Abstract
This study investigated the acceptability of daily use of free oral pre-exposure prophylaxis (PrEP) and associated factors among transgender women sex workers in Shenyang, China, following a briefing on PrEP. A total of 183 HIV negative or sero-status unknown participants completed the cross-sectional survey. The prevalence of acceptability of daily use of free oral PrEP was 61.2%. Adjusting for education level and monthly income, variables on negative attitudes toward PrEP (i.e., having concerns about the side-effects of PrEP) [Adjusted odds ratios (AOR): 0.26], perceived subjective norms (i.e., perceiving support from male partners to take PrEP) (AOR: 2.08), and perceived behavioral control (e.g., perceiving complete control over using PrEP) (AOR: 2.10–16.72) were significantly associated with acceptability of daily use of free oral PrEP. In addition, experiencing violence during sex work, perceived risk of contracting HIV from clients and probable anxiety were also significant. Future PrEP promotion campaigns should consider these factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Transgender women are assigned males at birth but identify or express themselves as women with or without undergoing feminizing medical interventions [1,2,3]. They are often socially, economically, politically and legally marginalized [3], leading to unemployment or underemployment. As a result, many of them are forced to take up sex work [3, 4]. It is reported that 54–80% of Asian transgender women have engaged in sex work [3]. Transgender women sex workers form a key population that requires focused attention for HIV prevention. As estimated by a meta-analysis, the overall HIV prevalence among transgender women sex workers was 27.2%, which was much higher than that of male (15.1%) and female (4.3%) sex workers [5]. The HIV prevalence was 25.9% among transgender women sex workers in China [6]. Previous studies also reported high prevalence of CRAI with male clients among transgender women sex workers, ranging from 25% in South Africa [7] to 92% in Pakistan [8]. In China, 26.8% of the transgender women sex workers reported CRAI with male clients in the last month [6]. Despite the severe HIV epidemic among transgender women sex workers, there is a dearth of interventions targeting them. To our knowledge, there are only a few behavioral interventions targeting transgender women or transgender women sex workers. Furthermore, these studies gave mixed results in reducing HIV/STD prevalence and/or sexual risk behaviors [9,10,11,12,13,14].
In the past few years, the growing amount of evidence for the effectiveness of bio-medical HIV interventions has changed HIV prevention strategies substantially [15]. PrEP, which refers to the initiation of TDF/FTC before and during periods of HIV exposure among HIV negative individuals, could effectively reduce the risk of HIV acquisition among MSM [15], transgender women [16], heterosexual women [17], sero-discordant heterosexual couples [18], and injective drug users [19]. A mathematical model suggested that prioritizing PrEP to transgender women or transgender women sex workers would be more likely to achieve the maximum effectiveness of reducing HIV incidence at a population level as compared to a uniform coverage of PrEP in every at-risk population [20]. The 2014 WHO Consolidated Guideline on HIV Prevention, Treatment and Care further recommends PrEP as a possible additional intervention for transgender women [21].
To our knowledge, eight quantitative studies investigating acceptability of PrEP for HIV prevention have included transgender women [22,23,24,25,26,27,28,29], four of them were specifically targeting transgender women [22,23,24,25]. The prevalence of acceptability of daily use of free oral PrEP was 30.2% in the U.S. study [25], 59.3% in the Vietnam study [24] and 89.3% in the Brazilian study [23]. The prevalence of acceptability was 37.0% among participants of the Thailand study, which did not mention the price of PrEP [22]. Furthermore, only the Thailand study reported factors associated with acceptability of PrEP, which included socio-demographic characteristics (i.e., having private insurance), risk behaviors and awareness of PrEP [22]. However, it did not consider potential important factors such as sex work related variables (e.g., CRAI with clients), mental health status or cognitive variables (e.g., perceived efficacy in HIV prevention, concerns of side effects). Also, there are three ongoing PrEP implementation projects that are providing PrEP to transgender women, all conducted in the U.S. [30.].
As compared to MSW and FSW, transgender women sex workers are more likely to experience violence from both police and clients due to their transgender identity [31,32,33]. They are at the bottom of the hierarchy of sex workers, as they charge lower than other sex workers but have much higher risk of unprotected sex during sex work [33]. Previous studies showed that sex work related variables (e.g., unprotected sex with clients) were associated with acceptability of PrEP among FSW [34]. The association between mental health status and acceptability of PrEP has not been investigated. Mental health problems (e.g., depression and anxiety) are prevalent among transgender women sex workers [31]. Poor mental health status was found to be a barrier for service utilization and adoption of preventive behaviors among transgender women [35, 36]. Cognitive variables (e.g., perceived efficacy in HIV prevention, concerns of side effects and stigma) were found to be associated with acceptability of PrEP among MSM [26, 37]. These variables are potentially associated with acceptability of daily use of PrEP among transgender women sex workers and were investigated in this study.
