Abstract
We examined virological non-suppression (VLN) among youth ages 13–24 years receiving HIV treatment in public health facilities in six southern Malawi districts. We also tested three ART adherence measures to determine how well each identified VLN: pill counts, a Likert scale item, and a visual analogue scale. VLN was defined as HIV RNA > 1000 copies/ml. Of the 209 youth, 81 (39%) were virally non-suppressed. Male gender and stigma were independently associated with VLN; social support and self-efficacy were independently protective. Pill count had the highest positive predictive value (66.3%). Using a pill count cut-off of < 80% nonadherence, 36 (17%) of the youth were non-adherent. Of the adherent, 120 (69%) were viral suppressed. Results indicate the need to address HIV-related stigma and to bolster social support and selfefficacy in order to enhance viral suppression. In the absence of viral load testing, pill count appears the most accurate means to assess VLN.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite receiving antiretroviral therapy (ART), adolescents and young people across the globe experience substantial AIDS- related morbidity and mortality [1]. In Africa, HIV is the leading cause of death among adolescents [2]. The high mortality rate in this age group may be due in part to low levels of ART adherence that is associated with viral load non-suppression (VLN). Establishing VLN among adolescents and young people is critical for timely detection of treatment failures and in identifying the characteristics of youth who might benefit from added adherence support [3].
Virological non-suppression is of considerable public health concern as high viral loads increase the risk for onward HIV transmission including drug-resistant strains [4, 5]. Routine laboratory monitoring of HIV viral loads (VL), therefore, is critical in establishing overall VLN population trends and for effective treatment outcomes. In Malawi, as in many resource-poor settings, the epidemiological prevalence of VLN is unknown as most public treatment programs do not routinely monitor HIV viral loads. As ART is scaled up in Malawi, knowing the rate of adolescents and young people who remain virally non-suppressed is essential.
Research shows that youth are the least ART adherent of all age groups [6], possibly due to their formative stage of psychosocial and cognitive development [7, 8]. Consequently, they are less likely than adults to achieve viral suppression. VLN, in turn, has been linked to such negative factors as depression [9], HIV-related stigma [10], inadequate social support and lower medication self-efficacy [11], nondisclosure, time awareness of a HIV-positive status [10, 12], and substance use [13]. These finding are mainly from populations in the high-income countries. Therefore, it is critical to understand and address preventable factors associated with VLN among adolescents in differing economic and socio-cultural contexts including Malawi.
Social Action Theory (SAT) [14] guided the study and informed its variable selection and data analysis. SAT is a theory of behavior change that considers the importance of: (1) the context within which health behavior occurs, (2) developmentally-driven self-regulatory and social interaction processes, and (3) the mechanisms by which these variables result in health-promoting behavior (Fig. 1) [15]. SAT also posits that health outcomes are a consequence of interaction among three domains [15]. These domains are shown in italics below along with factors commonly associated or in accord with VLN:
-
1.
Contextual influences are background characteristics that include age, gender, education, years receiving ART, years aware of HIV positive status, and sexual relationship status, the contexts in which actions occur including HIV-related stigmatization [10], mood/arousal factors including depression [9].
-
2.
Self-change processes include processes of social interaction such as HIV disclosure and obtaining social support [10], motivational appraisal and medication self-efficacy [10].
-
3.
Action states refer to health protective actions including ART adherence to reduce viral load [15].
The purpose of this study was to determine the prevalence of VLN in youth ages 13–24 and to explore the factors associated with viral non-suppression among these adolescents and young people receiving ART in southern Malawi. Using viral load as the gold standard, we also tested three ART adherence measures to establish whether or not they are correlated with viral non-suppression.
Methods
Study Design
This cross-sectional study was conducted in the southern region of Malawi that has a reported HIV prevalence rate of 14.5%, which is twice that of the country’s northern and central regions [16]. Participants were recruited from district hospitals located in Blantyre, Chiradzulu, Chikwawa, Mwanza, Mangochi and Zomba. Each district hospital has an ART clinic situated within the main hospital that provides HIV care including dispensing antiretroviral therapy. District hospitals serve more clients than other clinics within their district.
