Abstract
Quantifying HIV service provision along the HIV care continuum is increasingly important for monitoring and evaluating HIV interventions. We examined factors associated with linkage and retention in care longitudinally among MSM (n = 1974, 4933 person-years) diagnosed and living in Guangzhou, China, in 2008–2014. We measured longitudinal change of retention in care (≥2 CD4 tests per year) from linkage and antiretroviral therapy initiation (ART). We examined factors associated with linkage using logistic regression and with retention using generalized estimating equations. The rate of linkage to care was 89% in 2014. ART retention rate dropped from 71% (year 1) to 46% (year 2), suggesting that first-year retention measures likely overestimate retention over longer periods. Lower CD4 levels and older age predicted retention in ART care. These data can inform interventions to improve retention about some subgroups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There is an increasing need for implementation research on how best to achieve viral suppression for prevention and control of HIV transmission. This is detailed in the World Health Organization (WHO) Treat All approach [1]. There are numerous existing studies and interventions focused on improving HIV testing [2, 3], and so we focused on the subsequent stages of the HIV care continuum: linkage to care, retention in pre-antiretroviral therapy care and antiretroviral therapy (ART) care. Achieving high rates across all stages of the care continuum is important because interventions at these later stages may reduce risk behaviors after diagnosis [4], promote viral suppression, and save money [5]. Furthermore, diagnosed patients must be retained in care to receive interventions. In one study from the United States, 61% of HIV transmission was attributable to diagnosed cases lost to follow-up in the later stages of the HIV care continuum [6].
Attrition at each stage of the HIV care continuum is common even with expansion of the treatment initiation criteria [7]. Longitudinally, studies examining the change of retention in ART care among people living HIV (PLHIV) showed a decreasing proportion of retained patients over time [8,9,10]. However, except for a few short-term (one year or less) pre-ART retention studies in Sub-Saharan Africa and South Africa [11, 12], most studies focused on retention during ART care instead of during pre-ART care. Until a Treat All approach can be fully implemented, the pre-ART and ART care stages are equally important in controlling the HIV epidemic. Previous studies about the longitudinal change of retention in care have focused on PLHIV [10,11,12], people who inject drugs or women [8, 9, 13]. With the exception of a few cross-sectional studies [14, 15], men who have sex with men (MSM) have not yet been systematically studied in low and middle income countries.
China, a middle-income country, has experienced a marked increase in HIV prevalence among MSM from 1% in 2003 to 7.7% in 2014 [16]. The Chinese government has made HIV prevention among MSM a national priority [16, 17]. In 2003, the Chinese National Free Antiretroviral Treatment Program was implemented, providing free HIV testing, care, and ART for PLHIV [18]. Treatment initiation criteria were expanded from CD4 ≤ 200/µL to ≤350/µL in 2011, then to ≤500/µL in 2015, and finally to Treat All in 2016 [19]. Using surveillance data, prior studies have calculated the rate of retention in care in Chinese cities [20, 21] and examined factors associated with cross-sectional retention in care [22]. However, only one study has examined the temporal trend of ART attrition for PLHIV [10], and longitudinal studies of retention in care in China among MSM have been limited. In this study, we calculated the rate of linkage to care and the longitudinal change of retention in pre-ART and ART care among MSM diagnosed with HIV, and identified factors associated with retention in care in South China.