Uniqueness of This Study
This is the first study investigating acceptability of PrEP among transgender women sex workers.
Objectives
In a sample of HIV negative/unknown sero-status transgender women sex workers in Shenyang, China, we investigated the prevalence of acceptability of daily use of free oral PrEP. In addition to background variables, potential factors of acceptability of free oral daily PrEP included: (1) cognitive variables related to PrEP based on TPB (positive attitude, negative attitude, subjective norm and perceived behavioral control), (2) sex work related variables (i.e., experienced violence during sex work, CRAI and perceived risk of contracting HIV from male clients) and (3) mental health status (probable depression and probable anxiety).
Method
Study Design and Data Collection
Our study was conducted in Shenyang, China in 2014. Shenyang is the capital city of Liaoning Province in Northeastern China, which had a population size of 8.3 million in 2014. The participants self-identified as transgender women, were aged ≥18 years old, had had anal intercourse with ≥1 male client (last 3 months), and wore feminine attire during sex work. Staff of an NGO who provided services to transgender women sex workers contacted their clients and performed outreach for recruitment. Referrals were also made by some participants. Prospective participants were assured that refusing to participate in the study would not affect their right to use any services and that they could quit at any time without being questioned. Upon written informed consent, anonymous face-to-face interviews were conducted by staff of the aforementioned NGO in settings with privacy ensured. Monetary compensation (50 RMB or 8.1 USD) was given to participants upon completion of the interview. We interviewed 220 transgender women sex workers, 16.8% (n = 37) self-reported being HIV positive (data of the overall sample was presented in a published study) [6]. This study was based on a sub-sample (n = 183) of those who self-reported being HIV negative or unknown HIV sero-status. After completion of the survey, these 183 participants were invited to take a finger-prick HIV rapid test (Alere Determine™ HIV-1/2 rapid HIV screening test, Alere Inc, Waltham (MA), United States); 90 (49.2%) of them agreed and 20 (10.9%) were screened HIV positive [6]. Ethics approval was obtained from the Institutional Survey and Behavioral Research Ethics Committee.
Measures
Participants’ Profiles
Information collected included socio-demographics (age, educational level, monthly personal income, whether they are permanent registered residents of Shenyang, and duration of stay in Shenyang), utilization of any HIV prevention services in the last six months, any anal sex with non-commercial male RP or NRP in the last month, and whether they have undergone feminizing medical interventions (i.e., cosmetic surgery, hormone treatment, and reassignment surgeries). RP is defined as men who are in a stable relationship that do not involve transactional sex, while NRP is defined as men who are not RP and do not involve transactional sex.
Acceptability of Daily Use of Free Oral PrEP
Participants were briefed with the following: “PrEP is a strategy using antiretroviral drugs to prevent HIV infection among HIV negative individuals. PrEP has been approved by the U.S. FDA, and recommended by the WHO as a possible additional strategy for HIV prevention among transgender women. However, such service is not yet available in China. Daily use of oral PrEP can potentially reduce the risk of HIV infection by 70%. However, failure to take it every day will reduce its effectiveness. PrEP has possible side effects such as nausea, vomiting and headache”. The efficacy (i.e., 70%) was based on the randomized controlled trail published by Grant et al., which reported that using PrEP on ≥90% of the days during the follow up period reduced the risk of HIV acquisition by 73% [15]. They were then asked whether they were willing to take a free once-daily oral pill as PrEP in the next six months (response categories: 1 = definitely not, 2 = not much chance, 3 = neutral, 4 = some chance, 5 = definitely will). We dichotomized the responses and defined acceptability as “definitely will” in order to provide a more conservative estimation of such indicator, as only 43–62% of those with a behavioral intention would translate it into related action according to a meta-analysis [38]. We expected relatively high proportion of participants indicating “some chance” would not take action. The outcome we chose might be more indicative of actual behavior. Such a definition has been used in some published studies investigating acceptability of PrEP [22, 39,40,41].
