Evidence is reviewed for the efficacy of behavioral treatments for hypertension. The format chosen here is a review of reviews given that numerous consensus committee reports and quantitative reviews on the topic have been published. Extensive evidence from over 100 randomized controlled trials indicates that behavioral treatments reduce blood pressure (BP) to a modest degree, and this change is greater than what is seen in wait-list or other inactive controls. Effect sizes are quite variable. The observed BP reductions are much greater when BP levels were high at pre-test, and behavioral studies tend to underestimate possible benefits because of floor effects in their protocols. Blood pressure measured in the office may be confounded with measurement habituation. Multi-component, individualized psychological treatments lead to greater BP changes than do single-component treatments. Among biofeedback treatments, thermal feedback and electrodermal activity feedback fare better than EMG or direct BP feedback, which tend to produce null effects. There continues to be a scarcity of strong protocols that properly control for floor effects and potential measurement confounds.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Given a population prevalence of 13–30% for hypertension, the control of elevated BP is the most frequent activity of medical practitioners. With growing levels of education and easier access to medical knowledge through electronic information channels, patients have become better-informed consumers and want choices in treatment. Although there is clear evidence that antihypertensive medications are useful in controlling high BP and reduce the incidence of stroke and infarction (JNC VII, 2003; Tomiak & Gentleman, 1993), there also is a consensus that long-term drug treatment can be expensive and that side effects threaten patients’ adherence to drug prescriptions (Kaplan, 1990; Kawachi & Malcolm, 1991). In addition, the benefits of drug treatments as observed in controlled trials do not translate into similarly strong benefits in the entire treated hypertensive population: For all but the most severely hypertensive patients, treatment was associated with increased rather than decreased mortality rates in a clinical sample of 21,314 patients followed for 10 years (Thuermer, Lund-Larsen, & Tverdal, 1994).
Growing interest in non-pharmacological treatments for hypertension led to the composition of two expert panels that provided consensus positions on the effectiveness of non-pharmacological approaches in order to guide clinical practice, health care policy making, and future research (The Canadian Consensus Conference on non-pharmacological approaches to the management of high blood pressure, 1990; The Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure, 1988). Both panels reported that psychological interventions, in the form of relaxation training and stress management, had not been subjected to rigorous clinical trials and that it was premature to recommend these methods.
Subsequent reviews have criticized these consensus reports for having reviewed only a fraction of the already available, published data thus providing an incomplete and misleading picture of the evidence (Jacob, Chesney, Williams, Ding, & Shapiro, 1991; Linden, 2003; Linden & Chambers, 1994; McGrady & Linden, 2003; Spence, Barnett, Linden, Ramsden, & Taenzer, 1999). In addition to criticizing such selective sampling practices, these reviewers have argued that a comprehensive review needs to un-tease reported results with regard to critical differences in treatment type, measurement method, and patient selection criteria given that protocol differences have been shown to critically affect observable outcomes (Eisenberg et al., 1993; Linden, 2003; Linden & Chambers, 1994).
In this “review of reviews,” all available data will first be presented as a function of the different types of possible interventions and their respective, possibly differential, outcomes. Means and effect sizes [Cohen's d = (mean 1 – mean 2)/SD] are reported wherever possible. As per convention, a d = .2 will be considered small, d = .5 as moderate, and d = .8 or greater as a large effect. Next, evidence is presented that reporting of results organized only around choice of treatment technique, in the absence of a critical evaluation of the protocols themselves, can severely mislead readers in judging the true possible effects of psychological therapies. The discussion will illustrate which study features lead to overestimation and which can lead to underestimation of potential benefits of psychological treatments. For the purpose of this review, all psychological/behavioral treatments for hypertension will be considered psychophysiological in nature because (a) their target is to change a physiological parameter (blood pressure), and (b) even if biofeedback devices are not involved, the treatments have distinct psycho-somatic/psycho-physiological rationales.
