Abstract
PrEP persistence, or PrEP use over time, has been shown to be short, with most PrEP users stopping within 6–12 months. Furthermore, those most vulnerable to HIV often use PrEP for shorter periods. This qualitative study explores patient, provider, and contextual factors that influence PrEP persistence. In interviews with 25 PrEP users and 18 PrEP providers in San Francisco’s safety net clinics, we analyze the perceived benefits and difficulties of taking PrEP, including structural barriers. We identify different steps in receipt of PrEP care (clinic visits and lab tests, pharmacy interactions, and medication adherence), and describe barriers and facilitators for providers and patients at each step. Our findings suggest that drop-in visits, streamlined testing, standing orders for labs, and 90-day PrEP prescriptions are highly desirable for many PrEP users. Also important are the proactive provision of adherence support and counseling, and referrals for housing, substance use, and mental health services.
Reusmen
Se ha demostrado que la persistencia de PrEP, o el uso de PrEP a lo largo del tiempo, es corto, y la mayoría de los usuarios de PrEP lo deja de tomar dentro de 6-12 meses. Además, muchas veces las personas más vulnerables al VIH usan PrEP por períodos más cortos. Este estudio cualitativo explora pacientes, proveedores y factores contextuales que influyen en la persistencia de PrEP. En entrevistas con 25 usuarios de PrEP y 18 proveedores de PrEP en las clínicas de redes de seguridad de San Francisco, analizamos los beneficios y las dificultades percibidos de tomar PrEP, incluidas las barreras estructurales. Identificamos diferentes pasos en la recepción de la atención de PrEP (visitas a clínicas y pruebas de laboratorio, interacciones de farmacia y adherencia a medicamentos) y describimos las barreras y facilitadores para proveedores y pacientes en cada paso. Nuestros hallazgos sugieren que las visitas directas, las pruebas simplificadas, las órdenes permanentes para los laboratorios y las recetas de PrEP de 90 días son muy deseables para muchos usuarios de PrEP. También es importante la provisión proactiva de apoyo y asesoramiento de adherencia, y referencias para vivienda, uso de sustancias y servicios de salud mental.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
A daily regimen of tenofovir disoproxil fumarate and emtricitabine (TDF/FTC) as pre-exposure prophylaxis (PrEP) has been shown to be highly effective in several large clinical trials, demonstration projects, and clinical cohorts [1,2,3]. Adherence to PrEP, or consistent use as prescribed [4], has been well studied. In contrast, relatively little attention has been paid to the factors that contribute to PrEP non-persistence and time to discontinuation, irrespective of consistency of use [5]. In a variety of contexts, PrEP persistence is quite short with 50 percent or more users stopping within 6–12 months [6,7,8,9,10,11,12,13,14]. Among PrEP users at the San Francisco Department of Public Health Primary Care Clinics (SFPCC), the median time on PrEP was 8.2 months. Earlier discontinuation occurred among younger users, those who identify as Black or as trans female, and those with self-reported injection drug use [15].
Discontinuation of PrEP may be appropriate for some people who are no longer at risk for HIV; however, not all patients who stop PrEP do so because of reduced risk of acquiring HIV [8]. For example, HIV incidence after stopping PrEP among patients at a clinic in Montreal was as high as in the placebo arm of the iPrEx trial, the first trial to show PrEP’s efficacy [16]. Furthermore, a recent study by the US Centers for Disease Control and Prevention showed shorter persistence among younger users, those with Medicaid vs. private insurance, and among African Americans as compared to Whites [16], which suggests that structural factors (i.e., differences in systems and places of care, or insurance type) in addition to individual factors (i.e., demographics) are important reasons for discontinuation. In addition, providers report having difficulty keeping track of their patients’ taking PrEP and ensuring that they follow the recommended PrEP guidelines [17], which includes HIV and sexually transmitted infection (STI) testing, as well as engagement in routine primary care [18]. These data highlight some of the social, structural, and clinic-based factors affecting PrEP persistence.
This qualitative study focuses on individual and contextual factors affecting both PrEP providers and users. Building on a recent quantitative analysis of PrEP users within the SFPCC [6, 15, 18], we interviewed both PrEP providers and users to explore reasons for and disparities in persistence. Specifically, we sought to understand provider difficulties tracking and supporting PrEP patients, areas where patients encountered challenges, and differences between patient and provider experiences. Additionally, we aimed to interpret difficulties in PrEP persistence in a wider context of structural barriers, as well as clinic, pharmacy, and interpersonal experiences.
Methods
Setting
PrEP initiation and follow-up within the SFPCC follow national and local practice guidelines [17, 19]. Briefly, after an initial clinical visit, patients initiate PrEP if their HIV test is negative and safety laboratory testing does not identify a medical contraindication. After their initial PrEP visit, patients pick up their medications at their preferred local pharmacy and start taking PrEP with any adherence support tools that were provided, such as pill boxes or reminder apps. Subsequently, they are expected to return for quarterly follow-up HIV, STI, and safety laboratory testing, and to see a medical provider if there are clinical concerns. Four of the 14 clinics employ an onsite PrEP navigator part-time to provide patient counseling, education, and adherence support using panel management techniques. In addition, two clinics employ a pharmacist who provides support with PrEP panel management but without active outreach and follow-up. Providers received education and clinical guidelines, but prescribing and follow-up expectations are at the discretion of the prescribing provider [17, 19]. For example, some providers only prescribed a one-month supply at a time, while others provided 12 months or more; follow-up also varied from nearly monthly to less than annually.
