Abstract
Men who have sex with men (MSM) commonly report engaging in rectal douching (RD) practices prior to receptive anal intercourse. Researchers are interested in the possibility of designing a RD with a microbicide component. In our analyses, we examined whether YMSM who engaged in RD behaviors differ in HIV prevention behaviors from their non-RD peers. We then examined whether RD frequency was associated with rectal microbicide acceptability. Half the participants (47.8%) reported having ever douched. Participants were more likely to douche if they were racial/ethnic minorities (AOR = 2.24, p = 0.02) and had recently tested for HIV (AOR = 1.96, p = 0.04). Greater douching frequency was associated with racial/ethnic minorities (β = 0.20, p = 0.009) and recent HIV testing (β = 0.19, p < 0.01). Participants who reported frequently douching indicated greater microbicide acceptability (β = 0.32, p < 0.001). Designing behaviorally congruent products remains a priority in next generation Pre-Exposure Prophylaxis (PrEP) and a rectal douche might be an additional tool if found to be efficacious.
Resumen
Los hombres que tienen sexo con otros hombres (MSM) comúnmente utilizan duchas rectales (RD) antes de tener sexo anal receptivo. Ante la posibilidad de diseñar una ducha rectal con un componente microbicida, examinamos si los jóvenes MSM (YMSM) que usan RD difieren en las conductas de prevención del VIH cuando son comparados con pares que no usan RD. Además examinamos si la frecuencia de RD estaba asociada con la aceptabilidad de microbicidas rectales. La mitad de los participantes (47.8%) informaron haber usado RD. Los participantes con mayor propensidad a usar RD fueron las minorías raciales/étnicas (AOR = 2.24, p = .02) y aquellos YMSM que habían realizado una prueba de VIH recientemente (AOR = 1.96, p = .04). Mayor frecuencia en el uso de RD se asoció con ser una minoría racial/étnica (β = .20, p = .009) y entre aquellos quienes tuvieron una prueba reciente de VIH (β = .19, p <.01). Los participantes que informaron el uso de RD con mayor frecuencia indicaron una mayor aceptabilidad de los microbicidas (β = .32, p <.001). El diseño de productos conductualmente congruentes sigue siendo una prioridad en el desarrollo de la nueva generación de productos con profilaxis antes de la exposición (PrEP) y una ducha rectal podría ser una herramienta adicional si se considera eficaz en un futuro.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gay, bisexual, and other men who have sex with men (GBMSM) account for the greatest number of new HIV infections in the United States [1], accounting for 67% of all new diagnoses in 2016 [1]. Young GBMSM (YGBMSM; ages 13–29) experience the greatest vulnerability to HIV, with African American and Latino YGBMSM accounting for the largest proportion of new HIV cases [1]. Recent biomedical advances in HIV prevention (e.g., oral pre-exposure prophylaxis (PrEP)) may help curb these new infections, yet uptake and adherence to oral PrEP has been challenging among YMSM, particularly among racial/ethnic minority YMSM [2,3,4]. Mayer and colleagues [5], for example, found that only 6% of 18–24 year olds had ever used PrEP compared to 18% of MSM above the age of 30. Similarly, several recent reports have highlighted high rates of PrEP discontinuation. Morgan and colleagues [3], for instance, found 33% of YMSM discontinued PrEP use, with racial/ethnic minority YMSM being more likely to discontinue use. Undoubtedly, continued efforts to help YMSM reduce their vulnerability to HIV through effective PrEP adoption and retention are needed.
Alongside implementation strategies to strengthen daily oral PrEP, researchers have acknowledged that some population segments may benefit from other PrEP deliveries, both systemic (e.g., injectables, implants) and topical (e.g., gels, inserts). Among this array of next generation options, researchers are exploring the efficacy of a PrEP-product delivered as a rectal douche (RD) given the popularity of rectal douching among individuals who engage in receptive anal intercourse (RAI). In a recent Phase I, open label, dose-escalation trial, Hendrix and colleagues [6] found that macaques who were administered tenofovir-diphosphate douche had 1 to 3 logs higher concentration in the colon than counterparts who had received daily oral PrEP dosing with 7, 4, or 2 doses per week. Given the promising results from these animal studies, Hendrix and colleagues are currently examining their RD product’s safety, tolerability and pharmacokinetic properties with human participants.
