Abstract
In Botswana, 85% of persons living with HIV are aware of their status. We performed an economic analysis of HIV testing activities implemented during intensive campaigns, in 11 communities, between April 2015 and March 2016, through the Botswana Combination Prevention Project. The total cost was $1,098,312, or $99,847 per community, with 60% attributable to home-based testing and 40% attributable to mobile testing. The cost per person tested was $44, and $671 per person testing positive (2017 USD). Labor costs comprised 64% of total costs. In areas of high HIV prevalence and treatment coverage, the cost of untargeted home-based testing may be inflated by the efforts required to assess the testing eligibility of clients who are HIV-positive and on ART. Home-based and mobile testing delivered though an intensive community-based campaign allowed the identification of HIV positive persons, who may not access health facilities, at a cost comparable to other studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Botswana is an upper-middle income country with a population of 2.25 million and adult HIV prevalence is estimated at 22%, among the world’s highest [1]. UNAIDS estimates suggest that 360,000 people are living with HIV in Botswana of which 300,000 are on treatment, and 10,000 new infections occur annually [1]. Since 2016, the Government of Botswana’s Ministry of Health recommends antiretroviral treatment initiation for all HIV-infected citizens, irrespective of CD4 level [2].
HIV testing services in Botswana are widely available in antenatal settings, in facilities through provider initiated testing, and in walk-in voluntary counseling and testing (VCT) centers. UNAIDS’ 90-90-90 targets urge countries to have at least 90% of their HIV infected population know their status by 2020 and estimates suggest that, in Botswana, 83% to 85% of persons living with HIV (PLHIV) are aware of their status [3, 4]. Community testing efforts, including home-based and mobile, may be relatively cost-effective approaches to HIV case finding towards and beyond the “first 90” [5], particularly among high HIV prevalence populations unlikely to access HIV testing services through facilities.
A recent systematic review of community-based HIV testing approaches in sub-Saharan Africa estimated the per person costs of home-based testing at $9 (range: $8–$16) and the per person costs for mobile testing at $30 (range: $24–$32) [6]. Since the publication of this review, a cost analysis of HIV testing in South Africa, reported a cost per person tested of $32 for home-based testing [7]. Also in South Africa, the mean cost of mobile testing was estimated at $26, and $1095 per HIV diagnosis [8]. In Namibia, the cost of mobile testing was estimated at $69 per person tested for HIV and $656 per person testing positive [9]. Of note, South Africa, Botswana and Namibia are classified as upper middle-income countries [10], with costs more comparable to one another than countries of low-income or lower-middle income in Africa. The SEARCH study, a combination prevention trial of 32 communities across Kenya and Uganda, reported a mean cost of $14 per person tested and $160 per person testing positive through multi-disease community health campaigns [5]. The SEARCH study also reported a mean cost of $33 per person tested in their home, with a corresponding cost per person testing positive of $312 and ranging from $192 to $1390 with variability due to differences in HIV positivity rates [5]. All costs are expressed in 2017 US Dollars [11].
Data on the costs and outcomes of community-based HIV testing is critical to inform program officials and support their decision-making process for allocating scarce resources to increase HIV case identification. An understanding of the cost breakdown of HIV testing activities is key to determining the optimal mix of strategies to implement. Therefore, in this study, we examined the detailed cost of the intensive HIV testing campaign activities implemented in the Botswana Combination Prevention Project (BCPP). BCPP is a pair-matched community-randomized trial intended to evaluate the impact on HIV incidence of saturating 15 intervention communities with HIV prevention services, as compared with 15 communities in the study’s control arm [3]. We present the total cost of the intensive HIV testing community-based campaigns in BCPP, costs by category, cost per client tested and client testing positive, and estimate the cost of home-based and mobile testing activities.
Methods
The Botswana Combination Prevention Project (BCPP) is a pair-matched cluster-randomized trial designed to evaluate the impact of a package of prevention interventions on population-level HIV incidence. Within the BCPP, interventions were conducted in 15 rural or peri-urban communities, each with an average population size of 6,000. Interventions implemented as part of the combination prevention package included: intensive HIV testing campaigns, linkage to care, and universal ART. Attempts were made to reach all community residents and identify 90% of PLHIV through household enumeration, community mobilization, door-to-door home-based testing, and mobile testing. A full description of the study design is available elsewhere [3].