Method
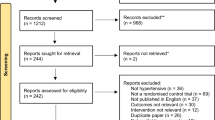
We collected all available consensus and quantitative review papers on psychological or behavioral treatments of hypertension using computer literature searches (using MedLine and PsychLit) and via search of the files of the first author who has done extensive work in this area. The search parameters were: (1) Studies published during 1990 or later (given the diligence of Jacobs et al.'s literature search up to 1991), and (2) use of combinations of the terms: “treatment,” “outcome,” “effectiveness,” “reviews,” “biofeedback,” “stress management,” “psychological therapy,” “relaxation,” “meditation.” In addition, any secondary sources identified by the first method were tracked. This resulted in a pool of four consensus reports (JNC-VII, 2003; The Canadian Consensus Conference on non-pharmacological approaches to the management of high blood pressure, 1990; The Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure, 1988; Spence et al., 1999) and eight quantitative reviews (Devine & Reifschneider, 1995; Eisenberg et al., 1993; Jacob et al., 1991; Kaufmann et al., 1988; Linden & Chambers, 1994; Nakao, Yano, Nomura, & Kuboki, 2003; Ward, Swan, & Chesney, 1987; Yucha et al., 2001). Note that no quantitative review differentially reported results for office versus home versus ambulatory BPs. We attribute this reporting pattern to the fact that almost all studies summarized in the reviews used exclusively office measures. Therefore, the reliability and validity disadvantages associated with office measures are equally applicable to the interpretation of all these reviews (JNC VII, 2003). The various reviews published and summarized here do not provide additive, independent results of different trials. To a large degree (estimated to be 2/3 of all reviewed studies; Spence et al., 1999), these reviewers are analyzing and reporting on the same studies, with however, varying selection criteria. Obviously, the more recently published trial results could not have been available to earlier reviews.
Nakao et al. (2003) reported the absolute BP changes from only those studies that had used a pre-test inclusion criterion of 140/90 mmHg or greater at pre-treatment; as such, these authors acted in synchrony with their own report of powerful effects of level of pre-treatment BP on extent of change following treatment. In order to permit easy comparison, we computed (wherever possible) the effect size d for various treatment effects. In some cases, the reviews provided means but not standard deviations for BP and we estimated the corresponding effect sizes by using a fixed set of numbers as substitute standard deviations. The substituted values reflect the average standard deviations for the pre- and post-treatment office BP values of all patients in the Linden, Lenz, and Con (2001) trial. These values were 9.8 for systolic BP and 8.4 for diastolic BP, and these figures are consistent with our experience of typical variation in BP data across various studies.
BP Reduction as a Function of Chosen Treatment Technique
The aggregation of different treatment techniques into clusters of conceptually similar approaches, requires a brief review of the rationale for psychological interventions in order to avoid comparing methods with each other that are critically dissimilar. Some of the dissatisfaction with psychological interventions for hypertension stems from the fact that it has been difficult to untangle technique-specific effects in psychotherapy from non-specific treatment effects (like hope or the quality of the therapeutic relationship). There is no widely accepted model of how psychological factors can directly “cause” high BP, and treatment rationales are not always clearly linked to underlying pathophysiology (for a discussion see Linden, 1988; or Gerin et al., 2000). Consistent with research findings that link stress to hypertension via elevated sympathetic tone and vagal dysregulation (Gerin et al., 2000; Grossman, Watkins, Wilhelm, Maolakis, & Lown, 1996; Sakakibara, Takeuchi, & Hayano, 1994, 1996), psychological treatments are designed to reduce BP by reducing stress and arousal. This is attempted via two different strategies. One approach is to emphasize physiological arousal reduction and autonomic balance through relaxation training, meditation, and/or biofeedback, all of which are designed to improve a person's autonomic, self-regulatory skills. Such methods can be taught in a standardized, manual-driven fashion, and one can package two or more methods together (for example relaxation and temperature feedback are often taught together; Jacob et al., 1991). A second approach is to conceive of stress as a multi-step process involving triggers, coping behaviors, cognitions, and physiological stress responses (Linden, 2004) that may require the teaching of a broad array of problem-solving skills. This more complex approach precludes strict adherence to a manual. Research using this second strategic approach targets deficient cognitive and behavioral stress coping skills and requires more individually tailored, multi-component interventions because the presumed critical skills deficits are not likely the same across all hypertensive patients nor are the patients’ stimulus environments presumed to be the same. The second approach also requires a higher level of skill and more training in psychological therapies for the therapist.
We are first reporting here a description of available reviews with outcomes expressed as raw mean changes and as effect sizes d for (a) pre–post behavioral treatment comparisons, and then (b) pre–post versus no treatment or wait-list control comparisons (Table I). Positive signs associated with either means or effect sizes reflect increases in BP and negative signs reflect reductions in BP (i.e., improvements). Not all cells in this table are filled because the reported outcome parameters vary across different reviews, and there is also much variety in how authors clustered intervention types into supposedly similar groups.