Perceptions Related to PrEP Based on TPB
A meta-analysis showed that theory-based interventions are more effective than non-theory-based ones [42]. The TPB [43] was used to explain acceptability of PrEP in this study. It postulates that, in order to form an intention to adopt a health-related behavior (e.g., use PrEP), one would first evaluate the behavior (positive and negative attitudes), consider whether their significant others would support such behavior (subjective norm) and appraise how much control they have over the behavior (perceived behavioral control) [44,45,46]. Items were used to measure positive attitudes toward PrEP (i.e., “PrEP can effectively reduce your risk of HIV infection”), negative attitudes toward PrEP (e.g., “The side effects of PrEP can affect your daily life”), perceived subjective norm related to PrEP (e.g., “Your male sex partner will support you take PrEP”) and perceived behavioral control of using PrEP (e.g., “You are confident to use free PrEP if you want to”) (Response categories: 1 = disagree, 2 = neutral, 3 = agree).
Sex Work Related Variables
Participants were asked about any CRAI with male clients in the last month and whether they had experienced any violence during sex work in the last month. They were also asked to perceive their level of risk of contracting HIV from their male clients (1 = not at all, 4 = very high).
Mental Health Status
Probable depression and probable anxiety were measured by the validated Chinese version of the CES-D-20 Scale [47, 48] and GAD-7 Scale [49], respectively. The Cronbach’s alpha values of these two scales were 0.90 and 0.91, respectively. Single factors were identified for these two scales by using EFA, and explained 60.1% and 65.1% of the total variance.
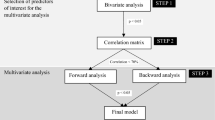
Statistical Analysis
Using acceptability of daily use of free oral PrEP as the dependent variable, OR for the associations between background independent variables and the dependent variable were estimated. Those background variables with P < 0.10 in the univariate analysis were adjusted for in subsequent multiple logistic regression analysis involving other independent variables (i.e., perceptions related to PrEP based on TPB, sex work related variables and mental health status), AOR and respective 95% CI were derived from such analyses. All variables that had P < 0.10 in the univariate analysis were considered as candidates of a forward stepwise logistic regression model, which had an entry criterion of P < 0.10 and an exclusion criterion if P > 0.20, and was used to derive ORm. SPSS version 16.0 was used for data analysis, with P values <0.05 taken as statistically significant.
Results
Background Characteristics
Majority of the participants were 18–30 years old (53.5%), were not permanently registered residents of Shenyang (87.4%), had resided in Shenyang for no more than five years (55.7%) and had had a monthly personal income of 5000 RMB (806.5 USD) or less (56.3%). Only 12% had attended college or university. The majority (91.7%) had utilized HIV prevention services in the last six months, and about two-thirds had had anal intercourse with RP (63.4%) or NRP (66.7%) in the last month. Only 17.5% had undergone at least one of the following feminizing medical interventions: cosmetic surgery (15.3%), hormone treatment (2.7%) and sex reassignment surgery (0.5%) (Table 1).
Acceptability of Daily Use of Free Oral PrEP
After a briefing on the facts of PrEP, the prevalence of acceptability of daily use of free oral PrEP in the next six months was 61.2% (Table 2).
Perceptions Related to PrEP
The majority perceived that PrEP could effectively reduce their risk of HIV infection (58.5%). Less than half showed some negative attitudes toward PrEP, i.e., side effects of PrEP would affect my daily life (28.4%), or their male sex partner would consider the use of PrEP as a symbol of distrust (35.5%). Regarding perceived subjective norm, 38.8 and 44.8% perceived their peers and male partners would support their use of PrEP, respectively. The level of perceived behavioral control was high, as 73.2–84.7% agreed with the three related statements (Table 2).
Sex Work Related Variables and Mental Health Status
In the last month, 25.7% reported CRAI with male clients, and 14.2% had experienced violence during sex work. The mean score of perceived risk of contracting HIV from male clients was 2.5 (SD: 1.0, range 1–4). The mean score of the CES-D-20 Scale and the GAD-7 Scale was 16.9 (SD: 11.2) and 4.3 (SD: 4.4), respectively (Table 2).
