Abstract
Stressed and tense individuals often are recommended to change the way they breathe. However, psychophysiological effects of breathing instructions on respiration are rarely measured. We tested the immediate effects of short and simple breathing instructions in 13 people seeking treatment for panic disorder, 15 people complaining of daily tension, and 15 controls. Participants underwent a 3-hour laboratory session during which instructions to direct attention to breathing and anti-hyperventilation instructions to breathe more slowly, shallowly, or both were given. Respiratory, cardiac, and electrodermal measures were recorded. The anti-hyperventilation instructions failed to raise end-tidal pCO2 above initial baseline levels for any of the groups because changes in respiratory rate were compensated for by changes in tidal volume and vice versa. Paying attention to breathing significantly reduced respiratory rate and decreased tidal volume instability compared to the other instructions. Shallow breathing made all groups more anxious than did other instructions. Heart rate and skin conductance were not differentially affected by instructions. We conclude that simple and short instructions to alter breathing do not change respiratory or autonomic measures in the direction of relaxation, except for attention to breathing, which increases respiratory stability. To understand the results of breathing instructions for stress and anxiety management, respiration needs to be monitored physiologically.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recommendations for modifying breathing patterns are commonly given to individuals with ordinary stress and tension and to patients with anxiety disorders as part of cognitive-behavioral treatment, meditative approaches, or somatic therapies (Wilhelm, Gevirtz, & Roth, 2001). A common goal of breathing instructions is to counteract the fast, deep, and irregular breathing of stressed or anxious individuals. This kind of breathing can lead to hyperventilation, the hallmark of which is reduced end-tidal pCO2 (Fried, 1993; Ley, 1994). Respiratory symptoms associated with hyperventilation are abundant among the DSM-IV (American Psychiatric Association, 1994) criteria for panic attacks: Examples are sensations of shortness of breath or smothering, feeling dizzy or light-headed, and feelings of choking. Dysfunctional respiration in panic disorder (PD) is central to both Ley’s hyperventilation theory (1985) and Klein’s (1993) false alarm theory. While Ley (1985) postulates hyperventilation to be a principal cause of severe panic attacks, Klein (1993) regards the underlying pathology in PD to be a sensitivity to elevations in pCO2 which trigger a medullary suffocation alarm mechanism that stimulates breathing, leading only secondarily to hyperventilation. However, hyperventilation is not restricted to the anxiety of PD: For example, in a study of Suess et al. (1980), normal participants showed a significant decrease in pCO2, when exposed to a stressful situation.
A different goal of some breathing instructions is to focus attention and produce a special state of consciousness, which depending on the theoretical rationale, often but not always, should be a relaxed one. For example, attention to breathing is recommended in mindfulness meditation (Kabat-Zin, 1990), transcendental meditation (Russel, 2002), the production of the “relaxation response” (Benson, 1975), and certain kinds of yoga (Shaw, 2004).
A major stumbling block to evaluating the usefulness of breathing instructions has been the lack of physiological data documenting what changes in respiration actually are produced. Thus, the aim of this laboratory study was to examine the initial physiological effects of breathing instructions along with their psychological effects. We were particularly interested in whether (a) direct voluntary modification of breathing is easy, simple and pleasant, (b) direct voluntary modification of breathing works in that it reduces stress and activation and increases pCO2, and (c) raising pCO2 can be relied on to relieve tension and anxiety (which would imply that hyperventilation mediates these emotions). We chose four breathing instructions similar to those in therapy manuals, books, and online self-help pages. The instructions were given to three different groups: (a) PD patients, because some PD theories mention abnormal breathing in panic patients (Klein, 1993; Ley, 1987) and a recent study has shown that capnometry-assisted breathing therapy is effective in treating PD (Meuret, Wilhelm, Ritz, & Roth, submitted), (b) individuals who describe themselves as tense, because this group is likely to enroll in stress management courses, and (c) controls, because, unlike for psychological or clinical tests, psychophysiological measures are not well enough standardized for comparisons between studies.