The data in Table I indicate that raw mean changes from pre- to post-test range from slight increases in BP due to treatment (+3.6 mmHg SBP and +2.6 mmHg DBP), to decreases of as much as −14.1 mmHg SBP and −11.1 mmHg DBP. The corresponding effects sizes range from d = +.37 and +.27 to d = −1.43 and −1.32, SBP and DBP. These numbers indicate that psychological interventions are highly variable in their potential to reduce BP and that some interventions are useless or even counterproductive. The greatest reported BP reductions, if accepted uncritically, would suggest that psychological treatment is readily comparable to the effects of drug treatment (Linden & Chambers, 1994). These summary data, however, reveal ample variation in outcomes that make it worthwhile to look for consistency in the results about comparative efficacy of different techniques. Nevertheless, drawing differential conclusions about technique-specific effects is handicapped by the fact that different reviewers use different ways of labeling and clustering techniques into groups.
The greatest variation in outcomes for techniques, which appear similar at first, is found among biofeedback interventions. All biofeedback protocols share a similar rationale; namely that skill at autonomic self-regulation can be enhanced with the simultaneous feedback of a biological signal that reflects vascular flow, muscular relaxation, and/or sympathetic activation. Interestingly, the type of biofeedback that appears to most directly target the intended endpoint, namely BP biofeedback, is consistently the least effective—cf., Jacob et al. (1991), Ward et al. (1987), and Yucha et al. (2001). A similar failure to reduce BP is reported for muscle tone biofeedback (Yucha et al., 2001). Thermal and electrodermal activity biofeedback are consistently the most effective types of biofeedback, which is intriguing because neither of these approaches directly teaches patients to change the ultimate endpoint, namely BP. Relaxation and meditation effects also vary greatly across different reviews; at times meditation is reported as more effective than relaxation (Eisenberg et al., 1993; Ward et al., 1987), but the reverse is found as well (Jacobs et al., 1991), and the associated effect sizes range from +.37/+.26 to −.66/−1.06 (SBP/DBP). Hence, to date there is no clear evidence that relaxation differs from meditation in its effect on BP, nor is there a consistent picture of the effects of even the same method. This finding parallels with observed similarities in relaxation versus meditation outcomes for other endpoints such as stress and anxiety (Linden, 2004, p. 124).
There also is a pattern across multiple reviews (Jacob et al., 1991; Linden & Chambers, 1994) that (1) technique combinations are more effective than single-technique applications, (2) ‘stress management’ (which usually is a multi-technique intervention; see Ong, Linden, and Young, 2004) produces stronger effects than simple relaxation or biofeedback interventions, and (3) individualized interventions produce significantly stronger effects than standardized treatments (Linden & Chambers, 1994).
In order to ultimately make clinical recommendations based on reviews, it will be important to separate conclusions about effectiveness of different methods relative to each other from absolute changes. We posit that the absolute outcome effect sizes and raw mean changes in BP levels are particularly important for clinical practice recommendations. Critical protocol variations in BP levels at treatment entry and different measurement choices (further discussed later) have no known effect on the comparison of relative differences of varying techniques with each other because almost all reported studies share the same weaknesses, namely low pre-treatment BP levels and a predominant choice of BP office measures. The effects of these protocol weaknesses are therefore a constant in these reviews. For this reason, and in light of the fairly consistent findings reported in Table I, we conclude that multi-component treatments and individualized treatments are more effective than single-technique interventions. However, we warn against rash acceptance of the observed absolute changes described in these reviews (see Table I) as truly reflecting what psychological treatments with different selection and measurement protocols can ultimately produce.
Outcome Differences as a Function of Measurement Choices and Trial Design
There is a considerable body of evidence suggesting that the choice of BP measurement protocol greatly affects the observed treatment effects (Eisenberg et al., 1993; Jacob et al., 1991). One critical distinction is where and how often BP is sampled (i.e., physician office versus at home versus ambulatory), who measures it (i.e., physician, nurse, patient), how many samples are taken, and at what intervals samples are taken. The recommended choice is 24-hr ambulatory measurement or repeated at-home measurement following a well-defined protocol (JNC VII, 2003; National High Blood Pressure Education Program Working Group, 1990) but none of the available quantitative reviews provides separate results for ambulatory versus office measures of BP because almost all studies used office measures only. Office measures are unreliable, as they are prone to include white-coat hypertensives (i.e., those individuals who react with a large BP increase to the measurement situation itself). Also, if only office measures are taken, habituation can occur and measurement habituation can be mistaken as a treatment effect (Liu et al., 1999; Selenta, Hogan, & Linden, 2000). Given that office BPs may confound with measurement reactivity and habituation, length of baseline will affect the measured BP differences that represent pre- and post-treatment BP levels. Jacob et al. (1991) and Eisenberg et al. (1993) observed that studies with longer baselines usually started with lower BPs that were attributed to measurement habituation effects, and that studies with low initial BP levels lead to much smaller treatment responses. The larger treatment effects seen in studies with high initial office BP readings and short baselines, may then masquerade as a treatment effect.