Factors Associated with Acceptability of Daily Use of Free Oral PrEP
In the univariate analysis, only two background variables (education level and monthly personal income) were significantly associated with acceptability (ORs are shown in Table 3). Adjusted for these two background variables, five TPB-related variables were significantly associated with acceptability and the associations were in the expected directions, including: (1) one item on negative attitude toward PrEP [the side effects of PrEP can affect your daily life (AOR: 0.26, 95%CI: 0.13, 0.54)], (2) one item on perceived subjective norm related to PrEP [your male sex partner will support you take PrEP (AOR: 2.08, 95%CI: 1.06, 4.06)], and (3) agreement with the three items on perceived behavioral control for using PrEP [you are confident to take PrEP if you want to (AOR: 4.89, 95%CI: 2.26, 10.56), whether to take PrEP or not is completely under your control (AOR: 2.10, 95%CI: 1.01, 4.82), and you can take PrEP everyday if you want to (AOR: 16.72, 95%CI: 4.94, 56.53)]. In addition, having experienced violence during sex work (AOR: 3.71, 95%CI: 1.41, 9.78) and perceived risk of contracting HIV from clients (AOR: 1.79, 95%CI: 1.29, 2.50) were positively associated with acceptability, while probable anxiety (score of GAD-7 scale) was negatively associated with this dependent variable (AOR: 0.94, 95%CI: 0.87, 0.98) (Table 4).
All but one of these eight independent variables (except the one on perceived subjective norm) were selected by the forward stepwise logistic regression model (Table 4). Hence, the associations between these seven variables and acceptability of daily use of free oral PrEP were independent from each other.
Discussion
Our sampled transgender women sex workers were at high risk of HIV infection as the prevalence of CRAI with male clients was considerably high. PrEP, which was newly recommended to this population by the 2014 WHO Consolidated Guideline on HIV Prevention, Diagnosis, Treatment and Care [21], is potentially important in reducing their risk of HIV infection. To our knowledge, this is the first study investigating acceptability of PrEP and associated factors in this population.
About two-thirds of the participants showed acceptability of daily use of free PrEP. The prevalence was comparable to those studies targeting transgender women in Vietnam (59.3%) [24] and FSW or MSM in China (54.3 and 67.8%) [34, 37] that also investigated acceptability of daily use of free PrEP. The observed high acceptability demonstrated high demand for PrEP in the community. Currently, there are eleven PrEP implementation projects being planned or underway in ten countries (e.g., Thailand, U.S., and U.K.) [30]. However, the inclusion of transgender women or transgender women sex workers in these programs was minimal; none of these programs specifically targeted transgender women or transgender women sex workers [30]. As compared to MSM in China, transgender women sex workers are less accessible and smaller in population size, and there is a dearth of NGOs serving this group. As a result, they might be neglected by the existing HIV prevention programs. Given this context, PrEP may create a significant impact in reducing HIV incidence in this population [50].
We advocate for PrEP-related services to be given to this group. Even with such services made available, we still need to promote PrEP use as self-reported acceptability would only be partially translated into real action. We need to understand factors associated with acceptability in order to design future PrEP promotion programs. Similar to a previous study among FSW in China [34], higher education level was associated with higher acceptability of PrEP. However, unlike studies of MSM that reported 40.7–69.6% in Chinese cities had attained university education, the proportion of transgender women sex workers who had attained the same education level was very low. The lower education level may create challenges for PrEP promotion among transgender women sex workers. We found that those with higher monthly income were more responsive to PrEP. Since majority of the transgender women sex workers in China had low income level, free PrEP-related services should be considered to increase the public health impact.
Cognitive variables related to PrEP based on the TPB were significantly associated with acceptability of PrEP. Contents of future PrEP promotion program may make references to such findings. First, about 30% of the participants had some concerns related to the side effects of PrEP, which was significantly and negatively associated with acceptability of PrEP. Health communication messages should emphasis that PrEP is safe (e.g., severe side effects are rare) and that the common mild side effects (e.g., nausea, vomiting and headache) can be easily managed [50] in order to remove such concerns. Transgender friendly services should be made available to support PrEP users who have side effects. Second, many of our participants had non-commercial male sex partners and about half of them perceived such partners would support their use of PrEP, which was associated with higher likelihood of acceptability. It is hence important to encourage transgender women sex workers to discuss PrEP with their non-commercial male sex partners, so as to reduce potential misunderstandings about the lack of support and to obtain support regarding PrEP use. Third, participants had a high level of perceived behavioral control to use PrEP, which was positively associated with acceptability of PrEP. It is important to further strengthen their perceived behavioral control related to PrEP. Multiple strategies may be applied in future PrEP promotion programs, which may include simplification of the procedures to obtain PrEP and provision of transgender friendly PrEP-related services to support adherence of PrEP.