Method
Inclusion criteria
Participants were recruited by advertisement in the local media. On the day of testing, subjects underwent the structured clinical interview for DSM-IV (SCID, First, Spitzer, Gibbon, & Williams, 2002). The panic group met DSM-IV diagnostic criteria for PD. The tense group (T) had to endorse the following: (1) frequent feelings of tension, (2) interference of tension with their lives or greater feelings of tension than in other people, (3) feelings of tension more than half the days during the last 6 weeks, (4) experiencing these feelings as unpleasant, and (5) interest in learning how to be less tense and to relax. Controls (C) had to feel calm most of the days in the last 6 weeks and could not meet criteria for Axis I disorders other than specific phobia. In case of specific phobia, the fearful object was not to be present during testing. We rejected applicants with current or past psychosis, cognitive impairment, or abuse or dependence on alcohol or drugs in the past year, applicants taking benzodiazepines as needed or drugs with known effects on the physiological measures of interest, and applicants with a history of relaxation or meditation practice. We included applicants taking non-tricyclic antidepressants if they were on stable doses in the month before the assessment.
Subjects
The sample consisted of 13 PD patients, 15 tense participants, and 15 controls. As noted in Table 1, groups were successfully selected to not differ in age, gender, BMI, race, or ethnicity. Twenty-three percent of PD and 60% of tense participants were taking medication, and often more than one. None of the controls were taking medication. Eight percent of PD patients were taking antidepressants (1, selective serotonin reuptake inhibitor) and 23% were taking other medication (3, analgesics; 1, antihistamine; 2, antihypertensives). Twenty percent of tense participants were taking antidepressants (1, bupropion; 2, selective serotonin reuptake inhibitors), while 47% were taking some other medication (3, analgesics; 1, antibiotic; 1, antihypertensive; 1, beta antagonist; 1 bisphosphonate; 1, nasal preparation; 1, thyroid agent). The cardiovascular data of the PD participant who took a beta-blocker and the electrodermal data of the PD participant who took an antihistamine were excluded. Additional DSM-IV diagnoses were made in 8% percent of the PD patients (1, specific phobia) and 60% of the tense participants (1, major depressive disorder; 2, posttraumatic stress disorder; 2, anxiety disorder NOS; 2, generalized anxiety disorder; 1, social anxiety disorder; 1, adjustment disorder). One participant in the control group (7%) was diagnosed with snake phobia.
Laboratory assessment
Participants reported to our laboratory for psychophysiological testing, during which they sat upright in a comfortable chair in a large, sound-attenuated, temperature-controlled, and well-lit room. The experimenter could see them through a one-way mirror and communicate with them via intercom. After the attachment of sensors, participants completed a respiration calibration procedure in which they completely inflated and deflated an 800 ml plastic bag fitted with a mouthpiece eight times, while wearing a nose clip that prevented breathing through their nose. Next participants were asked to simply relax for 8 min with their eyes open by finding a comfortable position and moving as little as possible. Then in randomized order they were asked to perform the following maneuvers, each lasting 4 minutes: (a) breathe at their usual depth and rate, counting the breath silently while inhaling and thinking the word “relax” while exhaling; counting was to alternate between going forward from 1 to 10 and backward from 10 to 1, (b) breathe at a slower pace than usual, (c) breathe shallower (inhaling less air) than usual, and (d) breathe shallower and slower than usual. During each part of the testing period, they were to keep their eyes open, move as little as possible, and to keep their mouth closed at all times, thus breathing only through their nose.
Self-report measures
Before the laboratory assessments, participants completed the Beck Depression Inventory (BDI; Beck, Ward, Mendelson, Mock, & Erbaugh, 1961), the Beck Anxiety Inventory (BAI; Beck, Epstein, Brown, & Steer, 1988), the Anxiety Sensitivity Index (ASI; Peterson & Reiss, 1992), the Penn State Worry Questionnaire (PSWQ; Meyer, Miller, Metzger, & Borkovec, 1990), and the Perceived Stress Scale (PSS; Cohen, Kamarck, & Mermelstein, 1983). The reader is referred to the original articles or practitioners’ guides of anxiety and depression questionnaires (Anthony, Orsillo, & Roemer, 2001; Nezu, Ronan, Meadows, & McClure, 2000) for more detailed information on those questionnaires. Due to experimenter error, the PSWQ and PSS were not completed by the PD group. In addition, participants completed a customized mood questionnaire after the relaxation baseline period and the four different breathing instruction periods. Participants rated their current state before and during the last minute of relaxation and breathing instructions with descriptive adjectives rated on a scale from 0, “not at all,” to 10, “extremely.” Adjectives of interest here are “tense,” “relaxed,” and “anxious.”
