQ, intelligence quotient; DST, digit symbol test; STM, short-term memory; LCT, letter cancellation test; TMT-B, trail-making test; VIG, vigilance. Numbers on left-sided Y-axis refer to IQ-score (IQ), standard value (DST, STM, LCT) and percentage range (TMT-B). Numbers on right-sided Y-axis refer to reaction time in minutes during vigilance test
A significant negative correlation was found between cortisol levels at the time of the second blood sample and the results of “short-term memory” (r = −0.55, p < 0.047, Fig. 5). A higher cortisol level was associated with a worse performance. No such correlation was found with the other cognitive tests (data not shown).
Correlation between serum cortisol concentrations (time point B in Fig. 1, after night time hydrocortisone infusion and oral GC replacement) and short term memory. Numbers on the Y-axis refer to individual T-score of WMS. r = −0.55, p = 0.047
Quality of Life
There were no significant changes in the SF-36 assessment tool and the Beck Depression Inventory on the two occasions. Regarding well-being, pep, calmness, energy, nervousness, being down in dumps, exhaustion, happiness and tiredness after hydrocortisone infusion these differences were not significant either (Fig. 6). Quality of sleep appeared to be worse after i. v. hydrocortisone, but again, the difference was not significant (data not shown). Similarly, there were no significant correlations between the variables of quality of life and cortisol levels at the time of the first blood sample.
Discussion
Temporary hypocortisolism in patients with adrenal insufficiency might be associated with side-effects, the extent of which is not completely known. This applies especially to the nocturnal cortisol deficiency and the lack of physiological rise of this hormone in the early morning. Considering the need of lifelong cortisol substitution in these patients it is important to establish an effective cortisol replacement therapy.
A long-acting glucocorticoid given at bedtime would not sufficiently restore the physiological pattern of diurnal cortisol secretion.
By mimicking the physiological rise in cortisol secretion during the first 8 h of the day we could not observe any improvement regarding quality of life, cognitive performance, or vegetative functions. Similarly, there was no improvement in general well being. These negative findings may be due to the short duration of nocturnal cortisol substitution and the small sample size of this pilot study. Moreover, we investigated a heterogenous group of patients with regard to the underlying diseases. Patients with secondary adrenal insufficiency often suffer from additional hormone deficiencies such as growth hormone deficiency that may adversely affect mental and/or physical performance and may thus have influenced the test results. Three of the five patients with primary adrenal insufficiency reported less weariness after i.v. hydrocortisone replacement, whereas only three out of nine patients with adrenal insufficiency due to pituitary diseases did so. This may reflect the fact that patients with pituitary diseases often have an ACTH- independent residual secretion of cortisol. In addition, the oral morning dose might have caused transient hypercortisolism in some patients which might have adversely affected the results, as high glucocorticoid levels are known to impair cognitive function (Lupien et al. 2005). This is supported by our findings that a higher cortisol level at the time of the second blood sample was associated with a worse performance in short-term memory.
Apart from these limitations related to study design, the remarkable variability in cortisol concentrations following hydrocortisone infusion and oral ingestion indicates that an improved cortisol replacement regimen may be difficult to achieve. A possible explanation for the variability could be the influence of cortisol binding globulin (CBG). Approximately 80% of total cortisol is bound to CBG, and serum total cortisol levels are significantly affected by variations in CBG serum concentration (Bright & Darmaun 1995). CBG varies significantly within and between individuals (Dhillo et al. 2002; Le Roux et al. 2003) and was shown to be normal in patients with adrenal insufficiency (Coolens et al. 1987). In addition to its function as a transport protein, CBG plays an active role in determining the disposition of cortisol in humans (Bright 1995; Breuner & Orchinik 2002). The exact mechanism by which CBG is responsible for the modulation of cortisol concentration responses has not yet been identified but it is hypothesised that CBG might act by altering kinetic parameters of cortisol transport (Bright 1995). In a previous study it was shown that CBG concentration was responsible for 39% of the variance in cortisol responses to a given cortisol production rate (Bright & Darmaun 1995). Furthermore, there is a considerable interindividual variability and tissue-specific glucocorticoid (GC) sensitivity in the population due to GC receptor expression levels, intracellular GC availability, GC receptor gene polymorphism, and hormone binding affinity (Chriguer et al. 2005; Torphy & Ho 2007). These effects may also contribute to the variability of cortisol levels observed in this study. In addition, 11-beta-hydroxisteroid-dehydrogenase type 1 activity plays an important role for the modulation of GC sensitivity in a tissue- specific manner (Seckl & Walker 2004).