Subjects and Recruitment
A total of 450 youths were recruited and completed face-to-face interviews. This analysis is based on a subset of 209 youths (13–24 years of age) whose viral load had been assessed within the 60 days prior to study enrollment and was available in their medical record. Recruitment procedures, as summarized in Fig. 2, began with a health provider (ART coordinator/manager) at each district hospital independently compiling a list with serial numbers of youth (13–24 years) appearing in a register for people living with HIV who had ever initiated ART whether or not they currently were collecting medication. For privacy reasons, this list was never shared with the research team. Each health provider was instructed to randomly sample 90 potential subjects from the list. The health provider was trained to use random number tables for sampling. The provider then contacted the young people either by phone or through a home visit to those without a phone to ensure inclusion independent of clinic attendance. Upon reaching a potential subject, the health provider described the study and provided the study team’s contact information should the youth wish to enroll in or learn more about the research before making a decision to enroll or not.
To enroll in the study, youth of either gender had to be: (1) HIV positive, (2) between 13 and 24 years of age, (3) aware of their HIV-positive status, and (4) registered for ART for at least 6 months, and (5) have had their viral load assessed within 60 days irrespective of whether or not they had received their results. Voluntary informed consent was obtained from those 18–24 years of age and both assent and parental permission from those ages 13–17. Before seeking informed consent or assent, youths were screened to establish whether or not they were aware of their HIV positive status. In Malawi, some youth may be unaware of their HIV status although they take ART. Youth who were assessed by researchers as unaware of their HIV status during initial screening were excluded, although researchers were careful not to disclose to these youths that they were HIV-positive. Figure 1 depicts the recruitment process.
Data Collection and Measurement
Three trained interviewers collected the data through face-to-face, semi-structured interviews held at either the district hospital or a clinic in the participant’s community. Data were collected from August to October 2016. To assure conceptual and cultural equivalence, the questionnaire had been translated and then back-translated between English, Chichewa and Yao. Young people could choose which of the three languages in which to be interviewed. Visual prompt cards used successfully in prior Malawi studies helped to facilitate responses to the Likert rating. The following measures were used in the data collection:
Demographics and HIV clinical characteristics: Participants self-reported their age, gender, participation in a sexual relationship or not, years they had known their HIV-positive status, and highest level of education attained. The date that ART was initiated was abstracted from the respondents’ clinical records.
Depression was measured using the Self-Reporting Questionnaire (SRQ 20), a WHO 20-item depression scale that had been previously validated and used with women in Malawi [17]. Respondents answered “yes” or “no” to items asking if certain symptoms occurred over the preceding 4 weeks [17]. The summing of affirmative answers yielded an SRQ score between 0 and 20 with a Cronbach’s alpha in the current study of 0.83.
HIV-related stigma was assessed by the HIV/AIDS Stigma Instrument-PLWA (HASI-P), which previously had been validated in Malawi [18]. The instrument measures internalized and enacted stigma. The items for the HASI-P are scored from 0—never; 1—once or twice; 2—several times; and 3—most of the time. Two of the scale’s items originally asked about stigma in the work place. These were adapted to make them more relevant for youth as most of the study sample were either students or unemployed. For example, the item “someone tried to get me fired from my job” was adapted to “someone tried to get me removed from a sports team/or group.” In the current study, the Cronbach’s alpha was 0.93.
Social support was measured using the Multidimensional Scale of Perceived Social Support (MSPSS) that measures respondents’ perception of support received from three sources: significant other, family, and friends. The scale had been adapted and validated in Malawi with a Cronbach’s alpha of 0.9 [19]. In this study, the Cronbach’s alpha was 0.81. The ratings of the measure were dichotomized using the mean score as the cutoff point [20] and coded 0 for poor and 1 for adequate to present the magnitude of social support received. In the logistic regression, the continuous score was standardized.
ART Medication self-efficacy, defined as a measure of confidence in one’s ability to take medicine as prescribed, was assessed using the Adherence Self-Efficacy Scale (HIV-ASES). HIV-ASES is a 12-item scale that measures an individual’s confidence in taking medication as prescribed under differing conditions [21]. Responses range from 1 (cannot do it at all) to 10 (certain that I can) [21]. This scale had never been validated in Malawi, and thus was subjected to rigorous translation and back-translation before its use. In this study, the Cronbach’s alpha was 0.81. A self-efficacy score was computed for each participant. Ratings of the scale were dichotomized using the mean score as the cutoff point [20] and then coded 0 for low level and 1 for high level of self-efficacy.