The present study evaluates the cost of the intensive HIV testing campaigns held across 11 communities, between April 2015 and March 2016, as part of the BCPP. To allow the intervention model to stabilize, we omitted the initial four communities of the BCPP and restricted the costing analysis to the remaining 11 communities, thus, start-up costs may be underestimated.
The intensive HIV testing campaigns consisted of community mobilization, followed by two main types of testing activities held simultaneously: door-to-door home-based testing, and mobile testing using tents. A team of mobilizers was hired locally, within each community, to promote the upcoming intensive HIV testing campaign. Mobilization activities began 1 week prior to the testing campaign and included: meeting with village leaders to gain support, posters, public announcements, door-to-door sensitization of household members, and community events (e.g. soccer games). Mobilizers remained in the community to support the testing efforts.
Once the testing activities began, HIV testing counselors worked two 4-h shifts, 5 days a week, on average. HIV testing counselors were cross-trained to deliver both home-based and mobile testing. Each morning, HIV testing counselors received their work assignment for the day. Those assigned to mobile testing for their first shift of the day, were given a site from which to operate, and drivers brought the counselors and materials such as tents, table, chairs, to the designated site. Those assigned to home-based testing for their first shift of the day, were given a list of households to visit and, as needed, drivers dropped off the testing counselors to their starting point, following which they went from door-to-door on foot. A team of HIV testing counselors stayed within a single study community for the duration of the intensive HIV testing campaign, and was then relocated to serve a subsequent community. The intensive HIV testing campaign lasted 55 days per community, on average. In BCPP, two teams, of about 35 testing counselors each, operated in parallel communities and it took nine and a half months for those two teams to complete the testing campaigns in the 11 communities.
All persons 16 years or older identified through either home-based and mobile testing activities were assessed through an intake interview and asked about their HIV status. Only those who did not know their status, did not have documentation of an HIV-positive status (ARV pill bottle, appointment card, etc.), nor documentation of an HIV-negative test within the past 3 months, were eligible for and offered HIV testing. Thus, in settings where coverage of testing and HIV prevalence were high, a large proportion of clients were assessed but not eligible for an HIV test. Following HIV testing consent, the Botswana national testing algorithm was followed and point-of-care finger stick testing was conducted. Each testing event included post-test counseling and an active referral to HIV care and treatment for those with a positive test result, or referral to applicable risk-reduction services for those with a negative test result. Known HIV-positive persons not on ART identified through the assessment were referred to the local HIV clinic. Interview and HIV test result data were collected on encrypted handheld Samsung Galaxy Tab 3 tablets, data were transferred daily to a central database and removed from the tablets for confidentiality purposes.
We performed an economic analysis using a mixed top-down and bottom-up costing approach to estimate the costs of the intensive HIV testing. The analysis was conducted from the program perspective suggesting that the costs included are those typically borne by the providers, while direct and indirect costs, and productivity losses incurred by patients and their informal caregivers were excluded. We considered all direct medical costs including labor, equipment and materials, and direct non-medical costs such as program support (training, travel, etc.) and administrative overhead. In order for the cost analysis to be useful for the projection of operational program costs, all research related costs were excluded.
We collected cost data recorded it under six main categories: labor, equipment and supplies, facilities and administrative, materials, training and events, and travel.
We estimated labor costs by analyzing salary records. For staff not involved in direct service delivery, we excluded the proportion of their time spent on research activities, in consultation with staff and managers. For HIV testing counselors, we excluded research related costs by subtracting the product of the average time spent per client on research tasks and the number of clients seen. The research tasks considered were household enumeration of residents and geo-locating of clients’ homes when they presented in a mobile testing tent. We estimated the average time spent on these research tasks per client through observation of 22 home-based visits across two communities, and 51 mobile testing events across three communities.