Physiological measures
Multiple channels of physiological data were recorded with the Biopac MP150 system (Biopac Systems Inc., Goleta, CA).
-
1.
Skin conductance was recorded at 125 Hz with the constant voltage technique from two electrodes placed at the palmar surface of the middle phalanges of digits 2 and 3 of the nondominant hand. Disposable electrodes with a circular contact area of 1 cm diameter pre-filled with isotonic gel were used. Participants were asked to wash their hands with non-antibacterial soap in preparation for the application of skin conductance electrodes. The time difference between attachment and recording was at least 20 min.
-
2.
Expiratory pCO2 was measured continuously by a calibrated infrared capnograph (N-1000, Nellcor, Hayward, CA) into which air was drawn with a flow rate of 150 ml/min through a disposable 1.2 mm diameter plastic tube ending in dual nostril prongs. The pCO2 waveform was inputted to the MP150 system via a universal interface module and sampled at 125 Hz.
-
3.
Respiratory patterns were estimated using a thoracic bellow (Lafayette Instrument, Inc., Lafayette, IN) connected to a pneumographic transducer (James Long Company, Inc., Caroga Lake, NY). The waveform was input to the MP150 system via a universal interface module and sampled at 125 Hz.
-
4.
An electrocardiogram was recorded at 250 Hz from two disposable electrodes. Electrodes were placed below the left and right collarbone. Prior to electrode attachment, participants’ skin was abraded to reduce contact impedance.
Physiological data reduction
Physiological signals were analyzed offline and averaged for 1-min periods using an integrated set of biosignal analysis programs written by the first author in MATLAB 7.0 (Mathworks, Inc., Natick, MA). Some details of the analysis are these:
-
1.
Skin conductance was resampled to 4 Hz and averaged across 1-sec segments after movement artifacts had been edited out. Non-specific fluctuations (NSFs) were defined as amplitude differences exceeding 0.02 μS between consecutive zero slopes (Vossel & Zimmer, 1990).
-
2.
End-tidal pCO2 was determined from the capnometry signal as the level at which pCO2 stopped rising at the end of an expiration (final maximum). Expirations in which the pCO2 waveform did not reach a distinct plateau were deleted and replaced by linearly interpolated values. The criterion for a distinct plateau was that in the last 0.25 sec of expiration values could not be more than 3 mmHg less than the final maximum.
-
3.
Tidal volume (TV) was calculated as the amplitude difference between peaks and valleys of valid breaths. This was calibrated in ml using data from the inflations and deflation of the fixed volume plastic bag. Respiratory rate (RR) was expressed in breaths per minute. Root mean square successive differences of respiratory rate and depth were computed as indicators of instability (respiratory rate instability [RRI], tidal volume instability [TVI]).
-
4.
Heart rate (HR) was calculated by automatic detection of R-waves followed by the calculation of successive heart periods. Artifacts in the signal were edited by inspecting the electrocardiogram data stream on a beat-by-beat basis: R-waves that had been missed by the detection algorithm were marked, and falsely detected R-waves were deleted. Respiratory sinus arrhythmia adjusted for confounds of respiratory rate and depth (RSATF) was calculated from the transfer function based on the quotient of the cross-spectral density of heart period and lung volume and the power spectral density of lung volume at the peak respiratory frequency (Saul et al., 1991). RSATF corresponds to the magnitude of rhythmic oscillations in heart rate accompanying breathing, which is related to the amount of vagal activation of the heart and parasympathetic function (Berntson et al., 1997). RSATF data were excluded if spectral coherence between TV- and RR-interval was below 0.5, because less coherence would indicate sources for RR-interval variation other than respiration (Rottenberg, Wilhelm, Gross, & Gotlib, 2002).