ART adherence was assessed using three approaches: pill count (PC), visual analogue (VAS), and a single Likert formatted item. The three approaches measured adherence to medication over the last 4 weeks. The adolescent’s pill count adherence rate was abstracted from a printout affixed to the patient’s health passport. The printout was generated by an electronic medical record (EMR) system that performs clinical calculations including ART adherence [22]. Individual ART adherence rates were calculated based on the number of unused pills that the adolescents brought back when refilling their monthly ART medication. The VAS was presented to the participant as a numerical scale of proportion of doses taken, anchored by 0 and 100 on either end of a horizontal line. Youth were asked to mark an X on the line representing their ART adherence for the past 30 days. The resulting VAS score reported a percentage from 0% (complete nonadherence) to 100% (complete adherence). Youth also were asked to respond to the question: “In the past 4 weeks, how was your ability to take your anti-HIV medications that were prescribed by your doctor?” [23]. Responses ranged on a 5-point Likert-style format from “very poor” to “excellent.” In recognizing that the youth had differing levels of literacy comprehension, the Likert response categories were depicted on a non-verbal continuum from a bright “happy” face (“excellent”) to a grey “sad” face (“very poor”). Similar prompt cards to aid response have been used successfully in Malawi [19].
The three measures of medication adherence were dichotomized into adherent and non-adherent based on two cut-off points, 80% and 95%. These cut-off points were chosen based on current adherence literature. A meta-analysis of 43 studies designed to determine the relationship between cut-off point optimal adherence to ART and virological outcomes concluded that the threshold needed to achieve better virological outcomes was wider than the commonly used cut-off point of ≥ 95% [24]. Consequently, we examined virologic outcome with cut-off points of both 95% and 80%.
Viral load and the timing of the last determination were abstracted from the participants’ medical records. Prior to the timing of this research, physicians only initiated VL evaluations when virologic failure was suspected. In the period that corresponds to this study, a new program had been rolled out that called for assessing all adolescents. Nonetheless, although their specimens had been submitted to a central laboratory for analyses, many youths’ results had yet to be returned to the ART clinics. Upon completion of their interview, adolescents with pending results were instructed to submit them to the study when available. Youths whose results were unavailable when the study’s data collection period ended were excluded from the current analysis. Viral load was dichotomized to suppressed and unsuppressed. Viral load non-suppression was defined as HIV RNA > 1000 copies per ml of plasma based on WHO recommendation [3]. Malawi is currently using this WHO threshold [25].
The variable, “years known HIV-positive” was collected by asking the youth how long ago they learned about their HIV-positive status. Such awareness could have occurred as the result of having tested positive for HIV or when informed about perinatal infection. The variable “years on ART” was extracted from the youths’ health records. Variables “disclosure” and “alcohol use” were measured through a direct question. For disclosure, they were asked whether or not they had disclosed their HIV status to a friend. For alcohol use, they were asked about having ever consumed alcohol.
Data Analysis
The data were analyzed using SPSS version 23.0. Bivariate analyses were conducted to assess the association between demographic characteristics and study variables with HIV viral non-suppression. Viral non-suppression was dichotomized (< or ≥ 1000 copies/ml). χ2 tests were used for testing association with categorical variables. We used t-tests to compare continuous variables with HIV RNA viral load. Our continuous variables (HIV-related stigma, depression, social support and self-efficacy) were standardized for all regression analysis so that the results reflect an effect based on one standard deviation (SD) change in these variables on the odds of being VL non-suppressed. Before continuous variables were standardized, bivariate correlational analyses (not shown) employing Variance Inflation Factor (VIF), a collinearity statistic, showed no multicollinearity among the variables.
We dichotomized ART nonadherence based on two established cutoff points (< 80% vs. < 95%) in order to conduct validation tests to determine the measure(s) that could reliably be used to predict viral load non-suppression [26, 27]. Bivariate simple logistic regression determined the unadjusted odds ratio (uOR) of the demographic and other correlates with the outcome—virological non-suppression. In examining the correlates of viral load non-suppression, all contextual and self-change process variables of SAT were treated as independent variables in the regression models while the action states outcome variable (viral load) was the dependent variable.
Multivariate logistic regression analysis assessed adjusted associations between VL non-suppression. All variables associated with VLN at the p < 0.25 level from the bivariate analysis were included in order to estimate correlates that might independently determine it.
In both simple and multivariate logistic regression, standardized continuous variables (HIV-related stigma, depression, social support and self-efficacy) were used. The results reflect the odds of being viral non-suppressed by one (1) SD increase in the independent variables.