Despite participants’ high risk profiles, their level of perceived risk of contracting HIV was moderate. In our study, perceived risk of contracting HIV from male clients was strongly and independently associated with acceptability of PrEP. It is important for future PrEP promotion programs to increase perception of HIV infection risk among transgender women sex workers, and to identify high risk individuals to discuss PrEP use. About 1/7 (15%) of the participants experienced violence during sex work in the last month, which was comparable to street-based FSW in China [51]. Such experience was also independently associated with higher acceptability of PrEP in this study. Condom use might be a potential cause of dispute and violence among them, and PrEP might be seen by transgender women sex workers as a means of preventing occurrence of client-initiated violence. It can offer more protection if they are unable to use condoms during violence. However, it is also possible that some of them will give up condom negotiation after using PrEP, which raises the concern of risk compensation [52, 53], which is defined as the phenomenon that one would increase risk behaviors due to the lowered risk perception after using PrEP. Future PrEP promotion in this population should include skill training to negotiate condom use with clients, while emphasizing that CRAI will reduce or even diminish the protective effect offered by PrEP [20].
No study has investigated the impact of mental health problems on acceptability of PrEP. Probable anxiety was significantly and negatively associated with acceptability of PrEP among our participants. Previous studies showed that poor mental health would undermine individual’s intention to take up protective measures (e.g., condom use) [54] and result in poor support-seeking [55]. Our findings suggested that future PrEP related services should include mental health support reducing probable anxiety.
Strengths and Limitations
This is the first study investigating acceptability of PrEP and associated factors among transgender women sex workers. A wide range of factors were considered by this study, including sex work related variables, mental health status and cognitive variables based on a behavioral health theory. However, it also has some limitations. First, like previous studies, identity as a transgender woman was self-defined [1, 56,57,58,59,60]; there is no standard instrument assessing gender identity. Second, similar to other studies surveying transgender women sex workers, participants were recruited mainly through outreach and referrals [6, 58,59,60]. There was no sampling frame, and random sampling was not feasible. The results may not be representative of transgender women sex workers in China, and caution should be taken when generalizing the results to this population in China. Third, we did not ask prior awareness SO4 2− and utilization of PrEP. Although we have explained benefits and harms before asking about acceptability to ensure that uniform information has been received by all participants, first time knowledge of PrEP may lower the reliability of acceptability. Moreover, the question items were constructed for this study as no validated scale was available. Lastly, this was a cross-sectional study that could not establish causality.
Conclusion
Transgender women sex workers in China are at high risk of HIV infection as the prevalence of CRAI with male clients was considerably high. PrEP may be one of the most promising strategies to reduce their HIV incidence. The observed high acceptability demonstrated high demand for PrEP in the community. We advocate for free PrEP-related services to be given to this group. Future PrEP promotion campaigns should not only modify cognitions related to PrEP, but also provide transgender friendly service to manage side effects, support adherence and promote mental health.
Abbreviations
- AOR:
-
Adjusted odds ratios
- CI:
-
Confidence interval
- CRAI:
-
Condomless receptive anal intercourse
- EFA:
-
Exploratory factor analysis
- FSW:
-
Female sex workers
- FTC:
-
Emtricitabine
- HIV:
-
Human immunodeficiency virus
- MSM:
-
Men who have sex with men
- MSW:
-
Male sex workers
- NGO:
-
Non-governmental organization
- NRP:
-
Non-regular sex partner
- OR:
-
Univariate odds ratios
- ORm:
-
Multivariate odds ratios
- PrEP:
-
Pre-exposure prophylaxis
- RP:
-
Regular sex partner
- SD:
-
Standard deviation
- STD:
-
Sexually transmitted diseases
- TDF:
-
Tenofovir disoproxil fumarate
- TPB:
-
Theory of planned behavior
- WHO:
-
World Health Organization
References
Nemoto T, Iwamoto M, Perngparn U, Areesantichai C, Kamitani E, Sakata M. HIV-related risk behaviors among kathoey (male-to-female transgender) sex workers in Bangkok, Thailand. AIDS Care. 2012;24(2):210–9.
Center for AIDS Prevention Studies. What are the prevention needs of male-to-female transgender persons (MTFs)? San Francisco, CA: University of California, San Francisco. 2001. http://www.caps.ucsf.edu/pubs/FS/MTF.php.