Methods
Study Population
This study was conducted in Guangzhou, the capital city of Guangdong Province in southern China. The HIV prevalence among MSM in Guangzhou was high at 11.4% in 2013 [23]. In Guangzhou, the only location that provides free CD4 tests is the Center for Disease Control and Prevention (CDC). Since 2008, interventions addressing HIV testing, linkage and retention in care have been implemented as collaboration projects between Guangzhou CDC and community-based organizations (CBOs) [3]. At the time of data collection, all free ART was provided by one hospital in the city and CD4 results were entered into a centralized database, which was accessed for this study. Eighty-nine percent of diagnosed cases self-reported their transmission route at HIV diagnosis or follow-up in 2008–2014. We defined MSM as route of HIV transmission if a man ever self-reported having sexual intercourse with another man either at diagnosis or updated in follow-ups. We selected for MSM living with HIV who were diagnosed and living in Guangzhou at diagnosis (i.e. local MSM) from January 2008 through September 2014 (simplified to 2014 thereafter). MSM diagnosed in the 3 months prior to the set end point of data collection (31 December 2014) were excluded from analysis due to insufficient follow-up.
Data sources and Descriptions
In China, a confirmed case of HIV is one that has tested positive in both a screening test and a confirmatory Western Blot. All diagnoses of HIV are reported to the national web-based HIV reporting system [24]. In this study, we accessed the case-reporting and follow-up data for all MSM diagnosed with HIV in Guangzhou. The data was collected from 2008 to 2014, when the reporting database was well-managed, more centralized and systematic. The case-reporting dataset was updated annually. Records of cases who migrated out of Guangzhou to other cities or provinces in China were not included in the case-reporting dataset of the respective year. The database included socio-demographic information, HIV diagnostic results, route of transmission, HIV testing site(s), and history of sexually transmitted diseases (STD). In particular, we categorized HIV testing sites into voluntary counseling and testing sites (VCTs) or CBOs, STD clinics, hospitals (for non-STD patients or patients undergoing surgery), and institutions (including entertainment sites, prisons, immigration sites, drug rehabilitation centers, blood transfusion centers and partner service sites). We combined VCT sites and CBOs into one category because there is significant overlap between the two sites. Follow-up datasets recorded date of follow-up, whether or not patients followed up, any history of STDs, and date and result of all CD4 tests. IRB approval was obtained from the Guangzhou CDC, and the Guangdong Provincial Center for Skin Diseases and STI Control, China, and from University of North Carolina at Chapel Hill.
Definition, Data Processing and Statistical Analysis of Linkage to Care
A case was considered linked to care if the individual received a CD4 test within 90 days of diagnosis [25]. We quantified linkage to care in two ways. First, we measured linkage to care of the entire population over time. For each calendar year from 2008 to 2014, the annual rate of linkage to care in the study population was calculated by dividing the number of linked cases by the total number of new diagnoses in each respective year. We also calculated the amount of time that passed between diagnosis and first CD4 test for each newly diagnosed MSM. Bivariable analysis and multivariable logistic regression were performed in SPSS to compare the characteristics between linked and not linked to care cases.
Definition, Data Processing and Statistical Analyses of Retention in Care
Retention in pre-ART care was defined as an individual receiving ≥2 CD4 tests in one year (performed ≥3 months apart) from time of linkage [22], and retention in ART care was defined with the same criteria from time of ART initiation. Viral load testing criteria were not used as it is optional and infrequently used in China during the study period. Time was calculated in years starting from the date of linkage, regardless of time interval from diagnosis, with months 0–11 defined as year one, months 12–23 as year two, months 24–35 as year three, months 36–47 as year four and months 48–59 as year five. Our data endpoints were defined as either date of death (if applicable) or year of last updated record in the case-reporting dataset (migrated outside the city or data end point). Data from the first five years were included in pre-ART retention analyses and the first three years were selected for ART retention analyses. The sample size in later years was too small for analysis and was therefore removed. The rate of retention for each time period was calculated by dividing the number of cases retained in care by the total number of cases alive and with available records. We did not calculate trend of retention rate by calendar year as it was highly affected by the proportion of diagnosed cases in the first year. Socio-demographic factors including marital status, education level, employment status, Guangzhou registered residence and STD history were updated annually in the longitudinal dataset for analyses, and were transcribed from the corresponding time point in case-reporting dataset. The minimum CD4 level from the previous year was used as an independent variable of retention in care.