As an event-driven product, a rectal microbicide douche could serve as an alternative to daily oral PrEP by promoting behavioral congruence between a biomedical prevention product and users’ current sexual behaviors and motivations to engage in RD practices (e.g., to feel clean). In a recent review of rectal douching among MSM engaging in RAI, 87–97% have douched before sex within the past 12 months and 13–48% douched after sex [7]. In a subsequent survey of Grindr users, Carballo-Diéguez et al. [8] found that 98% of participants who douche would be likely to use a microbicide douche. Interestingly, they also found that 94% of participants who do not douche currently would be willing to use a microbicide douche. Most participants who acted as the insertive partner (96%) also expressed support for a partner who would use a rectal microbicide douche [8]. At present, however, limited data exist on the rectal douching practices of YMSM. Prior MSM samples reporting their RD practices had mean ages in the mid-thirties (e.g., 33.9 years [9]; 36.6 years [8]). Given the potential for YMSM to benefit greatly from a rectal microbicide douche in the future, as well as recognizing the developmental differences that may be present for this group relative to their older peers, it is vital that we ascertain YMSM’s RD practices alongside their rectal microbicide acceptability separately.
The goal of this study was to examine the prevalence of RD practices in a racially/ethnically diverse sample of YGBMSM, and subsequently to explore their acceptability of a rectal microbicide product. We had three objectives to support the study’s goals. First, we examined whether the prevalence of RD practices differed based on YMSM’s sociodemographic characteristics and HIV risk behaviors. Consistent with the prior literature review [9], we hypothesized that RD behaviors would be more common among were racial/ethnic minorities, YMSM who had been diagnosed with a sexually-transmitted infection (STI) in the past, and those who reported engaging in RAI recently. Second, we examined whether RD frequency differed by YMSM’s sociodemographic and HIV risk behaviors. Similar to our first objective, we hypothesized that YMSM would report greater RD frequency if they were racial/ethnic minorities, had been diagnosed with a sexually-transmitted infection (STI) in the past, and reported recently using alcohol prior to or during sex. Finally, we tested whether YMSM who engage in RD would be more accepting of rectal microbicides than YMSM who did not engage in RD. Consistent with the premise of developing behaviorally congruent PrEP products, we hypothesized that YMSM who douched more frequently would be more accepting a of a future rectal microbicide product.
Methods
Sample
Data for this study come from the baseline survey of an online pilot randomized trial (N = 180) seeking to reduce HIV risks among YGBMSM in the United States [10]. The study included a population of young men who have sex with men (YMSM) who were between the ages of 18–24 (inclusive) years old. To be eligible for participation, recruits also had to identify as a cisgender male, report being single, self-report as HIV-negative or as not knowing their HIV status, and using online sites to meet partners with whom to have condomless anal intercourse in the prior 6 months. Participants were primarily recruited through advertisements on two popular social and sexual networking sites. Social network advertisements were viewable only to men who fit our age range and who lived in the United States.
Procedures
Upon entering the study site, participants were asked to complete a study screener. If eligible, participants created a study account and received a detailed consent form that explained the purpose of the study and their rights as participants. Consented participants then answered a baseline 30-min questionnaire including questions regarding their sociodemographic characteristics, HIV prevention behaviors, sexual behaviors, and acceptability to rectal microbicide products. We used best practices [11, 12] to identify duplicates and falsified entries by manually examining participants’ online presence, email and IP addresses, operating system and browser information, irregular answer patterns, and time taken to complete survey. Participants were compensated with $30 Amazon gift card via email upon completion of the baseline questionnaire. Study data were protected with a 256-bit SSL encryption and kept within a university firewalled server. Our Institutional Review Board approved the study procedures.