Sample
This analysis draws on interviews with 25 PrEP users receiving primary care through SFPCC and 18 providers who provide PrEP care. PrEP users were invited to participate via telephone, and providers were emailed. We approached 28 providers and 110 patients to interview (this includes unanswered emails and messages left on voice mail). Patients were selected from a randomly generated list of 364 PrEP users within the SFPCC and stratified by age, race/ethnicity, gender identity, and PrEP indication. Users on the list were contacted using purposive sampling in order to ensure diversity within each of these categories [6]. At least half were sampled to be African American or Latinx (participants were classified as Black or non-Black, Latinx or not Latinx) and under 30 years of age, and at least one-fifth were sampled to be transgender women. Indication for PrEP had been previously collected for this cohort by chart review and classified as in a sero-different relationship, men who have sex with men (MSM), people who inject drugs (PWID), transgender women who have sex with men (TGWSM), or high-risk heterosexual [6]. Similarly, we sampled providers with at least one PrEP patient under their care at one of the SFPCC clinics, which treat varied patient populations. Providers included family medicine, internal medicine, and pediatric physicians, advanced nurse practitioners, pharmacists, and PrEP navigators, and all had varying experience with PrEP. Interviews with PrEP users were completed in the Bridge HIV clinic in San Francisco, and provider interviews were conducted in the provider’s workplace. Interviews were semi-structured and based on a guide that was informed by the Motivational PrEP Cascade model [20], which is a transtheoretical model of change featuring five steps a patient proceeds through in getting on and staying on PrEP (Objective Identification of PrEP candidate, PrEP pre-contemplation, PrEP contemplation, PrEParation, PrEP action and initiation, PrEP maintenance). The guide was further developed through a review of the literature on PrEP uptake, adherence, and persistence [e.g. 6–8, 11, 12, 22]. The guide was then reviewed and revised periodically based on information collected in previous interviews to capture more information about emerging information and themes. Once the team decided we had reached saturation of data we ceased our outreach to participants. Ethics approval was received through the University of California, San Francisco Institutional Review Board. All participants reviewed and signed the informed consent with the interviewer.
Qualitative Analysis
The six-person research team was led by an anthropologist and included research assistants and physicians. At the conclusion of each interview, a member of the research team uploaded the audio file to a secure server and then wrote a ‘debriefing memo’ to summarize the most salient findings from the interview, which were shared with the study team. Interviews were also recorded and transcribed. A thematic approach was used in analyzing interview transcripts [21]. The 4 members of the team who participated in coding defined 37 analytic codes based on the interview guides, as well as a review of the debriefing memos to capture emerging themes. We then iteratively adapted code definitions and confirmed their consistent application in regular team meetings. Ten percent of the transcripts were double coded and compared to ensure consistent application of codes. Once coding was completed using Dedoose analytic software, the team ran code reports for 18 codes, created brief summaries of each excerpt, and then identified emergent themes in each code report. Finally, these themes were summarized for user and provider subgroups and discussed in regular meetings with a view towards identifying overarching themes relevant to PrEP persistence.
Results
Among the 25 total participants, eight identified as Black and seven as Latinx; the majority were MSM (60%) or TGWSM (20%). Participants were diverse in age (range 18–57) and received care at 13 out of 14 SFPCC clinics. At the time of the interviews, six participants reported daily PrEP use, nine reported non-daily PrEP use, and ten had discontinued PrEP.
Costs and Benefits
Both at PrEP initiation and subsequently, our interviews suggest that users continuously weigh the benefits of PrEP, which may include protection against HIV, decreased anxiety during sex, and reduced need for condoms, against the inconvenience of repeated lab, provider, and pharmacy visits and, in some cases, changes in insurance status and/or out-of-pocket costs. Participants reported a range of reasons for deciding to pause or stop using PrEP, including changes in relationship status or sexual activity, side effects, and fear of toxicity. Based on these considerations, decisions ranged from deciding not to take a pill on a given day, thereby reducing costs or the need for refills, to deciding to discontinue PrEP use completely.
One former PrEP user, a 33-year-old White MSM, expressed two common reasons for discontinuation:
I stopped, because, I guess, two reasons. One is that I got into sort of a long-term relationship, so it was like less... the value wasn’t there. And then, the second was just I was always hesitant to stay on PrEP, because just worried about putting like chemicals, drugs into my body. Like, I’m very aware of like what I put into my body… I try to eat as well as I can, organic, and so I just didn’t want something – I didn’t want to be taking something long-term that I didn’t have to. But for the period up until when I quit, I like just weighed, weighed it, and it made sense for me to be on it.
Gaps in sexual activity motivated one 37-year-old Black MSM to repeatedly pause and then finally discontinue PrEP: “If a month went by, or two months went by where I wasn’t having sex, then I would stop taking it. And I wouldn’t have sex unless I was on PrEP for at least a week. So, I stopped taking PrEP, I would probably say, like six months ago?”.
A 55-year-old Latinx MSM who subsequently seroconverted cited side effects as a reason for discontinuation: “Feels like, obviously, lots of upset stomach and horrible headaches and kind of feel[ing] weak at some point. So, I talked to my doctor and both we decide to get out of the PrEP, because it didn’t work that well for me.”
Providers, on the other hand, focused on whether their patient was at risk of HIV, whether there were any medical contra-indications to PrEP, and whether they believed the patients were able to adhere to the regimen. This evaluation was made both at PrEP initiation and when PrEP users express concerns about persisting on PrEP, including the need for continuation. Providers reported focusing primarily on short PrEP follow-up visits, ordering recommended lab tests, and addressing chronic medical conditions. Preventative and sexual health issues were generally addressed only if there was time.
