Abstract
Persons who inject drugs (PWID) continue to experience disproportionate HIV burden. Though studies demonstrate PWID find pre-exposure prophylaxis (PrEP) acceptable, awareness and uptake remains low. Data from the 2015 PWID cycle of the National HIV Behavioral Surveillance (n = 612) in Philadelphia, Pennsylvania (USA) were analyzed to evaluate how socio-demographics and behavioral factors impact PrEP awareness. Only 12.4% of PWID surveyed were PrEP-aware and 2.6% reported receiving a prescription. Factors associated with PrEP awareness included having at least some college education (aOR 2.13, 95% CI 1.03, 4.43), sharing paraphernalia (aOR 2.37, 95% CI 1.23, 4.56), obtaining syringes/needles primarily from a syringe exchange program (aOR 2.28, 95% CI 1.35, 3.87), STI testing (aOR 1.71, 95% CI 1.01, 2.89) and drug treatment (aOR 2.81, 95% CI 1.62, 4.87). Accessing prevention and health services increased the odds of being PrEP-aware; however, awareness was low overall. Additional promotion efforts are warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nearly 6.5 million persons living in the United States have injected drugs in their lifetime [1]. Persons who inject drugs (PWID) are disproportionally impacted by HIV in the United States. They comprised about 3% of adults but accounted for 6% of new HIV infections and 23% of persons living with HIV nationwide in 2015 [2, 3]. Recent estimates indicate that 1 in 23 women and 1 in 36 men who inject drugs will acquire HIV if nothing is done to prevent these infections [3]. HIV among PWID has decreased dramatically over time in large part due to the proliferation of syringe exchange programs (SEP), which reduce parenteral exposures from syringe sharing [4,5,6]. However, PWID continue to experience a disproportional vulnerability to HIV.
Pre-exposure prophylaxis (PrEP) is a promising bio-medical HIV prevention strategy that involves the daily use of antiretroviral medications by HIV-negative individuals to reduce their risk of acquiring HIV. In 2013, the Centers for Disease Control and Prevention (CDC) recommended emtricitabine/tenofovir disoproxil fumarate (FTC/TDF) as PrEP for PWID as one HIV prevention option in this population [7]. However, research and programs to bring PrEP to scale have yet to focus on PWID. Therefore, research is necessary to identify strategies to successfully promote engagement in PrEP care among at-risk PWID. This study addresses this gap by assessing factors associated with PrEP awareness, the first step in engagement in PrEP care, among PWID in Philadelphia, the most prominent heroin market in the mid-Atlantic region of the United States [8,9,10].
Drug Use and HIV Among PWID in Philadelphia
In 1991, more than 33% of persons diagnosed with AIDS in Philadelphia were PWID [11]. To combat blood-borne transmission of HIV, Prevention Point Philadelphia (PPP) began to clandestinely operate an SEP in the city. In 1992, PPP was officially sanctioned to operate an SEP [11, 12]. In addition to their SEP, PPP began offering HIV education, testing, linkage to care, and case management. In 2015, PPP served approximately 5700 unduplicated clients (J. Benitez, personal communication, January 31, 2018). Scale-up of their services, along with other SEPs in the city like Project SAFE, is correlated with decreasing HIV incidence among PWID, who represented only 5.6% of new diagnoses in 2016 [13]. Similar trends in decreasing HIV incidence have been associated with the introduction of SEP programs worldwide [4,5,6].
Awareness and Acceptability of PrEP Among PWID
The Bangkok Tenofovir Study showed that PrEP was 49–74% effective at preventing HIV acquisition among PWID taking once daily TDF as PrEP with highest rates of effectiveness among those most adherent [14]. Other clinical trials demonstrated the effectiveness of PrEP to reduce HIV transmission with use of once daily FTC/TDF among MSM [15,16,17] and heterosexual men and women [18, 19]. Compared to MSM, relatively few studies have assessed acceptability of PrEP among PWID [20]. Those that have demonstrate low PrEP awareness but high acceptability once PWID are educated about PrEP [21,22,23,24,25,26,27,28].
