Abstract
Despite the high incidence of HIV among young Black MSM in the United States and engagement in high risk behaviors, many men in this group avoid infection. This suggests that some men may engage in systematic risk reduction behaviors when not always using condoms or abstaining from substances. Using a “positive deviance” framework, we conducted qualitative interviews with HIV-negative, Black MSM between 25 and 35 who reported unprotected anal sex and drug use in the past six months or current heavy drinking (N = 29) to discover behaviors that could facilitate remaining HIV-uninfected. Findings showed that MSM who remain HIV negative despite continuing to engage in high-risk behaviors may be engaging in adaptive risk reduction behaviors that, through successive decisions and advance planning along the timeline to a sexual event, could lead to increased condom use, avoidance or delay of a risky sexual event, or reduction of HIV positive partners.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although the overall incidence of HIV in the United States (U.S.) is declining, new infections among men who have sex with men (MSM) have increased steadily since the 1990s [1,2,3,4]. Black men of all ages in the U.S. are disproportionately affected by the disease but more new infections occur among Black MSM between 13 and 29 as in any other age and racial/ethnic group of MSM [5]. Among Black MSM in this age group, new infections increased by 48% between 2006 and 2009 [2]. In 2010, young Black MSM between 13 and 24 accounted for approximately 4800 new HIV infections—more than twice as many than either young White or young Hispanic/Latino MSM [5]. An estimated 16.5% of young Black MSM in the United States are infected with HIV, a prevalence rate almost as high as the 17.8% rate among all adults in South Africa [6]. Among urban Black MSM who face multiple risks such as poverty and substance use, prevalence is even higher. In Los Angeles in 2014, HIV prevalence among Black MSM over the age of 18 was 34% [7]; incidence among Black MSM who reported unprotected anal sex in the last six months was 6.9% [8].
Most behavioral interventions have failed to lower HIV incidence among young Black MSM [9] and use of pre-exposure prophylaxis (PrEP) medication in general [10, 11] and among Black MSM in particular [12] remains low. However, despite the unacceptably high incidence of HIV among young Black MSM, many men successfully avoid HIV infection. While some men may follow standard prevention strategies, such as using condoms, others may be managing their behaviors, possibly in a systematic way, even though they do not remain 100% adherent to condoms.
A study of positive deviance, defined as behaviors that contribute to otherwise high-risk individuals remaining free from a disease or condition [13, 14], offers a different lens by which to understand ways in which men with a high likelihood of encountering HIV remain HIV uninfected. In the context of HIV prevention, a “positive deviant” refers to a person who deviates from a high-risk trajectory; that is, someone who is exposed to and even engages in high-risk behaviors (like having unprotected anal intercourse, with or without drug use) but who does not contract infection. Adaptive risk reduction behaviors are defined as uncommon risk reduction strategies, or uncommon behaviors that contribute to commonly known prevention strategies, like condom use [15].
Positive deviance interventions typically involve identifying individuals with better outcomes than their peers; interviewing these individuals to discover adaptive and presumably uncommon behaviors; analyzing findings to confirm that the behaviors are uncommon in general but common among those who avoid the disease despite the risks they are engaging in; and when feasible, developing community-based, peer-led behavior change interventions based on the behaviors and strategies of “positive deviants” [13, 14]. Positive deviance fits into the growing interest in resilience as a resource in the fight against HIV/AIDS [16,17,18,19]. However, where resilience approaches tend to examine psychological and external social contributors to positive adaptive outcomes [16, 18, 20, 21], positive deviance approaches typically examine uncommon behaviors that may be protective.
Friedman et al. examined positive deviance among people who inject drugs (PWID) who remained HIV- and Hepatitis C Virus (HCV)-negative after 8-15 years of injecting [15, 22]. They found that PWID who remained both HIV and HCV negative had developed strategies for “symbiotic goals” (such as avoiding withdrawal) as well as deliberate strategies that helped them to avoid infection. Other studies have examined short-term strategies for avoiding HIV among PWID and sex workers. For example, some PWID only use syringes if they are sealed in the package and some may sniff the drug instead of injecting it if clean syringes are not available; sex workers employ creative strategies to ensure client condom use [23].
This study sought to discover whether behaviors reported by young, Black HIV-negative MSM who have used substances that increase risk for HIV in the past six months, such as methamphetamine, cocaine, club drugs, as well as those who currently have hazardous alcohol use [24,25,26] (as assessed by the Alcohol Use Disorders Identification Test (AUDIT-C)) [27] could be serving as adaptive risk reduction strategies that help them avoid HIV infection. This article describes findings from 29 qualitative interviews. We conducted these interviews as Phase I of a larger study (Project Discover) which is using the findings from this work to develop an “Adaptive Strategies Questionnaire.” Developing a better understanding of behaviors that could be facilitating safer sex practices by men at high risk for HIV could ultimately contribute to innovative harm reduction interventions that are highly relevant to this population. To our knowledge, this is the first study to use a positive deviance approach to study adaptive strategies among MSM.
Methods
Participants
Participants were a convenience sample of HIV-negative Black men (i.e., men who described themselves as Black, African American, Caribbean, or African) between ages 25 and 35 who reported drug use (powder or crack cocaine, methamphetamine, 3,4-methylenedioxy-methamphetamine (MDMA), Gama Hydroxybutyric Acid (GHB), ketamine, rohypnol, amyl nitrite and other versions of “poppers” in the past six months, or who had current hazardous alcohol use (i.e., a score of 4 or higher on the AUDIT-C [27]), and reported anal sex with another man in the past 6 months. The AUDIT-C is a brief alcohol screen that identifies hazardous drinkers or those with an active alcohol use disorder. The AUDIT-C takes into account frequency, amount and binge-drinking and is scored on a scale from 0 to 12. In men, a score of 4 or higher is considered positive, or indicative of hazardous drinking or worse. In this phase of the study, we restricted the age range to 25–35—slightly older than the Black men currently at the highest risk for HIV—because we wanted to discover adaptive strategies among HIV-negative Black MSM who had been exposed to risk for a longer period of time than younger Black MSM who may not have been exposed to as much risk [15]. We recruited participants through fliers and palm cards posted at a variety of entertainment, health care, and substance use disorder treatment venues throughout Los Angeles (primarily in West Hollywood, an area with multiple gay-identified venues), Craig’s list advertisements, and Facebook posts on sites of community organizations that serve Black MSM.