Resource use including type, quantity and unit cost was abstracted retrospectively from expenditure records, covering the period corresponding to the intensive HIV testing campaigns in the 11 communities from April 1, 2015 to March 31, 2016, and confirmed by interviews with staff where clarifications were needed. Vehicles were amortized linearly over 7 years, and based on experience over the course of the BCPP, laptops and computer tablets were amortized linearly over 2 years.
We present the total costs of the intensive community-based HIV testing campaigns by cost category. We detail labor costs by type of personnel including number of staff, mean monthly salary and proportion of their time allocated to intensive community-based HIV testing campaigns in BCPP. We also present total costs, cost by home-based and mobile testing activities for the following outcome measures: number of persons assessed, number of persons tested, and number of persons testing positive. To estimate the costs of the home-based and mobile testing activities, we analyzed program outcome data to estimate the number of counselor-days assigned to home-based testing and to mobile testing. We then allocated all shared costs, proportionally, based on counselors’ time assigned to home-based, and to mobile testing. Outcome data were obtained from routine monitoring program data stored in the central study database. Data analysis was performed using Microsoft Excel and SAS. All costs were collected in Botswana Pula then converted from Botswana Pula and presented in 2017 US dollars [11].
We conducted additional analyses to evaluate the impact of alternative scenarios on the cost estimates. First, we altered the staffing model to assume a locally hired team of HIV testing counselors in each community, rather than having the teams of HIV testing counselors relocate to subsequent communities. At the time of study implementation, Botswana’s national HIV testing guidelines required a two-assay parallel HIV rapid testing algorithm. In June 2016, these national guidelines were revised and Botswana is now implementing a two-assay serial testing algorithm, where the second assay is conducted only if the first is reactive, thus reducing the number of rapid test kits used [2]. In scenario analysis, we also evaluated the costs assuming Botswana’s national HIV testing guidelines required a serial, rather than parallel, HIV rapid testing algorithm, at time of implementation. We evaluated the impact of these scenarios separately and in combination with each other, and compared them to the base case.
Results
Total costs and distribution of costs within each of the six main cost categories are presented in Table 1. The cost of intensive community-based HIV testing campaigns across the 11 communities was $1,098,312, and labor costs comprised the majority (64%) of total costs. Events and travel cost US$144,552 (13%), of which $62,679 (6%) were attributed to relocating the HIV testing teams to subsequent communities. Per client materials, primarily rapid test kits, represented 10% (US$110,402) of total costs, and equipment and supplies represented 9% (US$102,384) of the total.
Labor costs totaled US$703,756 and are detailed in Table 2. Seventy HIV testing counselors, with a mean monthly salary of US$890, and 12 field-based supervisors, with a mean monthly salary of US$1524, represented a combined 83% of labor costs. Staff based at the head office, in Gaborone, represented a combined 7% of total labor costs.
Table 3 presents the costs and outcomes of the intensive community-based HIV testing campaigns, overall and by testing approach. During the intensive HIV testing campaigns across the 11 communities, 31,777 persons were assessed for HIV testing eligibility, 25,235 (79%) were tested and, of those, 1636 (6.5%) tested positive. The resulting unit costs are $35 per person assessed, $44 person tested and $671 person testing positive.
Apart from the costs of per client materials and supplies used specifically for mobile testing (i.e. tents, folding tables and chairs, etc.), all other costs included were shared across both the home-based and mobile testing activities. We estimated the cost of home-based testing activities at $659,886, and $438,426 for mobile testing activities by allocating all shared costs proportionally according to counselors’ time assigned those campaign activities. Program data including activity schedules showed that testing counselors were assigned to home-based testing 63% of the time and to mobile testing 37% of the time (data not shown). A total of 18,320 persons were assessed in their home, for a per person cost of $36, and 13,457 were assessed in a mobile venue for a per person cost of $33. Of those assessed in their home, 68% were tested, and of those assessed through a mobile venue, 95% were tested. The cost per person tested is $53 and $34 for home-based and mobile testing, respectively. Of those tested in their homes, 7% had a positive test result at $758 per positive test. In mobile settings, 6% of those tested had a positive test result for a cost of $572 per positive test.