We compared the three adherence measures using specificity, sensitivity, and positive and negative predictive values for each measure computed from contingency tables generated in SPSS. The PPV represents the measures’ (test) ability to identify a person who was non-adherent and non-suppressed. A Chi square test determined whether or not significant difference existed between the measures’ adherence result and suppression outcome. The differences were statistically significant for all three measures.
Results
Respondent Characteristics
Table 1 shows the characteristics and results of the bivariate simple logistic regression of the 209 youth who had their viral load examined within 60 days prior to being interviewed. Slightly more than half (53%) of the youth were between 13 and 16 years of age while 11% were 21–24 years old. More than half of the sample were female (57%) and most (79%) of the youth were in a sexual relationship. Nearly two-thirds of the youth (59%) were attending or had graduated from primary school. Almost half of the youths had been aware of both their HIV status and been receiving ART for a period of 5–8 years. Only 9 (4%) participants reported consuming alcohol. Approximately 70% had not disclosed their HIV status to a friend.
While no differences were found by age or relationship status in the proportion of youth who were viral non-suppressed versus suppressed, gender differences did exist with more males (47%) being non-suppressed than females (OR 1.89 (1.06–3.27). Also, the odds of VLN were greater among those with higher mean scores of stigma (OR 2.49, 95% CI 1.63–3.78) and depression (OR 1.33, 95% CI 0.99–1.78) and with lower mean scores on social support (OR 0.68, 95% CI 0.51–0.89) and self-efficacy (OR 0.58, 95% CI 0.43–0.78).
Validation of Adherence Measures
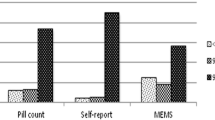
Viral load was used to validate the study’s three adherence measures that were dichotomized into adherent versus non-adherent (Table 2). Viral load was dichotomized into suppressed (< 1000 cells/ml) and unsuppressed (≥ 1000 cells/ml) based on the cut-off point used by the Malawi government as well as recommended by WHO [25]. Pill count had the highest positive predictive value (PPV), 66.3% versus 48.2% for the Likert item and 45.2% for the VAS. Pill count also had the highest negative predictive value (80.5%) followed by the Likert item (72.3%) and VAS (66.4%). Both the sensitivity and specificity of pill counts in assessing viral load were higher than for either the Likert item or VAS, suggesting that this method misses fewer cases of non-suppression and more accurately reports actual cases (see Table 2).
Virological Non-suppression and ART Non-adherence
Results using ≥ 1000 cells/ml to depict non-suppression indicate that 39% of youth were virally non-suppressed. Using a cut-off point of < 80.0% to define ART nonadherence, 17% were ART non-adherent based on pill counting, 11% were non-adherent based on the Likert measure, and 15% based on VAS. Using a cut-off point of < 95.0% to define nonadherence (Table 3), nonadherence rates were 41.1% (pill count), 53.6% (Likert measure) and 44.5% (VAS).
Multivariate Logistic Regression Results
Multivariate logistic regression included all variables in the bivariate analysis with a p value < 0.25. Results indicate for every unit increase in HIV-related stigma, the odds of being virally unsuppressed increased by 1.08 (aOR 1.08, 95% CI 1.03–1.1.13). A one-unit increase in social support and self-efficacy, however, decreased the odds of being unsuppressed (aOR 0.97, 95% CI 0.94–0.99) and (aOR 0.79, 95% CI 0.63–0.98) respectively. Years knowing one’s HIV status and depression were not significantly associated with non-suppression after adjusting for confounders (Table 4).
Discussion
This study may well be the first to examine the rate of VLN and its correlates among adolescents and young people in Malawi. In analyzing our data, we found that more than a third (39%) of the youths in southern Malawi are virally non-suppressed. This result is worrisome given the negative individual and public health consequences of VLN. Our findings also indicate that Malawi is far from achieving the UNAIDS target of 90% of PLWH being virally suppressed among its youth.
While it is difficult to compare our non-suppression results with other studies due to variations in the thresholds utilized, the observed rate in our study appears higher than those found in other studies in Sub-Saharan Africa. For example, a study in Uganda using the same VL non-suppression threshold of > 1000 copies/ml found a lower proportion of non-suppression among three different youth age groups: 57% (10–14 years), 27% (15–19 years) and 16% (20–24 years) [3]. Eight studies among adolescents in South Africa, using a different VL threshold of > 400 copies/ml, reported lower non-suppression rates ranging from 7 to 27% [28]. Meanwhile, higher rates of VLN among youth have been reported in non-SSA countries using a different threshold of > 50 copies/ml among youth. A study in Brazil among adolescents 13–18 years found that 51% were virally unsuppressed while a study in USA among youth 12–24 years found that 49% of the participants had undetectable plasma HIV RNA [29, 30].