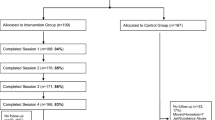
Procedures
This study used in-depth qualitative interview methods to uncover behaviors that may help young, high-risk Black MSM avoid HIV infection. Participants were screened over the telephone for preliminary eligibility. Upon completion of in-person eligibility screening and consent, participants were given a free rapid HIV test (Oraquick®) to verify HIV-negative status. Men who believed they were HIV-negative but tested HIV-positive (N = 1) were not eligible for the study, but were given a confirmatory western blot test and assisted into care. Confirmed HIV-negative participants participated in a 90-min interview with the Discover Study Coordinator. All interviews were audio-recorded. Interviews and HIV tests were conducted at the UCLA Vine Street Clinic between October 2013 and May 2014. All procedures were approved by the RAND Human Subjects Protection Committee.
Measures
Demographics and Sexually Transmitted Infections (STIs)
Prior to the interview, we asked about age, education, living arrangements, income, partnership status, sexual identification and current and past sexually transmitted infections (STIs).
Qualitative Interview Data
We developed a qualitative interview guide for the in-depth interviews. The Discover project team developed the initial guide and then obtained input from two community members (young Black MSM) and two consultants (researchers who conduct research on HIV risk among young Black MSM) on the language, tone and overall approach. The interview covered three primary domains: life management (i.e., employment, housing, free time) and social networks; sex partners, sexual behaviors, and drug use; and HIV and health. The last part of the interview captured participants’ final thoughts about remaining HIV-negative. Throughout the interview, the interviewer asked open-ended questions followed by closed-ended questions to avoid biasing responses [28, 29]. The interview also contained multiple probes to uncover potentially adaptive behaviors [29, 30]. Probes included questions such as, if the person reported using condoms regularly, “some people say it’s difficult to use condoms all or most of the time. How do you manage?” Or, if a participant reported not using drugs or drinking before having sex, “people tell us they have trouble managing their drug use. What has helped you?” And, “are there any exceptions to doing things this way?”
Qualitative Data Analysis
We audio-recorded and transcribed the interviews. We used standard qualitative methods to identify themes that indicated adaptive strategies. Themes are defined as patterns associated with a specific research question [31, 32]. The PI and study coordinator read all transcripts to identify overarching themes, looking for repetitions across interviews, and then developed a codebook listing each theme. Using Atlas.ti, we coded areas of text pertaining to each theme. Next, we worked on the first five interviews independently, after which we measured coder consistency, evidenced by a Kappa of 0.68 (considered “good” consistency) [33]. The codebook contains 88 themes; we coded 5,811 segments of text. Team members then reviewed all coded text, examined the most frequently mentioned themes, and then selected those that were directly relevant to adaptive behaviors that could facilitate avoidance of HIV. Themes and salient comments relevant to behaviors that could be serving to intentionally or unintentionally avoid HIV are presented in this article and are the foundation of the “Adaptive Strategies Questionnaire” (ASQ), which is currently being field tested.
Results
Participant Characteristics
Seventy-two percent of 29 participants in the study reported being “single” in that they were not in a committed partnership of any kind. However, even for men who reported that they were currently in committed relationships, the activities they described during the interview primarily were during first-time meetings and sexual encounters with sexual partners. Almost half of the men in the sample had at least some college, most (83%) rented or owned their own home, and slightly more than half had an income of 20,000 or less. Two thirds of the men of the men identified with being gay (See Table 1).
As a measure of current risk for HIV and other sexually transmitted infections (STI), 41% reported ever having an STI (see Table 2). Twenty-one percent reported having gonorrhea in their lifetime, with one man reporting diagnosis in the last three months, 17% ever had chlamydia, 10% ever had human papilloma virus (HPV), and one person reported having had syphilis. Two participants reported having symptoms of a current STD.
Ninety-three percent of the men reported hazardous alcohol use. Exclusive of marijuana, powder cocaine, ecstasy, poppers and methamphetamine were the most commonly reported drugs (see Table 2).
During the qualitative interviews, three men reported that they “always use condoms” during anal sex while 26 (90%) described at least one time that they did not use condoms.
Adaptive Risk Reduction Behaviors
Participants reported a number of behaviors that could lead to risk reduction, such as using a condom during a sexual event, avoidance or delay of a sexual event, or reducing exposure to HIV positive partners. Some behaviors seemed to be intentional strategies for avoiding HIV, such as asking to see results of a partner’s last HIV test, while other behaviors, though they could ultimately lower HIV risk, were not intentionally selected for that reason. Some men also reported personal attitudes, goals and values that may be driving some of their adaptive behaviors; we refer to these attitudes, goals and values as “symbiotic” factors [22]. Of note, risk reduction, while it is ultimately driven by behaviors (e.g., not going to bathhouses) which are often codified into cognitive rules (e.g., “I avoid bathhouses”), is supported by underlying beliefs, preferences and values (e.g., “I avoid bathhouses because I’m scared of germs and places like that are filled with germs” or “I avoid the gay scene”). Thus, men may have adaptive behaviors in common but may engage in these behaviors for different reasons.
We report behaviors in categories along a continuum consisting of successive steps and decisions at each step that may occur prior to and during a sexual encounter or “hookup” that could cumulatively lead to lower risk. The first step involves exposure to a pool of potential partners (e.g., through personal networks, places or online searches). The next step is filtering the partner pool down to a smaller set and screening potential candidates to fit personal preferences. The final step is engaging in behaviors that serve to prevent risk during the sexual event. Thus, adaptive strategies can come into play at various points that lead to a sexual encounter. The categories, which are not always discrete, along the continuum to a sexual event, are as follows: (1) looking for sex partners (i.e., places and methods for finding partners), (2) screening and selecting sex partners (i.e. who is selected or not selected), (3) planning for a sexual event (i.e., planning around condoms, drinking and drug use), and (4) behaviors that occur immediately prior to and during the sexual encounter itself.
Fifteen themes emerged from the interviews. Table 3 outlines these themes as they fall along the continuum leading to a sexual event. In this section we describe the themes and provide illustrative quotes from the men in the study. Of note, some of the themes on which we report are not necessarily unstudied or uncommon, but within each theme, common or not, we sought to understand why the behaviors were adopted, how they are maintained, and how they could be serving to reduce exposure to risk.
Looking for Sex Partners
This category pertains to places where men said they look for partners or places they said they avoid. The dominant theme in this category was avoidance of gay-identified venues.