In view of the tight functional connection between the sympathicoadrenal and the hypothalamic-pituitary-adrenal gland system (Kvetnansky et al. 1993, 1995), we also measured catecholamine plasma concentrations before and after neurocognitive testing. Interestingly, epinephrine plasma concentrations were far beyond normal at baseline and both epinephrine and norepinephrine plasma concentration increased significantly during neurocognitive testing after iv hydrocortisone replacement, but remained unchanged when the patients were on their usual oral therapy. In contrast, epinephrine levels failed to reach the normal range in any experimental setting.
These results indicate a functional impairment of the adrenal medulla in patients with primary as well as in patients with secondary adrenal insufficiency, similar to what has been demonstrated in patients with congenital adrenal hyperplasia (Merke & Bornstein 2005). The expression of phenylethanolamine N-methyltransferase (PNMT), a key enzyme for the conversion of norepinephrine to epinephrine, is induced in the presence of glucocorticoids (Wan & Livett 1989, Wong et al. 2004). Thus, it is conceivable that intravenous GC substitution during night time is capable of augmenting the adrenomedullary reserve. The observation that epinephrine levels did not reach the normal range might indicate a chronic impairment of adrenomedullay function. It was shown in rats and mice that the development of PNMT in the periphery is dependent on maintenance of physiological levels of glucocorticoids (Bohn et al. 1986; Jeong et al. 2000; Kvetnansky et al. 2006). Therefore, adrenomedullary function might be adversely affected by prolonged periods of hypocortisolism, in particular during night time, which inevitably ensues in patients on conventional GC replacement regimens. The significant increase of norepinephrine after i. v. hydrocortisone infusion remains unexplained.
In conclusion, in this pilot study we were not able to demonstrate that night time hydrocortisone replacement improves cognitive function and quality of life in patients with primary or secondary adrenal insufficiency. In view of possible detrimental effects of chronic hypocortisolism, in particular on adrenomedullary function, it is necessary to conduct long-term studies to pursue the present approach over a longer period.
Because investigations using continuous intravenous administration of hydrocortisone are difficult to perform on a large group of patients and i. v. hydrocortisone is not suitable for long-term treatment, future studies should be planned using slow-release glucocorticoid preparations given at night time.
References
Al-Shoumer, K. A. S., Ali, K., Anyaoku, V., Niththyananthau, R., & Johnston, D. G. (1996). Overnight metabolic fuel deficiency in patients treated conventionally for hypopituitarism. Clinical Endocrinology, 45, 171–178.
Al-Shoumer, K. A. S., Anyaoku, V., Ali, K., & Johnston, D. G. (1997). Metabolic effects of short-term reproduction of the normal diurnal cortisol rhythm in hypopituitary adults. Endocrinology and Metabolism, 4, 207–214.
Bohn, M. C., Goldstein, M., & Black, I. B. (1986). Expression and development of phenylethanolamine-N-methyltransferase (PNMT) in rat brain stem: studies with glucocorticoids. Developmental Biology, 114, 180–193.
Bornstein, S. R., Tajima, T., Eisenhofer, T., Haidan, A., & Aguilera, G. (1999). Adrenomedullary function is severely impaired in 21-hydroxylase-deficient mice. FASEB Journal, 13, 1185–1194.
Breuner, C. W., & Orchinik, M. (2002). Plasma binding proteins as mediators of corticosteroid action in vertebrates. Journal of Endocrinology, 175, 99–112.
Brickenkamp, R. (2000). Test d2, Handanweisung. Göttingen: Hogrefe.
Bright, G. M. (1995). Corticosteroid-binding globulin influences kinetic parameters of plasma cortisol transport and clearance. Journal of Clinical Endocrinology and Metabolism, 80, 770–775.
Bright, G. M., & Darmaun, D. (1995). Corticosteroid-binding globulin modulates cortisol concentration responses to a given production rate. Journal of Clinical Endocrinology and Metabolism, 80, 764–769.
