Abstract
Racial and ethnic disparities exist in HIV pre-exposure prophylaxis (PrEP) awareness and care. We evaluated how racial and ethnic disparities in PrEP awareness among MSM presenting to a sexually transmitted disease clinic changed from 2013 to 2016. Among 1243 MSM (68% non-Hispanic White, 22% Hispanic, and 10% non-Hispanic Black), PrEP awareness increased overall, but awareness was lower among Hispanic and non-Hispanic Black MSM relative to non-Hispanic White MSM. Awareness converged among non-Hispanic Black and White MSM by 2016, but remained consistently lower among Hispanic MSM. Improved efforts are needed to address disparities in PrEP awareness.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Men who have sex with men (MSM) in the United States (US) have an estimated 1 in 6 lifetime risk of HIV [1]. Pre-exposure prophylaxis (PrEP), a daily pill composed of tenofovir disoproxil fumarate (TDF) and emtricitabine (FTC), is effective for preventing HIV and has the potential to reduce high HIV incidence among MSM in the US [2]. Despite high interest among MSM once they become aware of PrEP [3], PrEP awareness and uptake remain suboptimal. Among MSM surveyed in 20 cities across the US in 2014, less than 5% of MSM had taken PrEP [3]. Although PrEP use has increased in subsequent years, estimates indicate less than 10% of those with indications for PrEP are benefiting from it [4].
There is also emerging evidence of racial and ethnic disparities across the PrEP care continuum [3, 5,6,7]. As one of the first steps in the PrEP care continuum [8, 9], PrEP awareness affects outcomes related to PrEP uptake and adherence at later stages of the continuum. Previous studies suggest that Black MSM have significantly lower odds of PrEP awareness relative to White MSM [10]. The 2014 National HIV Behavioral Surveillance survey of MSM across 20 US cities found that non-Hispanic Black MSM were half as likely to use PrEP as White MSM [3]. Among 972 individuals initiating PrEP in the Kaiser Permanente Northern California network, Black patients had three times the odds of low PrEP adherence relative to White patients [7]. Evidence of racial and ethnic disparities in PrEP awareness is concerning given that they may exacerbate existing disparities in the burden of HIV [1].
In this study, we aimed to evaluate racial and ethnic disparities in PrEP awareness and changes over time among MSM presenting to a New England STD clinic. Using data on PrEP awareness that were collected continuously between January 1, 2013 and December 31, 2016, we evaluated racial and ethnic differences in PrEP awareness over time. Our findings can help inform intervention and policy efforts to improve PrEP implementation, particularly among racial and ethnic groups most at risk of HIV.
Methods
Sample
We reviewed data on PrEP awareness collected through self-report by patients presenting for screening services at an STD clinic between January 1, 2013 and December 31, 2016. The clinic studied is the primary STD clinic in the state, and patients who present to the clinic are typically at risk for STDs including HIV. At STD clinic visits, patients completed an intake form by providing information on demographic and behavioral characteristics, as well as information on PrEP awareness. We restricted the sample to MSM who were HIV-negative, aged 18 years or older, and visiting the clinic for the first time.
Ethics Approval and Consent
The study was approved by the presiding institutional review board, which granted a waiver of consent for the use of de-identified secondary data from patient intake forms (Project Number 216513).
Exposure and Outcome
The main independent variable was non-Hispanic Black race and ethnicity and Hispanic ethnicity, relative to non-Hispanic White race and ethnicity. The race and ethnicity measures were based on patients’ answers to two separate questions on race and ethnicity. We did not analyze PrEP awareness among MSM of other races/ethnicities due to the low number of patients. The main outcome of interest was PrEP awareness as measured by a “yes” or “no” answer to the question, “Have you heard of taking HIV medications to prevent infection in people who are HIV negative? (Pre-exposure prophylaxis, PrEP).”
Analysis
We first described patient demographic characteristics and the year of STD clinic visits. We evaluated differences in PrEP awareness by race and ethnicity through logistic regression analyses controlling for year and age group and using robust standard errors to account for an increasing sample size over time. We included indicator variables for non-Hispanic Black race and ethnicity and Hispanic ethnicity relative to non-Hispanic White.
Results
Of 1243 MSM patients, 853 (68%) identified as non-Hispanic White, 120 (10%) identified as non-Hispanic Black, and 270 (22%) identified as Hispanic (Supplement Table I). The mean age of patients was 33 years, and 66% of patients were under 35 years of age. The number of patients visiting the STD clinic who met inclusion criteria increased over time, from 231 in 2013 to 363 in 2016. The mean number of male sexual partners in the past 12 months was 7.7 among White MSM, 7.5 among Black MSM, and 6.5 among Hispanic MSM. The mean number of male sexual partners with whom no condom was used was 2.4 among White MSM, 1.7 among Black MSM, and 1.8 among Hispanic MSM.