Avoid Bathhouses and Gay-Identified Venues
Six (21%) participants mentioned avoiding gay-identified spaces, including gay clubs, the house and ball community, and the City of West Hollywood, an area of Los Angeles where there are multiple gay-identified social and sexual venues, and 12 out of the 29 (41%) participants explicitly mentioned avoiding bathhouses when looking for sexual partners. Although avoidance of gay-identified venues may not be considered uncommon or adaptive, it is an example of a behavior that could lead to exposure to fewer HIV positive partners, or in the case of bathhouses, avoidance of a venue where sex can be immediate, with little time for partners to disclose HIV status or otherwise become acquainted with one another.
One participant described his avoidance of gay-identified venues this way:
For some reason I have issues with going into West Hollywood. I don’t know why. I just don’t. They get on my nerves. They get on my nerves out here. They do. Bunch of bitchy queens. I don’t have time for that shit. I’m not like that. (laughs) I don’t like that shit. (P007, age 27, ecstasy, marijuana, methamphetamine, and heavy alcohol user).
The following is an unsolicited response about avoiding bathhouses in which the participant states his explicit intention of avoiding bathhouses to avoid HIV: “Well most of the places that they [friends] pretty much want to go to, we all want to go to, but I would not go into the bathhouse (P003, age 30, heavy alcohol user).”
When the interviewer asked, “why not,” the participant responded this way:
Because it’s like a place for disease. That’s like a place for STDs just waiting for you. They give out condoms and all that, lube and all that, but no. As germ-a-phobic as I am, like you can cough right now and I would like jump out of my skin. I would jump so far into this corner, so it’s like I have to know you in order to—I mean I would spend time with you, date you, to even get to kiss my lips.
Where these participants discussed avoiding bathhouses to avoid HIV and other STDs, others said they avoid bathhouses for reasons related more to their values and personal preferences than intentional avoidance of STIs. For example, when asked about places he avoids looking for partners, this participant commented:
Bathhouses, I just don’t think that’s the type of environment that I should be in. Like I would be too afraid to have sex with anybody there because I don’t know them. I don’t know who they’ve had sex with and I’m not sure I even want to know that, and if I can’t know I’m not going to do it. So, it’s just not my scene. I don’t want people touching on me. I don’t need to see your body. (P022, age 32, heavy alcohol user)
Spend Time with Diverse Social Networks
Another theme that emerged as men described “looking for sex partners” was having a diverse social network with regard to race, ethnicity, gender and sexual orientation. Having a racially and ethnically diverse social network could lead to more a diverse pool of partners. Because Black MSM have the highest rate of HIV, a diverse network could lower the risk of selecting an HIV positive partner. Nine of 29 (31%) participants explicitly mentioned having a diverse social network that includes men and women of differing racial/ethnic backgrounds and sexual orientations. As one participant noted,
… Like, where I see as most people have one social group, I have many. I have multiple that I can go in and out of and it’s like so it may be, like, one or two months before I see them again. I might see them for a little while and then I go on to another one or whatever. I meet other people and get into another social circle. It’s just crazy. I’m extremely social. It’s easy for me to not be into, like, one group, and I kind of like it like that because if I get tired, I just go somewhere else. (P007, age 27, ecstasy, marijuana, methamphetamine, and heavy alcohol user.)
Selecting Sex Partners
Themes in this section refer to types of sex partners men tend to select or avoid and how they screen for preferences. Important to note is that participants distinctly mentioned avoiding three types of sexual partners: people they believed were HIV-positive or who disclosed their HIV-positive status; users of injection drugs or heavy users of non-injection drugs; and men that participants described as “flamboyant” or “feminine.” These themes seemed to be a function of two overarching goals: strategic (as perceived by the participant) avoidance of HIV and a more symbiotic goal of adhering to personal values. Here again we report all themes that emerged, regardless of whether they were uncommon, previously unstudied, or whether they are, at face value, associated with HIV prevention.
Avoid HIV-Positive Partners
Nine of the 29 (31%) participants explicitly mentioned avoiding having sex with partners who they believed were HIV-positive or partners who disclosed their HIV-positive status. When asked about the types of sexual partners he tries to avoid, one participant mentioned this:
If somebody’s positive—told me they positive, we just conversate and that’s it. But I wouldn’t—they told me they was positive I wouldn’t indulge in no sexual activities. I wouldn’t indulge in no sexual activity because that’s risky even with a condom to me that’s risky. I don’t even want to be a part of that. And I know there’s guys that will but not me… If somebody told me they’re HIV positive, to me that would frighten me to even want to participate in anything but conversation. (P016, age 33, poppers, powder cocaine and heavy alcohol user.)
Another had this to say:
If I’m talking to somebody online that is just like going to be a random hookup, then, yes, I talk about all that kind of stuff. We talk about HIV status. If they’re HIV positive then I probably won’t. If they disclose it to me then… My mind is not all the way made up on this but it’s never been an issue. I’ve never run across this where they’re HIV positive or they didn’t tell me. But if they say no then I’m going to; we’re using protection anyway. But if they said yes then I’m pretty sure I would make the conversation go in a different route or something. (P014, age 27, marijuana and heavy alcohol user.)
Use Strategic Online Screening
Six (21%) of the men said that when they look for partners on online social platforms such as Craigslist, Adam 4 Adam, Facebook, and Scruff, they engage in strategic screening with potential sexual partners prior to meeting them in person to evaluate their HIV status. One participant described his screening process this way:
… First, pick, see if you’re cute. But you don’t have to be crazy in shape, because I’m into all types. They’ve just got to be something that I’m attracted to, that’s the first step. Then I ask if you’re STD free. Then it’s weird because I do two different things: I’ll try to trick them, to ask them whether or not they would ever have sex without a condom or how often would they do that, like I’d ask them “Are you willing to have…” And if they say yes, then they’re not a person for me. That means they’re crazy, so I go, “no.” So then once I find out that they’re actually pretty secure in how they like protecting themselves as much as I do, then I usually give them my number and we talk maybe five seconds. Then my address and then they come over. (P008, age 27, powder cocaine and heavy alcohol user.)
Other participants also alluded to an extensive screening process such as this and mentioned specifically searching for profiles that stated that men were “HIV or STI free;” some even asked for documentation proving their partners’ HIV status. As one participant described, “I’d meet somebody on an app, and I’d say exactly what I wanted. It would be like using College Guide, “looking for a fuck buddy,” or “STD free,” or “let’s play safe,” something like that.” (P008, age 27, powder cocaine and heavy alcohol user.)