Probably the most promising avenue for researchers to avoid the reliability and validity problems of office measures is via the use of ambulatory BP measurement (ABPM) devices, which obtain 24-hr BP averages in the natural environment. The advantages of ABPM are: (a) Much improved test–retest stability given the increased number of measures and wider sampling, and (b) a greater potential for differentiating true hypertensives from measurement-reactive patients (“white-coat” responders; Pickering et al., 1988). Given that white-coat responders do not habituate to repeated measurement, they also cannot be detected if only office measures are used (Selenta et al., 2000). Furthermore, ABPM is more clinically meaningful in that 24-hr averaged ambulatory pressures are better long-term predictors of the development of hypertension than lab resting measures (Perloff, Sokolow, & Cowan, 1983, Perloff, Sokolow, Cowan, & Juster, 1989), and averaged ambulatory BPs also relate more closely to target-organ damage and mortality outcomes than do lab measures (Parati, Pomidossi, Albini, Malaspina, & Mancia, 1987). The disadvantages of ABPM are well known, namely higher equipment cost and a more cumbersome and demanding protocol that requires additional motivation and time of the patient and research staff.
A second, even more critical feature for the observable differences in outcome, is the degree of BP elevation at the beginning of treatment. Linden and Chambers (1994) confirmed Jacob et al.'s observation that initial BP levels strongly influence the magnitude of observed treatment effects irrespective of what treatment is given. Drug therapies were initiated at significantly higher initial levels of BP than non-drug therapies, with average pressures of 154.1 versus 145.4 mmHg SBP and 101.5 versus 94.3 mmHg DBP for drug/non-drug treatments, respectively. Given that the regression coefficients for BP change as a function of initial BP level are already known, it was possible to make mathematical adjustments to observed treatment effects. After such adjustment for differences in initial BP levels, the effect sizes for non-drug therapies increased from d = −1.19 to d = −1.71 for SBP, and from d = −1.13 to d = −1.92 for DBP. These effect sizes of individualized psychological therapy matched the effect sizes of drug treatments for SBP and DBP reduction (Linden & Chambers, 1994). These findings suggest that some non-drug therapies may be quite effective, especially when these differences in pre-treatment BP levels are taken into account. This effect of a powerful impact of pre-treatment BP level on subsequent BP reduction is highly consistent across studies (see Table II), indicating that 40% of the variance in BP reductions after treatment is accounted for by initial BP level and is unrelated to treatment type.
Given prevailing beliefs about the limited efficacy of psychological treatments for hypertension (JNC VII, 2003), it is typically difficult to recruit patients with truly high BPs into non-drug studies, especially when researchers are trying to recruit via physician referral.
We are aware of only one study that systematically used high entry BP and ambulatory BP monitoring (Linden et al., 2001). While a single study cannot absolutely settle any claim for effectiveness, this study nevertheless illustrates the possibly different conclusions that would be drawn from office versus ambulatory BP studies and low versus high initial BP studies. Consistent with conclusions and recommendations from previous reviews, this clinical trial used conservative measurement strategies (e.g., ABPM as a screening tool and as study endpoint), high initial BPs, and individualized, one-on-one treatments. Men and women aged 28–75 years, with mean ambulatory BP greater than 140/90 mmHg, received 10 hr of individualized stress management training using semi-standardized treatment components. Patients were randomly assigned to either immediate treatment (n = 27) or a wait-list control group (n = 33). Participants on the wait-list were subsequently offered treatment. Six months follow-up data were available from 36 of the 45 participants who completed the treatment. Measures were 24-hr mean ambulatory BP, lipid levels, weight, and psychological measures. Treatment led to a significant reduction in BP, whereas BP remained unchanged in control subjects ( interventions.
CONCLUSIONS AND RECOMMENDATIONS
Very much contrary to the conclusions drawn by early consensus committees (JNC VII, 2003; The Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure, 1988) there appears to be a rich body of randomized controlled trials of psychological treatments for hypertension that permits a variety of clinically relevant conclusions. When all studies are aggregated and quantitatively reviewed without consideration for critical protocol differences, the behavioral treatments produce moderately reliable effects, in the neighborhood of 6–10 mmHg BP reduction for pre–post comparisons (Linden & Chambers, 1994). Slightly lower values are observed when psychological interventions are compared to wait-list or other minimal attention controls. Effects appear to be significantly larger (reduction of 7–15 mmHg; Linden & Chambers, 1994) when individualized or multi-component approaches are offered. The most effective psychological treatments produce the same level of SBP reductions as do typically used antihypertensive drugs; with respect to DBP changes, however, drug effects are notably stronger (which is at least in part attributable to the fact that the drug treatment trials were initiated at higher BP levels; Linden & Chambers, 1994). To create additional context for the interpretation of these results, the reported absolute BP reductions for drug treatments averaged −16/−11 (SBP/DBP) mmHg; for other non-drug approaches, the numbers were −11/−8 mmHg for weight-reduction programs, −13/−9 mmHg for exercise programs, and −16/−8 mmHg for sodium restriction approaches (Linden & Chambers, 1994).