Cost collection efforts revealed that the vast majority of costs were shared or similar across all communities, with only minor exceptions, for example, where supplies or repairs to a clinic were needed to accommodate the project staff. The mean cost of the intensive HIV testing campaigns is $99,847 per community, with 60% attributable to home-based activities and 40% attributable to mobile testing (Table 3).
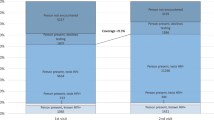
Per Fig. 1, using a serial testing algorithm would reduce the total cost by $37,785, or $1.50 per person tested; a difference directly attributable to a reduction in the cost of per client materials (see Table S1).
We also assumed a locally hired team of HIV testing counselors. In this scenario, we reduced the monthly salary of HIV testing counselors by $250 to reflect the monthly commuted allowance (Table 2) not required as compensation for staff who reside within the community. We removed the costs of temporary accommodation and delivery truck rental associated with relocation of the counselors (Table 1). And, we replaced counselors training costs with that of a 5-day training for a locally hired team of HIV testing counselors in each community. Hiring teams of testing counselors locally may require an increase in human resource management and other administrative costs; conversely, intensive testing campaigns could be held simultaneously across all communities, thereby reducing the length of time that overhead costs are incurred, therefore, in this scenario, we did not alter administrative costs. Per Fig. 1, assuming a locally hired team of HIV testing counselors, in addition to serial testing, would reduce total costs by $217,004, or $8.60 per person tested, representing a 20% reduction relative to the base case. That difference is mainly attributable to a decrease in labor and travel costs. Costs by category and by testing activity for the alternative scenarios are presented in Table S1.
Discussion
HIV case finding is becoming increasingly difficult and more costly as the proportion of PLHIV who are aware of their status increases. To define an optimal portfolio of HIV testing approaches, decision-makers must understand the costs and outcomes of all approaches, in addition to the gap in testing coverage by subpopulation, and the capacity for each approach to fill those gaps. In this economic analysis, we presented the costs of an intensive HIV community testing campaign using both home-based and mobile approaches to saturate eleven communities in Botswana with HIV testing services.
Our results indicate that the cost of an intensive HIV community testing campaign is approximately $100,000 for a rural community averaging 6000 residents. The costs presented here averaged $44 per person tested and $671 per person testing positive, which is consistent with the latest comparable cost studies of home-based and mobile testing set in upper-middle income countries in Africa. A cost analysis of home-based HIV testing in South Africa, reported a cost of $32 per person tested [7]. Also in South Africa, the mean cost of mobile testing was estimated at $26, and $1095 per HIV diagnosis [8]. In Namibia, the cost of mobile testing was estimated at $69 per person tested for HIV and $656 per person testing positive [9]. HIV testing costs are dependent on the country where the study is set, which costs are included, and the scale of the program evaluated [6]. Hospital-, clinic- or other facility-based HIV testing costs, from studies set in upper-middle income countries in Africa suggest a cost per person tested ranging from $8 to $43 [7, 12,13,14]. On average, community-based HIV testing costs are higher than facility-based approaches, however, community approaches reach persons who are less likely to access HIV testing services through facilities [6]. Community approaches are also known to be more effective at reaching persons who are asymptomatic and at an earlier stage of HIV disease, relative to provider initiated testing [6, 15].
At $36 and $33, the costs per person assessed are similar for both home-based and mobile testing activities. However, a more marked difference is apparent when comparing the costs per person tested of home-based vs. mobile activities, at $53 and $34. That difference is associated with the additional labor time needed to assess persons who were not eligible for testing because they provided documentation of their serostatus. In home-based testing, only 68% of those assessed were eligible for an HIV test while 95% of those who presented to a mobile tent for testing were eligible; presumably, because mobile testing is client-initiated and those who know their HIV status are less likely to walk into a mobile HIV testing site.
The staffing scenario evaluated indicates that costs are 20% lower assuming a locally hired team. While hiring local teams requires training those teams within each community, these additional training costs are more than offset by the reduction in moving costs, travel allowances and per diem paid to a relocating team. Consistent with most studies, labor costs are by far the largest cost component [16]. Further, the cost of the field-based staff represent 93% of the labor costs and 60% of total costs in our base case analysis. Therefore, substantial attention should be brought to the staffing model adopted in resource-constrained settings when implementing community-based HIV testing.