Study Objectives
Research that identifies strategies to successfully promote engagement in PrEP care is central to the development of high impact, cost-effective PrEP interventions. Engagement in the PrEP care continuum includes (1) awareness and willingness to use PrEP, (2) ability to access PrEP care, (3) receiving a PrEP prescription, (4) adhering to PrEP, and (5) remaining engaged in care [29]. We assessed factors associated with engagement in the PrEP continuum among PWID participating in the Philadelphia arm of the 2015 NHBS IDU-4 [30,31,32]. Our primary outcome was PrEP awareness. Secondary outcomes were discussing PrEP with a health care provider and receiving a PrEP prescription, which were assessed among only those who were aware of PrEP.
Methods
Sampling Design and Recruitment
Data are from the 2015 NHBS survey in Philadelphia among PWID. Participants were recruited using Respondent Driven Sampling (RDS) [30]. NHBS and RDS methods have been previously described in detail [31, 32]. Briefly, RDS is a modified chain recruitment strategy that utilizes social networks to tap into and derive population estimates from ‘hidden populations’ such as PWID. Study staff recruited a small number of seeds (8–10 individuals) through focus groups and community outreach. These seeds completed the survey, were offered optional HIV and Hepatitis C (HCV) testing, and were then asked to recruit up to five peers who also inject drugs. Peer respondents were offered the opportunity to be screened for eligibility; if found eligible they were also surveyed and asked to recruit up to five peers. The recruitment process continues until the desired sample size (n = 500) is achieved at the end of the study period. All participants were offered optional HIV and HCV testing and at the end of the survey were asked to recruit additional peers. Participants were compensated $25 for completing the survey, $25 for optional HIV testing, and $10 per recruit; no additional incentive was offered for HCV testing. The NHBS protocol was approved by the City of Philadelphia Institutional Review Board.
Eligible participants were 18 years of age or older, able to complete the interview in English or Spanish, in possession of a valid RDS coupon (coded, non-replicable coupons that link the recruiter and the recruit), currently living in the Philadelphia Metropolitan Statistical Area defined as: Philadelphia County, Delaware County, Montgomery County, Bucks County and Chester County, and reported injecting drugs in the 12 months prior to the interview. Participants were asked to show physical evidence of their injection (e.g., track marks). If unable to provide this, they were asked a series of in-depth injection practice questions. After consenting, eligible participants completed the procedures described above.
Measures
NHBS includes questions on socio-demographics, HIV-related risk behavior, access to and engagement in health and prevention services. For this analysis, age, current gender identity, race/ethnicity, and sexual orientation were categorized into: 18–29, 30–39, 40–49, 50 and older; male or female; non-Hispanic White, non-Hispanic Black, Hispanic/Latinx, and other; and heterosexual/straight or lesbian/gay/bisexual, respectively. Education was categorized into three groups: less than high school, high school degree/GED, and college or above. Homelessness was defined as living in the streets, a shelter, a single room occupancy hotel, or a car at any point in the past 12 months. Engagement in prevention and health services included yes/no responses to: having health insurance, any medical visit within 12 months, sexually transmitted infection (STI) testing within 12 months, and drug treatment within 12 months. Most common source of syringes in the past 12 months, our primary exposure of interest, was categorized into SEP, clinic/pharmacy, and secondary sources (e.g., friend, relative, sex partner, dealer, shooting gallery, or off the streets). We choose this variable as opposed to SEP access within 12 months because we hypothesized that there may be a dose relationship between accessing one HIV prevention service and the awareness of another, namely PrEP.
HIV risk behavior questions used a 12-month recall with yes/no responses unless otherwise noted. These included: condomless vaginal or anal sex, transactional sex, non-injection drug use, and poly-injection drug use. Use of injection drugs were categorized based on the frequency of drug use, including daily drug use vs. non-daily drug use. Sharing drug equipment in the past 12 months was categorized as, “does not share any drug equipment” (i.e., participants indicated not sharing syringes, cookers, cottons, or water), “share syringe only” (i.e., participants that indicated only sharing syringes) “sharing paraphernalia only” (i.e., participants that indicated sharing only paraphernalia such as cookers, cottons, or water), and “sharing syringes/paraphernalia” (i.e., participants that indicated sharing both syringes and paraphernalia).