Since adherence to treatment is the strongest determinant of virological response to ART [31], and because viral load testing is not available in many care and treatment facilities in Malawi, we examined three different measures of adherence to establish which might be useful to apply under conditions when viral load counts are unavailable [32]. Our findings indicate that pill count, an adherence objective measure, had the highest sensitivity, specificity, and PPV compared to the two self-reporting measures (VAS and a Likert item). In the absence of the capacity to measure viral load and any other validated measure, pill counts appear to be the best available tool to determine suboptimal ART adherence and also to select patients for viral load measurement. The use of pill counting, however, also has limitations. For example, mere removal of pills from the medication bottle does not guarantee that the antiretroviral tablets were consumed given the possibility of pill dumping. Also, the relative strength of a single item Likert item in predicting viral non-suppression is noteworthy and implies that researchers can use this self-report measure as a relatively quick and easy- to-collect indicator of adolescent and young adult ART adherence. VAS did not perform as well as pill count or the Likert measure, but possibly could prove useful in circumstances where other indicators are infeasible.
Research suggests that the more recent antiretroviral regimens are more forgiving than in the past. With these newer medications, adherence levels as low as 80% might be sufficient to achieve viral suppression similar to the stricter levels of > 95% adherence [33]. As true in many SSA countries, however, the first-line regimen in Malawi when this study was conducted was neither the long-acting nor the daily single fixed-dose formulation [2]. Consequently, encouraging youth to achieve levels of adherence higher than 80% seems advisable. Furthermore, the observed nonadherence level at < 95% cut-off point (41%) was comparable to viral non-suppression (39%) in our study, thus strengthening the premise that levels of adherence as high as > 95% should be the recommended goal. Nonetheless, by reporting both the < 80% and 95% adherence rates, our study helps to make our findings comparable to research that use either of these cut-off points. For example, a study in Malawi of adolescents (12–18 years) found that 44% reported ever missing a dosage in the past 30 days [2]. This finding is similar to the 41% level of nonadherence at a < 95% cut-off point reported in our study.
At a < 80% cutoff point using pill counting, nearly a fifth of the youth were non-adherent while more than a third was non-adherent at < 95%. These findings point to the need for adherence-enhancing interventions that are specially tailored for the youth to help ensure better clinical outcomes. Furthermore, it is important for HIV-positive youths to achieve viral suppression to reduce the chances of infecting others. This is especially critical for a country like Malawi with high HIV prevalence [34].
Examining factors associated with VLN within the background contextual domain of Social Action Theory, gender was found to be associated with VLN in bivariate analysis although the association did not remain significant in a model adjusting for covariates. Thus, in bivariate analysis our findings show that males were more likely to be viral non-suppressed than females. This result runs contrary to findings on gender from a U.S. study of HIV patients 12 years of age or older in which females showed twofold odds of having virological failure when compared to males [35].
A recent study of adherence among adolescents in Malawi [2] found alcohol use to be independently associated with missing ART dosages in the past 30 days. As with this study, our research found low alcohol consumption rates among participants even though our sample included a wider range of young people ages 13–24 as compared to 13–18. Nonetheless, alcohol use was not associated with VLN in our study.
Stigma, an action context factor within SAT, was determined in our study to be independently associated with viral load non-suppression. This finding is consistent with results from various studies of adults that were conducted in western world countries as well as SSA [10, 36]. Stigma also has been found to affect younger people more than their older counterparts [3]. This normative tendency should be considered when developing interventions to counter the negative influence of stigma on viral suppression among youth.
The self-change domain of SAT includes social interaction and motivational appraisal processes. Our study found that social support, a social interaction process factor, was independently associated with viral load non-suppression. A large body of research in SSA also confirms a positive association between social support and ART adherence [37]. Our study’s finding that low levels of social support were associated with viral non-suppression echoes what has been found in studies with adults and extends these findings to adolescents and young people within the Malawian context [2].