Statistical analysis
The groups were compared on demographic and clinical continuous variables with one-way Analyses of Variance (ANOVA) followed up by independent-samples t-tests in the case of significant group effects. χ2 tests were applied to non-ordered categorical variables.
Following the recommendation of Bagiella, Sloan, and Heitjan (2000) for analyzing psychophysiological data, mixed-effects models fitted by maximum likelihood and assuming first-order autoregressive variance covariance structures with homogenous variances were used to examine potential main effects or interactions in any self-report or physiological variables of the laboratory assessment. Factors were entered as fixed effects. For the self-report data, we computed mixed-effects models with the factors group (3 levels; PD, T, C), condition (5 levels; relaxation, four breathing instructions), and time (2 levels: at the beginning, at the end) on individual items of the customized mood questionnaires. Analogously, we computed mixed-effects models with the factors group, condition, and time (4 levels: min 1 to 4) for each of the physiological measures. Significant main effects were followed up with pairwise comparisons based on estimated marginal means. We did not adjust confidence intervals to account for multiple comparisons, but relied upon least significant differences (LSD). In the case of a significant interaction, multiple lower-order mixed-effects models were computed in order to identify the source of the effect.
The criterion for statistical significance was p ≤ .05, two-tailed. To reduce the possibility of Type I error in the many physiological measures, a small set of variables were considered to be the primary measures for testing our hypotheses (respiratory variables; end-tidal pCO2, RR, TV, RRI, TVI) while all others were considered secondary. For those primary measures, the significance level was p ≤ .05, two-tailed, for the secondary measures the probability was set at p < .01, two-tailed.
Results
Self-report measures
Table 1 depicts the scores of the ASI, BAI, BDI, PSWQ, and PSS. PD and tense participants scored significantly higher on anxiety and depression than the control group. Panic patients ranked higher on anxiety sensitivity than the tense and control groups. Tense participants rated higher on worry and perceived stress (which were not assessed in the PD participants) than controls.
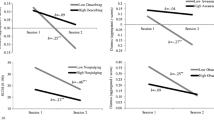
The results of the mixed-effects model analysis of the psychometric data collected during the psychophysiological assessment are summarized in Table 2. There were significant group differences in anxiety, tension, and relaxation, with PD and tense participants being more anxious and tense and less relaxed than the controls (C < T = PD). The Time × Condition interaction for anxiety was caused by an increase in anxiety during shallow and slow + shallow breathing, while the self-rating of anxiety did not change during the other conditions. Similarly, the Time × Condition interaction for relaxation was caused by a decrease in relaxation during shallow and slow + shallow breathing and an increase during meditational breathing. The self-rating of relaxation during relaxation and slow breathing did not change. For tension, there was a Group × Time × Condition interaction. Similar to the self-rating of anxiety, tension increased during shallow and slow + shallow breathing in all groups, and did not change during meditation or slow breathing. During the relaxation condition, tension decreased in the tense group while it did not change in PD participants and controls. Figures 1 and 2 depict ratings on anxiety and tension.
Physiological measures
Table 3 summarizes the results of the mixed-effects models of the physiological data during the laboratory assessment. For indicators of general emotional stress activation (HR, SCL, NSF, RSATF), there were significant time effects for electrodermal but not cardiovascular variables: SCL and NSF decreased over time, while HR and RSATF did not change. There was only one significant group effect, which was caused by higher RSATF values in the PD group than in the tense and control groups (C = T < PD).
