Abstract
Uptake of contraceptives is generally low in low-income settings. For women with HIV, contraception is a reliable and affordable method of minimizing vertical transmission. We investigated the factors that affect contraceptive use among Kenyan women using data collected during the Kenya Demographic & Health Survey (KDHS) of 2014. Data on contraceptive use were extracted from the 2014 KDHS database. Records of 31,079 Kenyan women of reproductive age (15–49 years) were analyzed. Frequencies were calculated; cross-tabulations and bivariate and multivariate analyses were conducted. Twelve thousand thirty-two women (39%) reported using a contraceptive method. Region, religion, education, number of living children, marital status, and prior testing for HIV were significantly associated with contraceptive use among women (P < 0.001). Social, economic, and demographic factors predict contraceptive use among Kenyan women and should be addressed in order to increase contraceptive uptake.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sub-Saharan Africa had the highest fertility rate globally, at four or more children born per woman, in the years 2010–2015 [1]. The proportion of women of reproductive age who use contraceptives is 22%, which is lower than half the rate in South Asia (53%) and a third the rate in East Asia (77%) [2]. The population in sub-Saharan Africa continues to grow at a rate of 2.3% because of declining mortality coupled with high fertility [2]. While contraceptive use is increasing by 0.7% per year across the African continent, many women still have difficulties accessing contraceptives [3].
HIV-infected women in sub-Saharan Africa are at great risk for unwanted pregnancy [4]. Use of contraception is important in preventing unwanted pregnancy and is a reliable and affordable method of preventing vertical transmission of HIV from mother to child [5]. In India, on average, 10.3% of women living with HIV reported that their current pregnancy was unwanted [6]. Among pregnant HIV-positive women participating in a Nigerian study [7], 37.2% confirmed not wanting their pregnancy. Similarly, in a recent study in eastern and southern Africa [8], approximately 24% of all deaths among pregnant and postpartum women were associated with HIV. More than 40% of pregnancies in Kenya are either unwanted or mistimed [9]. Through mother-to-child transmission of HIV, Kenya is accountable for 4% of all new pediatric HIV infections globally and 7% of all child deaths [10].
Several decades after the introduction of modern contraceptive methods, Kenya’s population continues to grow and is projected to exceed 60 million by 2025 [11]. Like other developing countries, Kenya experienced a decline in fertility, from 4.9 births per woman in 2003 to 3.9 births per woman in 2014 [12]. However, the decline in fertility has stagnated due to factors such as reduced availability of modern contraceptive methods, diversion of resources to HIV/AIDS prevention and treatment, and inadequate support for family planning programs [11]. According to the Kenya Demographic & Health Survey (KDHS) 2008–2009, contraceptive-use prevalence was 46%, a result that did not meet the 2010 benchmark of 62% set by the Kenya National Population Policy for Sustainable Development in the year 2000. KDHS 2008–2009 further reported that the use of modern contraceptives was low (37.6%) in urban Kenya [13]. The rapid population growth driven by high fertility poses serious challenges for social and economic development.
In Kenya, there is limited research on contraceptive use among women. We sought to determine the prevalence and factors associated with use of contraceptives among Kenyan women of reproductive age to inform the improvement of family planning services.
Methods
Study Design
This study was a secondary analysis of data from the KDHS 2014, a national survey conducted by the Kenya National Bureau of Statistics (KNBS) in partnership with other government and donor agencies [12]. KNBS conducts surveys every 5 years to monitor population and health in Kenya. The KDHS provides estimates of selected demographic and health indicators at the national level. It also provides data on general health, family planning, and HIV/AIDS programs needed by the government to effectively plan and implement future interventions.
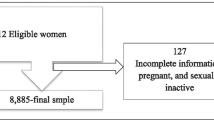
Sampling
The methods used to collect data for the KDHS have been described elsewhere [12]. Briefly, all 47 counties in Kenya were stratified into rural and urban cluster. Using the Fifth National Sample Survey and Evaluation Program (NASSEP V) sampling frame, the KDHS had a 2-stage design. The first stage identified 1612 clusters: 617 urban and 995 rural. In the second stage of sampling, 25 households per cluster were selected using household listings, for a total of 40,300 households. Within these households, 31,079 Kenyan women of reproductive age (15–49 years) were surveyed.