Poteat T, Wirtz AL, Radix A, Borquez A, Silva-Santisteban A, Deutsch MB, et al. HIV risk and preventive interventions in transgender women sex workers. Lancet. 2015;385(9964):274–86.
Roche K, Keith C. How stigma affects healthcare access for transgender sex workers. Br J Nurs. 2014;23(21):1147–52.
Operario D, Soma T, Underhill K. Sex work and HIV status among transgender women: systematic review and meta-analysis. J Acquir Immune Defic Syndr. 2008;48(1):97–103.
Cai Y, Wang Z, Lau JT, Li J, Ma T, Liu Y. Prevalence and associated factors of condomless receptive anal intercourse with male clients among transgender women sex workers in Shenyang, China. J Int AIDS Soc. 2016;19(3 Suppl 2):20800.
Richter ML, Chersich M, Temmerman M, Luchters S. Characteristics, sexual behaviour and risk factors of female, male and transgender sex workers in South Africa. S Afr Med J. 2013;103(4):246–51.
Hawkes S, Collumbien M, Platt L, Lalji N, Rizvi N, Andreasen A, et al. HIV and other sexually transmitted infections among men, transgenders and women selling sex in two cities in Pakistan: a cross-sectional prevalence survey. Sex Transm Infect. 2009;85(Suppl 2):ii8–16.
Taylor RD, Bimbi DS, Joseph HA, Margolis AD, Parsons JT. Girlfriends: evaluation of an HIV-risk reduction intervention for adult transgender women. AIDS Educ Prev. 2011;23(5):469–78.
Longfield K, Panyanouvong X, Chen J, Kays MB. Increasing safer sexual behavior among Lao kathoy through an integrated social marketing approach. BMC Public Health. 2011;11:872.
Lipsitz MC, Segura ER, Castro JL, Smith E, Medrano C, Clark JL, et al. Bringing testing to the people—benefits of mobile unit HIV/syphilis testing in Lima, Peru, 2007-2009. Int J STD AIDS. 2014;25(5):325–31.
Pawa D, Firestone R, Ratchasi S, Dowling O, Jittakoat Y, Duke A, et al. Reducing HIV risk among transgender women in Thailand: a quasi-experimental evaluation of the sisters program. PLoS ONE. 2013;8(10):e77113.
Goswami P, Rachakulla HK, Ramakrishnan L, Mathew S, Ramanathan S, George B, et al. An assessment of a large-scale HIV prevention programme for high-risk men who have sex with men and transgenders in Andhra Pradesh, India: using data from routine programme monitoring and repeated cross-sectional surveys. BMJ Open. 2013;3(4):e002183.
Subramanian T, Ramakrishnan L, Aridoss S, Goswami P, Kanguswami B, Shajan M, et al. Increasing condom use and declining STI prevalence in high-risk MSM and TGs: evaluation of a large-scale prevention program in Tamil Nadu, India. BMC Public Health. 2013;13:857.
Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99.
Deutsch MB, Glidden DV, Sevelius J, Keatley J, McMahan V, Guanira J, et al. HIV pre-exposure prophylaxis in transgender women: a subgroup analysis of the iPrEx trial. Lancet HIV. 2015;2(12):e512–9.
Abdool Karim Q, Abdool Karim SS, Frohlich JA, Grobler AC, Baxter C, Mansoor LE, et al. Effectiveness and safety of tenofovir gel, an antiretroviral microbicide, for the prevention of HIV infection in women. Science. 2010;329(5996):1168–74.
Baeten J, Celum C. Antiretroviral pre-exposure prophylaxis for HIV-1 prevention among heterosexual African men and women: the Partners PrEP Study. In: 6th IAS Conference on HIV Pathogenesis, Treatment and Prevention. Rome. 2011.
Choopanya K, Martin M, Suntharasamai P, Sangkum U, Mock PA, Leethochawalit M, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2013;381(9883):2083–90.
Gomez GB, Borquez A, Caceres CF, Segura ER, Grant RM, Garnett GP, et al. The potential impact of pre-exposure prophylaxis for HIV prevention among men who have sex with men and transwomen in Lima, Peru: a mathematical modelling study. PLoS Med. 2012;9(10):e1001323.
World Health Organization. Consolidated guidelines on HIV prevention, diagnosis, treatment and care for key populations. 2014. http://www.who.int/hiv/pub/guidelines/keypopulations/en/.