Providers did recognize the challenge of taking a pill every day as a preventive measure. One clinician said: “And [the patient] said, ‘Why would I take a pill every day for something I don’t have?’ And younger patients in particular, I think, who now see HIV as not this deadly disease, but just like a chronic disease, are like ‘I would just be taking a pill if I had that.’ (laughs) Isn’t that crazy but true, for some people?” Nonetheless, providers relied primarily on their patients to reach out to them with specific concerns. Most providers reported not being aware that their patients had modified or stopped their PrEP regimens until several months later.
Contextual Factors
Participants also identified contextual factors that affected persistence, including housing instability, substance use, stigma, and mental health. Patients who were using PrEP regularly often found that sudden life changes made it difficult to prioritize taking PrEP. As one 26-year-old White male in a sero-different relationship noted, “Well, so I lost my housing, and so in the midst of all that, there’s just not going to doctor appointments…I was not really taking care of myself.”
Other participants noted that often people at risk for HIV may have suffered stigma that makes them wary of asking for help, including accessing PrEP. The 55-year-old Latinx MSM who seroconverted after stopping PrEP described the difficulty of talking about mental health and HIV for Latinx immigrants: “When you [are gay and] came from places like Mexico. It’s like the entire world is against you.” He suffered from depression, which he believed led him to pursue many sexual partners, but the stigma he had experienced around talking about mental illness and about HIV made it difficult for him to seek help.
Medical mistrust came up for a few patients. One African American transwoman described growing up in a family that did not regularly access medical care and only went to the hospital for emergencies. The gay community and Latinx communities were also described as distrusting the medical system, pharmaceutical companies, and PrEP medication itself, as one 55-year-old Latinx MSM: “I'm …asking people, how many of the Latinos really [are] taking or trust this pill.”
Some participants were able to stay on PrEP despite structural difficulties, including housing instability. A 39-year-old Black MSM/PWID living in a homeless encampment found ways of staying on PrEP: “In–in the encampment, I would…have the pill bottle thing. I mean, a pill box. And it’s like, I may forget in the morning, but sometime during the day, I’ll be like, oh, I forgot to take my pills. And they’d already be on me.”
Providers were largely aware of the complications of staying on PrEP, including the difficulty of keeping track of medication in a context of unstable housing, substance use, and/or mental health problems. As one clinician described it:
I mean they have to check all of their meds in when they go to the shelter. And so, you know, that presents a certain kind of barrier, but you know, it’s more that people’s stuff is lost or stolen if they’re out on the streets…and then, of course, you know, the looming sort of elephant in the room about substance use and how that affects sort of sense of time and… taking a pill may or may not fall in their priorities, and then underlying mental health stuff, you know. So, those are big things that come into play that sometimes interfere with starting PrEP or staying on PrEP.
Providers noted that these contextual issues increased risk for HIV but also felt that other medical and social issues took priority in their short visits. Accordingly, they suggested training pharmacists, behaviorists, or psychiatric nurses to provide PrEP. Likewise, PrEP navigators dedicated significant effort to linking clients to housing and mental health programs.
Insurance Coverage and Cost
Changes in insurance status were another major cause of disruptions or changes in PrEP persistence. The majority of patients in the SFPCC were insured through Medicaid or Healthy San Francisco, a health access program for uninsured San Franciscans, including undocumented immigrants, among others. Both programs cover the full cost of PrEP. However, delays in insurance renewals and increases in earnings could cause loss of insurance, thereby ending coverage of the cost of PrEP medication and clinical services. For example, one 27-year-old Latinx MSM had to change from SFPCC to a large health maintenance organization (HMO), increasing his deductible to $400. As a result, he was unable to pay: “And then my insurance changed. So, then that’s when my PrEP usage changed, because I was an everyday, 12:00-on-the-dot person with it. I didn’t miss it. It was fine… But when my insurance changed, I’m like, ‘Okay, this is a bit different now. Now, how am I going to get this?’” For others trying to choose an insurance provider, it could be very difficult to determine whether PrEP would be covered and what the deductible and co-pays would be because insurance sales teams are often unfamiliar with PrEP. One participant described his frustration after spending hours on the phone with insurance companies who ultimately gave him the wrong information.
In addition, providers found it difficult to know if their patients had stopped taking PrEP or changed their insurance. One clinician stated: “Because I think that happens a lot—like people start it and then we kind of lose track of them and then they stop taking it or they got new insurance, so then they ended up going to [a large HMO provider], but we didn’t know that they went, and so we just assumed they like stopped and fell off. Yeah, that’s the other hard thing about insurance changing, like people come in and out.”
Many providers assumed that their patients would be covered for the cost of PrEP services and were unaware of the barrier of maintaining insurance that some patients face. An experienced PrEP navigator we interviewed found the system inefficient and challenging: “So, yeah, there are days where I end up spending half the day like fighting with an insurance company…[I]t’s difficult – when you support that many patients, but then also knowing that [insurance] could make or break… a patient’s success on PrEP.” While insurance coverage, contextual factors, and cost–benefit analysis affect persistence throughout PrEP use, there are also specific steps in staying on PrEP that impact PrEP use.
Steps Required in PrEP Persistence
PrEP persistence consists of following three independent steps, including clinic visits with lab testing, pharmacy refills, and daily pill taking.
Clinic and Testing Visits
A dominant theme that emerged for patients and providers was the difficulty of keeping up with PrEP follow-up requirements. Providers faced several difficulties in supporting their patients persistence on PrEP, including the inability to track and efficiently communicate with them, and challenges with scheduling and obtaining lab samples. Providers who saw themselves as PrEP advocates, as well as PrEP coordinators, were often intensely involved in helping patients follow up.