Measurements
Two questionnaires—1 for each household and 1 for a selected woman in each household—were used to collect contraceptive-use data in the KDHS. The household questionnaire was used to record all members of a household and to identify a woman therein to interview. If a household had more than 1 woman of reproductive age, the woman to interview was chosen by consensus among the women in the household. The chosen woman was asked whether she was using any method of contraception. If her response was yes, she was asked to name it, selecting from modern methods [i.e., injectable, implant, oral pill, male condom, and other (e.g., diaphragm, female sterilization, male sterilization, female condom, foam/jelly)] and natural methods (e.g., periodic abstinence, withdrawal (pre-ejaculation), abstinence, lactational amenorrhea).
Independent variables included age, highest education attained, marital status, number of children and number still living, employment status, self-ranking in the wealth index (i.e., poor, middle class, or rich), whether she had ever tested for HIV, and type of residence (i.e., rural or urban).
Data Analysis
STATA version 12 (StataCorp, College Station, Texas, USA) was used for data analysis. Frequency distributions and percentages were calculated to describe the characteristics of the target population. Prevalence of contraceptive use was estimated as the number of women who reported using contraceptives divided by the total number of women interviewed, expressed as a percentage. Cross-tabulations were used to determine the prevalence of contraceptive use by independent variable, each expressed as a percentage. Log-binomial regression models were used for estimating unadjusted and adjusted prevalence ratios and corresponding 95% confidence intervals. Log-binomial models were preferable to logistic regression models because they can give more precise estimates when prevalence is high. Variables associated with contraceptive use in the bivariate analysis (likelihood ratio test [LRT] P < 0.05) were included in the multivariate log-binomial model. Factors were retained in the log-binomial model if their inclusion did not make the model significantly worse at an LRT P value of less than 0.05.
Ethical Considerations
We made a request to MEASURE DHS (Monitoring and Evaluation to Assess and Use Results of Demographic and Health Surveys program) for authorization to use the KDHS 2014 data set. Permission was granted, and a link to access the data set was provided.
Results
There were 31,079 women who participated in the KDHS 2014, and they were split fairly evenly among 3 age categories (37.0% were aged 15–24 years; 33.4% were 25–34 years; and 29.6% were 35–49 years) (Table 1). Most (50.2%) had primary education, and 13.5% had no education. The majority (61.3%) were married. Most of the women (62.6%) resided in rural areas, and most (64.6%) were Protestant Christians. Wealth-index status was split mostly between poor (42.6%) and rich (38.3%), with significantly fewer in the middle-class category (19.1%). A large majority of women (83.1%) had been tested for HIV.
Prevalence of Contraceptive Use
The prevalence of contraceptive use among all women in the study was 38.7%. Use of contraceptives was more common among women aged 25–34 years (51.2%), women who had tertiary education (47.6%), and women who were married (51.6%). Contraceptive use varied by region, from 2.8% in the North Eastern region to 51.3% in the Central region. Muslim women had the lowest rate of contraceptive use (13.1%), compared with women who had other religions. Contraceptive use was more common among those who were working (51.0%) vs not working (23.2%). It decreased as the number of living children increased—with the exception of women who had no children; they had the lowest rate of contraceptive use (7.3%). It was also far more common among women who had tested for HIV (44.9%) than among those who had not (8.6%).
Determinants of Contraceptive Use
Factors independently associated with contraceptive use in a multivariate analysis included education, marital status, region, religion, number of living children, and having tested for HIV. Women who had secondary or tertiary education were more likely to use contraceptives [adjusted prevalence ratio (aPR) = 1.64 and 1.77, respectively], followed by women who had primary education [adjusted prevalence ratio (aPR) = 1.60], compared with women who had no education (Table 1). Widowed and separated women were 0.48 times and 0.62 times, respectively, as likely as single women to use contraceptives, and women in the North Eastern region of Kenya were 0.17 times as likely as their coastal counterparts. Muslim women (0.41, 95% CI 0.37–0.45) and women who had no religion (0.44, 95% CI 0.37–0.54) were less likely to use contraceptives in comparison with Catholics. Having at least 1 child was positively associated with contraceptive use [1–3 children (aPR 2.30), 4–6 children (2.46), 7–9 children (2.42), and 10–12 children (1.18)], compared with having no children. Women who responded yes to ever having tested for HIV were 1.52 times as likely to use contraceptives as women who had not tested.
Types of Contraceptive Methods
Table 2 describes preferred methods among the 12,032 women in the KDHS 2014 who used contraception. Among all of these women, injectable was the most preferred method at 45.8%, followed by implant (16.4%), oral pill (12.0%), other modern method (10.8%), natural method (8.5%), and male condom (6.5%). The most dramatic difference in contraception choice was based on the number of living children a woman had; 53.9% of women who had no living children preferred male condoms, whereas only 4.6% of women who had 1–3 living children (and lower for those who had more) preferred male condoms. There were also differences by HIV testing status: more women who had ever tested for HIV preferred injectables (46.1%) and implants (16.7%), compared with women who had never tested (37.9% and 7.4%, respectively).