Another said this when asked how he usually finds out a potential partner’s HIV status:
Look in the face, the face can have some kind of deformity, like, I know the cheek, one cheek—one jaw look bigger than the other, something’s not right. Even skin, if skin has like some type of rash, just on them, I know something’s not right. So those things I would stay away from. If a guy or a girl say—we was with this man and they talking about don’t use condoms, something’s not right. So those are things I would look for and I would try to refrain from if they don’t produce no type of paperwork showing that, you know, they took the test within the last 30 days or even—I might even go 60 days, max, … (P016, age 33, powder cocaine and heavy alcohol user.)
Avoid Users of Injection Drugs or Heavy Users of Non-injection Drugs
Five participants (17%), some of whom were themselves people who use drugs and others who used alcohol only, mentioned that they explicitly avoid users of injection drugs and users of other drugs as sexual partners. For example, when asked if there were any types of sexual partners he explicitly avoids, one participant said this: “Mm-hmm. Drug addicts. I try to avoid them because those are the most people that have HIV and the more people that HIV things are not taken care of.” (P017, age 26, marijuana, poppers, powder cocaine, and heavy alcohol user.)
Some participants expressed a similar sentiment about avoiding people who inject and those who use non-injectable drugs because they perceived them to be mostly likely to be HIV-positive. Participants also mentioned avoiding people who use drugs because of personal values about the types of partners they would like to have sex with. One participant described his feelings this way:
I wouldn’t have sex with somebody who I knew was like on coke or drugs, and crystal meth and all that kind of stuff. I wouldn’t have sex with somebody who just like appeared not to have no self-respect, yeah. Like somebody who’s just always in the club and in somebody’s face. Every time you turn around it’s somebody different. Like, no, I’m not doing that. (P012, age 29, ecstasy and heavy alcohol user.)
When the interviewer asked why he tries to avoid these people, the participant said this:
I don’t know. I always say it’s not what you do, it’s how you do it. And if you’re going to have sex with people be careful who you’re having sex with. Like, for one, I’m a private person so I would never want to fuck with somebody who’s like out and like who talked a lot or whatever like that, like I’m very selective with the people that I sleep with. Because I think reputation is everything, especially in the gay lifestyle.
In this statement and others that are similar, avoiding partners who use drugs is for some participants believed to be a strategic method to avoid HIV based on stereotyping people who drugs as either HIV positive our unable to maintain control; for others it seems to be a means to maintaining a sense of core values associated with the types of people with whom they have sex.
Avoid Partners Perceived as “Flamboyant” or “Feminine”
Another theme that arose around selecting partners was avoidance of partners perceived to be feminine or “very gay.” Five (17%) participants noted avoiding this type of partner. Among these men, this avoidance behavior seemed to be due more to homophobia or homonegativity and stereotyping than due to perceptions of higher HIV prevalence in this group. When asked if there are some partners he avoids having sex with, one participant stated his preference this way:
Yes. Like very gay people. Like outwardly like flamboyant people. I don’t really like that… Like they can be gay, but don’t…Very outwardly flamboyant. It’s not my type. Like, it’s cool for people to be that way, I don’t mind them but they’re just not for me. (P013, age 26, heavy alcohol user.)
Another participant described his preference this way:
I’m not going to have sex with a fem queen, a drag queen, a fem queen, I’ll never have sex with a fem queen. First, I don’t want a girlfriend, no disrespect, I had girlfriends, I don’t want a girlfriend, if I want a girlfriend I’ll get a girlfriend, you look like a girl, you got breasts, then you have a penis, too … I don’t like feminine boys, no more, not really, but it’s really weird because as far as topping me, I have it in my head, I don’t see it. (P004, age 30, heavy alcohol user.)
Planning the Sexual Encounter/Hookup
“Planning the sexual encounter/hookup” refers to behaviors related to events that happen after partner selection and prior to meeting someone for the first time for sex. Although planning for sexual encounters is different for men planning to have sex with committed partners compared with men planning to have sex with casual sexual partners or one-time “hookups,” commentary about planning sexual encounters did not seem to differ between the two groups. In this sample, seven men were in committed relationships, one of whom was married to a woman, but none of the committed relationships described (except for the married man) were established longer than a year prior to the interview. Additionally, most men described the initial sexual encounters with their committed partners in addition to sexual encounters with new partners they had in the past. Themes that arose around planning for a sexual encounter included always carrying condoms and restricting drug use to certain people, places and times to avoid being too high or drunk. We include carrying condoms here because, while condom use itself clearly is not an uncommon way to prevent HIV, who carries condoms, how they remember to carry them and other unique facets of this behavior are not as well known or understood.
Always or Almost Always Carry Condoms
Five (17%) participants said they always or typically carry condoms with them. One participant said this, as he pulled a plastic bag filled with condoms out of his backpack to demonstrate: “I carry condoms with me everywhere I go” (P002, 29, heroin, powder cocaine, and heavy alcohol user.)
Two other participants mentioned carrying condoms with them when they thought they would be engaging in anal sex with partners. One participant noted that he keeps condoms available, out in the open in his apartment:
I have a candy dish that I had bought it a few years ago when I was working at a job and I used to keep candy in it. But since I don’t have a desk or a place to put the candy in, I now keep condoms in it. And so, it sits right there at my bed. (P009, age 34, marijuana, powder cocaine, and heavy alcohol user.)
Restrict Drug and Alcohol Use to Certain Times, People and Places
Twelve of the 29 (41%) participants mentioned restricting alcohol and/or drug use to certain times, people, and places with the specific intention, in most cases, of keeping presence of mind during nights out. When asked about who they use drugs and drink with, one participant said, “Yeah, when I usually do certain like harder drugs. I mean, they have to be cool and have some of rapport with me. If I’m just drinking and some social drinks it’s not that big of a deal” (P001, age 34, methamphetamine, marijuana and heavy alcohol user.)
Another said this:
I’m not normally a drug guy, so I don’t normally like drugs, and I like reality a little bit. So it’s not something I want, but if, to be honest with you, if my [best friends] asked me to do cocaine again, I would do it in a heartbeat. So it’s only with those people. It’s a people kinda thing. But just with random, everyday people I met, like in a party and shit, no. It’s not worth it. (P008, age 27, powder cocaine and heavy alcohol user.)