Scenario analysis indicates that the recent adoption of a serial testing algorithm would reduce the cost of per client materials by 34%, associated with the reduction in use of rapid test kits. There may be additional savings associated with storage and handling costs of rapid test kits as well as reduction in stock outs, which we did not attempt to quantify in the present analysis.
Our results should be interpreted in the context of several limitations. First, this analysis addresses intermediate outcomes, and does not provide unit costs per new HIV diagnosis, per person linked to care or per year of life saved; however, we expect to provide these costs in subsequent analyses. Also, given that home-based and mobile testing activities occurred simultaneously during the intensive HIV testing campaigns, the extent to which each activity impacted the efforts of the other is not known; and, the number of persons tested via mobile and home-based activities would be different should the approaches be implemented separately and sequentially. In addition, subsequent rounds of testing in BCPP communities used a different staffing and implementation model, where smaller teams of three to six testing counselors were assigned to each community continuously. We did not conduct an economic analysis of this subsequent round of testing because, having undergone the initial intensive HIV testing campaign activities, those communities would not provide grounds for a comparison of outcomes. However, the total labor costs of the testing efforts in the subsequent rounds ought to be similar to those presented here because the initial two larger teams of testing counselors were divided amongst the 15 intervention communities of the BCPP. Further, given the straightforwardness of this analysis, exploring the effects of potential variations in the input costs would not provide further insights nor measure the robustness of the results, and alternative scenarios analyses were presented in lieu of sensitivity analyses. Lastly, the comprehensive door-to-door home-based assessments conferred the additional benefit of finding already-tested HIV positive persons not on treatment or lost to follow-up, and of linking them to care; these outcomes were not considered in the present analysis.
Efforts and resources required to raise the level of knowledge of HIV status likely depend on the baseline level of knowledge, with decreasing marginal returns to scale. At baseline, knowledge of HIV-positive status across the 11 communities was 79%, which is high relative to other countries [4]. In home-based testing, 32% of clients assessed were not eventually tested, a majority of whom provided documentation of their serostatus (ART pill bottle, appointment card, or recent proof of a negative test). Settings where knowledge of HIV status is lower than that exhibited in this study may have a lower cost per test and positive test because a greater proportion of clients assessed would be eligible for testing. At time of writing, data on the increase in knowledge of HIV status in BCPP communities are under evaluation and a comprehensive analysis is forthcoming.
Conclusion
The cost of intensive HIV testing campaigns across 11 communities in Botswana, including mobilization, home-based testing, and mobile testing, is approximately $100,000 for a rural community averaging 6000 residents, and $44 per person tested. Labor is the largest cost component and attention should be brought to staffing models in order to minimize overall costs. In areas of high HIV prevalence and high treatment coverage, the cost of untargeted home-based testing may be inflated by the efforts required to assess the testing eligibility of clients who are HIV-positive and on ART. Relative to untargeted home-based testing, clients who self-select to approach a mobile testing venue are more likely to be eligible for testing, thereby spending less resources per person tested. Combined, home-based and mobile testing are effective case finding approaches for reaching those who tend not to access health facilities. This study provides detailed resource requirements that can be used to support program managers in governments and NGOs with their budgeting and decision-making process for implementing the community-based HIV testing interventions needed to increase HIV case finding and close the gap by reaching the remaining PLHIV who are unaware of their status.
References
UNAIDS. Botswana Country fact sheet. http://www.unaids.org/en/regionscountries/countries/botswana (2017). Accessed 18 Feb 2018
Botswana Ministry of Health. Handbook of the Botswana 2016 Integrated HIV Clinical Care guidelines. Botswana: Gaborone; 2016.
Gaolathe T, Wirth KE, Holme MP, Makhema J, Moyo S, Chakalisa U, et al. Botswana’s progress toward achieving the 2020 UNAIDS 90–90–90 antiretroviral treatment and virologic suppression goals: results of a population-based survey. Lancet HIV. 2016;3(5):e221–30.