Data for retention in pre-ART and ART care (≥2 CD4 tests in the year) was a within-subject repeated measurement. As the status changed across time, we used a binary logistic generalizing estimating equation (GEE) in SPSS to analyze this longitudinal pattern [26]. In the GEE model of pre-ART care (“in care” as 1, “not in care” as 0), pre-ART care of the year after linkage was used as an outcome variable. In the GEE model of ART care (“in care” as 1, “not in care” as 0), ART care in the year after ART initiation was used as an outcome variable. In GEE, we defined case as a subject-variable and time as a within-subject variable with an unstructured working correlation matrix. Sequential bonferroni adjustments were made for multiple comparisons.
Results
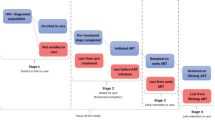
We identified 1974 MSM (4933 person-years follow-up) who were diagnosed with HIV living in Guangzhou between January 2008 and September 2014. The median age at diagnosis was 29 years old [interquartile range (IQR) = 24–35], with median CD4 count at diagnosis of 383/µL (IQR = 277–491.5/µL, n = 1833). (Table 1) At diagnosis, 1147 (79%) MSM were working, 331 (17%) were married, 435 (22%) had a lower education level (below high school), and 564 (29%) had Guangzhou registered residency. Among the 918 MSM with available data on HIV testing experiences, only 149 (16%) had previous HIV testing experience (having tested negative for HIV) before diagnosis. HIV testing sites were mostly CBOs and VCT sites (77%). After diagnosis, 84% of diagnosed MSM were linked within 90 days and 43% of diagnosed MSM were initiated on ART. (Fig. 1).
Linkage to Care
The rate of linkage to care increased from 69% in 2008 to 89% in 2014. (Fig. 2) Cumulatively, from the time of HIV diagnosis, 78% of MSM were linked within one month, and 84% were linked within three months. By the end of study period, 93% of newly diagnosed cases had received their first CD4 test after diagnosis. (Fig. 1).
In evaluating linkage to care, MSM with lower education levels [crude odds ratio (OR) = 0.60, 95% CI 0.46–0.79] and with Guangzhou registered residency (OR 0.44, 95% CI 0.35–0.57) were less likely to be linked to care (received a CD4 test within 90 days) in bivariable analysis (Table 2). After adjusting for residency in the multivariable logistic regression model, those testing for HIV at CBOs or VCT sites (aOR 3.24; 95% CI 2.29–4.59) were more likely to be linked to care than those receiving testing at hospitals (reference group). Education level was not used as a confounder because the change in the adjusted odds ratio was less than 10%.
Retention in pre-ART Care
After initial linkage to care, the rate of retention in pre-ART care (≥2 CD4 tests) dropped sharply from 75% in year one to 43% in year two. The rate then slowly declined to 35% in year five.(Fig. 1) The declining rate of retention in care during pre-ART from year one to year five was also observed in the GEE models.(Model A–B, Table 3) Baseline variables of HIV testing sites and CD4 levels at linkage were significant predictors of retention in pre-ART care. Comparing with MSM testing for HIV in CBOs or VCT sites (reference group), MSM testing in STD clinics were less likely to be retained in pre-ART (aOR 0.64, 95% CI 0.47–0.88 in Model A; aOR 0.63, 95% CI 0.46–0.87 in Model B). Comparing with MSM with CD4 > 500/µL at linkage (reference group), MSM with lower CD4 levels (aOR 1.64 for ≤ 200/µL, 1.29 for 201–350/µL in Model B) were more likely to be retained in pre-ART care. Age at linkage and at CD4 level in the previous year were not predictors of retention in pre-ART care.