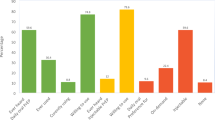
PrEP awareness increased among patients of each race and ethnicity over time (Supplement Fig. I). Non-Hispanic White patients had greater levels of PrEP awareness relative to Hispanic and non-Hispanic Black patients in 2013–2015, while PrEP awareness among non-Hispanic Black and non-Hispanic White patients converged in 2016. Hispanic patients had consistently lower PrEP awareness over time.
We present estimates of changes in PrEP awareness over time in Table 1. PrEP awareness among all MSM increased from 45% in 2013 to 66% in 2015 (adjusted odds ratio [AOR] 2.56, 95% confidence interval [CI] 1.79–3.65) and to 75% in 2016 (AOR 3.90, 95% CI 2.73–5.59). There were also statistically significant differences in PrEP awareness among MSM of difference races, ethnicities, and age groups on average during the 2013–2016 period.
Relative to an average of 63% of non-Hispanic White MSM being aware of PrEP during the 2012–2016 period, PrEP awareness was significantly lower among Hispanic patients (53%; AOR 0.55, 95% CI 0.41–0.74) and non-Hispanic Black patients (52%; AOR 0.66, 95% CI 0.44–0.98). PrEP awareness was lower among patients who were between the ages of 18 and 24 years (53%, AOR 0.59, 95% CI 0.44–0.80) and older than 55 years (50%, AOR 0.46, 95% CI 0.30–0.73) relative to those between the ages of 25 and 34 years (65%).
Discussion
This is among the first studies to demonstrate significant ethnic and racial disparities in PrEP awareness among MSM. Among patients presenting to the Rhode Island STD Clinic, PrEP awareness among non-Hispanic Black MSM was initially lower but converged with PrEP awareness among non-Hispanic White MSM by 2016, while PrEP awareness among Hispanic MSM remained consistently lower than PrEP awareness among non-Hispanic White MSM. Racial and ethnic disparities in PrEP awareness, an early step in the PrEP care continuum [8], contribute to racial and ethnic disparities in further continuum steps, including PrEP uptake and adherence [3, 5,6,7]. These disparities in the use of a highly effective prevention tool, if not addressed, could exacerbate the two- to five-fold higher lifetime risk of HIV among non-Hispanic Black and Hispanic MSM relative to non-Hispanic White MSM [1]. PrEP is a highly effective HIV prevention strategy, and it is important for MSM to be aware of it in addition to condoms and other HIV prevention strategies.
Prior research indicates that income, health literacy, and medical mistrust may be related to racial and ethnic disparities in PrEP awareness [11]. Experiences of provider discrimination based on race or ethnicity are also associated with lower HIV treatment adherence [12], and language barriers may affect PrEP awareness among Hispanic patients. Young MSM are unlikely to learn about PrEP through health education courses [13] and may be less connected to MSM social networks and less likely to learn about PrEP through such networks. These factors likely also contribute to racial and ethnic disparities in PrEP awareness.
It is unclear why PrEP awareness among Black MSM converged with PrEP awareness among White MSM. It is possible that public health efforts to increase PrEP awareness generally [10] or specifically among Black MSM contributed to larger increases in PrEP awareness over time. Further research exploring sources of PrEP awareness could improve understanding of trends in PrEP awareness among Black MSM and its relationship to PrEP uptake and adherence.
Given that PrEP awareness is the first step of the PrEP care continuum [8], low PrEP awareness among Non-Hispanic Black and Hispanic MSM may reduce subsequent PrEP uptake. Our findings demonstrate that it remains particularly important to increase PrEP awareness among Hispanic MSM as well as young and older adult MSM. Approaches that may improve PrEP awareness among Hispanic MSM include informing healthcare providers about the need to share information on PrEP with Hispanic MSM and providing Spanish-language materials and resources on PrEP. There is also a need for culturally-sensitive interventions focused specifically on increasing PrEP awareness and knowledge among Hispanic MSM. With Food and Drug Administration approval of generic FTC/TDF as PrEP and as innovation continues, potentially leading to novel regimens or injectable versions of PrEP, it will be critical to ensure that new advances and PrEP delivery options are communicated to Hispanic and non-Hispanic Black MSM through social marketing campaigns, by providers, and through other interventions.
Our study has a number of strengths and limitations. One strength is that we used have continuous data from the single STD program in one state that began collecting PrEP awareness questions in January 2013, and queried all STD clinic clients. A limitation is that the data come from individuals presenting to a single STD clinic who may not be representative of the MSM population in the state or nationally. We also lacked data on patient income, educational attainment, sexual orientation, and social networks that could potentially affect PrEP awareness. It is likely that MSM visiting the STD clinic are more likely to have symptomatic STDs than the general MSM population, which would also be associated with increased risk for HIV. Such risk would make PrEP particularly relevant for this population. The outcome data on PrEP awareness are also based on self-report, which may suffer from social desirability bias. However, we do not have reason to expect any social desirability bias to have differed over time, or by race or ethnicity.