Take Pre-exposure Prophylaxis (PrEP)
Four (14%) participants said they were taking PrEP. We include this is an uncommon and possibly adaptive strategy because uptake of PrEP among MSM, and Black MSM in particular, has been slow. Understanding more about who takes it and how they decided to start is useful to understanding how to increase uptake. One participant explained his decision to take the medication: “Because, last year, I was exposed and then this year I just decided to take it.” Another participant had this to say:
If it’s [PrEP] the first step to helping people stay negative, I’m for it. I don’t necessarily care for all the listed side effects that it’s believed to cause it and I don’t really care for—because it works, in a sense, for me … It works for me, hopefully it works for other people too. (P009, age 34, marijuana and powder cocaine user.)
Interestingly, four participants said they supported the idea of PrEP for others, but didn’t view it is as something that would be appropriate for them. One participant said he did not like taking pills, another said he wouldn’t remember to take the pill, and two commented that medication was more for men with very high risk behavior, such as those who frequent bathhouses or those who have a lot of sexual partners and engage in unprotected receptive anal sex often.
Immediately Prior to and During the Sexual Event
Themes involving behaviors that occur immediately prior to and during the sexual event include being cautious about drug and alcohol consumption (mentioned as more proximal to the sexual encounter than the quotations about drinking and drug use included above), discussing HIV with sexual partners before sex, and strategic sexual positioning.
Exercise Caution Around Drug and Alcohol Consumption
With regard to drug use and drinking immediately prior to and during the sexual event, 5 (17%) participants mentioned explicit, intentional strategies to avoid being “too high” or “too drunk” before a sexual encounter. Some men suggested that they restrict their drinking and drug use to stay safe.
When asked about how drinking might affect his condom use, one participant said, “I’m a control freak so I never get too intoxicated to where I don’t know what’s going on.” (P012, age 29, heavy alcohol user.) Another had this to say: “That’s pretty much it. That’s my only boundaries – no crazy drugs and always condom.” (P008, age 27, powder cocaine and heavy alcohol user.) Similarly, a third said:
In my life, drugs are just like kind of more social, like going out. And then for sex I usually don’t have drugs and sex. But if I do, it would probably just be something like ‘G’ [GHB], where it kind of just makes me feel a little bit more like sexual (P010, age 35, GHB, powder cocaine, and heavy alcohol user.)
Similarly, another participant, when asked if values play a role in decisions about sex, condoms or drug use, said simply “no sex with drugs.” (P011, age 26, ecstasy, GHB, ketamine, marijuana, poppers, powder cocaine and user.)
Discuss HIV Status Immediately Before Sex
Ten (34%) participants explicitly mentioned discussing their partners’ HIV status immediately before having sex. This is another behavior that is not necessarily an uncommon prevention strategy, however, the proximity of disclosure to the sexual event is not well understood. These men said they intentionally discuss their partner’s HIV status, whether there is a condom involved or not, immediately before having sex if they haven’t learned their partner’s status in advance. This participant explained this type of discussion this way: “I like to be up front and I always like to put those sort of things out there. I like to discuss those sort of things when I’m having sex with somebody” (P011, age 26, ecstasy, GHB, ketamine, marijuana, poppers, powder cocaine and user.) When the interviewer asked when he usually discusses HIV, the participant replied, “When we’re about to have sex. You know, I like to sort of like clear the air before we have sex.” The interviewer then asked what he usually says to his partner, to which he replied, “What’s your status? You know. And when’s the last time you were tested. And you know, go from there.”
Engage in Strategic Sexual Positioning
Another theme that arose during the sexual encounter is that of intentional, adaptive sexual positioning strategies. Six (21%) men mentioned “topping” causal partners as part of strategies to stay HIV negative. As noted by one participant upon being asked about whether he had any rules for himself for staying healthy and avoiding HIV: Yeah, just the things I talked about. Getting screened, getting tested, just being a top, kind of minimize your risk. Yeah.”
(P010, age 35, GHB, powder cocaine, and heavy alcohol user.)
Another participant put it this way: “…I always just top anyways, if they’re positive it’s the same position. Yeah. Just because as a top it’s like it’s less of a risk for me to catch HIV.” And, when asked why he thinks he has stayed HIV-negative, he said:
Again, I don’t bottom, that’s just rule number one. Number two is if you do bottom, do it with a condom. That’s pretty much my biggest fear is just doing anything like that without a condom or shooting up behind somebody, those are the main two ways a guy’s going to get it—straight guy’s going to get it or the top is going to get it. (P019, age 34, marijuana and heavy alcohol user.)
Always Use Condoms
Although only three of the men actually always used condoms with every partner, more common was for men to always use condoms with certain partners. Although using condoms is certainly not an uncommon way to prevent HIV, we sought to understand how some many manage to always use them, or always use them with some partners, and if whether they might have strategies for doing so. In the following examples, the interviewer explored some of the ways that these men managed to “always” use them.
I mean, there’re those moments of course, where you’re like, you know, while we’re, you know, foreplay. It would be just so simple but it’s gotten to the point for me, it’s like a sigh of relief. I feel—it’s kind of funny but, I feel so much better and there’s like a sense of relief. I perform better knowing that there is one thing that I have less to worry about, and so, condom, great. That means we’re going to have some fun because there’s no stress in my head about, okay. (P009, age 34, marijuana, powder cocaine and heavy alcohol user.)
Another said this: “I’m not going to bring anything out. So my desire to not want to bring anything home is stronger than the desire to want to not use condoms.” (P019, age 34, marijuana and heavy alcohol user.)
Discussion
We conducted in-depth qualitative interviews to discover uncommon behaviors (and common behaviors with uncommon variations) that could be helping young, Black MSM who are at increased risk for HIV from substance use stay safe from acquiring HIV. Themes that emerged from our qualitative interviews fell along a continuum of successive steps leading to a sexual encounter, from behaviors men engage in while looking for partners, selecting partners, preparing for a sexual encounter, and immediately prior to and during the sexual encounter. Of note, some of the behaviors appear to be intentional strategies for avoiding HIV, while others do not. Further, although we report all of the behaviors that emerged as themes because we believe they contribute to our understanding of ways that men might be avoiding risk (or ways men believe they are avoiding risk), some personal preferences stated by the men may be perceived as stigmatizing and clearly are not applicable to future interventions.