For patients lacking a responsive provider and/or navigator, scheduling and communication was a significant frustration, particularly in the context of busy work schedules and other obligations. A 33-year-old White MSM told us: “Yeah. I mean, scheduling an appointment was an absolute nightmare. Like, the doctors there seem completely overworked; way, way, way too many patients. There were always people coming. Like, the waits were really long. There were always people coming in asking for appointments. They said they couldn't get them. Whenever I called to get an appointment, it was always weeks and weeks out. So, I think that was like a big, big issue.”
When asked about either telephone or video calls for follow-up visits, most patients responded positively. This appointment type was also seen as a way of keeping up with patients with housing instability because, as a 39-year-old Black MSM/PWID told us: “You know, most people, homeless, they got cell phone[s].” Given the difficulty of attending scheduled appointments and the need to be at work during clinic hours, drop-in appointments or extended hours were mentioned as an important component for PrEP care by multiple participants. As one 22-year-old Black MSM stated:
[T]he times that I am free, they're closed. And the times they're open, I'm not free, so that's just how it goes. It's just like a little bit of a cat and mouse game. But I'll go to school, and basically I’m in training from 8:30 to 3:30 - that's without homework and stuff like that. By the time I get to [youth clinic], [it's] closed. So yeah, it's kind of conflicting agendas or schedule.
In addition, most clinics offered on-site phlebotomy services, but clinics varied in their capacity to conduct phlebotomy associated with a visit or through drop-in. Patients might be required to set up separate laboratory appointments during specific hours, return to clinic on a different day and time, or go to a different clinical site altogether to have quarterly laboratory tests completed.
Scheduling was also a barrier for providers, who noted that appointments sometimes could not be made three months in advance (the interval for follow-up visits and laboratory tests for PrEP), and they speculated that high no-show rates, trainee schedules, and lack of scheduling staff may explain this policy. As a result, providers often had to rely on patients to remember to schedule their own appointments in the future, rather than scheduling the next appointment during the current visit.
Some components of the system did support follow-up. For example, providers reported receiving laboratory test results via the electronic medical records system and notifications of patient missed visits or refill requests, and these served as reminders to follow-up. One clinician stated: “I like it because it ensures that I don't have to keep track of them. (laughs) And if I forget that a patient needs their labs or things refilled and I hadn't made a follow-up appointment, there's a catch underneath me. Which I generally support, because one of my biggest fears is just missing stuff, you know?”.
Providers reported using prescription duration strategically. For example, some limited the total prescription duration to 90 days to ensure that the patient got follow-up testing. One doctor indicated: “If I do 30 days, I give them three refills. If I do 90 days, I don't generally do refills. And then I'll get a notice from the pharmacy for a refill request.” However, other providers wrote prescriptions with refills for a year on that grounds that it was more important to keep the patient on PrEP, even at the risk of delayed follow-up HIV and safety testing.
Providers also noted that, because this was a preventive medication, PrEP users were less tolerant of scheduling difficulties than patients with chronic conditions or acute illnesses, as well as less diligent in overcoming them. As one primary care doctor noted: “I'm noticing the PrEP patients may not [keep on top of appointments]. But my regular, my other patients, who are just regular…[with]other chronic diseases they could show up all—they generally show up.”
Communication between providers and their patients was often difficult. For example, incoming calls would sometimes take days to get to a provider, adversely affecting their ability to follow-up with patients over the phone. Similarly, providers reported difficulty contacting patients. One pharmacist stated:
A lot of our patients here are on the younger age group, right? In their 30s to 40s, or upper 20s. They never answer their phones. I can't really leave a message, because a lot of times it's a generic voicemail and even if it's a personal voicemail, I can't leave a message. And you just call and call and call; they don't answer.... The problem is, I'm not here every day. And I really don't have a phone number to give them. And I can't give them my office phone number, so - they can't get back to me.
To address this issue, some providers give patients their personal mobile phone numbers or email addresses. One doctor in a high-risk obstetrics clinic framed this as the only possible workaround: “I mean, yeah, scheduling is hard, because you can rarely get a clerk on the phone like in a really timely manner to schedule an appointment. So, our patients that have mine and [the RNs] cellphone, they text us all the time to like schedule an appointment, because they like literally can't get through.” However, other providers stated that such direct patient access would be overwhelming and inefficient.
Pharmacy Experiences
Patients expressed a strong preference for 90-day rather than 30-day refills. Although some pharmacies were easier to access than clinic visits and laboratory testing, trips to the pharmacy could interfere with work and school schedules, and 90-day prescriptions decreased time spent on this crucial step in staying on PrEP. A 53-year-old White male in a sero-different relationship told us: “The other thing that's a really great, great thing that optimizes the process is getting a 90-day prescription." Several participants found pharmacy refill and pickup reminders helpful. Electronic prescriptions were also desirable because it removed a step in the process. As one 27-year-old Black MSM noted, “It was really easy. I would just go to Target and just pick it up. It was usually there. I don't remember ever having to call [the doctor] to ask him for a new prescription. I think it was always just there.”
Some participants experienced stigma in pharmacies when filling their prescriptions. One explained: “So then, dealing with pharmacies. There's this whole other layer of frustration, dealing with straight people who don't know what PrEP is.” Another transwoman participant was going to be denied her PrEP because the pharmacist assumed that she was a ciswoman, and the insurance company did not see that as a sufficient PrEP indication. She had to tell staff to look back into her record to verify that she was in a high-risk group.
Others expected to experience stigma but instead felt supported by their community pharmacist. A 24-year-old Black MSM told us:
I was like I'm here to pick up my PrEP and you know the lady she's been there—she's been working there for years. So, she kind of personally knew me and my sister and my grandmother when we would pick up her allergy medicine. And she's like I remember you. And so, when I told her I was here to pick up… PrEP she was like oh yeah. You need that like—so, she gave me three pills even though she didn't see me in the system. Yeah. She's like no. You need that. You just need to make sure that you [have a prescription] …so we can get you your full doses.