Retention in ART Care
Among diagnosed MSM (n = 1974), 840 (43%) were initiated ART. The median interval from linkage to care to ART initiation was 5.38 months (IQR = 1.37–14.95). In year one after linkage, 45% of cases were eligible for ART (CD4 ≤ 350/µL), and 53% of eligible cases were initiated on ART.(Fig. 1) After ART initiation, retention in ART care declined from 71% in year one to 46% in year two. In comparison with year one after treatment initiation (reference group), MSM in year two and three were less likely to be retained in ART care (aOR 0.31 in year two and aOR 0.13 in year three, Model D in Table 3).
Baseline variables of age and CD4 level at linkage, and HIV testing sites were significantly associated with retention in ART care. In comparison with MSM testing for HIV at CBOs or VCT sites, those testing at a STD clinic were less likely to be retained in care (aOR 0.55, 95%CI 0.37–0.81, Model D), while those testing at an institution were more likely to be retained in ART care (aOR 1.76, 95% CI 1.04–2.97). Comparing with MSM with CD4 > 500/µL at linkage, MSM with lower CD4 levels at linkage were more strongly associated with retention in ART care (aOR 3.35 for ≤200/µL, 2.69 for 201–350/µL, 1.79 for 351–500/µL, Model D). Furthermore, MSM with lower previous year’s CD4 levels were more likely to be retained in ART care than those with CD4 > 500/µL (reference group) (aOR 9.46 for ≤200/µL, 5.49 for 201–350/µL, 4.29 for 351–500/µL, Model C). In addition, MSM aged >35 at linkage were more likely (aOR 1.45, 95% CI 1.06–1.99, Model D) to be retained in ART care than those aged ≤25. Other variables such as linkage to care within 90 days from diagnosis, employment status, marital status, education level, Guangzhou registered residence and STD history were not significantly associated with retention in pre-ART and ART care over time in the GEE models.
Discussion
The rate of HIV linkage to care was high and significantly associated with HIV testing sites in Guangzhou, China. The rate of retention in both pre-ART care and ART care was high in the first year but dropped significantly in the second year. This study expands on current literature by examining factors associated with longitudinal change of retention in care among MSM in China. HIV testing sites, CD4 levels and age were all significant predictors of retention in care.
The linkage to care rate among MSM in Guangzhou was high, reaching nearly 90% in 2014. If linkage to care was defined using successful follow-up visits rather than CD4 tests, the rate of linkage approached 100%. This rate is consistent with another study completed in Guangzhou [3], and is higher than studies completed in other cities in China (42–82.5%) [20, 21, 27]. The rates of linkage to care from 2008 to 2014 were also higher than or equal to those from overseas regions such as Philadelphia in the United States (62%) [28], Canada (>90%) [29], Europe (84%) [30], and Sub-Saharan Africa (80.1%) [31] despite our stricter definition criteria.
In our study, those testing for HIV at CBOs or VCT sites for HIV diagnosis were more likely to be associated with linkage to care than those testing at hospitals. The significant predictor of testing site is consistent with a linkage to care study in the United States [32], which found that testing in a hospital was less likely to be associated with linkage to care. Our findings highlight the important role of CBOs and VCT sites for providing HIV services, and their contributions in enhancing HIV testing and the HIV care continuum. This is consistent with the previous study that CBOs’ involvement in the testing stage could enhance the care continuum among MSM in China [33]. Both CBOs and VCTs are likely to enhance linkage to care: CBOs focus on building strong relationships with and understanding the MSM population [34], and VCT sites are staffed with HIV specialists to provide counseling services and free HIV testing. In comparison, patients who were tested routinely prior to surgery may receive HIV testing in hospitals not staffed with HIV specialists or not equipped with counseling services. This underscores the importance of expanding voluntary testing opportunities and providing HIV specialists and counseling services at routine testing sites to optimize linkage to care. The impact of voluntary testing on linkage and retention in care among MSM has been shown in a 2008 collaborative effort between public sector agencies and CBOs in Guangzhou. The collaboration provided integrated HIV services, including pre- and post-test counseling along with psychosocial support through CBOs in the MSM community. This effort resulted in 95% rate of linkage of care, 94% rate of retention in pre-ART care, and 85% rate of ART initiation among participants [3].