The most salient theme mentioned in the context of “looking for sexual partners” was the avoidance of bathhouses. Although this might be thought of as a standard and common HIV prevention strategy, the reasons for avoiding bathhouses are more nuanced. Almost half of the men (41%) said they never look for sexual partners in bathhouses. For some men, this is a strategy for avoiding HIV, while for others it is more a matter of personal preference. Although avoidance of bathhouses could reflect a typology of MSM who may be at lower risk for HIV in general (i.e., perhaps men who avoid bathhouses also have fewer sexual partners, use condoms more often and do not engage in sex while using drugs), our findings suggest, at a minimum, that there may be strategic decision-making about where to look for partners and that this may be a first attempt (conscious or not, effective or not) at minimizing risk. Although the research on associations between venue and risk-taking is limited, some research suggests greater risk behaviors among men who meet partners outdoors or a public place and that alcohol use prior to sexual encounters is highest among men who meet at bathhouses [34, 35]. Of note, several men avoid bathhouses despite having friends that frequent them and despite their knowledge that condoms and lubricant may be offered at the venues.
This theorized process of incrementally minimizing risk through successive adaptive decisions, continues in the “selecting sex partners” period. When selecting sex partners, men said they tend to actively avoid men they perceive to be HIV positive, inject drugs, or those who appear to be very feminine or flamboyant. These are examples of the persistence of stigma in personal preferences, but nevertheless are important to understand in the context of men’s beliefs about how they are avoiding HIV. Interestingly, even those who report avoiding people who use drugs do engage in drug use and other risk behaviors when they believe they’ve minimized harm. Further several men describe strategic procedures for screening men to determine their HIV status. Screening behaviors include serosorting on telephone applications (“apps”) and online dating sites where men have indicated they are HIV positive, talking or texting at length before meeting up and including a discussion of HIV and other STIs, and asking to see HIV testing paperwork. Serosorting actually has been found in prior studies to be fairly common among HIV negative MSM across races and ethnicities [36,37,38]. Further study is needed to distill who uses serosorting, whether it actually offers protection from contracting HIV, and whether other protective behaviors are used in combination with serosorting.
With regard to some men’s avoidance of men who are feminine or flamboyant, it is unclear whether these selection criteria are consciously related to HIV avoidance, whether they are rationalizations used to defend against internalized homophobia or homonegativity, or whether they are simply a personal preference having nothing to do with either, albeit stigmatizing. Conscious or not, avoiding feminine partners implicitly may allow these men to avoid partners who may be more likely to practice frequent receptive anal intercourse, which is a known risk factor for HIV infection [8, 39, 40]. Indeed, some studies have in fact found that (self-perceived) femininity is associated with MSM self-labeling as a “bottom” or preferring to practice receptive anal intercourse [41,42,43]. A personal preference such as this would of course have limited utility in an intervention, but is, nonetheless, important to understanding how some men might be reducing their risk pool.
While actively “planning to meet up with a partner” for sex, men may plan in advance to protect themselves by “always” or “mostly” carrying condoms with them and/or by planning their drinking and drug use. It was not clear from our interviews whether the men have strategies for remembering to carry condoms, but advance planning could determine whether or not a condom is used during the sexual event. As reported by Tucker et al. (2014), the use of condoms during a sexual event is contingent upon three factors at different time points leading to the sexual event: (1) deciding prior to a sexual event about whether to use condoms; (2) whether a condom is available at the sexual event; and (3) whether a condom was used at the event. In that study, condom use was more likely among those who decided ahead of time to use a condom, but less likely, regardless of advanced planning about whether to use a condom, when hard drugs were used prior to sex [44].
Of note, in some cases planning behaviors around drinking and drug use among men in this study seemed to be a conscious effort to avoid factors that could interfere with condom use, while in other cases the behaviors seem to be more a desire to avoid social danger associated with losing control. Although we did not discuss anxiety or tendency to avoid risk during the interviews, it is possible that there could be higher risk avoidance among men who remain HIV negative and who engage in adaptive strategies. Indeed, anxiety has been linked to risk aversion and taking extreme safety precautions [45].
Planning behaviors, if they do serve to increase condom use, suggest that men who typically engage in drug use and drinking may be able to consciously modulate their condom use and drinking/drug use and perhaps their own impulsivity [46]. Of course, this precludes spontaneous sexual encounters that may occur as a function of excessive drug use and drinking, or sudden lust or love, but these preliminary findings highlight that drug users and heavy drinkers may be able to manage their behaviors well in advance of a sexual encounter. In fact, as some of the men mentioned, they only drink heavily, use drugs or go out with certain trusted people so they can rely on their social networks to help keep them safe if they do get too high or drunk. This could indicate that norms around drug use and drinking embedded in social networks could serve as protective strategies.
Although not fully explored in this study, dependable social networks could also allow for exposure to positive, pro-social experiences that reinforce the value of the self. This could, in turn, reduce likelihood of a decision sequence that seeks a high reinforcement value behavior (such as UAI) with unknown/new partners. Indeed, there is an underlying theme throughout many of the comments that indicates that men’s values about their own health are reinforced by getting to know their sexual partners, their stories, their values, and, ultimately, their likelihood of having HIV. These values, perhaps embedded within social networks, could serve to balance the decision to have impulse-driven UAI and more thoughtful, meaningful sex that is consistent with personal and social network values.
As noted throughout this article, some of these findings are not unique as strategies for avoiding HIV, since there have been many mass media campaigns that promote condom use, HIV testing, and disclosure of HIV status and many of these behaviors are known and commonly used as prevention strategies among MSM; however, in-depth knowledge about who engages in these behaviors, to what extent, in what combinations, and how men otherwise at very high risk for HIV manage to do so, are limited. Further, mass media campaigns tend not to include information about planning in advance to use condoms or about strategies for managing drinking and drug use and little work has been done to uncover more subtle strategies as well as motivations and symbiotic goals that may drive the larger strategies.
One of the key messages from this study is that among men at high-risk for HIV who remain HIV negative (i.e., “positive deviants”), there may be successive decision-making across a timeline to a sexual event that reduces risk, even if a condom is not used. Some decisions are based on well-known HIV-prevention messages and are intentional, while others are based on personal preferences and values and possibly personality types. In combination, some of these decisions can be viewed adaptive risk reduction behaviors that facilitate avoidance of HIV, and some may have applicability to risk reduction interventions.