The main outcome of interest was PrEP awareness defined as: “Before today, have you ever heard of people who do not have HIV taking PrEP, the antiretroviral medicine taken every day for months or years to reduce the risk of getting HIV?” Secondary outcomes, assessed among those who were aware of PrEP, included discussing PrEP with a health care provider (yes/no) and receiving a PrEP prescription (yes/no).
Analyses
Data presented here represent unweighted, cross-sectional data. χ2 tests and Fisher’s Exact tests (for expected small cell size < 5) were performed to describe the sample and assess the relationship between demographic characteristics, HIV risk behaviors, healthcare engagement, and PrEP awareness. Multicollinearity of HIV risk behaviors were assessed using variance inflation factor. No major concerns for multicollinearity were detected as estimates of variance inflation were less than 2.5. Backwards stepwise multivariable models were then manually built. All predictor variables with significance level ≤ 0.10 from the bivariate analyses were included and with covariates with significance level > 0.05 were removed after assessing for goodness of fit (i.e., Hosmer–Lemeshow goodness-of-fit test) and potential confounding (i.e., changes in effect estimates ≥ 10%). Thus, covariates with significance level > 0.05 were included in the final model if change in estimate was > 10%. Gender was included in the final multivariable model as a confounder regardless of statistical significance. All analyses were conducted using SAS 9.4 (Cary, N.C.).
Results
A total of 849 PWID were recruited. Of these, 662 participants met eligibility criteria and were screened and enrolled in the 2015 IDU IV cycle. PWID with invalid responses (n = 16), incomplete survey data (n = 10), self-reported as HIV positive either during the survey or counseling (n = 18), or those who identified as transgender (n = 5) were excluded from our analysis. In total, 612 participants with complete survey data were included in the final analysis.
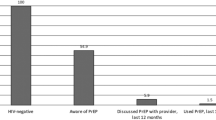
The sociodemographic characteristics, frequency and type of drug use, healthcare engagement, and HIV risk behaviors of the sample (n = 612) are detailed in Table 1. Our sample was relatively diverse in sociodemographic characteristics: 25.3% were female, 32.0% were persons of color (10.6% were non-Hispanic Black, 19.0% were Hispanic/Latinx, and 2.4% were other racial/ethnic groups), 13.7% identified as lesbian/gay/bisexual, 41.7% were age 30–39, and 71.2% had at least a high school education; various forms of health utilization and HIV risk factors were also relatively high among PWID. Of the 612 participants, only 76 (12.4%) were aware of PrEP. Of those, 14 (18.4%) PWID indicated they had discussed PrEP with a health care provider. Participants who reported being aware of PrEP compared to those unaware of PrEP were more likely to be women (35.5% vs. 23.9%, p = 0.03), lesbian/gay/bisexual participants (21.0% vs. 12.7%, p = 0.05) and have at least some college education (32.9% vs. 21.5%, p = 0.04). PrEP-aware PWID were also more likely to report attending drug treatment (71.1% vs. 47.0%, p < 0.01), receiving an STI test (56.6% vs. 39.7%, p < 0.01), sharing paraphernalia only (52.6% vs. 31.3%, p < 0.01), using non-injection drugs (86.8% vs. 73.1%, p = 0.01), and obtaining syringes primarily from an SEP (61.8% vs. 44.0%, p < 0.01). Obtaining syringes from other sources, including obtaining syringes from a clinic/pharmacy (8.2% vs. 2.6%, p = 0.08) and from secondary sources (47.8% vs. 35.5%, p = 0.05) were significantly associated with being unaware of PrEP.
After adjusting for gender in our multivariable model, significant predictors associated with PrEP awareness (see Table 2) included: higher educational attainment [adjusted odds ratio (aOR) 2.13; 95% confidence interval (CI) 1.03, 4.43], having an STI test in past 12 months (aOR 1.71; 95% CI: 1.01, 2.89), sharing paraphernalia only in past 12 months (aOR 2.0; 95% CI 1.35, 3.87), obtaining syringes primarily from an SEP in past 12 months (aOR 2.28; 95% CI 1.35, 3.87), and participating in a drug treatment program in past 12 months (aOR 2.81; 95% CI 1.62, 4.87).