UNAIDS. Ending AIDS: progress towards the 90-90-90 targets. Geneva, Switzerland: UNAIDS; 2017.
Chang W, Chamie G, Mwai D, Clark TD, Thirumurthy H, Charlebois ED, et al. Implementation and operational research: cost and efficiency of a hybrid mobile multidisease testing approach with high HIV testing coverage in East Africa. J Acquir Immune Defic Syndr. 2016;73(3):e39–45.
Sharma M, Ying R, Tarr G, Barnabas R. Systematic review and meta-analysis of community and facility-based HIV testing to address linkage to care gaps in sub-Saharan Africa. Nature. 2015;528(7580):S77–85.
Tabana H, Nkonki L, Hongoro C, Doherty T, Ekstrom AM, Naik R, et al. A cost-effectiveness analysis of a home-based HIV counselling and testing intervention versus the standard (facility based) HIV testing strategy in rural South Africa. PLoS ONE. 2015;10(8):e0135048.
Meehan S-A, Beyers N, Burger R. Cost analysis of two community-based HIV testing service modalities led by a non-governmental organization in Cape Town, South Africa. BMC Health Serv Res. 2017;17:801.
de Beer I, Chani K, Feeley FG, de Wit TFR, Sweeney-Bindels E, Mulongeni P. Assessing the costs of mobile voluntary counseling and testing at the work place versus facility based voluntary counseling and testing in Namibia. Rural Remote Health. 2015;15(4):3357.
Country income levels [Internet]. http://data.worldbank.org/country. Accessed 2 Sept 2016.
Table 1.1.9. Implicit price deflators for gross domestic product [Internet]. https://www.bea.gov/iTable/iTable.cfm?reqid=9&step=3&isuri=1&903=13#reqid=9&step=3&isuri=1&903=13 Accessed 2 Sept 2016.
Aliyu HB, Chuku NN, Kola-Jebutu A, Abubakar Z, Torpey K, Chabikuli ON. What is the cost of providing outpatient HIV counseling and testing and antiretroviral therapy services in selected public health facilities in Nigeria? J Acquir Immune Defic Syndr. 2012;61(2):221–5.
Bassett IV, Giddy J, Nkera J, Wang B, Losina E, Lu Z, et al. Routine voluntary HIV testing in Durban, South Africa: the experience from an outpatient department. J Acquir Immune Defic Syndr. 2007;46(2):181–6.
Bautista-Arredondo S, Sosa-Rubi SG, Opuni M, Contreras-Loya D, Kwan A, Chaumont C, et al. Costs along the HTC and PMTCT service cascades: findings from Kenya, South Africa, and Zambia. Rwanda: Aids; 2016.
World Health Organization. Consolidated guidelines on HIV testing services: 5Cs: consent, confidentiality, counselling, correct results and connection. Geneva: WHO; 2015.
Johnson C, Dalal S, Baggaley R, Hogan D, Parrott G, Mathews R, et al. Systematic review of HIV testing costs in high and low income settings. Consolidated guidelines on HIV testing services: 5Cs: consent, confidentiality, counselling, correct results and connection. ANNEX 5. Geneva: World Health Organization; 2015.
Disclaimer
The findings and conclusions in this paper are those of the authors and do not necessarily represent the views of the official position of the funding agencies.
Funding
This project has been supported by the President’s Emergency Plan for AIDS Relief (PEPFAR) through the Centers for Disease Control and Prevention (CDC) under the terms of Cooperative Agreements U2G GH000073 and U2G GH000419.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical Approval
The Botswana Combination Prevention Project study was approved by the Centers for Disease Control and Prevention Institutional Review Board (Protocol #6475) and the Botswana Health Research and Development Committee (HRDC; Institutional Review Board of the Botswana Ministry of Health and Wellness).
Informed Consent
Informed consent was obtained from all individual participants included in the Botswana Combination Prevention Project.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lasry, A., Bachanas, P., Suraratdecha, C. et al. Cost of Community-Based HIV Testing Activities to Reach Saturation in Botswana. AIDS Behav 23, 875–882 (2019). https://doi.org/10.1007/s10461-019-02408-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-019-02408-9