There were time effects for all respiratory variables: End-tidal pCO2 (Fig. 3), RR (Fig. 4), and RRI increased in each condition, while TV (Fig. 5) and TVI (Fig. 6) decreased. The only respiratory group effect was found for TV, and was due to higher TVs in controls than PD patients (PD < C; PD = T; C = T). Condition effects in each of the respiratory variables indicated that the breathing instructions had an effect on breathing. Compared to simple relaxation, TV was higher during meditational and slow breathing and lower during shallow breathing. The opposite was true for RR and RRI: Compared to relaxation, RRs and RRIs were lower during meditational and slow breathing and higher during shallow breathing. The instructions to breathe slow and shallow at the same time neutralized each other: Neither TV nor RR nor RRI were significantly different from simple relaxation. The instruction to focus attention on inspiration and expiration had profound effects on TVI: TVI was near 0 ml during meditational breathing, compared to about 45 ml during relaxation. Besides this, TVI during relaxation was significantly different from TVI only during shallow breathing (relaxation > shallow breathing).
Although the breathing instructions resulted in a significant condition effect for end-tidal pCO2, post-hoc testing did not indicate that mean levels of CO2 during relaxation were different from the levels during the four breathing instructions. Still, CO2 was significantly lower during meditational and shallow breathing than during slow and slow + shallow breathing (meditation = shallow < slow = slow + shallow).
There were only two significant interactions: A Group × Condition interaction for RR suggested that the groups reacted differently to the five instructions. Visual inspection of the graphs (Fig. 4) suggested that the effect was due to higher RRs in panic patients than tense and control participants during the shallow breathing, while RRs were lower in PD patients than the other groups during slow + shallow breathing. However, the five follow-up mixed-effects models with the factor group (one model for each condition) did not indicate that RRs varied among groups. The Time × Condition interaction for TVI was due to TVI not varying during meditational and slow + shallow breathing, while TVI decreased from min 1 to 4 during relaxation, slow breathing, and shallow breathing.
Discussion
As expected, panic and tense patients scored higher on anxiety and depression than controls on the questionnaires given after the SCID interview. In addition, PD patients scored higher on anxiety sensitivity than the other groups, showing that our sample was similar to previously reported ones. The expected group effects in the self-report data from the laboratory were also confirmed: Controls were less anxious and less tense than their PD and tense counterparts. Time × Condition interactions indicated that the breathing instructions affected the psychological state differently. Most notably, shallow breathing and slow + shallow breathing made participants more anxious and tense and less relaxed than in the other three conditions. However, we found little evidence of different reactions to the breathing instructions among the three groups: There was only one interaction involving group, which was caused by self-reported tension increasing during the baseline relaxation condition in the PD group and decreasing in the tense group. One explanation for the increase in tension in the PD group may be that our PD patients perceived relaxation as dangerous and anxiety provoking (e.g., Heide & Borkovec, 1983; Heide & Borkovec, 1984). According to the suffocation false alarm theory (Klein, 1993), rising pCO2 during relaxation could induce panic anxiety in PD patients and might lead to compensatory hyperventilation.
Groups also reacted similarly in terms of physiological indicators of general emotional stress activation. Moreover, these variables did not show any condition effect of different breathing instructions. No instruction led to more deactivation of the emotional stress variables than simply sitting quietly and attempting to relax. SCL and NSFs did decline in every experimental condition, but since this was not accompanied with signs of deactivation in HR and RSATF, these declines may have reflected epidermal mechanisms not associated with emotional deactivation. The finding of greater vagal tone in PD patients than controls was surprising, since other studies have reported lower parasympathetic tone in PD than in controls (e.g., Friedman & Thayer, 1998; McCraty, Atkinson, Tomasino, & Stuppy, 2001). Our result may result from a predominance of women: Our PD sample consisted of 11 women and 2 men, and heart rate variability has been found to be higher in women than in men (e.g., Ryan, Goldberger, Pincus, Mietus, & Lipsitz, 1994).