In addition to attesting to the efficacy of behavioral treatments for hypertension, the available results can also be considered a consensus opinion if related to the guidelines that were created by the Association for Applied Psychophysiology and Biofeedback (LaVaque et al., 2002) and that are also used by medical consensus committees (Concato, Shah, & Horwitz, 2000). Our review process itself was guided by these review principles. As such, hypertension is a clearly defined disease endpoint that can be reliably measured and confounds are well known (i.e., age, medication status, race).
The guidelines urge that classifications of claims about the usefulness of interventions should be linked to a five-step hierarchy, where Level 5 represents the strongest evidence. By definition, the existence of a single meta-analysis on therapy outcome implies that multiple randomized controlled trials have been conducted, and the presence of replicated, significant treatment effects (relative to a wait-list control condition) reflects Level 4 evidence. Our findings indicate that behavioral/psychophysiological interventions typically are superior to sham or wait-list treatments, thus unequivocally representing Level 4 evidence.
A requirement for double-blind studies cannot reasonably be adopted for psychological interventions; both patients and therapists will know that they are actively engaged in treatment. An exception to this claim is the possibility of offering sham treatments, which in pure biofeedback studies can consist of non-contingent biofeedback signals. The Nakao et al. (2003) review of biofeedback interventions indeed reveals that sham treatments lead to lesser BP reductions than active treatments, while sham treatments themselves were not inert. Claims about the presence of Level 5 evidence are equivocal for this review, as they require an investigational treatment to be superior to a sham treatment (true for biofeedback studies, Nakao et al., 2003) and/or superior to drug or other bona fide treatments. The latter is not true of biofeedback because biofeedback is not superior to drug treatments. Level 5 evidence (LaVaque et al., 2002) requires that, in at least two studies, credible sham treatments have been shown to be superior to no treatment, and that the experimental treatment is additionally superior to the sham treatment outcome. The review by Nakao et al. (2003) indicates that this level of evidence is available for some biofeedback treatments but only when compared to other bona fide biofeedback treatments. This conclusion cannot be extended to the comparison of biofeedback with drugs that produce larger effects, nor is there Level 5 evidence that biofeedback outcomes are superior to other bona fide psychological treatments. Note that all of these conclusions require that one accepts office BP readings as clinically useful.
The findings presented in Table I clearly show that psychological interventions are efficacious with typically modest-to-large effects sizes. Comparison of psychological treatments with drug treatments can serve as a test of clinical utility because pharmacological agents are considered the gold standard and have been shown to reduce morbidity and mortality (JNC-VII, 2003). The most sophisticated psychophysiological treatments, in turn, when initiated at the same level of BP as drug treatments, are likely to lead to the same clinical benefits (Linden & Chambers, 1994). However, this has not yet been subjected to a direct trial, and the true long-term effects of psychological treatments for hypertension are unknown. Hence, there continues to be a void of knowledge regarding long-term clinical utility of psychophysiological interventions. To summarize, psychological treatments meet Level 4 Evidence of Efficacy (for ambulatory and office BP).
A randomized assignment comparison of a purely psychological treatment with a frequently prescribed, known-to-be-effective drug is urgently needed. Although not directly comparable, Kostis et al.'s (1992) work is illustrative in this respect. Patients with established hypertension were randomized to receive either a multi-component non-drug package (relaxation, exercise, and nutrition counseling) or were given a standard, therapeutic dose of a known, effective antihypertensive medication (i.e., propranolol). Both treatment conditions were associated with equally large and clinically meaningful BP reductions, and the non-drug approach led to additional desirable reductions in body weight (whereas the drugs did not).