Additional analyses were conducted to understand the relationship between equipment sharing behaviors and most common sources of syringes (see Table 3). PWID obtaining their syringes primarily from the SEP were less likely to share syringes and paraphernalia (unadjusted OR 0.61; 95% CI 0.43, 0.87) compared to those acquiring syringes from clinics/pharmacy/secondary sources. Furthermore, PWID reporting secondary sources as their most common source of syringes were 50% more likely (unadjusted OR 1.50; 95% CI 1.07, 2.10) and 76% more likely (unadjusted OR 1.76; 95% CI 1.24, 2.49) to share any drug equipment as well as share both syringes and paraphernalia, respectively.
Discussion
Despite high levels of ongoing injection and sexual HIV risk behaviors among PWID, PrEP awareness in this population remains very low. In our Philadelphia-based study, only one in eight (12.4%) participants reported ever hearing of PrEP. This low rate of PrEP awareness is similar to other NHBS samples in NY and Washington D.C. from the IDU-3 survey conducted in 2012 (8.9% and 13.4%, respectively) [22, 28] prior to the CDC’s endorsement of PrEP to prevent HIV among PWID in 2013 [7]. However, PrEP awareness in this sample is lower than among women who inject drugs in the New York City MSA from the same NHBS cycle in 2015 (12.4% in Philadelphia vs. 31.4% in NY) [23]. This signals a need to increase efforts to promote PrEP to this vulnerable population.
When we assessed for the independent predictors of PrEP awareness, not surprisingly, PWID who had engaged with harm and risk reduction programs such as the SEP (aOR 2.28; 95% CI 1.35, 3.87), drug treatment (aOR 2.81; 95% CI 1.62, 4.87), and sexual health services (aOR 1.71; 95% CI 1.01, 2.89) were nearly twice as likely to be aware of PrEP compared to PWID who did not access these programs within the past year. Access to an SEP had the greatest impact on PrEP awareness. Among those PrEP aware, a higher percentage reported obtaining syringes most commonly from the SEP compared to secondary sources or a clinic/pharmacy. While SEP engagement is associated with higher PrEP awareness, additional efforts are still needed to promote PrEP within these sites.
Interestingly, in a multivariable model, PWID who reported sharing only paraphernalia were significantly more likely to be PrEP aware compared to participants sharing both syringes and paraphernalia. PWID that share syringes face a greater risk for HIV acquisition than those sharing only paraphernalia since HIV can survive for 6 weeks or more within a syringe and results in infected blood being injected directly into the bloodstream [33, 34]. Further exploration of this association illustrated that PWID reporting lower risk for HIV (i.e., those endorsing no sharing or sharing only paraphernalia) were more likely to obtain their syringes from SEPs compared to those sharing paraphernalia and syringes. SEPs have long been leaders in HIV prevention to this population so it is not surprising they may lead the charge in promoting PrEP to this community.
Conversely, a greater proportion of those obtaining syringes from a secondary source such as friend, relative, sex partner, dealer, shooting gallery, or off the streets were PrEP unaware. These PWID have fewer opportunities to benefit from interaction with SEP staff or educational programs/materials at the SEP. Research has also shown that primary and secondary SEP users have a different risk profile with secondary SEP clients being more vulnerable than primary clients who directly access SEPs [35, 36].
Our findings indicate that there is untapped potential to provide PrEP education within the population of PWID that primarily utilize secondary sources for syringes. Peer-to-peer interventions are a well-established strategy for HIV prevention with this population and potentially could also work for the dissemination of PrEP information [37,38,39,40]. However, no research to date has explored the feasibility or acceptability of this approach. Despite this, we hypothesize this strategy could have great potential for reaching a large number of at-risk persons who might benefit from learning about, and potentially utilizing, PrEP.