Respiratory variables showed a number of condition effects and one group effect. End-tidal pCO2 is of particular interest because reduced CO2 from often imperceptible hyperventilation accompanies stress (e.g., Ley & Yelich, 1998; Suess et al., 1980) and thus relaxation would be expected to be accompanied by the opposite, namely, increased CO2. We indeed found that CO2 rose during each breathing instruction, thus suggesting relaxation, but no group managed to increase its CO2 to above the relaxation baseline levels even though participants did breathe slower or shallower when so instructed. Instructions to slow respiration caused all groups to do so, but CO2 did not rise because TV increased compensatorily. Similarly, instructions to breathe shallowly caused all groups to do so, but CO2 did not rise because RR rose compensatorily. RRI increased suggesting that participants had difficulty finding a comfortable breathing rate in this condition, which is supported by increases in anxiety and tension.Footnote 1 Instructions to breathe both slowly and shallowly did not cause any group to change RR, TV, or CO2, but increased discomfort like the shallow breathing condition. Focusing attention on breathing by counting reduced TVI dramatically in all groups, but did not reduce anxiety. Groups reacted to the instructions similarly with the exception of a weak Group × Condition effect for RR.
CO2 was lower during meditational and shallow breathing than during slow and slow+shallow breathing. The shallow breathing felt uncomfortable to the participants, and thus was associated with low CO2. However, the low CO2 during the meditational breathing was surprising. One explanation is that counting while breathing increased the attentional demand and therefore reduced CO2. For example, Schleifer and Ley (1994) found that CO2 was reduced during attentional demand (a PC-based task) compared to relaxation. Still, we do not understand why the reduced CO2 was not reflected in the psychometric measures of our data.
We conclude that giving simple and short breathing instructions does not change levels of emotional activation either in terms of self-report or physiological measures. Certain respiratory variables were affected as intended by these instructions, but end-tidal pCO2 did not change because changes in RR were compensated by changes in TV and vice versa. Automatic homeostatic mechanisms overrode the intended anti-hyperventilation effects of the breathing instructions. The most dramatic effect of an instruction on a physiological measure was on TVI when attention was directed towards breathing by counting. Yet, self-reported well-being was unaltered. Finally, respiratory responses to the respiratory instructions did not differ between controls, tense individuals, and PD patients. We neither found evidence for Ley’s hyperventilation theory (lower CO2 in PD patients than in the other groups) nor evidence for Klein’s suffocation false alarm theory (higher CO2 making PD patients more anxious than the other groups).
Our results force us to reject the notion that direct voluntary manipulation of breathing is easy, simple, and pleasant. Neither group managed to change its breathing in the intended way after it was given simple and short instructions. We found that the short instructions neither changed general physiological activation nor CO2 levels. In particular, physiological regulatory mechanisms for maintaining CO2 at normal levels were more potent than attempts at behavioral change. Finally, we could neither confirm nor disconfirm that raising CO2 relieves tension and anxiety because our conditions had so little effect.
It is important to realize that our conclusions are based on a rather small number of subjects. We did not perform a pilot study beforehand (for cautionary notes regarding the use of pilot studies for power calculations, see Kraemer, Mintz, Noda, Tinklenberg, & Yesavage, 2006), but simply based the number of subjects on the idea that differences not significant with a sample of this size would be unlikely to be clinically relevant. In addition, many of our PD and tense patients were medicated to make them calmer and more like control subjects. Thus, these medications tended to bias our results towards not finding group differences. Unfortunately, our small subject numbers did not give us enough power for a meaningful separate analysis of medicated and non-medicated individuals. Finally, group-based analyses such as ours may obscure the fact that in certain individuals or groups of individuals the instructions were effective. For example, subjects who found an instruction relaxing might have been the ones who could actually change their CO2 with this instruction.Footnote 2
The next step in this line of research should be to find out if other instructions or practice can accomplish greater changes. We did not try to teach people to change their breathing from thoracic to diaphragmatic since we did not think that we could do this with short verbal instructions alone. We did not test combining instructions with feedback of end-tidal pCO2, which appears to be effective after several sessions in teaching PD patients to increase their pCO2 (Meuret et al., submitted). In any case, in order to learn what breathing training for stress and anxiety can do, researchers will need to look at both cognitive-verbal and physiological measures. As is true of the rationales of other clinical interventions in psychology, breathing instructions may not work as advertised (for a discussion on the mechanisms of muscle relaxation therapy, see Conrad & Roth, 2007). Clients may be able to learn to feel relaxed after modifying the way that they breathe without showing any physiological signs of reduced emotional activation or reversal of hyperventilation. Relaxation training may work on a cognitive rather than a somatic level, which would be in line with the recent emphasis in clinical psychology on modifying pathological cognitions.