Measures
Douching Behaviors
Participants indicated whether they had ever used a rectal douche before engaging in RAI (0 = No; 1 = Yes). Participants who had douched were asked to report the age (in years) when they began douching, how frequently they douche before RAI (0 = Never, 1 = Infrequently, 2 = Frequently, 3 = Always), and how long they waited after RD to have RAI (0 = less than 30 min, 1 = 30 min to 1 h, 2 = between 1 and 2 h, 3 = between 2 and 3 h, 4 = between 3 and 4 h, and 5 = 4 h or more). Participants were also asked to note the reasons for douching before RAI: To be clean, Sex partner suggested it, Friends talked about it, and/or Other Reasons.
Microbicide Acceptability
Participants responded to three questions relating to: [1] the overall use of a microbicide; [2] when you do not use condoms; and [3] if you had to wait 30 min before sexual intercourse. Each rectal microbicide item was measured using a 10-point scale (1 = Extremely Unlikely; 10 = Extremely Likely). We created a mean overall acceptability score, where higher scores indicated greater acceptability of microbicide products (α = 0.70).
Recent Sexual Behaviors
YMSM were asked to report their sexual behavior with men in the prior 30 days using the Sexual Practices Assessment Schedule [13]. Participants were asked to report the number of sexual partners with whom they had engaged in RAI. We assigned a value of zero to participants who reported not having engaged in RAI. We created a dichotomous variable to indicate whether YMSM engaged in RAI in the prior 30 days (0 = No; 1 = Yes). Participants were also asked to indicate when they had used alcohol before or during sex in the past 30 days (0 = No; 1 = Yes).
HIV and STI Testing
Participants were asked about if they have ever been tested for HIV and asked to indicate the date of their last HIV test. We then created a dichotomous measure to reflect whether YGBMSM complied with CDC’s (2018) recommended HIV testing schedule (i.e., every 3 months) for high-risk MSM (0 = Not tested in prior 3 months; 1 = Tested in prior 3 months). We also ascertained whether participants had ever been diagnosed with a STI by a provider (0 = No; 1 = Yes).
Socio-Demographic Characteristics
Participants were asked to report their date of birth (in years), race (Black/African American, White, American Indian/Alaskan Native, Middle Eastern, Asian, Native Hawaiian or Other Pacific Islander, Other), Hispanic/Latino ethnicity, and highest level of educational attainment (response options: 8th grade or less, some high school, graduated high school/GED, technical school, associate degree, some college, college, some graduate school, graduate school). For analytical purposes in multivariable analyses, both education (0 = Non-high school degree; 1 = High school degree or greater) and race/ethnicity (0 = Non-Hispanic Whites; 1 = Racial/Ethnic Minorities) were dichotomized.
Data Analytic Strategy
We calculated descriptive statistics for the variables included in our analysis, using bivariate statistics to examine whether there were differences between participants who engaged in douching and their non-douching counterparts (see Table 1). Using a multivariable logistic regression, we then explored the association between rectal douching likelihood and participants’ sociodemographic characteristics, HIV/STI testing behaviors, and having used alcohol prior to or during sex. We then used a multivariable linear regression to explore the association between douching frequency and the aforementioned covariates. Finally, we tested the association between overall microbicide acceptability and douching frequency, after adjusting for the covariates of interest. Analyses were conducted using SPSS v22 (Chicago, IL). For brevity, only statistically-significant findings (p < 0.05) are described below.
Results
Sample characteristics
The mean age of participants is 21.67 (SD = 1.81). The majority of participants identified as gay (n = 159; 88.3%) followed by bisexual (n = 14; 7.8%) and queer (n = 7; 3.9%). The majority of participants self-identified as White (n = 120; 66.7%) followed by Multiracial (n = 30; 16.7%), Black (n = 18; 10%), Asian (n = 10; 5.6%), and Middle Eastern or Native American (n = 2; 1.1%). Thirty-percent (n = 54) of the sample reported Hispanic/Latino ethnicity.
In the prior 30 days, 61.1% (n = 110) of YMSM reported having RAI and 38.9% (n = 70) reported using alcohol before or during sex. Forty-six percent (n = 82) had tested for HIV in the prior 3 months. Thirteen percent (n = 25) of participants reported currently using PrEP. Nearly twenty percent of participants (n = 32; 17.8%) reported a prior STI diagnosis.