Conclusion
PrEP awareness increased among MSM of each race and ethnicity during the study period, but Hispanic MSM and non-Hispanic Black MSM had significantly lower PrEP awareness relative to White MSM on average from 2012 to 2016. By 2016, PrEP awareness among non-Hispanic Black MSM converged with that of non-Hispanic White MSM, while Hispanic MSM continued to have lower PrEP awareness. Racial and ethnic disparities in PrEP awareness may lead to further disparities in PrEP uptake and adherence at later stages of the PrEP care continuum. There is a need to better disseminate information on PrEP to Hispanic MSM through approaches such as Spanish-language materials on PrEP. It will also be important to ensure that new PrEP innovations and delivery options are communicated to Black and Hispanic MSM.
References
Hess KL, Hu X, Lansky A, Mermin J, Hall HI. Lifetime risk of a diagnosis of HIV infection in the United States. Ann Epidemiol. 2017;27(4):238–43.
Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99.
Hoots BE, Finlayson T, Nerlander L, Paz-Bailey G. Willingness to take, use of, and indications for pre-exposure prophylaxis among men who have sex with men—20 US cities, 2014. Clin Infect Dis. 2016;63(5):672–7.
Siegler AJ, Mouhanna F, Giler RM, Weiss K, Pembleton E, Guest J, et al. The prevalence of pre-exposure prophylaxis use and the pre-exposure prophylaxis-to-need ratio in the fourth quarter of 2017, United States. Ann Epidemiol. 2018;28(12):841–9.
Johnsen LE, Thimm MA, Singer JM, Page KR. Awareness and interest in pre-exposure prophylaxis (PREP) among patients receiving services at a public sexually transmitted diseases (STD) clinic in a high prevalence urban setting. Sex Transm Infect. 2017;93(Suppl 2):A79.
Kuhns LM, Hotton AL, Schneider J, Garofalo R, Fujimoto K. Use of pre-exposure prophylaxis (PrEP) in young men who have sex with men is associated with race, sexual risk behavior and peer network size. AIDS Behav N Y. 2017;21(5):1376–82.
Marcus JL, Hurley LB, Hare CB, Nguyen DP, Phengrasamy T, Silverberg MJ, et al. Preexposure prophylaxis for HIV prevention in a large integrated health care system: adherence, renal safety, and discontinuation. J Acquir Immune Defic Syndr. 2016;73(5):540–6.
Nunn AS, Brinkley-Rubinstein L, Oldenburg CE, Mayer K, Mimiaga MJ, Chan PA. Defining the pre-exposure prophylaxis care continuum. AIDS. 2017;31(5):731–4.
Parsons JT, Rendina HJ, Lassiter JM, Whitfield THF, Starks TJ, Grov C. Uptake of HIV pre-exposure prophylaxis (PrEP) in a national cohort of gay and bisexual men in the United States: the motivational PrEP cascade. J Acquir Immune Defic Syndr. 2017;74(3):285–92.
Raifman J, Nunn A, Oldenburg CE, Montgomery MC, Almonte A, Agwu AL, et al. An evaluation of a clinical pre-exposure prophylaxis education intervention among men who have sex with men. Health Serv Res. 2017;53:2249–67.
Millett GA, Peterson JL, Flores SA, Hart TA, Jeffries WL, Wilson PA, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380(9839):341–8.
Thrasher AD, Earp JAL, Golin CE, Zimmer CR. Discrimination, distrust, and racial/ethnic disparities in antiretroviral therapy adherence among a national sample of HIV-infected patients. J Acquir Immune Defic Syndr. 2008;49(1):84–93.
Raifman J, Beyrer C, Arrington-Sanders R. HIV education and sexual risk behaviors among young men who have sex with men. LGBT Health. 2018;5(2):131–8.
Funding
Dr. Raifman received support from NIH Grants T32AI102623, R25MH083620, R21MH113431, and K01MH116817. Dr. Dean was supported by NIH Grants R25MH083620, K01CA184288, P30CA006973, and P30AI094189. Dr. Chan was supported by NIH Grants R34DA042648, R34MH110369, R34MH109371, R21MH113431, and R21MH109360.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
The study was approved by the presiding institutional review board (IRB), which granted a waiver of consent for the use of de-identified, secondary data from patient intake forms (The Miriam Hospital IRB Project Number 216513).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Raifman, J., Dean, L.T., Montgomery, M.C. et al. Racial and Ethnic Disparities in HIV Pre-exposure Prophylaxis Awareness Among Men Who have Sex with Men. AIDS Behav 23, 2706–2709 (2019). https://doi.org/10.1007/s10461-019-02462-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-019-02462-3