Notes
We have interpreted increased variability as a sign of discomfort because anxiety patients tend to show greater respiratory variability than controls (Wilhelm, Trabert, & Roth, 2001). On the other hand, we recognize that healthy breathing has a chaotic nature with a certain minimum variability (Boiten, Frijda, & Wientjes, 1994)
We explored this possibility by correlating (Spearman’s rho) the change scores of relaxation with the change scores of CO2 for the relaxation instruction and each breathing instruction. Of the 5 correlations, the association between relaxation and CO2 was significant only for slow breathing (ρ = 0.33, p = 0.04).
References
American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th edn.). Washington D. C.: Author.
Anthony, M. M., Orsillo, S. M., & Roemer, L. (2001). Practitioner’s guide to empirically based measures of anxiety. New York: Kluwer Academic/Plenum Publishers.
Bagiella, E., Sloan, R. P., & Heitjan, D. F. (2000). Mixed-effects models in psychophysiology. Psychophysiology, 37(1), 13–20.
Beck, A. T., Epstein, N., Brown, G., & Steer, R. (1988). An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology, 56, 893– 897.
Beck, A. T., Ward, C. H., Mendelson, M., Mock, J., & Erbaugh, J. (1961). An inventory for measuring depression. Archives of General Psychiatry, 41, 561–571.
Benson, H. (1975). The relaxation response. New York: Morrow.
Berntson, G. G., Bigger, J. T., Jr., Eckberg, D. L., Grossman, P., Kaufmann, P. G., Malik, M., et al. (1997). Heart rate variability: origins, methods, and interpretive caveats. Psychophysiology, 34(6), 623–648.
Boiten, F. A., Frijda, N. H., & Wientjes, C. J. E. (1994). Emotions and respiratory patterns: Review and critical analysis. International Journal of Psychophysiology, 17, 103–128.
Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24, 385–396.
Conrad, A., & Roth, W. T. (2007). Muscle relaxation therapy for anxiety disorders: It works but how? Journal of Anxiety Disorders, 21, 243–264.
First, M., Spitzer, R., Gibbon, M., & Williams, J. (2002). Structured clinical interview for DSM-IV-TR Axis I disorders, research version, patient edition with psychotic screen (SCID-I/P W/PSY SCREEN). New York, NY: Biometrics Research, New York State Psychiatric Institute.
Fried, R. (1993). Elements of the Anatomy and Physiology of the Respiratory System. In R. Fried (ed.), The psychology and physiology of breathing: In behavioral medicine, clinical psychology and psychiatry. New York: Plenum Press.
Friedman, B. H., & Thayer, J. F. (1998). Autonomic balance revisited: panic anxiety and heart rate variability. Journal of Psychosomatic Research, 44(1), 133–151.
Heide, F. J., & Borkovec, T. D. (1983). Relaxation-induced anxiety: Paradoxical anxiety enhancement due to relaxation training. Journal of Consulting and Clinical Psychology, 51(2), 171– 182.
Heide, F. J., & Borkovec, T. D. (1984). Relaxation-induced anxiety: Mechanisms and theoretical implications. Behaviour Research and Therapy, 22(1), 1–12.
Kabat-Zin, J. (1990). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York: Dell Publishing.
Klein, D. F. (1993). False suffocation alarms, spontaneous panics, and related conditions. An integrative hypothesis. Archives of General Psychiatry, 50(4), 306–317.
Kraemer, H. C., Mintz, J., Noda, A., Tinklenberg, J., & Yesavage, J. A. (2006). Caution regarding the use of pilot studies to guide power calculations for study proposals. Archives of General Psychiatry, 63(5), 484–489.
Ley, R. (1985). Blood, breath, and fears: A hyperventilation theory of panic attacks and agoraphobia. Clinical Psychology Review, 5, 271–285.