Conclusions
This study used a positive deviance framework to study whether men who are otherwise at very high risk for HIV—young Black MSM who use drugs and/or drink in risky amounts—have managed to avoid infection by engaging in intentional or unintentional risk reduction behaviors. Findings suggest that men who do not contract HIV may be engaging in risk reduction strategies before and during sexual events that could lead to increased condom use, avoidance or delay of a risky sexual event (such as when the men discussed not getting so high or drunk they might end up in a situation in which they do not use a condom), or reduction of their risk pool (i.e., reducing the number or type of partners likely to have HIV through screening and pre-selection). Although condom use (and PrEP) may be the ultimate prevention goal, most men in the study admittedly do not use condoms consistently and most were not amenable to PrEP. The findings suggest there may be additional strategies that can contribute to risk reduction. This study was the first phase of a larger study to develop an adaptive strategies questionnaire. The questionnaire will measure the extent to which adaptive strategies are used, who uses them, in what combinations they are used, and whether they indeed serve to help young, Black MSM avoid contracting HIV.
A positive deviance framework in which a grassroots approach is used to discover specific behaviors by members of a high-risk community who successfully avoid a disease (“positive deviants”) when many peers are not able to do so may ultimately serve to inform a community-based, peer-led risk reduction intervention. Local, peer-led interventions are the ultimate goal of positive deviance, where members of an at-risk community share their own successful strategies for avoiding a disease with others who face the same risk. Although peer-led public health campaigns to use condoms and get tested are not novel and have become embedded in MSM communities, a local approach that seeks to uncover uncommon sometimes more subtle behaviors in which HIV-negative men are engaged, the motivations behind them, and how these could protect those at high risk for HIV, offers an innovative approach to leveraging existing prevention messages and tailoring interventions. Uncovering the more subtle strategies and motivations is the first step in the positive deviance approach and was done in this study by engaging men in in-depth discussions not only of known strategies for avoiding HIV, but of how they manage to sustain behaviors that are generally challenging for most men to sustain over time, and of behaviors that may not at face value seem protective, but when taken together could serve to lower exposure to risk.
Although the development of an adaptive strategies questionnaire to determine the extent of engagement in adaptive strategies and the relationship of adaptive strategies to remaining HIV negative over time was the end-goal of our study, we also see applicability of our qualitative findings to the development of a risk reduction intervention. An example of such an intervention is a peer-led, individual “discovery” interview that assesses an individual’s personal “positive deviance” strategies. A tailored intervention based on these, when combined with known strategies such as condom use and PrEP, could serve to lower HIV risk. Our study also illuminates the persistence of stigmatized beliefs about others and myths about HIV prevention strategies, both of which also could be addressed in individualized interventions.
Findings must be interpreted with caution, as they are the result of a small number of qualitative interviews with participants who were not randomly sampled. Larger studies of Black MSM that attempt to approximate a representative sample have recruited men who are lower-income and less well-educated than the men in this sample [47]. Nevertheless, the findings are a first step in a new approach to preventing the further spread of HIV among young Black MSM. The adaptive strategies questionnaire developed as part of the larger study also will contribute to generalizability of these findings.
References
Sullivan PS, Hamouda O, Delpech V, Geduld JE, Prejean J, Semaille C, et al. Reemergence of the HIV epidemic among men who have sex with men in North America, Western Europe, and Australia, 1996–2005. Ann Epidemiol. 2009;19(6):423–31.
Prejean J, Song R, Hernandez A, Ziebell R, Green T, Walker F, et al. Estimated HIV incidence in the United States, 2006–2009. PLoS ONE. 2011;6(8):e17502.
Binson D, Michaels S, Stall R, et al. Prevalence and social distribution of men who have sex with men: United States and its urban centers. J Sex Res. 1995;32:245–54.
Centers for Disease Control and Prevention. Prevalence and awareness of HIV infection among men who have sex with men—21 cities. Morb Mortal Wkly Rep. 2010;59:1201–7.
Centers for Disease Control and Prevention. Estimated HIV incidence among adults and adolescents in the United States, 2007–2010. HIV surveillance supplemental report 2012. 2012;17(4).
Balaji A, Bowles K, Le B, Paz-Bailey G, Oster A, editors. High HIV incidence and prevalence and associated factors among young MSM in 21 cities: US, 2008. 9th conference on retroviruses and opportunistic infections; 2012 March 5-8; Seattle.
Los Angeles County Department of Health Division if HIV and STD Programs. 2014 Annual HIV/STD Surveillance Report 2014.
Koblin BA, Mayer KH, Eshleman SH, Wang L, Mannheimer S, del Rio C, et al. Correlates of HIV acquisition in a cohort of Black men who have sex with men in the United States: HIV prevention trials network (HPTN) 061. PLoS ONE. 2013;8(7):e70413.
Sullivan PS, Carballo-Dieguez A, Coates T, Goodreau SM, McGowan I, Sanders EJ, et al. Successes and challenges of HIV prevention in men who have sex with men. Lancet. 2012;380(9839):388–99.
Saberi P, Gamarel KE, Neilands TB, Comfort M, Sheon N, Darbes LA, et al. Ambiguity, ambivalence, and apprehensions of taking HIV-1 pre-exposure prophylaxis among male couples in San Francisco: a mixed methods study. PLoS ONE. 2012;7(11):e50061.
Bauermeister JA, Meanley S, Pingel E, Soler JH, Harper GW. PrEP awareness and perceived barriers among single young men who have sex with men. Curr HIV Res. 2013;11(7):520–7.
Eaton LA, Driffin DD, Bauermeister J, Smith H, Conway-Washington C. Minimal awareness and stalled uptake of pre-exposure prophylaxis (PrEP) among at risk, HIV-negative, black men who have sex with men. AIDS Patient Care STDS. 2015.
Wray JD. Editorial: can we learn from successful mothers? J Trop Pediatr Environ Child Health. 1972;18(4):279.
Marsh DR, Schroeder DG, Dearden KA, Sternin J, Sternin M. The power of positive deviance. BMJ. 2004;329(7475):1177–9.
Friedman SR, Mateu-Gelabert P, Sandoval M, Hagan H, Des Jarlais DC. Positive deviance control-case life history: a method to develop grounded hypotheses about successful long-term avoidance of infection. BMC Public Health. 2008;8:94.
Gwadz MV, Clatts MC, Yi H, Leonard NR, Goldsamt L, Lankenau S. Resilience among young men who have sex with men in New York City. Sex Res Soc Policy. 2006;3(1):13.
Wyatt GE. Enhancing cultural and contextual intervention strategies to reduce HIV/AIDS among African Americans. Am J Public Health. 2009;99(11):1941–5.
Herrick AL, Lim SH, Wei C, Smith H, Guadamuz T, Friedman MS, et al. Resilience as an untapped resource in behavioral intervention design for gay men. AIDS Behav. 2011;15(Suppl 1):S25–9.