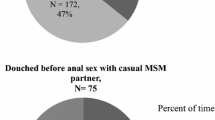
Douching Likelihood
Nearly half of the participants (47.8%) reported ever douching, with the mean age of onset being 19 years (SD = 2.05). YMSM who engaged in receptive anal intercourse (54.5%) were more likely to douche than those who had not engaged in RAI (37.1%; \(\chi^{ 2}_{\left( 1\right)}\) = 5.19; p = 0.02). Individuals who had recently tested for HIV (57.3%) were more likely to douche than counterparts who had not tested in the prior 3 months (39.8%; \(\chi^{ 2}_{\left( 1\right)}\) = 5.49; p = 0.02).
When entered into a logistic regression framework (\(\chi^{ 2}_{\left( 6\right)}\) = 19.47; p < 0.01), YMSM who had ever douched were more likely to be a racial/ethnic minority (AOR = 2.24, p = 0.015). YMSM who douched were more likely to have tested in prior 3 months (AOR = 1.96, p = 0.04). There were no associations observed between ever douching and having a high school education, prior STI diagnosis, recent RAS, or using alcohol with sex (see Table 2).
Douching Frequency
Forty percent of YMSM reported frequent douching, with the majority (96.5%) douching to be clean. Most participants who douche reported pre-coital douching an hour or less before sex (61.5%), between 1 and three hours (34.9%), and three or more hours (3.6%).
In a multivariable regression (F(5,172) = 2.93, p < 0.02, R2 = 7.80%), douching frequency was greater among racial/ethnic minorities than Non-Hispanic White counterparts (β = 0.20, p = 0.009) and YMSM who had recently tested for HIV (β = 0.19, p = 0.01). Douching frequency was not associated with having a high school education, a prior STI diagnosis, or using alcohol before or during sex (see Table 3).
Microbicide Acceptability
YMSM who engaged in RD practices reported greater overall rectal microbicide acceptability (M = 9.09, SD = 1.89) than counterparts not engaging in RD (M = 8.64, SD = 1.65; t = − 2.07, p = 0.04). YMSM who had douched were also more accepting of a rectal microbicide if a condom was not needed during sex (M = 9.62, SD = 0.90) compared to YMSM who did not douche (M = 8.94, SD = 1.62; t = − 3.51, p = 0.001). YMSM who douche were also more willing to use a rectal microbicide if they had to wait 30 min before sex (M = 7.36, SD = 2.58) than counterparts who do not douche (M = 5.90, SD = 2.86; t = − 3.57, p < 0.001).
In a multivariable regression model (F(6, 171) = 4.76, p < 0.001), the composite microbicide acceptability score was positively associated with greater douching frequency (β = 0.32, p < 0.001). We found no other association between YMSM’s overall microbicide acceptability score and having a high school education, being a racial/ethnic minority, HIV testing, having a prior STI diagnosis, or using alcohol before or during sex (see Table 4).
Discussion
Given the popularity of douching prior to receptive anal intercourse identified in the literature, we examined the prevalence of RD practices in a racially/ethnically diverse sample of YGBMSM, and subsequently explored whether rectal microbicide acceptability differed based on YGBMSM’s RD behaviors. Currently, limited research has documented the prevalence of douching behaviors among YGBMSM. Our findings highlight the popularity of RD among YGBMSM prior to RAI, with over half of participants reporting having engaged in RD in the past. We also found that over one-third of individuals frequently douche prior to RAI and YGBMSM in our sample reporting an earlier age of RD onset than previously reported in the literature [8]. Taken together, efforts to support research and behavioral surveillance examining the RD behaviors among YGBMSM are warranted.
YGBMSM’s reasons for douching prior to RAI echoed prior findings, including RD’s perceived hygienic benefits, partner and peer encouragement, and feeling more satisfied when engaging in RAI [14,15,16]. Our findings suggest that YGBMSM who douche are more accepting of rectal microbicides, including in contexts where no condom is going to be used for RAI, and where its application would require at least 30 min before engaging in sex. Given the popularity of RD among MSM populations and its potential to be a modality through which PrEP might be delivered, our findings reinforce on-going efforts to create a behaviorally-congruent rectal microbicide douche as an additional prevention alternative. Moreover, our findings suggest that future rectal microbicide trials should focus on the experiences of YGBMSM given their heightened vulnerability to acquire HIV, onset of douching during late adolescence, and interest in other forms of PrEP-delivery.