Providers similarly noted that having a supportive, culturally concordant pharmacist could play a big role. They saw the pharmacy as a potential hurdle for youth who were learning a new skill and in need of coaching, given their lack of experience with insurance and filling prescriptions. PrEP navigators could help with this patient education. Providers also saw pharmacists as providing continuity, given the need for frequent PrEP refills. One provider thought PrEP should be offered at the suboxone pharmacy to meet the needs of the PWID population.
Some providers seemed unaware that patients found 30-day prescriptions inconvenient or could experience stigma at the pharmacy. However, providers did acknowledge the difficulties patients experience with insurance coverage at the pharmacy, which they found particularly troublesome and appreciated navigation help when available.
Adherence
Patients described many strategies to support daily pill taking. For example, location-based memory aids and the importance of getting into a routine were common themes. One 41-year-old White MSM said: “Well sometimes I would forget. Like a day or so. But normally I would take it in the morning. When I get up. And just have a pill out, laying out, you know? On the–on the dresser, so, a reminder.” Other participants stressed the importance of getting into a routine and having a backup plan. A 37-year-old Black MSM told us:
I got into a routine, so if I knew I was consciously doing it, I would take it out and put one in my pocket the night before I would go to work. Or whatever I would do in the morning, I would put one in my—the coin part of my pocket—and something so that I had one on me, so if I forgot to take it in the morning, I had one on me that I could take. So, it was like a backup plan to remember to take it.
Additional facilitators to PrEP adherence included having refills shipped to the home. Participants experiencing homelessness developed routines to help them adhere to PrEP, including having refills shipped to an organization that could hold the meds and then dispense them on a weekly or monthly basis. Additional aids for participants experiencing homelessness included phone apps that provide daily adherence reminders, taking PrEP along with other daily medications like Hepatitis C treatment or mental health medications, and pill boxes to store medication.
Prior experience taking a daily medication facilitated PrEP adherence. A 57-year old White MSM described how taking PrEP fit in the preexisting system that he used to take his thyroid medication:
Well, I have, because I'm taking another medicine since I was in my mid-20s, and I can't discontinue that. It's a thyroid medicine, because my thyroid doesn't work anymore. So, every morning, I get up, I go the kitchen, I take that one. Now, with the Truvada, I decided that it's better to have something in my stomach before I take it. You know, it's a big… pill. It's not little. So, I usually take [my thyroid pill] first when I have some coffee and maybe a little bit of a cheese or fruit or something, and then I take the Truvada. And then I have my breakfast. So, I take—it's easy, in the cabinet, the kitchen cabinet, another pill.
For other patients, pill taking has historically been a negative experience, and large pill size exacerbates this perception. For example, one 29-year-old Black MSM recalled starting PrEP and thinking, “At first, it was like a big old horse pill, and I was just like, ‘Oh my God.’ And I have hard time with swallowing pills all my life, and I'm getting better with it. It took a minute. I used to just chew pills.”
Providers commented on how they perceived homelessness and substance use as negatively affecting adherence among their patients. One clinician reflected on how these dynamics worked for one PrEP patient:
I think just life—disorganization, in general. Like when my one patient was homeless for a while, I think there’s so much going on. Like, how do you remember to take a pill every single day in the midst of all of that? And he's kind of all over the place, physically, in terms of being here one day, and here the next day. And so, there's not a lot of structure and routine that he had that enabled him to remember to take a pill every single day…And, also, substance use. So, he was also actively using meth pretty much every day, at that time. And so that makes it hard to remember to take a pill, too, I would imagine?
Providers consistently named the need for more adherence counseling, but they did not have time during visits to provide it routinely and suggested having a PrEP navigator, medical assistant, or nursing staff to support client adherence. Some providers described important adherence counseling strategies and messaging. One clinician emphasized the relationship between adherence and patient readiness to take a pill: “And I think one of the things I know with HIV is that we are assessing someone's stage of change, and we ask them to do something that they feel like they can't do—if we ask them at the wrong time, we hurt them.”
Providers suggested that some patients may feel ready and motivated to take PrEP but have not yet developed the necessary skills and behavior to adhere to a daily pill. As one clinician suggested, additional adherence counseling is often needed for youth: “You know, for a lot of our patients this is the first time they've taken a med every day, and dealt with anything like how do I fill a prescription, like if I run out is it just over or how do I call the pharmacy or—so there's a lot of sort of like just skill building, you know, sort of an age-appropriate skill building that they've never dealt with this before, and often times they're doing it without the knowledge of their parents or without any connection to their parents either. So, you kind of have to offer that support.”
Lastly, one provider reported that some patients have confidentiality concerns, especially if they live with family or roommates, that get in the way of daily PrEP adherence, and the provider encourages these patients to store PrEP pills in a 7-day medication organizer rather than keeping the pill bottles visible in their living or working space.
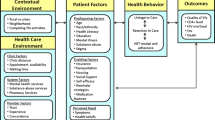
Table 1 summarizes factors affecting PrEP persistence as well as steps required for PrEP persistence, from the perspective of both providers and patients.