Our findings show that retention in care among MSM decreased by >25% between the first and second year after linkage. This decrease in retention in pre-ART care over time was similar to findings from a multi-city study in Sub-Saharan Africa and a study in South Africa, both of which described an increasing proportion of attrition from pre-ART care from month 3 to month 12 [11, 12]. The decline of ART retention in our study is consistent with findings from another national Chinese study using data from 2003 to 2010, though this group defined retention in care as ≥1 CD4 test [10]. Demographically, MSM aged >35 were more likely to be retained in ART care than those aged ≤25, which is consistent with other studies [10, 35]. This implies that more efforts should be directed at retaining this younger population group in care [36].
The measured CD4 level was a significant predictor of retention in pre-ART and ART care. At linkage, MSM with lower CD4 levels were more likely to be retained in pre-ART and ART care than those with CD4 levels >500/µL (reference group). This is consistent with findings from previous studies [7, 10, 22]. On the other hand, CD4 levels from the previous year was a predictor of retention in ART care. If retention in care was defined as at least 1 CD4 test within the year, an additional 32% of cases with a high CD4 level (>500/µL) in the previous year could be regarded as retained in ART care in year two. This finding may be more indicative of inadequate care of MSM with high CD4 levels than of loss to follow-up. Another explanation is that MSM with high CD4 levels may feel reassured of their good health and may not be as persistent in seeking care. This illustrates how defining retention in care as ≥ 2 CD4 tests per year excludes MSM with relatively high CD4 levels who only undergo CD4 testing once a year. We have performed sensitivity analyses using ≥1 CD4 tests as an outcome variable in GEE. However, there was no significant change in factors associated with pre-ART and ART care in GEE. Of note, previous studies have shown that younger patients have more satisfactory CD4 recovery after ART initiation than older adults [37, 38]. These all suggest that interventions for enhancing retention in ART care among younger patients and those with higher CD4 levels are needed.
The implementation of Treat All as suggested by the WHO [19] will help to improve care as all cases would be eligible for treatment, despite CD4 levels [29]. In China, a previous study has demonstrated the satisfactory benefit (62% reduction of mortality) of simplified HIV test and immediate treatment [39]. In 2016, Treat All was recommended by the Chinese government [19]. If all patients were initiated on treatment within one year, this would prevent the steep drop in pre-ART care retention from year one to year two. The treatment is a lifelong therapy. Interventions will be necessary to mitigate the steep drop in retention in ART care beyond the first year as observed in this study. Promoting awareness of maintaining good ART care retention despite high CD4 levels will be essential both clinically and epidemiologically. Furthermore, patients achieving stable clinical conditions (e.g. satisfactory CD4 recovery and full viral load suppression) require less frequent follow-up visits. Thus, the definition of retention in care should reflect this in future. Selection and implementation of an ART delivery model, such as a one-stop patient-centered care model and decentralization of ART delivery through the CDC using less well-trained staff, would depend on local epidemiology. The Chinese government has also recommended “one-stop” model in high HIV burden areas [40]. Previous studies have shown that a “one-stop” model might achieve better retention in care, CD4 recovery and viral load suppression [41]. A CDC-based drug delivery model was found to have lower rate of retention in care despite the extensive network [42].
This study has two main limitations. First, our dataset did not clearly document when individuals migrated in and out of the city. We were therefore only able to include cases that were diagnosed and living in the city at time of diagnosis to minimize the influence of migrants. If, among these eligible cases, an individual received an occasional CD4 test outside Guangzhou with no record of migration from the city, they were still included in analyses. Our estimate of the ART retention rate was lower than a Guangdong study (84–94%), which used a crude point estimation of cases remained in ART divided by cases initiated ART in the study period [42]. Thus, the rates of retention in care in our study may be underestimated by excluding possible visits and tests outside the city. However, the estimation reflects the local HIV care continuum. Second, MSM were designated using data entered by doctor as provided by diagnosed patients. Given the stigma against MSM in China, there may have been a social desirability bias in reporting the route of transmission, and some MSM may fail to disclose any previous history of sex with other men. Thus, the retention in care of this group of hidden MSM is unknown, and future research about identifying and analyzing their behaviors is needed.