Yang D, Chariyalertsak C, Wongthanee A, Kawichai S, Yotruean K, Saokhieo P, et al. Acceptability of pre-exposure prophylaxis among men who have sex with men and transgender women in Northern Thailand. PLoS ONE. 2013;8(10):e76650.
Hoagland B, De Boni RB, Moreira RI, Madruga JV, Kallas EG, Goulart SP, et al. Awareness and willingness to use pre-exposure prophylaxis (PrEP) among men who have sex with men and transgender women in Brazil. AIDS Behav. 2016.
Oldenburg CE, Le B, Toan T, Thien DD, Huyen HT, Friedman MR, et al. HIV pre-exposure prophylaxis indication and readiness among HIV-uninfected transgender women in Ho Chi Minh City, Vietnam. AIDS Behav. 2016.
Wilson EC, Jin H, Liu A, Raymond HF. Knowledge, indications and willingness to take pre-exposure prophylaxis among transwomen in San Francisco, 2013. PLoS ONE. 2015;10(6):e0128971.
Golub SA, Gamarel KE, Rendina HJ, Surace A, Lelutiu-Weinberger CL. From efficacy to effectiveness: facilitators and barriers to PrEP acceptability and motivations for adherence among MSM and transgender women in New York City. AIDS Patient Care STDs. 2013;27(4):248–54.
Peinado J, Lama JR, Galea JT, Segura P, Casapia M, Ortiz A, et al. Acceptability of oral versus rectal HIV preexposure prophylaxis among men who have sex with men and transgender women in Peru. J Int Assoc Provid AIDS Care. 2013;12(4):278–83.
Wheelock A, Eisingerich AB, Ananworanich J, Gomez GB, Hallett TB, Dybul MR, et al. Are Thai MSM willing to take PrEP for HIV prevention? An analysis of attitudes, preferences and acceptance. PLoS ONE. 2013;8(1):e54288.
Mimiaga MJ, Closson EF, Kothary V, Mitty JA. Sexual partnerships and considerations for HIV antiretroviral pre-exposure prophylaxis utilization among high-risk substance using men who have sex with men. Arch Sex Behav. 2014;43(1):99–106.
Baeten JM, Haberer JE, Liu AY, Sista N. Preexposure prophylaxis for HIV prevention: where have we been and where are we going? J Acquir Immune Defic Syndr. 2013;63(Suppl 2):S122–9.
Nemoto T, Bodeker B, Iwamoto M. Social support, exposure to violence and transphobia, and correlates of depression among male-to-female transgender women with a history of sex work. Am J Public Health. 2011;101(10):1980–8.
Cohan D, Lutnick A, Davidson P, Cloniger C, Herlyn A, Breyer J, et al. Sex worker health: San Francisco style. Sex Transm Infect. 2006;82(5):418–22.
Boles J, Elifson KW. The social organization of transvestite prostitution and AIDS. Soc Sci Med. 1994;39(1):85–93.
Ye L, Wei S, Zou Y, Yang X, Abdullah AS, Zhong X, et al. HIV pre-exposure prophylaxis interest among female sex workers in Guangxi, China. PLoS ONE. 2014;9(1):e86200.
Peacock E, Andrinopoulos K, Hembling J. Binge drinking among men who have sex with men and transgender women in san salvador: correlates and sexual health implications. J Urban Health. 2015;92(4):701–16.
Flentje A, Heck NC, Sorensen JL. Characteristics of transgender individuals entering substance abuse treatment. Addict Behav. 2014;39(5):969–75.
Zhou F, Gao L, Li S, Li D, Zhang L, Fan W, et al. Willingness to accept HIV pre-exposure prophylaxis among Chinese men who have sex with men. PLoS ONE. 2012;7(3):e32329.
McEachana RRC, Conner M, Taylor NJ, Lawton RJ. Prospective prediction of health-related behaviours with the theory of planned behaviour: a meta-analysis. Health Psychol Rev. 2011;5(2):97–144.
Brooks RA, Landovitz RJ, Regan R, Lee SJ, Allen VC Jr. Perceptions of and intentions to adopt HIV pre-exposure prophylaxis among black men who have sex with men in Los Angeles. Int J STD AIDS. 2015;26(14):1040–8.
Veloso VG, Mesquita F, Grinsztejn B. Pre-exposure prophylaxis for men and transgender women who have sex with men in Brazil: opportunities and challenges. J Int AIDS Soc. 2015;18(4 Suppl 3):20010.