Discussion
In this qualitative study, we explored patient, provider, and contextual factors that influence PrEP persistence. These factors include the perceived benefits and difficulties of taking PrEP, difficulties with insurance coverage, competing priorities, and structural barriers. In particular, the contextual factors of stigma and medical mistrust were salient themes raised by Black and Latinx patients and transwomen who were oversampled in our interviews. Difficulties meeting the fairly demanding PrEP follow-up requirements, as reported by both users and providers, include scheduling and attending follow-up visits and laboratory tests, as well as communication between patients and providers. Obtaining pharmacy refills was inconvenient and alienating for some patients but supportive and culturally concordant for others. Adherence to taking a daily pill was often seen as difficult, especially for PrEP users experiencing homelessness or with substance use disorders, but adherence could be enhanced by patient-driven strategies or taught by navigators and providers.
While many of the components of PrEP persistence that we identified have been noted in the literature, this is the first analysis we are aware of that includes both provider and patient perspectives. Further, we were able to identify important overarching differences in the ways providers and patients approach PrEP persistence. For example, providers decide to start, continue, and stop PrEP based on indications (patient risk) and contraindications, as indicated by laboratory results and perceived ability to adhere. Patients, in contrast, continuously weigh the costs and benefits of PrEP, some of which are never discussed with providers. These include competing health and life priorities [22]; changes in sexual activity, as well as managing intimate relationships and changes in commitment [23, 24]; finding and maintaining insurance coverage and covering out of pocket costs [25]; side effects and perceptions of toxicity [26]; the inconvenience of PrEP follow-up guidelines [10]; and finally the difficulty and, for many young users, the unfamiliarity of daily pill-taking [27]. Our analysis indicates that patients were willing to engage with providers on these factors and valued proactive outreach from providers to discuss these decisions, particularly those being considered between clinical visits. Supporting this view, a recent study found that patients who were prescribed PrEP by attending physicians (as opposed to a trainee or mid-level physician) stayed on PrEP longer; the authors attributed this to a more stable relationship with the provider and greater provider knowledge of PrEP [28].
Another difference between providers and patients was that while risk perception was seen by providers as a primary motivator for PrEP persistence, PrEP users focused less on HIV risk than on other challenges and barriers. Further, participants did not see PrEP as the only way to navigate risk of acquiring HIV. To participants, sexual engagement is much more complex and nuanced than an assessment of HIV risk [23]. Moreover, some have argued that focusing predominantly on HIV risk in PrEP engagement may contribute to HIV and PrEP stigma and likely reinforce racial/ethnic disparities. Further, because homophobia, medical mistrust, and stigma around HIV may discourage patients from disclosing sexual behaviors and providers from asking about them, a focus on identifying PrEP candidates based on risk categorization may exclude those who might most benefit from PrEP [29]. Studies with medical trainees have suggested that providers are less likely to prescribe PrEP to people who indicated that they do not want to use condoms, especially for Black and Latinx MSM because of fears about risk compensation, as well as racism and homophobia [30,31,32]. In the United States, using sexual behavior to determine risk will also underestimate HIV risk among many groups, including Black MSM, who are at higher risk of HIV despite similar or lower individual risk behavior than non-Black MSM because of structural and sexual network factors that are driving the epidemic in these populations [33,34,35,36,37,38]. Universal education to patients about PrEP would help avoid exclusion of candidates based on assumptions about sexual preference or risk compensation. Others have argued that in order to improve access and equity, health professionals should integrate PrEP into routine preventive health care for adult patients, particularly in primary care, reproductive health, and behavioral health settings [39].
Both patients and providers reported feeling overburdened by the current clinical guidelines in PrEP follow-up. Clinical records systems are not set up to track PrEP users or to schedule their repeated laboratory tests and follow-up visits. The follow-up, pharmacy, and insurance procedures were perceived as onerous, in part by medicalizing sexual life and detracting from perceived benefits. Simplified PrEP follow-up procedures could likely reduce these barriers, such as patient-centered models using drop-in laboratory testing, home-based sample collection, and telephone-based follow-up [10, 30].
This study has some important limitations. First, it was conducted in San Francisco, which is a well-resourced city that benefits from high access to PrEP, a high proportion of insured patients, and a high density of PrEP navigators relative to other jurisdictions. This study was conducted in safety net primary care settings, in which over 90 percent of patients are publicly insured. Several of these clinics implemented PrEP coordination programs with PrEP navigators and/or panel management programs. Challenges may be different in settings in which patients are privately insured or uninsured and in settings without PrEP navigators. In addition, the number of providers and patients we interviewed does not allow for us to make population level generalizations. However, by doing in-depth, semi-structured interviewing, we were able to achieve insights into issues affecting PrEP persistence. Finally, we did not interview any patients who were prescribed PrEP because of injection drug use alone. This population is disproportionally impacted by HIV infection and has had poor PrEP uptake compared to other key populations. Very few in the SFPCC used PrEP for this indication, limiting our ability to include them in the study. We did, however, oversample other populations disproportionately impacted by HIV, including Black and Latinx MSM and transgender women.
This study highlights the challenges in PrEP delivery in primary care settings and barriers to PrEP persistence. Our findings suggest that low-barrier PrEP provision with extended care, drop-in visits, streamlined testing, standing orders for laboratory tests, and longer PrEP prescriptions (i.e., 90 days) are highly desirable for many PrEP users. In addition, proactive provision of adherence support and counseling, as well as referrals to mental health treatment, housing resources, and substance use treatment, may be useful to some PrEP users and support their ongoing PrEP use. Telehealth [40, 41], as well as frequent remote check-ins by smart phone and computer have also shown promise [42, 43], as has flexibility in terms of who provides care. Other acceptable approaches suggested by our data include drop-in visits, same-day PrEP starts or restarts facilitated by rapid HIV testing, STI self-collection via express visits or home-based testing options, and use of standing orders for quarterly tests in a drop-in setting with expanded hours. These patient-centered approaches would likely have wide applicability in a variety of PrEP care settings globally. There is a clear need to detect and prevent forward transmission of incident HIV infections through regular HIV testing, but overly onerous PrEP follow-up procedures may counter this intended goal by making it more difficulty for patients to persist on PrEP. Flexible, patient-centered PrEP implementation will need to reduce these barriers to improve PrEP persistence while also offering additional support proactively to those who need it. Further research on PrEP persistence in other settings in the United States and internationally are necessary to understand if the suggested implications are suitable for other health systems.