Conclusions
High rates of linkage to care and retention in the first year of pre-ART and ART care indicate a good start of the HIV care continuum. However, interventions to maintain retention in ART care beyond the second year are urgently needed, especially after the recommendation of Treat All in China in 2016 [19]. To enhance retention in ART care, interventions targeting younger patients and those with higher CD4 levels should be considered. In addition, further research is needed to analyze the feasibility and effectiveness of different ART delivery models (i.e. one-stop patient-centered care and decentralized drug delivery without HIV specialists) to maintain high ART retention rates. We believe that our study methods and results are applicable to other locations with MSM HIV epidemic conditions and HIV service provision systems similar to those in China.
References
Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793–800.
Tang W, Han L, Best J, et al. Crowdsourcing HIV test promotion videos: a noninferiority randomized controlled trial in China. Clin Infect Dis. 2016;62(11):1436–42.
Cheng W, Cai Y, Tang W, et al. Providing HIV-related services in China for men who have sex with men. Bull World Health Organ. 2016;94(3):222–7.
Marks G, Crepaz N, Senterfitt JW, Janssen RS. Meta-analysis of high-risk sexual behavior in persons aware and unaware they are infected with HIV in the United States: implications for HIV prevention programs. J Acquir Immune Def Synd. 2005;39:446–53.
Maulsby C, Jain KM, Weir BW, et al. The cost and threshold analysis of retention in care (RiC): a Multi-Site National HIV Care Program. AIDS Behav. 2017;21(3):643–9.
Skarbinski J, Rosenberg E, Paz-Bailey G, et al. Human immunodeficiency virus transmission at each step of the care continuum in the United States. JAMA Intern Med. 2015;175(4):588–96.
Koenig SP, Bernard D, Devieux JG, et al. Trends in CD4 count testing, retention in pre-ART care, and ART initiation rates over the first decade of expansion of HIV services in Haiti. PLoS ONE. 2016;11(2):e0146903.
Cornell M, Grimsrud A, Fairall L, et al. Temporal changes in programme outcomes among adult patients initiating antiretroviral therapy across South Africa, 2002–2007. AIDS. 2010;24(14):2263–70.
Westergaard RP, Hess T, Astemborski J, Mehta SH, Kirk GD. Longitudinal changes in engagement in care and viral suppression for HIV-infected injection drug users. AIDS. 2013;27(16):2559–66.
Zhu H, Napravnik S, Eron J, et al. Attrition among human immunodeficiency virus (HIV)- infected patients initiating antiretroviral therapy in China, 2003–2010. PLoS ONE. 2012;7(6):e39414.
McNairy ML, Lamb MR, Abrams EJ, et al. Use of a Comprehensive HIV care cascade for evaluating HIV Program Performance: findings from 4 Sub-Saharan African countries. J Acquir Immune Defic Syndr. 2015;70(2):e44–51.
Clouse K, Pettifor AE, Maskew M, et al. Patient retention from HIV diagnosis through one year on antiretroviral therapy at a primary health care clinic in Johannesburg, South Africa. J Acquir Immune Defic Syndr. 2013;62(2):e39–46.
Haas AD, Tenthani L, Msukwa MT, et al. Retention in care during the first 3 years of antiretroviral therapy for women in Malawi’s option B+ programme: an observational cohort study. Lancet HIV. 2016;3(4):e175–82.