Discussion
Contraceptive uptake in our study was 39%, which was lower than the target of 62% set by the Kenya National Population Policy for Sustainable Development in 2000 [11]. Regional disparities in usage were evident in our study, between the North Eastern region and all other regions in Kenya. The North Eastern part of Kenya is populated predominantly by Muslims, who were also the least likely to use contraceptives in this study. This is comparable with an analysis by the National Family Health Surveys in India on barriers to modern contraceptive practices among Asian women, which showed that Muslim women had greater opposition to using contraceptives than women who had other religions [14]. The authors explained that Muslim wives usually have more children than non-Muslim wives, are more likely to desire additional children, and hence are less likely to use contraception.
We found that most study participants (83%) had ever tested for HIV, and we found a positive association between having tested for HIV and using contraception. Wekesa and Coast found that two-thirds of people living with HIV/AIDS in Nairobi wanted to stop having children [5]. This indicates a possibility that women will use multiple technologies to prevent both HIV and pregnancy. A woman who has been tested for HIV and uses contraception may be open to the use of other technologies, such as pre-exposure prophylaxis, for HIV prevention. Additionally, this can be an encouragement for women to participate in HIV clinical vaccine trials in which HIV counseling and testing as well as pregnancy prevention are required.
Our study could not determine reasons for low contraceptive uptake, as this question was not asked in the KDHS. As observed by Kabagenyi et al. lack of men’s involvement in family planning has largely contributed to low uptake of contraceptives [15]. Because men often lead the decision-making process in family matters, their noninvolvement in family planning can affect a woman’s decision regarding use of contraceptives [15]. Having misconceptions about contraception is another reason why women avoid it [16]. Contraceptive use is often thought to be for married women only [16], and some women avoid contraceptives because They fear physical or medical complications [17]. Some people are also concerned about a possible increase in the risk for HIV transmission among women who use injectable depot medroxyprogesterone acetate (DMPA) [18]. These factors may contribute greatly to the low uptake of contraceptives among women of reproductive age in Kenya. Studies that explore deterrents to contraceptive use among Kenyan women could help provide answers.
This study had limitations. It was conducted at 1 time point and relied on participant recall. However, the effect may be minimal given the large sample size. There could have been confounding or effect modification among the different factors, as shown by the prevalence ratios in the bivariate and multivariate analyses. However, we did not hypothesize any primary exposure while estimating changes in the prevalence ratios. Our analysis sought only to explore factors associated with contraceptive use. Finally, the large sample size may have resulted in small differences becoming statistically significant without being clinically meaningful.
Conclusion
This study sought to measure contraceptive use and the factors that influence it among women in Kenya. Low uptake of contraceptives can have negative repercussions on maternal and infant health, including mistimed or unwanted pregnancy, as well as adolescent pregnancy that can lead to unsafe abortion or early marriage. It can also result in population growth, posing serious socioeconomic and developmental challenges. Studies are needed to understand the reasons for low uptake of contraception among Kenyan women in order to develop appropriate education and counseling messages. Such messages may need to be region- and population-specific and integrated into HIV testing and counseling services.
References
World-fertility-patterns-2015.pdf [Internet]. http://www.un.org/en/development/desa/population/publications/pdf/fertility/world-fertility-patterns-2015.pdf. Accessed 9 April 2018.
Sharan M, Ahmed S, May J, Soucat A. Family planning trends in Sub-Saharan Africa: progress, prospects, and lessons learned. Baltimore, Maryland: Johns Hopkins Bloomberg School of Public Health; 2010.
Ssali A, Namukwaya S, Bufumbo L, et al. Pregnancy in HIV clinical trials in sub Saharan Africa: failure of consent or contraception? Sued O, editor. PLoS ONE. 2013;8(9):e73556.
Berhane Y, Berhe H, Abera GB, Berhe H. Utilization of modern contraceptives among HIV positive reproductive age women in Tigray, Ethiopia: a cross sectional study. ISRN AIDS [Internet]. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3800562/. Accessed 25 Sept 2013.
Wekesa E, Coast E. Contraceptive need and use among individuals with HIV/AIDS living in the slums of Nairobi, Kenya. Int J Gynecol Obstet. 2015;130:E31–6.