References
Grant RM, Anderson PL, McMahan V, Liu A, Amico KR, Mehrotra M, et al. Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: a cohort study. Lancet Infect Dis. 2014;14(9):820–9. https://doi.org/10.1016/s1473-3099(14)70847-3.
Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. NEngl J Med. 2010;363(27):2587–99.
McCormack S, Dunn DT, Desai M, Dolling DI, Gafos M, Gilson R, et al. Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. The Lancet. 2016;387(10013):53–60. https://doi.org/10.1016/s0140-6736(15)00056-2.
Bae JW, Guyer W, Grimm K, Altice FL. Medication persistence in the treatment of HIV infection: a review of the literature and implications for future clinical care and research. AIDS. 2011;25(3):279–90. https://doi.org/10.1097/QAD.0b013e328340feb0.
Cramer J, Roy A, Burrell A, Fairchild C, Fuldeore M, Ollendorf D, et al. Medication compliance and persistence: terminology and definitions. Value Health. 2008;11:44–7.
Spinelli MA, Scott HM, Vittinghoff E, Liu AY, Gonzalez R, Morehead-Gee A, et al., editors. Missed Visits associated with future preexposure prophylaxis (PrEP) discontinuation among PrEP users in a municipal primary care health network. Open forum infectious diseases. Oxford: Oxford University Press; 2019.
Blackstock OJ, Patel VV, Felsen U, Park C, Jain S. Pre-exposure prophylaxis prescribing and retention in care among heterosexual women at a community-based comprehensive sexual health clinic. AIDS Care. 2017;29(7):866–9. https://doi.org/10.1080/09540121.2017.1286287.
Krakower D, Maloney KM, Powell VE, Levine K, Grasso C, Melbourne K, et al. Patterns and clinical consequences of discontinuing HIV preexposure prophylaxis during primary care. J Int AIDS Soc. 2019;22(2):e25250.
Liu A. Learning from Oral PrEP care retention: rates, patterns, and interventions. NIAID-NIMH behavioral and social science meeting; May 13–14, 2019.
Rusie LK, Orengo C, Burrell D, Ramachandran A, Houlberg M, Keglovitz K, et al. Preexposure prophylaxis initiation and retention in care over 5 years, 2012–2017: are quarterly visits too much? Clin Infect Dis. 2018;67(2):283–7. https://doi.org/10.1093/cid/ciy160.
van Epps P, Maier M, Lund B, Howren MB, Beck B, Beste L, et al. Medication adherence in a nationwide cohort of veterans initiating pre-exposure prophylaxis (PrEP) to prevent HIV infection. J Acquir Immune Defic Syndr. 2018;77(3):272–8.
Zucker J, Carnevale C, Richards P, Slowikowski J, Borsa A, Gottlieb F, et al. Predictors of disengagement in care for individuals receiving pre-exposure prophylaxis (PrEP). J Int AIDS Soc. 2019. https://doi.org/10.1097/qai.0000000000002054.
Chan PA, Mena L, Patel R, Oldenburg CE, Beauchamps L, Perez-Brumer AG, et al. Retention in care outcomes for HIV pre-exposure prophylaxis implementation programmes among men who have sex with men in three US cities. J Int AIDS Soc. 2016;19(1):20903. https://doi.org/10.7448/ias.19.1.20903.
Dombrowski JC, Golden MR, Barbee LA, Khosropour CM. Patient disengagement from an HIV preexposure prophylaxis program in a sexually transmitted disease clinic. Sex Transm Dis. 2018;45(9):e62–e6464.
Scott H, Spinelli MA, Vittinghoff E, Morehead-Gee A, Nordell M, Liu A, et al. Racial/Ethnic and HIV risk category disparities in PrEP discontinuation among patients in publicly-funded primary care clinics. AIDS. 2019;33(14):2189–2195.
Greenwald Z, Beauchemin M, Benomar K, Landry G, Boissonnault M, Charest L, et al., editors. High seroconversion rates following prep discontinuance in a Montreal clinic. Boston, MA: CROI; 2018.
SFDPH. Ask about PrEP: How providers can prescribe PrEP to prevent HIV and reduce health disparities; 2017.
Spinelli MA, Scott HM, Vittinghoff E, Liu AY, Morehead-Gee A, Gonzalez R, et al., editors. Provider adherence to pre-exposure prophylaxis monitoring guidelines in a large primary care network. Open forum infectious diseases. Oxford: Oxford University Press; 2018.
CDC. Preexposure prophylaxis for the prevention of HIV infection in the United States—2017 update.
Parsons JT, Rendina HJ, Lassiter JM, Whitfield THF, Starks TJ, Grov C. Uptake of HIV pre-exposure prophylaxis (PrEP) in a national cohort of gay and bisexual men in the United States. J Acquir Immune Defic Syndr. 2017;74(3):285–92. https://doi.org/10.1097/qai.0000000000001251.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. https://doi.org/10.1191/1478088706qp063oa.
Philbin MM, Parker CM, Parker RG, Wilson PA, Garcia J, Hirsch JS. The promise of pre-exposure prophylaxis for black men who have sex with men: an ecological approach to attitudes, beliefs, and barriers. AIDS Patient Care STDs. 2016;30(6):282–90. https://doi.org/10.1089/apc.2016.0037.