The results from the Linden et al. (2001) study, which utilized ambulatory BP endpoints and at least moderately high BP entry levels, also reaffirm that high initial BP levels are strongly predictive of large changes following treatment. In turn, this principle also applies to the typical pharmacological trial for hypertension (Linden & Chambers, 1994). Therefore, any fair comparison of various treatments for hypertension requires that all treatments start at the same BP levels. Such a requirement for pre-treatment equivalence has traditionally not been met when non-drug treatments have been tested, which leads to a co-incidental but rather critical underestimation of possible observable effects. There is a high likelihood that the Linden et al. (2001) study was more successful than previous studies because (1) white-coat hypertensives had been screened out by use of the elevated 24-hr BP inclusion criterion, and (2) the measurement habituation confound noted by Eisenberg et al. (1993) had been avoided.
Although speculative, the study of change in the psychological variables provided some clues as to the relationship between psychological and biological aspects of hypertension. At the biological level, reviewers routinely report a very high inter-correlation between SBP and DBP changes (in Linden et al., 2001 these correlation were r = .91); when one changes so does the other, and in the same direction. The relatively largest BP changes were seen in those patients who showed stress reduction and more adaptive anger coping styles. This is also consistent with other studies showing a link between BP levels and these same psychological variables (Davidson, MacGregor, Stuhr, & Gidron, 1999). It appears that successful stress reduction and changes in anger coping habits are the most promising targets for psychotherapy aimed at reducing BP. It is also noteworthy that different types of biofeedback have distinct effects on BP, with the seemingly most obvious biofeedback target, namely BP itself, being the least effective approach.
The emphasis of this review paper has been on the immediate BP response of hypertensives to psychological treatment although there is no doubt that the most critical questions relate to (a) long-term effects of such interventions, (b) ability to prevent the development or worsening of heart disease, and (c) ultimate reduction of cardiovascular mortality. The various review papers have paid little attention to the stability of benefits, and this is largely due to the relative neglect of follow-ups in the controlled trials. Existing data provide an ambiguous picture: Kaufmann et al. (1988) provided extensive follow-up information of up to 1-year that suggested that obtained BP benefits are maintained up to 9 months but then disappear at 12 months. Linden et al. (2001) conducted a 6-month follow-up and reported continuing reduction in BP at follow-up above and beyond the benefits seen at post-treatment. While there is general agreement that antihypertensive medications need to be taken continuously for maintained benefits, there is an implicit hope with psychological interventions that one bout of treatment will lead to lasting changes because patients are now presumed to be equipped with self-regulation skills. However, this hidden expectation has not been tested beyond the 12-month mark and, if anything (see Kaufmann et al., 1988), may not materialize. Repeated treatments or booster sessions may help. There is no properly conducted study to date to assess psychological treatment effects on mortality, although a study of meditation with quasi controls suggested an improved 3-year survival for meditation and mindfulness practitioners (Alexander, Chandler, Langer, Newman, & Davies, 1989). Lastly, some patients may not expect BP reductions with psychological treatments but would be happy if they could reduce or eliminate the need to take medication. We know of one such study (Shapiro, Hui, Oakley, Pasic, & Jamner, 1997) where a cognitive–behavioral treatment package yielded complete elimination of medication in 55% of the sample, compared to only 30% elimination in the control group.
CLINICAL PRACTICE GUIDELINES
We posit that this review provides convincing evidence for the relative superiority of some psychological treatment approaches over others; this claim for differential results of various treatments also applies within the somewhat more homogeneous literature on biofeedback interventions. The most effective interventions are individualized approaches, multi-component approaches, and temperature and electrodermal biofeedback. However, there is limited knowledge about the absolute changes that can be expected from psychological treatments when measurement habituation problems and floor effect problems are eliminated. In this respect, there remains a critical void in the literature and more trials with strong protocols and lengthy follow-ups are needed. Studies are also urgently needed that compare individualized with standardized treatments, provided that in both cases patients start out with equally high BP levels. Similarly, researchers need to tackle the question of whether careful pre-treatment screening of psychological predispositions can lead to differential outcomes when a variety of psychological treatment options are carefully matched to the specific presenting problems. For example, a patient with high anxiety levels would receive a different treatment than a patient with a great deal of suppressed anger.
An important consideration for actual practice is that patients cannot just be assigned to a psychological treatment; patients themselves need to agree to participate in psychological treatment, and some of them may prefer to take medication. Nevertheless, if patients were provided with promising and clear information about the benefits of psychological treatments, more of them might consider drugs to be only a second choice. Also, results from clinical trials are to some degree suspect in that patients who are willing to accept psychological therapies for hypertension are not necessarily representative of the entire hypertensive population; these patients may be particularly open to the concept of self-care.
With respect to clinical practice guidelines, the available data help to decide on choice of technique, measurement tools, and endpoints. Additional recommendations are possible but are mostly based on clinical experience and are not backed by unequivocal research findings. We suggest that psychological therapies, as first-line or additional treatment approaches for hypertensives, may be indicated when one or more of the following conditions apply:
-
1.