Greater efforts are also needed to educate and prescribe PrEP in non-traditional medical settings such as STD clinics and drug treatment facilities. While research on the viability of drug treatment facilities to distribute PrEP has yet to be conducted, STD clinics are increasingly being utilized to educate and enroll vulnerable patients in PrEP services, though the focus has been primarily on MSM [41]. Although we found access to STD testing and drug treatment was associated with higher PrEP awareness, access to medical care was not. In this sample, the majority of participants had attended any medical visit, including ER visits, in the last 12 months, yet they were not more likely to know about PrEP than their peers who had not. Previous research has found that primary care providers (PCP) do not feel comfortable prescribing PrEP, which may be exacerbated for PWID who often face stigma within health care settings [42, 43]. Additional outreach to clinicians serving PWID may be needed in order to encourage them to educate and prescribe PrEP to this population. While the ER may not be the appropriate place to prescribe and follow persons on PrEP, a basic PrEP referral could be provided in this setting with appropriate follow-up.
Our data must be interpreted with the limitations of the study design and measurement. All of the data presented are self-reported and are subject to social desirability and recall biases. Since PWID were recruited from Philadelphia with a low HIV prevalence among PWID [13], findings from our MSA might not be generalizable to other cities with a higher HIV prevalence in this population. Finally, our survey did not capture detailed information on source of PrEP awareness (i.e., how participants learned about PrEP) nor whether secondary sources were safe (i.e., new syringes provided via secondary exchange or bought on the street) or not. More information in these areas would help us to better understand PrEP dissemination and the potential for other outreach and educational strategies. Additional limitations include presenting unweighted estimates of association that do not account for peer network size or clustering within recruitment chains. However, there is no reason to assume this would impact our outcome of interest given the distribution of PrEP awareness.
Conclusion
In this sample of vulnerable PWID, PrEP awareness, the first step in the continuum of PrEP care, was low. While greater efforts should be made to promote PrEP to all PWID, tailored interventions may be needed to penetrate into networks of PWID who do not access SEPs. One possible mechanism is via secondary exchange networks. This may be crucial given this subpopulation representing unserved PWID is consistently found to be disproportionately vulnerable to PWID. With additional promotional efforts, PrEP will have greater potential to prevent HIV among this vulnerable population.
References
Lansky A, Finlayson T, Johnson C, et al. Estimating the number of persons who inject drugs in the united states by meta-analysis to calculate national rates of HIV and hepatitis C virus infections. PLoS ONE. 2014;9(5):e97596.
Centers for Disease Control and Prevention. Estimated HIV incidence and prevalence in the United States, 2010–2015. HIV Surveillance Supplemental Report 2018; 23(No. 1). http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published March 2018. Accessed 28 July 2018.
Centers for Disease Control and Prevention. HIV Surveillance Report, 2016; vol. 28. http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published November 2017. Accessed 28 July 2018.
Bastos FI, Strathdee SA. Evaluating effectiveness of syringe exchange programmes: current issues and future prospects. Soc Sci Med. 2000;51(12):1771–82.
Gibson DR, Flynn NM, Perales D. Effectiveness of syringe exchange programs in reducing HIV risk behavior and HIV seroconversion among injecting drug users. AIDS. 2001;15(11):1329–41.
Aspinall EJ, Nambiar D, Goldberg DJ, et al. Are needle and syringe programmes associated with a reduction in HIV transmission among people who inject drugs: a systematic review and meta-analysis. Int J Epidemiol. 2014;43(1):235–48.
Centers for Disease Control and Prevention. Preexposure prophylaxis for the prevention of HIV infection in the United States—2014: a clinical practice guideline. https://www.cdc.gov/hiv/pdf/guidelines/PrEPguidelines2014.pdf. Accessed [17 June 2018.
Substance Abuse and Mental Health Administration, Center for Behavioral Health Statistics and Quality. The DAWN report: highlights of the 2010 drug abuse warning network (DAWN) findings on drug-related emergency department visits. Rockville, MD: 2012. https://www.samhsa.gov/data/sites/default/files/DAWN096/DAWN096/SR096EDHighlights2010.pdf. Accessed 2 May 2018.