Hughes SD, Sheon N, Andrew EVW, Cohen SE, Doblecki-Lewis S, Liu AY. Body/selves and beyond: Men’s narratives of sexual behavior on PrEP. Med Anthropol. 2018;37(5):387–400. https://doi.org/10.1080/01459740.2017.1416608.
Gafos M, Horne R, Nutland W, Bell G, Rae C, Wayal S, et al. The context of sexual risk behaviour among men who have sex with men seeking PrEP, and the impact of PrEP on sexual behaviour. AIDS Behav. 2019;23(7):1708–20. https://doi.org/10.1007/s10461-018-2300-5.
Kelley CF, Kahle E, Siegler A, Sanchez T, del Rio C, Sullivan PS, et al. Applying a PrEP continuum of care for men who have sex with men in Atlanta, Georgia. Clin Infect Dis. 2015;61(10):1590–7.
Serota DP, Rosenberg ES, Lockard AM, Rolle C-PM, Luisi N, Cutro S, et al. Beyond the biomedical: preexposure prophylaxis failures in a cohort of young black men who have sex with men in Atlanta, Georgia. Clin Infect Dis. 2018;67(6):965–70. https://doi.org/10.1093/cid/ciy297
Laborde ND, Spinelli MA, Scott H, editors. Uncomfortable conversations: sexual health disparities in identifying PrEP candidates. San Jose, CA: American Anthropological Association; 2018.
Lankowski AJ, Bien-Gund CH, Patel VV, Felsen UR, Silvera R, Blackstock OJJA, et al. PrEP in the real world: predictors of 6-month retention in a diverse urban cohort. AIDS Behav. 2019;23(7):1797–802. https://doi.org/10.1007/s10461-018-2296-x.
Lancki N, Almirol E, Alon L, McNulty M, Schneider JA. Preexposure prophylaxis guidelines have low sensitivity for identifying seroconverters in a sample of young black MSM in Chicago. AIDS. 2018;32(3):383–92.
Golub S, editor. PrEP messaging: taking “Risk” out of the pitch. HIVR4P; Madrid; 2018.
Calabrese SK, Underhill K. How stigma surrounding the use of HIV preexposure prophylaxis undermines prevention and pleasure: a call to destigmatize “truvada whores”. Am J Public Health. 2015;105(10):1960–4.
Calabrese SK, Earnshaw VA, Underhill K, Hansen NB, Dovidio JF. The impact of patient race on clinical decisions related to prescribing HIV pre-exposure prophylaxis (PrEP): assumptions about sexual risk compensation and implications for access. AIDS Behav. 2014;18(2):226–40. https://doi.org/10.1007/s10461-013-0675-x
Millett GA, Flores SA, Peterson JL, Bakeman R. Explaining disparities in HIV infection among black and white men who have sex with men: a meta-analysis of HIV risk behaviors. AIDS. 2007;21(15):2083–91.
Mimiaga MJ, Reisner SL, Cranston K, Isenberg D, Bright D, Daffin G, et al. Sexual mixing patterns and partner characteristics of black MSM in Massachusetts at increased risk for HIV infection and transmission. J Urban Health. 2009;86(4):602–23.
Maulsby C, Millett G, Lindsey K, Kelley R, Johnson K, Montoya D, et al. HIV among black men who have sex with men (MSM) in the United States: a review of the literature. AIDS Behav. 2014;18(1):10–25.
Sullivan PS, Peterson J, Rosenberg ES, Kelley CF, Cooper H, Vaughan A, et al. Understanding racial HIV/STI disparities in black and white men who have sex with men: a multilevel approach. PLoS ONE. 2014;9(3):e90514.
Irvin R, Vallabhaneni S, Scott H, Williams JK, Wilton L, Li X, et al. Examining levels of risk behaviors among black men who have sex with Men (MSM) and the association with HIV acquisition. PLoS ONE. 2015;10(2):e0118281.
Sullivan PS, Rosenberg ES, Sanchez TH, Kelley CF, Luisi N, Cooper HL, et al. Explaining racial disparities in HIV incidence in black and white men who have sex with men in Atlanta, GA: a prospective observational cohort study. Ann Epidemiol. 2015;25(6):445–54.
Calabrese SK, Krakower DS, Mayer KH. Integrating HIV preexposure prophylaxis (PrEP) into routine preventive health care to avoid exacerbating disparities. Am J Public Health. 2017;107(12):1883–9. https://doi.org/10.2105/ajph.2017.304061.
Stekler JD, McMahan V, Ballinger L, Viquez L, Swanson F, Stockton J, et al. HIV pre-exposure prophylaxis prescribing through telehealth. JAIDS J Acquir Immune Defic Syndr. 2018;77(5):e40–e4242.
Touger R, Wood BR. A review of telehealth innovations for HIV pre-exposure prophylaxis (PrEP). Curr HIV/AIDS Rep. 2019;16(1):113–9.
Liu AY, Vittinghoff E, von Felten P, Rivet Amico K, Anderson PL, Lester R, et al. Randomized controlled trial of a mobile health intervention to promote retention and adherence to preexposure prophylaxis among young people at risk for human immunodeficiency virus: The EPIC Study. Clin Infect Dis. 2019;68(12):2010–7.
Getz L. Texting for Help. Social Work Today. 2014;14(4).
Funding
This study was supported by Foundation for the National Institutes of Health (R01AI104309).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Laborde, N.D., Kinley, P.M., Spinelli, M. et al. Understanding PrEP Persistence: Provider and Patient Perspectives. AIDS Behav 24, 2509–2519 (2020). https://doi.org/10.1007/s10461-020-02807-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-020-02807-3