Medication side effects are severe.
-
2.
Life-style changes (weight loss, exercise uptake) alone are not enough to lower the BP to the normotensive range, and/or the patient needs psychological support to implement and maintain these changes.
-
3.
The patient himself/herself prefers non-drug treatment, has a specific interest in the self-regulation of physiological function, and has realistic expectations.
-
4.
The patient has a family history of hypertension and cardiovascular disease and wishes a preventive measure even if his/her BP is not sufficiently elevated to warrant drug treatment.
-
5.
The patient has a stressful life-style and has noticed a slow increase in BP over time, or sees a great deal of variability in BPs as a function of daily stress exposure.
Abbreviations
- BP:
-
blood pressure
- SBP:
-
systolic blood pressure
- DBP:
-
diastolic blood pressure
- ABPM:
-
Ambulatory blood pressure measurement
- ES:
-
(effect size d)
References
Alexander, C. N., Chandler, H. M., Langer, E. J., Newman, R. I., & Davies, J. L. (1989). Transcendental meditation, mindfulness and longevity: An experimental study with the elderly. Journal of Personality and Social Psychology, 37, 930–964.
Concato, J., Shah, N., & Horwittz, R. I. (2000). Randomized, controlled trials, observational studies, and the hierarchy of research designs. New England Journal of Medicine, 324, 1887–1892.
Davidson, K., MacGregor, M. W., Stuhr, J., & Gidron, Y. (1999). Constructive anger verbal behavior decreases resting blood pressure: A secondary analysis of a randomized controlled hostility intervention. International Journal of Behavioral Medicine, 6, 268–278.
Devine, E. C., & Reifschneider, E. (1995). A meta-analysis of the effects of psycho-educational care in adults with hypertension. Nursing Research, 44, 237–245.
Eisenberg, D. M., Delbanco, T. L., Berkey, C. S., Kaptchuk, T. J., Kupelnick, B., Kuhl, J., et al. (1993). Cognitive behavioral techniques for hypertension: Are they effective? Annals of Internal Medicine, 118, 964–972.
Gerin, W., Pickering, T. G., Glynn, L., Christenfeld, N., Schwartz, A., Carroll, D., et al. (2000). A historical context for behavioral models of hypertension. Journal of Psychosomatic Research, 48, 369–378.
Grossman, P., Watkins, L. L., Wilhelm, F. H., Maolakis, D., & Lown, B. (1996). Cardiac vagal control and dynamic responses to psychological stressors among coronary artery disease patients. American Journal of Cardiology, 78, 1424–1427.
Jacob, R. G., Chesney, M. A., Williams, D. M., Ding, Y., & Shapiro, A. P. (1991). Relaxation therapy for hyper-tension: Design effects and treatment effects. Annals of Behavioral Medicine, 13, 5–17.
JNC VII. (2003). The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. The Journal of the American Medical Association, 289, 2560–2571.
Kaplan, N. M. (1990). Clinical hypertension. Baltimore: Williams & Wilkins.
Kaufmann, P. G., Jacob, R. G., Ewart, C. K., Chesney, M. A., Muenz, L. R., Doub, N., et al. (1988). Hypertension intervention pooling project. Health Psychology, 7(Suppl), 209–224.
Kawachi, I., & Malcolm, L. A. (1991). The cost-effectiveness of treating mild-to-moderate hypertension: A reappraisal. Journal of Hypertension, 9, 199–208.
Kostis, J. B., Rosen, R. C., Brondolo, E., Taska, L., Smith, D. E., & Wilson, A. C. (1992). Superiority of nonpharmacologic therapy compared to propranolol and placebo in men with mild hypertension: A randomized, prospective trial. American Heart Journal, 123, 466–474.
LaVaque, T., Hammond, D., Trudeau, D., Monastra, V., Perry, J., Lehrer, P., et al. (2002). Template for developing guidelines for the evaluation of the clinical efficacy of psychophysiological evaluations. Applied Psychophysiology and Biofeedback, 27, 273–281.
Linden, W. (Ed.) (1988). Self-regulation theory in behavioral medicine. In Linden, W. (Ed.). Biological barriers in behavioral medicine (pp. 1–12). New York: Plenum.
Linden, W. (2003). Psychological treatment can be an effective treatment for hypertension. Preventive Cardiology, 6, 48–53.
Linden, W. (2004). Stress management: From basic science to better practice. Thousand Oaks, USA: Sage.
Linden, W., Lenz, J. W., & Con, A. H. (2001). Individualized stress management for primary hypertension: A controlled trial. Archives of Internal Medicine, 161, 1071–1080.