Bülow, B., Hagmar, L., Mikoczy, Z., Nordström, C. H., & Erfurth, E. M. (1997). Increased cerebrovascular mortality in patients with hypopituitarism. Clinical Endocrinology, 46, 75–81.
Chriguer, R. S., Elias, L. L., da Silva, I. M., Vieira, J. G., Moreira, A. C., & da Castro, M. (2005). Glucocorticoid sensitivity in young healthy individuals: In vitro and in vivo studies. Journal of Clinical Endocrinology and Metabolism, 90, 5978–5984.
Coolens, J. L., Van Baelen, H., & Heyns, W. (1987). Clinical use of unbound plasma cortisol as calculated form total cortisol and corticosteroid-binding globulin. Journal of Steroid Biochemistry, 26, 197–202.
De Vile, C. J., & Stanhope, R. (1997). Hydrocortisone replacement therapy in children and adolescents with hypopituitarism. Clinical Endocrinology (Oxford), 47, 37–41.
Dhillo, W. S., Kong, W. M., Le Roux, C. W., Alaghband-Zadeh, J., Jones, J., Carter, G., et al. (2002). Cortisol-binding globulin is important in the interpretation of dynamic tests of the hypothalamic-pituitary-adrenal axis. European Journal of Endocrinology, 146, 231–235.
Erfurth, E. M., & Hagmar, L. (2005). Cerebrovascular disease in patients with pituitary tumors. Trends in Endocrinology and Metabolism, 16, 334–342.
Flemming, T. G., & Kristensen, L. O. (1999). Quality of self-care in patients on replacement therapy with hydrocortisone. Journal of Internal Medicine, 246, 497–501.
Groves, R. W., Toms, G. C., Houghton, B. J., & Monson, J. P. (1988). Corticosteroid replacement therapy: twice or thrice daily? Journal of the Royal Society of Medicine, 81, 514–516.
Howlett, T. A. (1997). Adrenocorticotrophin deficiency: Assessment and monitoring of glucocorticoid replacement. In S. W. J. Lamberts (Ed.), The diagnosis and treatment of pituitary insufficiency (Vol. 2, pp. 81–90). Bristol: BioScientifica.
Jeong, K. H., Jacobson, L., Pacak, K., Widmaier, E. P., Goldstein, D. S., & Majzoub, J. A. (2000). Impaired basal and restraint-induced epinephrine secretion in corticotropin-releasing hormone-deficient mice. Endocrinology, 141, 1142–1150.
Krzyzanowska, K., Schnack, C., Mittermayer, F., Kopp, H. P., Hofer, M., Kann, T., et al. (2005). High prevalence of abnormal circadian blood pressure regulation and impaired glucose tolerance in adults with hypopituitarism. Experimental and Clinical Endocrinology and Diabetes, 113, 430–434.
Kvetnansky, R., Fukuhara, K., Pacak, K., Cizza, G., Goldstein, D. S., & Kopin, I. J. (1993). Endogenous glucocorticoids restrain catecholamine synthesis and release at rest and during immobilization stress in rats. Endocrinology, 133, 1411–1419.
Kvetnansky, R., Kubovcakova, L., Tillinger, A., Micutkova, L., Krizanova, O., & Sabban, E. L. (2006). Gene expression of phenylethanolamine N-methyltransferase in corticotrophin-releasing hormone knockout mice during stress exposure. Cellular and Molecular Neurobiology, 26, 735–754.
Kvetnansky, R., Pacak, K., Fukuhara, K., Viskupic, E., Hiremagalur, B., Nankova, B., et al. (1995). Sympathoadrenal system in stress. Interaction with the hypothalamic-pituitary-adrenocortical system. Annals of the New York Academy of Sciences, 771, 131–158.
Le Roux, C. W., Chapman, G. A., Kong, W. M., Dhillo, W. S., Jones, J., & Alaghband-Zadeh, J. (2003). Free cortisol index is better than serum total cortisol in determining hypothalamic-pituitary-adrenal status in patients undergoing surgery. Journal of Clinical Endocrinology and Metabolism, 88, 2045–2048.
Li Voon Chon, J. S., Sen, J., Johnson, Z., Kyle, G., & MacFarlane, I. A. (2001). Hydrocortisone replacement dosage influences intraocular pressure in patients with primary and secondary hypocortisolism. Clinical Endocrinology (Oxford), 54, 267–271.