McFall AM, Mehta SH, Srikrishnan AK, et al. Getting to 90: linkage to HIV care among men who have sex with men and people who inject drugs in India. AIDS Care. 2016;28(10):1230–9.
Parchure R, Kulkarni V, Kulkarni S, Gangakhedkar R. Pattern of linkage and retention in HIV care continuum among patients attending referral HIV care clinic in private sector in India. AIDS Care. 2015;27(6):716–22.
National Health and Family Planning Commission of the People’s Republic of China. 2015 China AIDS Response Progress Report. Beijing, China May 2015 2015.
Wu Z, Sullivan SG, Wang Y, Rotheram-Borus MJ, Detels R. Evolution of China’s response to HIV/AIDS. Lancet. 2007;369(9562):679–90.
Zhang F, Dou Z, Ma Y, et al. Five-year outcomes of the China National Free Antiretroviral Treatment Program. Ann Intern Med. 2009;151(4):241–51.
National Center for AIDS/STD Control and Prevention China CDC (2016) [National Health and Family Planning Commission of the People’s Republic of China: antiretroviral therapy provision is not mandatory]. http://www.chinaaids.cn/zlgh/hdjz6/201606/t20160622_131594.htm.
Zhang D, Li C, Meng S, Qi J, Fu X, Sun J. Attrition of MSM with HIV/AIDS along the continuum of care from screening to CD4 testing in China. AIDS Care. 2014;26(9):1118–21.
Chow EP, Muessig KE, Yuan L, et al. Risk behaviours among female sex workers in China: a systematic review and data synthesis. PLoS ONE. 2015;10(3):e0120595.
Yang GL, Yan J, Liu Y, Huang ZL, Long S. Retention in care and factors affecting it among people living with HIV/AIDS in Changsha City, China. Asia Pac J Public Health. 2015;27(2 Suppl):86s–92s.
Zhong F, Liang B, Xu H, et al. Increasing HIV and decreasing syphilis prevalence in a context of persistently high unprotected anal intercourse, six consecutive annual surveys among men who have sex with men in Guangzhou, China, 2008–2013. PLoS ONE. 2014;9(7):e103136.
Zhang L, Chow EP, Zhang J, Jing J, Wilson DP. Describing the Chinese HIV surveillance system and the influences of political structures and social stigma. Open AIDS J. 2012;6:163–8.
Christopoulos KA, Das M, Colfax GN. Linkage and retention in HIV care among men who have sex with men in the United States. Clin Infect Dis. 2011;52(Suppl 2):S214–22.
Hanley JA, Negassa A, Edwardes MD, Forrester JE. Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol. 2003;157(4):364–75.
Yan H, Zhang R, Wei C, et al. A peer-led, community-based rapid HIV testing intervention among untested men who have sex with men in China: an operational model for expansion of HIV testing and linkage to care. Sex Transm Infect. 2014;90(5):388–93.
Eberhart MG, Yehia BR, Hillier A, et al. Behind the cascade: analyzing spatial patterns along the HIV care continuum. J Acquir Immune Defic Syndr. 2013;64(Suppl 1):S42–51.
Nosyk B, Montaner JS, Colley G, et al. The cascade of HIV care in British Columbia, Canada, 1996–2011: a population-based retrospective cohort study. Lancet Infect Dis. 2014;14(1):40–9.
Belza MJ, Hoyos J, Fernandez-Balbuena S, et al. Assessment of an outreach street-based HIV rapid testing programme as a strategy to promote early diagnosis: a comparison with two surveillance systems in Spain, 2008–2011. Euro Surveill. 2015;20(14):23–33.
Suthar AB, Ford N, Bachanas PJ, et al. Towards universal voluntary HIV testing and counselling: a systematic review and meta-analysis of community-based approaches. PLoS Med. 2013;10(8):e1001496.
Robertson M, Wei SC, Beer L, et al. Delayed entry into HIV medical care in a nationally representative sample of HIV-infected adults receiving medical care in the USA. AIDS Care. 2016;28(3):325–33.