YGBMSM who had recently tested for HIV were also more likely to douche and to do so frequently. Given prior associations between RD practices and HIV/STI acquisition [8, 9], these findings point to the necessity and potential opportunity to offer risk reduction counseling and harm reduction strategies related to douching practices during HIV testing and counseling sessions. Efforts to educate HIV test counselors on douching devices and practices known to reduce unintended injuries and/or damage to the rectal epithelium might be needed. For example, Leyva and colleagues [17] examined whether inflammation in the rectum differed based on the RD formulations used: i.e., hyperosmolar (e.g., commercial fleet phosphate enema), hypoosmolar (distilled water), and isoosmolar (normosol-r with pHv7.4) douches. Their findings suggest that the isoosmolar and hyperosmolar enema had minimal or no effect on the colonic epithelium compared to the hyperosmolar enema which caused sloughing of the epithelial layer [17]. Data such as these may help inform current HIV/STI prevention efforts, as well as help design a safe, effective, and behavioral congruent RD to be used prior to RAI. Additional research assessing what devices (e.g., hose, bulb, enema bottle, home-made equipment) and fluids (e.g., water, saline, scented commercial products) are used by YGBMSM is warranted to advance both comprehensive sex education and the design and delivery of a future rectal microbicide douche.
Racial/ethnic minority YGBMSM were more likely to report RD behaviors than their Non-Hispanic White counterparts. Given low uptake of daily oral PrEP among YGBMSM of color [18,19,20], a rectal microbicide douche might help circumvent systemic-barriers to a daily oral PrEP regimen for this group by offering an event-driven PrEP delivery modality that is behaviorally-congruent with their current behaviors. As PrEP douches are developed, however, careful attention will need to be placed in how to ensure easy access to these enemas among YBMSM of color and other vulnerable populations. Efforts to ensure the inclusion and representation of YGBMSM during the rectal microbicide douche developmental pipeline remains crucial to ensure their perspectives and experiences can be used to foreshadow and address anticipated uptake and adherence problems in the future. Interestingly, racial/ethnic minorities also reported greater rectal douching frequency than Non-Hispanic White peers. This finding diverges from the review of the douching literature completed by Carballo-Diéguez and colleagues [7], where they found no evidence of differences in rectal douching across racial/ethnic subgroups. While we do not know why racial/ethnic YMSM are douching more frequently in our study, prior research findings concerning the popularity of vaginal douches have noted greater frequency among ethnic minority women [21, 22]. While our analyses indicate that most participants douche to feel clean, future research examining how YMSM and their partners conceptualize “cleanliness” might be warranted. In prior studies examining vaginal douching, for example, both women and their male partners discussed “cleanliness” as a subjective experiences related to acquiring a desired scent or fragrance [23], tightening the vagina to promote male pleasure [24], and believing that douching would lead to a healthier microbiome and/or remove any potential infections [25, 26]. Although individuals may use different substances to achieve these effects, Carballo-Diéguez et al.’s review [7] noted that most adult MSM reporting using water as the primary non-commercial substance with which to douche. However, their review did note that a smaller proportion reported using water with soap, salts, and/or fragrances. Future research should explore what YMSM are using as douching agents, their reasons for selecting these products, and their association with douching frequency.