Low medication self-efficacy, a motivational appraisal factor within the SAT self-change domain, was independently associated with viral non-suppression. This finding is consistent with research that found higher levels of ART medication self-efficacy to be associated with ART adherence [38]. Prior studies [10, 36] depict high self-efficacy to be protective of viral load non-suppression. Conversely, a study of adolescents in Malawi found poor self-efficacy to be associated with ART nonadherence [2]. Medication self-efficacy can be very challenging for youth, particularly in terms of their confidence in taking medication in the presence of people unaware of their HIV positive status [39]. Such challenges need to be countered through strategies designed to address these barriers to adherence, especially for young adolescents transitioning from caregiver-medicated to autonomous medicating. Interventions are needed that enhance adolescents’ self-belief and provide skills that allow them to overcome barriers to successful self-medication.
Overall, our study demonstrates that both SAT’s contextual influence and self-change process domains (stigma, social support and self-efficacy) are strongly associated with VLN among the youth in Malawi. That both domains independently influence non-suppression possibly warrant a holistic approach to ART adherence interventions guided by SAT.
Limitations of the Study
This study has several noteworthy limitations. Due to financial and time constraints, we were unable to assess viral load ourselves and at one-time period for all participants. Rather, these were evaluated 60 days prior to enrollment and administration of the questionnaire. Another limitation is that many youths’ viral load either had not been assessed or they had not received their results. Therefore, the possibility of selection bias exists if health workers’ choice of people for whom to evaluate their viral load was influenced by suspicion of viral suppression failure. We believe, however, that the reasons for missing viral load results were unrelated to individual participants’ characteristics (including adherence) or their healthcare providers. Rather, viral load results were missing for substantial numbers of participants because the central laboratory where the assessments were to be conducted was unable to cope with the high demand. Another limitation is that our data were cross-sectional; therefore, the temporal relationship among variables studied is unknown and associations observed cannot be interpreted as causal. We initially intended to include CD4 cell count and/or the WHO stage for when ART was initiated, but these data were only available for a few participants. Another limitation, in order to protect privacy, a health provider belonging to the ART clinic identified and invited potential respondents. Consequently, we do not know how many youths receiving ART were in the registry or the personal characteristics of adolescents who might have been invited to join the research but declined. As a result, we cannot assess if youth who contacted the research team differed in key characteristics or adherence-related behavior from those who did not.
Conclusions
The study addresses the need for information about youth’s viral load non-suppression and its associated factors in planning effective HIV interventions for Malawian young people. Our results reveal that in southern Malawi, the proportion of adolescents and young people virally unsuppressed is high. Much effort will be required to meet the UNAIDS 90% viral suppression target. Interventions aiming at enhancing ART adherence that target the youth in Malawi must consider addressing HIV-related stigma and also increasing social support and self-efficacy. Such actions are critical in meeting the UNAIDS proposed “90-90-90” targets that aim to have 90% of all people receiving ART to be virally suppressed by 2020 [40].
References
Slogrove AL, Sohn AH. The global epidemiologyof adolescents living with HIV: time for more granular data to improve adolescent health outcomes. Curr Opin HIV AIDS. 2018;13(3):170–8.
Kim MH, Mazenga AC, Yu X, et al. High self-reported non-adherence to antiretroviral therapy amongst adolescents living with HIV in Malawi: barriers and associated factors. J Int AIDS Soc. 2017;20(1):1–12.
Bulage L, Ssewanyana I, Nankabirwa V, et al. Factors associated with virological non-suppression among HIV-positive patients on antiretroviral therapy in Uganda August 2014–July 2015. BMC Infect Dis. 2017;17(1):326.
Dworkin MS, Douglas GW, Sabilha Rani GP, Chakraborty A. Adherence to highly active antiretroviral therapy in Hyderabad, India: barriers, facilitators and identification of target groups. Int J STD AIDS. 2016;27(3):186–95.
Shubber Z, Mills EJ, Nachega JB, et al. Patient-reported barriers to adherence to antiretroviral therapy: a systematic review and meta-analysis. PLoS Med. 2016;13(11):e1002183.
Hudelson C, Cluver L. Factors associated with adherence to antiretroviral therapy among adolescents living with HIV/AIDS in low- and middle-income countries: a systematic review. AIDS Care. 2015;27(7):805–16.
Ramaiya MK, Sullivan KA, O’Donnell K, et al. A qualitative exploration of the mental health and psychosocial contexts of HIV-positive adolescents in Tanzania. PLoS ONE. 2016;11(11):e0165936.