Lupien, S. J., Fiocco, A., Wan, N., Maheu, F., Lord, C., Schramek, T., et al. (2005). Stress hormones and human memory function across the lifespan. Psychoneuroendocrinology, 30, 225–242.
McConnell, E. M., Bell, P. M., Hadden, D. R., McCance, D. R., Sheridan, B., & Atkinson, A. B. (2001). Prevalence of diabetes and impaired glucose tolerance in adult hypopituitarism on low dose oral hydrocortisone replacement therapy. Clinical Endocrinology (Oxford), 54, 593–599.
Merke, D. P., & Bornstein, S. R. (2005). Congenital adrenal hyperplasia. Lancet, 365, 2125–2136.
Micco, D. J., Jr., Mc Ewen, B. S., & Shein, W. (1979). Modulation of behavioural inhibition in appetive extinction following manipulation of adrenal steroids in rats: Implications for involvement of the hippocampus. Journal of Comparative and Physiological Psychology, 93, 323–329.
Mitchell, J. B., & Meaney, M. J. (1991). Effects of corticosterone on response consolidation and retrieval in the forced swim test. Behavioral Neuroscience, 105, 798–803.
Peacey, S. R., Guo, C. Y., Robinson, A. M., Price, A., Giles, M. A., Eastell, R., et al. (1997). Glucocorticoid replacement therapy: Are patients over treated and does it matter? Clinical Endocrinology (Oxford), 46, 255–261.
Seckl, J. R., & Walker, B. R. (2004). 11ß-hydroxysteroid dehydrogenase type 1 as a modulator of glucocorticoid action: From metabolism to memory. Trends in Endocrinology and Metabolism, 15, 418–424.
Spreen, O., & Strauss, E. (1991). A compendium of neuropsychological tests: Administration, norms and commentary. NY: Oxford University Press.
Steer, R. A., Brown, G. K., Beck, A. T., & Sanderson, W. C. (2001). Mean beck depression inventory-II scores by severity of major depressive episode. Psychological Reports, 88(3.2), 1075–1076.
Tauchmanová, L., Pivonello, R., De Martino, M. C., Rusciano, A., De Leo, M., Ruosi, C., et al. (2007). Effects of sex steroids on bone in women with subclinical or overt endogenous hypercortisolism. European Journal of Endocrinology, 157, 359–366.
Tewes, U. (1997). Der Hamburg-Wechsler-Intelligenztest für Erwachsene. 2. Göttingen:Auflage, Hogrefe.
Torphy, D. J., & Ho, J. T. (2007). Corticosteroid-binding globulin gene polymorphisms: Clinical implications and links to idiopathic chronic fatigue disorders. Clinical Endocrinology (Oxford), 67, 161–167.
Wan, D. C., & Livett, B. G. (1989). Induction of phenylethanolamine N-methyltransferase mRNA expression by glucocorticoids in cultured bovine adrenal chromaffin cells. European Journal of Pharmacology, 172, 107–115.
Ware, J. E., Jr. (2000). SF-36 health survey update. Spine, 25, 3130–3139.
Wichers, M., Springer, W., Bidlingmaier, F., & Klingmüller, D. (2000). How hydrocortisone substitution influences the quality of life and the bone metabolism of patients with secondary hypocortisolism. European Journal of Clinical Investigation, 30, 55–57.
Wong, D. L., Tai, T. C., Wong-Faull, D. C., Claycomb, R., & Kvetnansky, R. (2004). Genetic mechanisms for adrenergic control during stress. Annals of the New York Academy of Sciences, 1018, 387–397.
Zimmermann, P., & Fimm, B. (2002). A test battery for attentional performance. In M. Leclercq & P. Zimmermann (Eds.), Applied neuropsychology of attention. Theory, diagnosis and rehabilitation (pp. 110–151). London: Psychology Press.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Harbeck, B., Kropp, P. & Mönig, H. Effects of Short-Term Nocturnal Cortisol Replacement on Cognitive Function and Quality of Life in Patients with Primary or Secondary Adrenal Insufficiency: A Pilot Study. Appl Psychophysiol Biofeedback 34, 113–119 (2009). https://doi.org/10.1007/s10484-009-9082-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10484-009-9082-5