Williams J, Wyatt G. The four Cs of HIV prevention with African Americans: crisis, condoms, culture and community. HIV/AIDS Rep. 2010;7:185–93.
Greenwood GL, Paul JP, Pollack LM, Binson D, Catania JA, Chang J, et al. Tobacco use and cessation among a household-based sample of US urban men who have sex with men. Am J Public Health. 2005;95(1):145–51.
Lim SH, Ostrow D, Stall R, Chmiel J, Herrick A, Shoptaw S, et al. Changes in stimulant drug use over time in the MACS: evidence for resilience against stimulant drug use among men who have sex with men. AIDS Behav. 2010;16:151–8.
Friedman SR, Sandoval M, Mateu-Gelabert P, Meylakhs P, Des Jarlais DC. Symbiotic goals and the prevention of blood-borne viruses among injection drug users. Subst Use Misuse. 2011;46(2–3):307–15.
Save the Children Federation. Promising behaviors to mitigate HIV/AIDS in Viet Nam identified through the positive deviance approach In: Save the Children Federation, editor. USA, Westport, CT2002.
Vosburgh HW, Mansergh G, Sullivan PS, Purcell DW. A review of the literature on event-level substance use and sexual risk behavior among men who have sex with men. AIDS Behav. 2012;16(6):1394–410.
Boone MR, Cook SH, Wilson P. Substance use and sexual risk behavior in HIV-positive men who have sex with men: an episode-level analysis. AIDS Behav. 2012;17:1883–7.
Colfax G, Vittinghoff E, Husnik MJ, Mckirnan D, Buchbinder S, Koblin B, et al. Substance use and sexual risk: a participant-and episode-level analysis among a cohort of men who have sex with men. Am J Epidemiol. 2004;159:1002–12.
Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol use disorders identification test. Arch Intern Med. 1998;158(16):1789–95.
Spradley JP. The ethnographic interview. New York: Hold Rinehart and Winston; 1979.
Ryan G, Bernard H. Techniques to identify themes. Field Methods. 2003;15(1):85–109.
The Positive Deviance Initiative. Basic Field Guide to the Positive Deviance Approach,. In: Tufts University Friedman School of Nutrition Science and Policy, editor. Positive Deviance Initative 2010.
Denzin N, Lincoln Y. Handbook of qualitative research. 4th ed. Thousand Oaks, CA: Sage Publications; 2011.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Cohen J. Coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20(1):37–46.
Grov C, Hirshfield S, Remien RH, Humberstone M, Chiasson MA. Exploring the venue’s role in risky sexual behavior among gay and bisexual men: an event-level analysis from a national online survey in the U.S. Arch Sex Behav. 2013;42(2):291–302.
Grov C. HIV risk and substance use in men who have sex with men surveyed in bathhouses, bars/clubs, and on Craigslist.org: venue of recruitment matters. AIDS Behav. 2012;16(4):807–17.
Wei C, Raymond HF, Guadamuz TE, Stall R, Colfax GN, Snowden JM, et al. Racial/ethnic differences in seroadaptive and serodisclosure behaviors among men who have sex with men. AIDS Behav. 2010;15(1):22–9.
Eaton LA, Kalichman SC, Cain DN, Cherry C, Stearns HL, Amaral CM, et al. Serosorting sexual partners and risk for HIV among men who have sex with men. Am J Prev Med. 2007;33(6):479–85.
Kurtz SP, Buttram ME, Surratt HL, Stall RD. Resilience, syndemic factors, and serosorting behaviors among HIV-positive and HIV-negative substance-using msm. AIDS Educ Prev. 2012;24(3):193–205.
Coates RA, Calzavara LM, Read SE, Fanning MM, Shepherd FA, Klein MH, et al. Risk factors for HIV infection in male sexual contacts of men with AIDS or an AIDS-related condition. Am J Epidemiol. 1988;128(4):729–39.
Schechter MT, Boyko WJ, Douglas B, Willoughby B, McLeod A, Maynard M, et al. The Vancouver Lymphadenopathy-AIDS Study: 6. HIV seroconversion in a cohort of homosexual men. CMAJ. 1986;135(12):1355–60.
Jeffries WL, Zsembik BA, Peek CW, Uphold CR. A longitudinal analysis of sociodemographic and health correlates of sexual health among HIV-infected men in the USA. Sexual Health. 2009;6(4):285–92.
Carballo-Dieguez A, Bauermeister J. “Barebacking”: intentional condomless anal sex in HIV-risk contexts. Reasons for and against it. J Homosex. 2004;47(1):1–16.
Agronick G, O’Donnell L, Stueve A, Doval AS, Duran R, Vargo S. Sexual behaviors and risks among bisexually- and gay-identified young Latino men. AIDS Behav. 2004;8(2):185–97.
Tucker JS, Ober A, Ryan G, Golinelli D, Ewing B, Wenzel SL. To use or not to use: a stage-based approach to understanding condom use among homeless youth. AIDS Care. 2014;26(5):567–73.
Lorian CN, Grisham JR. Clinical implications of risk aversion: an online study of risk-avoidance and treatment utilization in pathological anxiety. J Anxiety Disord. 2011;25(6):840–8.
Jones J, Sullivan PS. Impulsivity as a risk factor for HIV transmission in men who have sex with men: a delay discounting approach. J Homosex. 2015;62(5):588–603.
Morgan E, Skaathun B, Michaels S, Young L, Khanna A, Friedman SR, et al. Marijuana use as a sex-drug is associated with HIV risk among black MSM and their network. AIDS Behav. 2016;20(3):600–7.
Acknowledgements
Primary support for this study was provided by National Institute on Drug Abuse Grant 5 03 DA035689-02. We acknowledge the Center for HIV Identification, Prevention and Treatment Services, University of California Los Angeles (P30 MH058107), and the UCLA Vine Street Clinic for their support and dedication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Funding for this study was providing by NIDA grant 5 R03 DA035689-02.
Ethical Approval
All procedures were in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards and were in accordance with the ethical standards of and approved by the RAND Human Subjects Protection Committee.
Rights and permissions
About this article
Cite this article
Ober, A.J., Dangerfield, D.T., Shoptaw, S. et al. Using a “Positive Deviance” Framework to Discover Adaptive Risk Reduction Behaviors Among High-Risk HIV Negative Black Men Who Have Sex with Men. AIDS Behav 22, 1699–1712 (2018). https://doi.org/10.1007/s10461-017-1790-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-017-1790-x