Ciccarone D. Heroin in brown, black and white: Structural factors and medical consequences in the US heroin market. Int J Drug Policy. 2009;20(3):277–82.
U.S. Department of Justice, National Drug Intelligence Center. Philadelphia/Camden high intensity drug trafficking area drug market analysis 2011. Washington, D.C.: 2011. https://www.justice.gov/archive/ndic/dmas/Philadelphia-Camden_DMA-2011(U).pdf. Accessed 2 May 2018.
City of Philadelphia. Executive Order No. 4-92. Philadelphia, PA: 1992. https://www.justice.gov/archive/ndic/dmas/Philadelphia-Camden_DMA-2011(U).pdf. Accessed 2 May 2018.
Prevention Point Philadelphia. History of PPP. 2016. https://ppponline.org/about-us/history-ppp. Accessed 4 December 2017.
Philadelphia Department of Public Health. AIDS activities coordinating office surveillance report, 2016. Philadelphia, PA: AIDS Activities Coordinating Office, Department of Public Health, 2016. https://www.phila.gov/health/pdfs/aaco/HIV%20Surveillance%20Report-2016web.pdf. Accessed 2 May 2018.
Choopanya K, Martin M, Suntharasamai P, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2013;381(9883):2083–90.
Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99.
MRC Clinical Trials Unit. The PROUD study: examining the impact on gay men of using pre-exposure prophylaxis (PrEP), study results, key messages, questions and answers. University College London, February 24, 2015. http://www.proud.mrc.ac.uk/results/.
Molina J-M, Capitant C, Spire B, Pialoux G, Chidiac C, Charreau I. On demand PrEP with oral TDF-FTC in MSM: results of the ANRS Ipergay trial [23LB]. Presented at: Conference on Retroviruses and Opportunistic Infections; 2015; Seattle, Washington.
Thigpen MC, Kebaabetswe PM, Paxton LA, et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N Engl J Med. 2012;367(5):423–34.
Baeten JM, Donnell D, Ndase P, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367(5):399–410.
Escudero DJ, Lurie MN, Kerr T, Howe CJ, Marshall BDL. HIV pre-exposure prophylaxis for people who inject drugs: a review of current results and an agenda for future research. J Int AIDS Soc. 2014;17(1):18899.
Eisingerich AB, Wheelock A, Gomez GB, Garnett GP, Dybul MR, Piot PK. Attitudes and acceptance of oral and parenteral HIV preexposure prophylaxis among potential user groups: a multinational study. PLoS ONE. 2012;7(1):e28238.
Kuo I, Olsen H, Patrick R, et al. Willingness to use HIV pre-exposure prophylaxis among community-recruited, older people who inject drugs in Washington, DC. Drug Alcohol Depend. 2016;164:8–13.
Walters SM, Reilly KH, Neaigus A, Braunstein S. Awareness of pre-exposure prophylaxis (PrEP) among women who inject drugs in NYC: the importance of networks and syringe exchange programs for HIV prevention. Harm Reduct J. 2017;14(1):40.
Escudero DJ, Kerr T, Wood E, et al. Acceptability of HIV pre-exposure prophylaxis (PrEP) among people who inject drugs (PWID) in a Canadian setting. AIDS Behav. 2015;19(5):752–7.
Stein M, Thurmond P, Bailey G. Willingness to use HIV pre-exposure prophylaxis among opiate users. AIDS Behav. 2014;18(9):1694–700.
Roth AM, Goldshear JL, Martinez-Donate AP, Welles S, Chavis M, Van Der Pol B. Reducing missed opportunities: pairing sexually transmitted infection screening with syringe exchange services. Sex Transm Dis. 2016;43(11):706–8.
Shrestha R, Karki P, Altice FL, et al. Correlates of willingness to initiate pre-exposure prophylaxis and anticipation of practicing safer drug- and sex-related behaviors among high-risk drug users on methadone treatment. Drug Alcohol Depend. 2017;173:107–16.