Folayan M, Odetoyinbo Morolake, Brown B, Harrison A, et al. Addressing the socio-development needs of adolescents living with HIV/AIDS in Nigeria: a call for action. Afr J Reprod Health. 2014;18(3):93–101.
Kacanek D, Angelidou K, Williams PL, Chernoff M, Gadow KD, Nachman S. Psychiatric symptoms and antiretroviral nonadherence in US youth with perinatal HIV: a longitudinal study. AIDS. 2015;29(10):1227–37.
Denison JA, Banda H, Dennis AC, et al. “The sky is the limit”: adhering to antiretroviral therapy and HIV self-management from the perspectives of adolescents living with HIV and their adult caregivers. J Int AIDS Soc. 2015;13(18):19358.
Kang E, Delzel DA, Chhabra M, Oberdorfer P. Factors associated with high rates of antiretroviral medication adherence among youth living with perinatal HIV in Thailand. Int J STD AIDS. 2015;26(8):534–41.
Xu L, Munir K, Kanabkaew C, Le Coeur S. Factors influencing antiretroviral treatment suboptimal adherence among perinatally HIV-infected adolescents in Thailand. PLoS ONE. 2017;12(2):e0172392.
MacDonell KK, Jacques-Tiura AJ, Naar S, Fernandez MI. Predictors of self-reported adherence to antiretroviral medication in a multisite study of ethnic and racial minority HIV-positive youth. J Pediatr Psychol. 2016;41(4):419–28.
Ewart CK. Social action theory for a public health psychology. Am Psychol. 1991;46(9):931–46.
Traube DE, Holloway IW, Schrager SM, Kipke MD. Utilizing Social Action Theory as a framework to determine correlates of illicit drug use among young men who have sex with men. Psychol Addict Behav. 2012;26(1):78–88.
Avert. HIV and AIDS in Malawi. 2015 01 May 2015 (cited 2015 30 December); http://www.avert.org/professionals/hiv-around-world/sub-saharan-africa/malawi.
Stewart RC, Umar E, Tomenson B, Creed F. Validation of screening tools for antenatal depression in Malawi–a comparison of the Edinburgh postnatal depression scale and self reporting questionnaire. J Affect Disord. 2013;150(3):1041–7.
Holzemer WL, Uys LR, Chirwa ML, et al. Validation of the HIV/AIDS stigma instrument—PLWA (HASI-P). AIDS Care. 2007;19(8):1002–12.
Stewart RC, Umar E, Tomenson B, Creed F. Validation of the multi-dimensional scale of perceived social support (MSPSS) and the relationship between social support, intimate partner violence and antenatal depression in Malawi. BMC Psychiatry. 2014;14:180.
Nakimuli-Mpungu E, Mojtabai R, Alexandre PK, et al. Lifetime depressive disorders and adherence to anti-retroviral therapy in HIV-infected Ugandan adults: a case-control study. J Affect Disord. 2013;145(2):221–6.
Johnson MO, Neilands TB, Dilworth SE, Morin SF, Remien RH, Chesney MA. The role of self-efficacy in HIV treatment adherence: validation of the HIV treatment adherence self-efficacy scale (HIV-ASES). J Behav Med. 2007;30(5):359–70.
Douglas GP, Gadabu OJ, Joukes S, et al. Using touchscreen electronic medical record systems to support and monitor national scale-up of antiretroviral therapy in Malawi. PLoS Med. 2010;7(8):e1000319.
Feldman BJ, Fredericksen RJ, Crane PK, et al. Evaluation of the single-item self-rating adherence scale for use in routine clinical care of people living with HIV. AIDS Behav. 2013;17(1):307–18.
Bezabhe WM, Charmers L, Bereznicki LR, Peterson GM. Adherence to antiretroviral therapy and virologic failure: a meta-analysis. Medicine (Baltimore). 2016;95(15):e3361.
Centers for Disease Control and Prevention (CDC), ICAP, Columbia University Mailman School of Public Health, Johns Hopkins University, Ministry of Health (Malawi), Statistical Center for HIV/AIDS Research and Prevention (SCHARP), University of Malawi College of Medicine, Westat. Malawi Population-Based HIV Impact Assessment 2015–2016. 2016.
Smith C, Gengiah TN, Yende-Zuma N, Upfold M, Naidoo K. Assessing adherence to antiretroviral therapy in a rural paediatric cohort in KwaZulu-Natal, South Africa. AIDS Behav. 2016;20(11):2729–38.