Several limitations are worth noting from our study that could be addressed with further research. First, our sample is an online-recruited, national convenience sample of high-risk YGBMSM participating in a mHealth prevention intervention. Thus, it may be preemptive to extrapolate the current findings to the larger population of YGBMSM. Second, while the sample includes YGBMSM from across the United States, we relied on a convenience sample given the absence of a population frame from which to randomly sample a representative pool of YGBMSM across the United States. Additionally, as this sample of YMSM are from the United States, further research is needed to understand the douching practices of MSM across the globe. Third, our study assessed hypothetical acceptability of a rectal microbicide product. Although hypothetical acceptability may not be indicative of YGBMSM’s willingness and intention to use a RD microbicide in the future, the robust association between douching frequency and rectal microbicide acceptability is encouraging. As rectal microbicide douche formulations become closer to Phase 2 and 3 trials, it will be imperative that researchers examine how treatment regimen (e.g., dosage, number of douches required per event), user characteristics and contexts (e.g., timing, partner type), and potential management of side effects (e.g., leakage, toxicity) affect its acceptability. Building on lessons learned from daily oral PrEP as well as our study findings, we encourage future research to move beyond hypothetical acceptability and apply sociobehavioral perspectives to explore these considerations through choice experiments (e.g., conjoint analysis) and/or run-in placebo trials.
Designing behaviorally congruent formulations of a rectal microbicide that serves as an alternative to daily oral PrEP regimen remains a priority in the community [27]. Consistent with the need for behaviorally congruent HIV prevention products, our findings suggest that YGBMSM are interested in RM products, with those who engage in RD being more accepting of formulations currently under consideration (e.g., rectal PrEP douche). The development of a rectal douche could revolutionize the way HIV acquisition is prevented by expanding the suite of options available. Future work on rectal microbicide formulations using a douche as a mode of transportation and focus on YMSM is warranted.
References
Centers for Disease Control and Prevention. HIV and Gay and Bisexual Men HIV by Group 2018. https://www.cdc.gov/hiv/group/msm/index.html. Accessed 26 Sept 2018.
Hammack PL, Meyer IH, Krueger EA, Lightfoot M, Frost DM. HIV testing and pre-exposure prophylaxis (PrEP) use, familiarity, and attitudes among gay and bisexual men in the United States: a national probability sample of three birth cohorts. PLoS ONE. 2018;13(9):e0202806.
Morgan E, Ryan DT, Newcomb ME, Mustanski B. High rate of discontinuation may diminish prep coverage among young men who have sex with men. AIDS Behav. 2018;22(11):3645–8.
Serota DP, Rosenberg ES, Lockard AM, Rolle C-PM, Luisi N, Cutro S, et al. Beyond the biomedical: preexposure prophylaxis failures in a cohort of young black men who have sex with men in Atlanta, Georgia. Clin Infect Dis. 2018;67(6):965–70.
Mayer K, Biello KB, Novak DS, Krakower D, Mimiaga MJ. PrEP uptake disparities in a diverse online sample of U.S. men who have sex with men. Conference on Retroviruses and Opportunistic Infections; Seattle, WA, 2017.
Hendrix C. On-demand topical agents for hiv pre-exposure prophylaxis. the future is now: next steps in developing new prevention options HIVR4P Webcasts 2018.
Carballo-Diéguez A, Lentz C, Giguere R, Fuchs EJ, Hendrix CW. Rectal douching associated with receptive anal intercourse: a literature review. AIDS Behav. 2018;22(4):1288–94.
Carballo-Diéguez A, Giguere R, Lentz C, Dolezal C, Fuchs EJ, Hendrix CW. Rectal Douching practices associated with anal intercourse: implications for the development of a behaviorally congruent HIV-prevention rectal microbicide douche. AIDS Behav. 2018;23:1484–93.
Noor SW, Rosser BRS. Enema use among men who have sex with men: a behavioral epidemiologic study with implications for HIV/STI prevention. Arch Sex Behav. 2014;43(4):755–69.
Bauermeister JA, Tingler RC, Demers M, Connochie D, Gillard G, Shaver J, Chavanduka T, Harper GW. Acceptability and preliminary efficacy of an online HIV prevention intervention for single young men who have sex with men seeking partners online: The myDEx Project. AIDS Beh. 2019. (in press).
Bauermeister JA, Zimmerman MA, Johns MM, Glowacki P, Stoddard S, Volz E. Innovative recruitment using online networks: lessons learned from an online study of alcohol and other drug use utilizing a Web-based, respondent-driven sampling (webRDS) strategy. J Stud Alcohol Drugs. 2012;73(5):834–8.