Walters SM, Rivera AV, Starbuck L, et al. Differences in awareness of pre-exposure prophylaxis and post-exposure prophylaxis among groups at-risk for HIV in New York State: New York City and Long Island, NY, 2011–2013. J Acquir Immune Defic Syndr. 2017;75:S383–91.
Kelley CF, Kahle E, Siegler A, et al. Applying a PrEP continuum of care for men who have sex with men in Atlanta. Georgia. Clin Infect Dis. 2015;61(10):1590–7.
Behavioral Surveillance Team NCHSTP/DHAP-SE/BCSB. Model Surveillance Protocol, Injecting Drug Users (NHBS-IDU3) Heterosexuals at Increased Risk of HIV (NHBS-HET3). National HIV Behavioral Surveillance System Round 3; 2011.
Gallagher KM, Sullivan PS, Lansky A, Onorato IM. Behavioral surveillance among people at risk for HIV infection in the US: the National HIV Behavioral Surveillance System. Public Health Rep. 2007;122:32–8.
Lansky A, Abdul-Quader AS, Cribbin M, et al. Developing an HIV behavioral surveillance system for injecting drug users: the National HIV Behavioral Surveillance System. Public Health Rep. 2007;122:48–55.
Heimer R, Abdala N. Viability of HIV-1 in syringes: implications for interventions among injection drug users. AIDS Read. 2000;10(7):410–7.
aidsmap. Why is injecting drug use a risk for HIV transmission? NAM Publications, October 1, 2011. http://www.aidsmap.com/Why-is-injecting-drug-use-a-risk-for-HIV-transmission/page/1324128/. Accessed Jan 31 2018.
Murphy S, Kelley MS, Lune H. The health benefits of secondary syringe exchange. J Drug Issues. 2004;34(2):245–68.
Valente TW, Foreman RK, Junge B, Vlahov D. Needle-exchange participation, effectiveness, and policy: syringe relay, gender, and the paradox of public health. J Urban Health. 2001;78(2):340–9.
Latkin CA, Sherman S, Knowlton A. HIV prevention among drug users: outcome of a network-oriented peer outreach intervention. Health Psychol. 2003;22(4):332–9.
Latkin CA. Outreach in natural settings: the use of peer leaders for HIV prevention among injecting drug users’ networks. Public Health Rep. 1998;113(Suppl 1):151–9.
Garfein RS, Golub ET, Greenberg AE, et al. A peer-education intervention to reduce injection risk behaviors for HIV and hepatitis C virus infection in young injection drug users. AIDS. 2007;21(14):1923–32.
Latkin CA, Donnell D, Metzger D, et al. The efficacy of a network intervention to reduce HIV risk behaviors among drug users and risk partners in Chiang Mai, Thailand and Philadelphia, USA. Soc Sci Med. 2009;68(4):740–8.
Chan PA, Glynn TR, Oldenburg CE, et al. Implementation of preexposure prophylaxis for human immunodeficiency virus prevention among men who have sex with men at a New England sexually transmitted diseases clinic. Sex Transm Dis. 2016;43(11):717–23.
Petroll AE, Walsh JL, Owczarzak JL, et al. PrEP awareness, familiarity, comfort, and prescribing experience among US primary care providers and HIV specialists. AIDS Behav. 2017;21(5):1256–67.
Paquette CE, Syvertsen JL, Pollini RA. Stigma at every turn: health services experiences among people who inject drugs. Int J Drug Policy. 2018;57:104–10.
Disclaimers
None to report.
Funding
Supported by Grant No. 5 U1BPS003253 and funded by the Centers for Disease Control and Prevention.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest.
Ethical Approval
All procedures involving human participants were reviewed and approved by the City of Philadelphia Institutional Review Board. This study does not contain animals.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Roth, A., Tran, N., Piecara, B. et al. Factors Associated with Awareness of Pre-exposure Prophylaxis for HIV Among Persons Who Inject Drugs in Philadelphia: National HIV Behavioral Surveillance, 2015. AIDS Behav 23, 1833–1840 (2019). https://doi.org/10.1007/s10461-018-2293-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-018-2293-0