Kerschberger B, Boulle AM, Kranzer K. Superior virologic and treatment outcomes when viral load is measured at 3 months compared to 6 months on antiretroviral therapy. J Int AIDS Soc. 2015;18:20092.
Zanoni BC, Archary M, Buchan S, Katz IT, Haberer JE. Systematic review and meta-analysis of the adolescent HIV continuum of care in South Africa: the cresting wave. BMJ Global Health. 2016;1(3):e000004.
Cruz ML, Cardoso CA, Darmont MQ, et al. Viral suppression and adherence among HIV-infected children and adolescents on antiretroviral therapy: results of a multicenter study. J Pediatr (Rio J). 2014;90(6):563–71.
Saberi P, Mayer K, Vittinghoff E, Naar-King S. Correlation between use of antiretroviral adherence devices by HIV-infected youth and plasma HIV RNA and self-reported adherence. AIDS Behav. 2015;19(1):93–103.
Burch LS, Smith CJ, Anderson J, et al. Socioeconomic status and treatment outcomes for individuals with HIV on antiretroviral treatment in the UK: cross-sectional and longitudinal analyses. Lancet Public Health. 2016;1(1):e26–36.
Simoni JM, Kurth AE, Pearson CR, Pantalone DW, Merrill JO, Frick PA. Self-report measures of antiretroviral therapy adherence: a review with recommendations for HIV research and clinical management. AIDS Behav. 2006;10(3):227–45.
Sutton SS, Magagnoli J, Hardin JW. Odds of viral suppression by single-tablet regimens, multiple-tablet regimens, and adherence level in HIV/AIDS patients receiving antiretroviral therapy. Pharmacotherapy. 2017;37(2):204–13.
Boily MC, Masse B, Alsallag R, et al. HIV treatment as prevention: considerations in the design, conduct, and analysis of cluster randomized controlled trials of combination HIV prevention. PLoS Med. 2012;9(7):e1001250.
Mave V, Gahunia M, Frontini M, Clark R, Mushatt D. Gender differences in HIV drug resistance mutations and virological outcome. J Womens Health (Larchmt). 2011;20(1):117–22.
Sumari-de Boer IM, Sprangers MA, Prins JM, Nieuwkerk PT. HIV stigma and depressive symptoms are related to adherence and virological response to antiretroviral treatment among immigrant and indigenous HIV infected patients. AIDS Behav. 2012;16(6):1681–9.
Croome N, Ahluwalia M, Hughes LD, Abas M. Patient-reported barriers and facilitators to antiretroviral adherence in Sub-Saharan Africa: a systematic review. AIDS. 2017;31(7):995–1007.
Tran BX, Nguyen LT, Nguyen NH, Hoang QV, Hwang J. Determinants of antiretroviral treatment adherence among HIV/AIDS patients: a multisite study. Glob Health Action. 2013;6:19570.
Reif S, Proeschold-Bell RJ, Yao J, et al. Three types of self-efficacy associated with medication adherence in patients with co-occurring HIV and substance use disorders, but only when mood disorders are present. J Multidiscip Healthc. 2013;6:229–37.
Abrams EJ, Strasser S, Kranzer K. 90-90-90—Charting a steady course to end the paediatric HIV epidemic. J Int AIDS Soc. 2015;18:20096.
Acknowledgements
We thank the study’s participants for their time and participation. We also are grateful to the health providers at each district hospital for their help in recruiting our study sample. Support for the study was provided through a dissertation award to the senior author by the UIC AIDS International Training and Research Program through funding from the John E. Fogarty International Center of the National Institutes of Health (D43 TW001419).
Funding
This study was funded by Fogarty AIDS International Training and Research Program (AITRP) (Grant No.: D43 TW001419).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Ethical Approval
Study procedures, instruments, and all materials were reviewed and approved by the Institutional Review Boards of the University of Illinois at Chicago and the University of Malawi’s College of Medicine Research and Ethics Committee. All procedures involving human participants were conducted in accord with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Voluntary informed consent was obtained from those participants who were 18-24 years of age and both assent and parental permission from those ages 13-17.
Rights and permissions
About this article
Cite this article
Umar, E., Levy, J.A., Bailey, R.C. et al. Virological Non-suppression and Its Correlates Among Adolescents and Young People Living with HIV in Southern Malawi. AIDS Behav 23, 513–522 (2019). https://doi.org/10.1007/s10461-018-2255-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-018-2255-6