Ley, R. (1987). Panic disorder: A hyperventilation interpretation. In L. Micheaelson & M. Ascher (eds.), Cognitive-behavioural assessment and treatment of anxiety disorders (pp. 191–212). New York: Guilford Press.
Ley, R. (1994). Breathing and the psychology of emotion, cognition, and behavior. In B. H. Timmons (ed.), Behavioral and psychological approaches to breathing disorders. N.Y. and London: Plenum Press.
Ley, R., & Yelich, G. (1998). Fractional end-tidal CO2 as an index of the effects of stress on math performance and verbal memory of test-anxious adolescents. Biological Psychology, 49(1–2), 83–94.
McCraty, R., Atkinson, M., Tomasino, D., & Stuppy, W. P. (2001). Analysis of twenty-four hour heart rate variability in patients with panic disorder. Biological Psychology, 56(2), 131–150.
Meuret, A. E., Wilhelm, F. H., Ritz, T., & Roth, W. T. (submitted). Feedback of end-tidal pCO2 as a therapeutic approach in panic disorder.
Meyer, T. J., Miller, M. L., Metzger, R. L., & Borkovec, T. D. (1990). Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy, 28(6), 487–495.
Nezu, A. M., Ronan, G. F., Meadows, E. A., & McClure, K. S. (2000). Practitioner’s guide to empirically based measures of depression. New York: Kluwer Academic/Plenum Publishers.
Peterson, R. A., & Reiss, R. J. (1992). Anxiety Sensitivity Index Manual (2nd edn.). Worthington, OH: International Diagnostic Systems.
Rottenberg, J., Wilhelm, F. H., Gross, J. J., & Gotlib, I. H. (2002). Respiratory sinus arrhythmia as a predictor of outcome in major depressive disorder. Journal of Affective Disorders, 71(1–3), 265–272.
Russel, P. (2002). The TM technique. Las Vegas: Elf Rock Publications.
Ryan, S. M., Goldberger, A. L., Pincus, S. M., Mietus, J., & Lipsitz, L. A. (1994). Gender- and age-related differences in heart rate dynamics: are women more complex than men? Journal of the American College of Cardiology, 24(7), 1700–1707.
Saul, J. P., Berger, R. D., Albrecht, P., Stein, S. P., Chen, M. H., & Cohen, R. J. (1991). Transfer function analysis of the circulation: Unique insights into cardiovascular regulation. American Journal of Physiology, 261(4 Pt 2), H1231–1245.
Schleifer, L. M., & Ley, R. (1994). End-tidal PCO2 as an index of psychophysiological activity during VDT data-entry work and relaxation. Ergonomics, 37(2), 245–254.
Shaw, S. (2004). The little book of yoga breathing: Pranayama made easy. Boston: Red Wheel.
Suess, W. M., Alexander, A. B., Smith, D. D., Sweeney, H. W., & Marion, R. J. (1980). The effects of psychological stress on respiration: a preliminary study of anxiety and hyperventilation. Psychophysiology, 17(6), 535–540.
Vossel, G., & Zimmer, H. (1990). Psychometric properties of non-specific electrodermal response frequency for a sample of male students. International Journal of Psychophysiology, 10(1), 69–73.
Wilhelm, F. H., Gevirtz, R., & Roth, W. T. (2001). Respiratory dysregulation in anxiety, functional cardiac, and pain disorders. Assessment, phenomenology, and treatment. Behavior Modification, 25(4), 513–545.
Wilhelm, F. H., Trabert, W., & Roth, W. T. (2001). Physiologic instability in panic disorder and generalized anxiety disorder. Biological Psychiatry, 49(7), 596–605.
Acknowledgement
This research was supported by grants of the National Institutes of Health (MH066953-01) and the Department of Veterans Affairs (ROT0042825) awarded to Dr. Roth.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Conrad, A., Müller, A., Doberenz, S. et al. Psychophysiological Effects of Breathing Instructions for Stress Management. Appl Psychophysiol Biofeedback 32, 89–98 (2007). https://doi.org/10.1007/s10484-007-9034-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10484-007-9034-x