Joshi B, Velhal G, Chauhan S, et al. Contraceptive use and unintended pregnancies among HIV-infected women in Mumbai. Indian J Commun Med. 2015;40(3):168–73.
Ezugwu EC, Iyoke CA, Nkwo PO, Ezegwui HU, Akabueze JC, Agu PU. Unintended pregnancy among HIV-positive pregnant women in Enugu, southeast Nigeria. Int J Gynaecol Obstet. 2016;132(1):60–3.
Yotebieng M, Norris A, Chalachala JL, Matumona Y, Ramadhani HO, Behets F. Fertility desires, unmet need for family planning, and unwanted pregnancies among HIV-infected women in care in Kinshasa, DR Congo. Pan Afr Med J [Internet]. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4919670/. Accessed 2015
Muma J, Kabiru C, Mukiira C, et al. APHRC-country-step-up-report-Final.pdf [Internet]. http://aphrc.org/wp-content/uploads/2014/05/APHRC-country-step-up-report-Final.pdf. Accessed 29 April 2017.
Sirengo M, Muthoni L, Kellogg TA, et al. Mother-to-child transmission of HIV in Kenya: results from a nationally representative study. J Acquir Immune Defic Syndr. 2014;66(suppl 1):S66–74.
Ochako R, Mbondo M, Aloo S, et al. Barriers to modern contraceptive methods uptake among young women in Kenya: a qualitative study. BMC Public Health [Internet]. 2015;15(1). http://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-015-1483-1. Accessed 22 Feb 2017.
Kenya National Bureau of Statistics, Ministry of Health/Kenya, National AIDS Control Council/Kenya, Kenya Medical Research Institute, National Council for Population and Development/Kenya. Kenya Demographic and Health Survey 2014. 2015. http://dhsprogram.com/publications/publication-fr308-dhs-final-reports.cfm. Accessed 29 April 2017.
Saliku T, Ochako R, Izugbara C. Use of contraceptives among women in Nairobi, Kenya [Internet]. 2011. http://www.abortionresearchconsortium.org/reports/APHRC-policy-brief-26.pdf. Accessed 29 April 2017.
Najafi-Sharjabad F, Syed Yahya SZ, Rahman HA, Hanafiah M, Abdul Manaf R. Barriers of modern contraceptive practices among asian women: a mini literature review. Glob J Health Sci. 2013;5(5):181–92.
Kabagenyi A, Jennings L, Reid A, Nalwadda G, Ntozi J, Atuyambe L. Barriers to male involvement in contraceptive uptake and reproductive health services: a qualitative study of men and women’s perceptions in two rural districts in Uganda. Reprod Health. 2014;11(1):21.
Apanga PA, Adam MA. Factors influencing the uptake of family planning services in the Talensi District, Ghana. Pan Afr Med J [Internet]. 2015;20. http://www.panafrican-med-journal.com/content/article/20/10/full/. Accessed 29 April 2017.
Mosha I, Ruben R, Kakoko D. Family planning decisions, perceptions and gender dynamics among couples in Mwanza, Tanzania: a qualitative study. BMC Public Health. 2013;13(1):523.
Haddad LB, Polis CB, Sheth AN, et al. Contraceptive methods and risk of HIV acquisition or female-to-male transmission. Curr HIV/AIDS Rep. 2014;11(4):447–58.
Acknowledgement
We wish to acknowledge support from the University of California, San Francisco’s International Traineeships in AIDS Prevention Studies (ITAPS), U.S. NIMH, and R25MH064712. International Aids Vaccine Initiative, Kenya Aids Vaccine Initiative-Institute of Clinical Trials, Measure DHS, and Kenya National Bureau of Statistics We wish to acknowledge Debbie Bain Brickley for her invaluable contribution towards this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be interpreted as potential conflict of interest.
Ethical Approval
We made a request to MEASURE DHS (Monitoring and Evaluation to Assess and Use Results of Demographic and Health Surveys program) for authorization to work on the KDHS 2014 data set. This was granted and a link to access the data set was provided.
Informed Consent
Secondary data collected by DHS program was utilized for analysis in this study. Therefore ethical approval and consent for participating was not applicable.
Rights and permissions
About this article
Cite this article
Lunani, L.L., Abaasa, A. & Omosa-Manyonyi, G. Prevalence and Factors Associated with Contraceptive Use Among Kenyan Women Aged 15–49 Years. AIDS Behav 22 (Suppl 1), 125–130 (2018). https://doi.org/10.1007/s10461-018-2203-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-018-2203-5