Zhang D, Lu H, Zhuang M, et al. Enhancing HIV testing and treatment among men who have sex with men in China: a pilot model with two-rapid tests, single blood draw session, and intensified case management in six cities in 2013. PLoS ONE. 2016;11(12):e0166812.
Tucker JD, Muessig KE, Cui R, et al. Organizational characteristics of HIV/syphilis testing services for men who have sex with men in South China: a social entrepreneurship analysis and implications for creating sustainable service models. BMC Infect Dis. 2014;14:601.
Vinikoor MJ, Joseph J, Mwale J, et al. Age at antiretroviral therapy initiation predicts immune recovery, death, and loss to follow-up among HIV-infected adults in urban Zambia. AIDS Res Hum Retroviruses. 2014;30(10):949–55.
Lall P, Lim SH, Khairuddin N, Kamarulzaman A. Review: an urgent need for research on factors impacting adherence to and retention in care among HIV-positive youth and adolescents from key populations. J Int AIDS Soc. 2015;18(2 Suppl 1):19393.
Wong NS, Reidpath DD, Wong KH, Lee SS. A multilevel approach to assessing temporal change of CD4 recovery following HAART initiation in a cohort of Chinese HIV positive patients. J Infect. 2015;70(6):676–8.
Naftalin CM, Wong NS, Chan DP, Wong KH, Reidpath DD, Lee SS. Three different patterns of CD4 recovery in a cohort of Chinese HIV patients following antiretroviral therapy—a five-year observational study. Int J STD AIDS. 2015;2015(26):803–9.
Wu Z, Zhao Y, Ge X, et al. Simplified HIV testing and treatment in China: analysis of mortality rates before and after a structural intervention. PLoS Med. 2015;12(9):e1001874.
State Council Office. [China’s 13th Five-year Action Plan for Reducing and Preventing the Spread of HIV/AIDS (2016–2020)]. Beijing. 2017.
Zhou W, Zhao M, Wang X, et al. Treatment adherence and health outcomes in MSM with HIV/AIDS: patients enrolled in “one-stop” and standard care clinics in Wuhan China. PLoS ONE. 2014;9(12):e113736.
Ning C, Smith KM, McCann CD, et al. Outcome of sentinel hospital-based and CDC-based ART service delivery: a prospective open cohort of people living with HIV in China. Sci Rep. 2017;7:42637.
Acknowledgements
The authors thank all staff of Guangzhou Center for Disease Control and Prevention for their assistance in the maintenance of the database used in this study. Li Ka Shing Institute of Health Sciences and Stanley Ho Centre for Emerging Infectious Diseases of The Chinese University of Hong Kong are acknowledged for providing technical support in conducting the research.
Funding
The authors disclosed receipt of the following financial support for the research, authorship and/or publication of this article: This research was funded by The Project for Key Medicine Discipline Construction of Guangzhou Municipality (Grant Number 2017-2019-07), Bill & Melinda Gates Foundation to the MeSH Consortium (BMGF-OPP1120138), NIH Fogarty International Center Grant, the South China-UNC STD Research Training Center Grant (FIC1D43TW009532-01), SESH R01 Grant (NIAID 1R01AI114310), and Doris Duke International Clinical Research Grant.
Disclaimer
The opinions and assertions contained herein are private views of the authors and do not necessarily reflect their affiliating institutions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
IRB approval was obtained from the Guangzhou CDC, and the Guangdong Provincial Center for Skin Diseases and STI Control, China, and from University of North Carolina at Chapel Hill.
Rights and permissions
About this article
Cite this article
Wong, N.S., Mao, J., Cheng, W. et al. HIV Linkage to Care and Retention in Care Rate Among MSM in Guangzhou, China. AIDS Behav 22, 701–710 (2018). https://doi.org/10.1007/s10461-017-1893-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-017-1893-4