Teitcher JEF, Bockting WO, Bauermeister JA, Hoefer CJ, Miner MH, Klitzman RL. Detecting, preventing, and responding to “Fraudsters” in internet research: ethics and tradeoffs. J Law Med Ethics. 2015;43(1):116–33.
Bauermeister JA. Sexual partner typologies among single young men who have sex with men. AIDS Behav. 2015;19(6):1116–28.
Carballo-Diéguez A, Bauermeister J, Ventuneac A, Dolezal C, Mayer K. Why rectal douches may be acceptable rectal-microbicide delivery vehicles for men who have sex with men. Sex Transm Dis. 2010;37(4):228–33.
Carballo-Diéguez A, Bauermeister JA, Ventuneac A, Dolezal C, Balan I, Remien RH. The use of rectal douches among HIV-uninfected and infected men who have unprotected receptive anal intercourse: implications for rectal microbicides. AIDS Behav. 2008;12(6):860–6.
Lamblet LCR, da Silva RJC. Prevalence and types of rectal douches used for anal intercourse among men who have sex with men in Brazil. BMJ Open. 2017;7(5):e011122.
Leyva FJ, Bakshi RP, Fuchs EJ, Li L, Caffo BS, Goldsmith AJ, et al. Isoosmolar enemas demonstrate preferential gastrointestinal distribution, safety, and acceptability compared with hyperosmolar and hypoosmolar enemas as a potential delivery vehicle for rectal microbicides. AIDS Res Hum Retroviruses. 2013;29(11):1487–95.
Kirby T, Thornber-Dunwell M. Uptake of PrEP for HIV slow among MSM. Lancet. 2014;383(9915):399–400.
Parisi D, Warren B, Leung SJ, Akkaya-Hocagil T, Qin Q, Hahn I, et al. A multicomponent approach to evaluating a pre-exposure prophylaxis (PrEP) implementation program in five agencies in New York. J Assoc Nurses AIDS Care. 2018;29(1):10–9.
Remy L, Enriquez M. Behavioral interventions to enhance PrEP uptake among black men who have sex with men: a review. J Assoc Nurses AIDS Care. 2019;30(2):151–63.
Rosenberg MJ, Holmes MD. Vaginal douching: Who and why? J Reprod Med. 1991;36(10):753–8.
Crann SE, Cunningham S, Albert A, Money DM, O’Doherty KC. Vaginal health and hygiene practices and product use in Canada: a national cross-sectional survey. BMC Womens Health. 2018;18(10):52.
McKee MD, Baquero M, Anderson MR, et al. Vaginal douching among latinas: practices and meaning. Matern Child Health J. 2009;13(1):98–106.
Martin Hilber AHT, Preston-Whyte E, Bagnol B, Smit J, Wacharasin C, et al. A cross cultural study of vaginal practices and sexuality: implications for sexual health. Soc Sci Med. 2010;70(3):392–400.
McKee D, Baquero M, Anderson M, Karasz A. Vaginal hygiene and douching: perspectives of Hispanic men. Cult Health Sex. 2009;11(2):159–71.
Menard JKE, Diem J, Lifleur M, Blanco J, Barton B. The sociocultural context of gynecological health among Haitian immigrant women in Florida: applying ethnographic methods to public health inquiry. Ethn Health. 2010;15(3):253–67.
Leblanc NM, Mitchell J. Providers’ perceptions of couples’ HIV testing and counseling (CHTC): perspectives From a US HIV epicenter. Couple Fam Psychol. 2018;7(1):22–33.
Acknowledgements
We greatly appreciate the hard work of the study staff, and are indebted to the study participants for volunteering their time. This research was sponsored by the US National Institutes of Health (NIH), under R34 MH101997. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH.
Funding
This study is supported by a R34 grand from the National Institute of Mental Health (R34MH101997-01A1). Views expressed in this manuscript do not necessarily represent the views of the funding agency.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tingler, R.C., Connochie, D. & Bauermeister, J.A. Rectal Douching and Microbicide Acceptability among Young Men who Have Sex with Men. AIDS Behav 24, 1414–1421 (2020). https://doi.org/10.1007/s10461-019-02662-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-019-02662-x