Linden, W., & Chambers, L. A. (1994). Clinical effectiveness of non-drug therapies for hypertension: A meta-analysis. Annals of Behavioral Medicine, 16, 35–45.
Liu, J. E., Roman, M. J., Pini, R., Schwartz, J. E., Pickering, T. G., & Devereux, R. B. (1999). Elevated ambulatory with normal clinic blood pressure (“white coat normotension”) is associated with cardiac and arterial target organ damage. Annals of Internal Medicine, 131, 564–572.
McGrady, A., & Linden, W. (2003). Hypertension. In M. S. Schwartz, & F. Andrasik (Eds.), Biofeedback: A practitioner's handbook (pp. 382–408). New York: Guilford Press.
National High Blood Pressure Education Program Working Group. (1990). Report on ambulatory blood pressure monitoring (NIH Publication No. 90-3028). Washington, DC.
Nakao, M., Yano, E., Nomura, S., & Kuboki, T. (2003). Blood pressure lowering effects of biofeedback treatment in hypertension: A meta-analysis of randomized controlled trials. Hypertension Research, 26, 37–46.
Ong, L., Linden, W., & Young, S. B. (2004) Stress management: What is it? Journal of Psychosomatic Research, 56, 133–137.
Parati, G., Pomidossi, G., Albini, F., Malaspina, D., & Mancia, G. (1987). Relationship of 24-hour blood pressure mean and variability to severity of target-organ damage in hypertension. Journal of Hypertension, 5, 93–98.
Perloff, D., Sokolow, M., Cowan, R. M., & Juster, R. P. (1989). Prognostic value of ambulatory blood pressure measurements: Further analyses. Journal of Hypertension, 7, S3–S10.
Perloff, D., Sokolow, M., & Cowan, R. (1983). The prognostic value of ambulatory blood pressures. The Journal of the American Medical Association, 249, 2792–2798.
Pickering, T. G., James, G. D., Boddie, C., Harshfield, G. A., Blank, S., & Laragh, J. H. (1988). How common is White Coat Hypertension? The Journal of the American Medical Association, 259, 225–228.
Sakakibara, M., & Hayano, J. (1996). Effect of slowed respiration on cardiac parasympathetic response to threat. Psychosomatic Medicine, 58, 32–37.
Sakakibara, M., Takeuchi, S., & Hayano, J. (1994). Effect of relaxation training on cardiac sympathetic tone. Psychophysiology, 31, 223–228.
Selenta, C., Hogan, B., & Linden, W. (2000). How often do office blood pressure measurements fail to identify true hypertension? Archives of Family Medicine, 9, 533–540.
Shapiro, D., Hui, K. K., Oakley, M. E., Pasic, J., & Jamner, L. D. (1997). Reduction in drug requirements by means of a cognitive-behavioral intervention. American Journal of Hypertension, 10, 9–17.
Spence, J. D., Barnett, P. A., Linden, W., Ramsden, V., & Taenzer, P. (1999). Recommendations on stress management. Canadian Medical Association Journal, 160, S46–S50.
The Canadian Consensus Conference on Non-Pharmacological Approaches to the Management of High Blood Pressure. (1990). Recommendations of the Canadian Consensus Conference on non-pharmacological approaches to the management of high blood pressure. Canadian Medical Association Journal, 42, 1397–1409.
The Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. (1988). The 1988 report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. Archives of Internal Medicine, 148, 1023–1038.
Thuermer, H. L., Lund-Larsen, P. G., & Tverdal, A. (1994). Is blood pressure treatment as effective in a population setting as in controlled trials? Results from a prospective study. Journal of Hypertension, 12, 481–490.
Tomiak, M., & Gentleman, J. F. (1993). Risk factors for hypertension as measured by the Canada Health Survey. Health Reports, 5, 419–430.
Ward, M. M., Swan, G. E., & Chesney, M. A. (1987). Arousal reduction treatments for mild hypertension: A meta-analysis of recent studies. In S. Julius & D. R. Bassett (Eds.), Behavioral factors in hypertension (pp. 285–302). North Holland: Elsevier.
Yucha, C. B., Clark, L., Smith, M., Uris, P., LaFleur, B., & Duval, S. (2001). The effects of biofeedback on hypertension. Applied Nursing Research, 14, 29–35.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Linden, W., Moseley, J.V. The Efficacy of Behavioral Treatments for Hypertension. Appl Psychophysiol Biofeedback 31, 51–63 (2006). https://doi.org/10.1007/s10484-006-9004-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10484-006-9004-8