Zhang Y, Peng B, She Y, Liang H, Peng HB, Qian HZ, et al. Attitudes toward HIV pre-exposure prophylaxis among men who have sex with men in western China. AIDS Patient Care STDs. 2013;27(3):137–41.
Michie S, Johnston M, Francis J, Hardeman W, Eccle M. From theory to intervention: mapping theoretically derived behaviorual determinants to behaviour change techniques. Appl Psychol. 2008;57:660–80.
Ajzen I. The theory of planned behaivor. Organ Behav Hum Decis. 1991;50(2):179–211.
Wang Z, Feng T, Lau JT. Needs assessment and theory-based promotion of voluntary medical male circumcision (VMMC) among male sexually transmitted diseases patients (MSTDP) in China. AIDS Behav. 2015.
Lau JT, Zhang J, Yan H, Lin C, Choi KC, Wang Z, et al. Acceptability of circumcision as a means of HIV prevention among men who have sex with men in China. AIDS Care. 2011;23(11):1472–82.
Ko NY, Yeh SH, Tsay SL, Ma HJ, Chen CH, Pan SM, et al. Intention to comply with post-exposure management among nurses exposed to blood and body fluids in Taiwan: application of the theory of planned behaviour. J Hosp Infect. 2011;77(4):321–6.
Song Y, Huang Y, Liu D, Kwan JS, Zhang F, Sham PC, et al. Depression in college: depressive symptoms and personality factors in Beijing and Hong Kong college freshmen. Compr Psychiatry. 2008;49(5):496–502.
Cheung CK, Bagley C. Validating an American scale in Hong Kong: the center for epidemiological studies depression scale (CES-D). J Psychol. 1998;132(2):169–86.
Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7.
Guidance for the use of pre-exposure prophylaxis (PrEP) to prevent HIV transmission. 2016. http://www.hivguidelines.org/wp-content/uploads/2016/02/PrEP-Guidance_10-14-15.pdf.
Hail-Jares K, Chang RC, Choi S, Zheng H, He N, Huang ZJ. Intimate-partner and client-initiated violence among female street-based sex workers in China: does a support network help? PLoS ONE. 2015;10(9):e0139161.
Richens J, Imrie J, Copas A. Condoms and seat belts: the parallels and the lessons. Lancet. 2000;355(9201):400–3.
Wilde GJS. Target risk: dealing with danger of death, disease, and damage in everday decisions. Ontario: PDE Publications; 1994.
Li D, Li C, Wang Z, Lau JT. Prevalence and associated factors of unprotected anal intercourse with regular male sex partners among HIV negative men who have sex with men in China: a cross-sectional survey. PLoS ONE. 2015;10(3):e0119977.
O’Cleirigh C, Skeer M, Mayer KH, Safren SA. Functional impairment and health care utilization among HIV-infected men who have sex with men: the relationship with depression and post-traumatic stress. J Behav Med. 2009;32(5):466–77.
Best J, Tang W, Zhang Y, Han L, Liu F, Huang S, et al. Sexual behaviors and HIV/syphilis testing among transgender individuals in China: implications for expanding HIV testing services. Sex Transm Dis. 2015;42(5):281–5.
Nemoto T, Operario D, Keatley J, Han L, Soma T. HIV risk behaviors among male-to-female transgender persons of color in San Francisco. Am J Public Health. 2004;94(7):1193–9.
Nemoto T, Operario D, Keatley J, Villegas D. Social context of HIV risk behaviours among male-to-female transgenders of colour. AIDS Care. 2004;16(6):724–35.
Bockting WO, Robinson BE, Rosser BR. Transgender HIV prevention: a qualitative needs assessment. AIDS Care. 1998;10(4):505–25.
Bianchi FT, Reisen CA, Zea MC, Vidal-Ortiz S, Gonzales FA, Betancourt F, et al. Sex work among men who have sex with men and transgender women in Bogota. Arch Sex Behav. 2014;43(8):1637–50.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research Involving Human Participants
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Survey and Behavioural Research Ethics Committee, the Chinese University of Hong Kong and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Wang, Z., Lau, J.T.F., Yang, X. et al. Acceptability of Daily Use of Free Oral Pre-exposure Prophylaxis (PrEP) Among Transgender Women Sex Workers in Shenyang, China. AIDS Behav 21, 3287–3298 (2017). https://doi.org/10.1007/s10461-017-1869-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-017-1869-4