Abstract
In Vietnam’s concentrated HIV epidemic, female sex workers (FSWs) are at increased risk for acquiring and transmitting HIV, largely through their male clients. A high proportion of males in Vietnam report being clients of FSWs. Studying HIV-related risk factors and prevalence among male clients is important, particularly given the potential for male clients to be a ‘bridge’ of HIV transmission to the more general population or to sex workers. Time-location sampling was used to identify FSW in Hanoi and Ho Chi Minh City, Vietnam’s largest cities, in 2013–2014. Recruited FSWs were asked to refer one male client to the study. Demographic and risk behavior data were collected from FSWs and male clients by administered questionnaires. Biologic specimens collected from male clients were tested for HIV and opiates. Sampling weights, calculated based on the FSWs probability of being selected for enrolment, were applied to prevalence estimates for both FSWs and male clients. Logistic regression models were developed to obtain odds ratios for HIV infection among male clients. A total of 804 male clients were enrolled. Overall, HIV prevalence among male clients was 10.2%; HIV prevalence was 20.7% (95% confidence interval (CI) 15.0–27.9%) among those reporting a history of illegal drug use and 32.4% (95% CI 20.2–47.7%) among those with opioids detected in urine. HIV prevalence among male clients did not differ across ‘bridging’ categories defined by condom use with FSWs and regular partners over the previous 6 months. HIV among male clients was associated with a reported history of illegal drug use (OR 3.76; 95% CI 1.87–7.56), current opioid use (OR 2.55; 95% CI 1.02–6.36), and being referred by an FSW who self-reported as HIV-positive (OR 5.37; 95% CI 1.46–19.75). Self-reported HIV prevalence among enrolled FSWs was 2.8%. Based on HIV test results of male clients and self-reported status from FSWs, an estimated 12.1% of male client-FSW pairs were sero-discordant. These results indicate high HIV prevalence among male clients of FSWs, particularly among those with a history of drug use. Programs to expand HIV testing, drug-use harm reduction, and HIV treatment for HIV-infected male clients of FSWs should be considered as key interventions for controlling the HIV epidemic in Vietnam.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Vietnam’s concentrated HIV/AIDS epidemic is driven primarily by key populations including people who inject drugs (PWID), female sex workers (FSWs), and men who have sex with men (MSM); as of 2013, there were an estimated 250,000 people living with HIV in Vietnam [1]. The extent to which these key populations overlap with other populations (e.g., general population) in terms of HIV-related risk behaviors is important to understanding the potential for the current and future HIV burden, transmission, and response. While the majority of PLHIV in Vietnam are estimated to be male, HIV/AIDS case reporting and epidemiologic modelling indicates a significant decline in the ratio of male to female PLHIV since 1998. These same models report that in 2010, an estimated 31% of new infections in Vietnam were male clients of female sex workers and a further 24% were low-risk women which includes sexual partners of these men [1]. Data from Vietnam indicate that large proportions of sexually active Vietnamese men have engaged in sexual relations with FSWs. A survey among young (aged 18–29 years) men in Hai Phong province in 2005 reported that 31% of sexually active men had visited an FSW in their lifetime; [2] in a survey from 2013 of male injecting drug users across eight provinces, up to 59% reported having sex with a FSW in past 12 months [3]. These clients of FSWs are likely to also have regular sex partners and could therefore act as a bridge for HIV transmission into the general population.
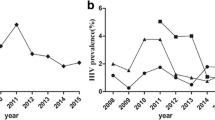
There are estimated to be between 30,000 and 100,000 FSWs in Vietnam with larger concentrations in urban settings [1]. While HIV surveillance among FSWs overall indicates steady or decreasing prevalence, there are regions of the country that continue to report high or increasing HIV prevalence (unpublished Vietnam Ministry of Health HIV sentinel surveillance reports). From the 2013 Integrated Behavioral and Biologic Survey (IBBS), HIV prevalence among venue-based FSW ranged between 2.4 and 11.0% by province; among street-based FSW, HIV prevalence ranged from 7.1 to 31.9%. Despite reports of condom use of greater than 75% with ‘one-time clients’, HIV transmission between FSW and their clients are potentially high with up to 25% of male clients having experienced condom slippage or breakage with a FSW potentially limiting their effectiveness [4]. Ho Chi Minh City (HCMC) (population: 7.8 million), located in the southeast region, and Hanoi (population: 6.5 million), located in the northern Red River Delta region, are the two largest cities in Vietnam [4]. In a survey among ‘establishments’ (e.g., bars, restaurants), an estimated 34.5 and 41.2% of males in HCMC and Hanoi respectively, reported having had sex with a commercial sex worker in the past 3 months [5]. While population size estimations vary, there are believed to be 3500 (range 1750–5300) and 20,000 (range 10–30,000) active FSWs in HCMC and Hanoi, respectively as recently as 2012 [6]. The 2013 IBBS reported that the HIV prevalence among street-based FSW was 13.1 and 10.4% in HCMC and Hanoi respectively. Among venue-based FSW, HIV prevalence was 9.0% in HCMC and 13.9% in Hanoi. In a trend analysis of surveys in 2005, 2009, and 2013, HIV prevalence among FSW in HCMC was statistically stable; in Hanoi, prevalence increased significantly among venue-based FSW but decreased significantly among street-based FSWs [3].
Male clients of FSWs serve as an important potential bridging population for HIV transmission to the general population. Understanding their risk behaviors, access to services, and HIV burden are essential towards ‘knowing ones HIV/AIDS epidemic’ and progress towards achieving local and international HIV program and impact goals [7]. To date there have been limited direct estimates of HIV prevalence and associated behaviors among male clients of FSWs in Vietnam. Surveys indicate that the HIV prevalence among male clients of FSWs ranges between 1 and 10% in the region [8,9,10]. Findings from a study in Bangkok, Thailand reported that 20% (95% CI 12.1–31.2%) of male clients were infected with HIV, and similar prevalence was found among FSW with whom they had sex. Almost 25% of these male clients were married and more than 85% reported more than one sexual partner in the past month [11]. Findings from Yunnan, China, on the border with Vietnam, showed HIV prevalence among male clients to be 9.2% and to be most associated with injecting drug use and co-infection with herpes simplex virus type 2 (HSV-2) [10]. A study in Hai Phong, Vietnam, which classified potential clients of FSW to be a bridge in transmitting HIV to lower-risk partners based on their reported condom use, estimated that HIV prevalence was highest among those male clients classified as ‘active bridgers’ (6.3%), followed by the ‘unlikely bridgers’ (4.8%) and ‘potential bridgers’ (4.1%) [12].
There are significant challenges to targeting male clients for surveillance and programming. Despite data that indicate extramarital sexual relationships are common in Vietnam, they are generally considered to be outside of social norms and are therefore hidden behaviors making subject recruitment difficult and potentially biased in their results [2, 13,14,15]. The objectives of this study are to estimate the HIV prevalence and associated risk factors among male clients of female sex workers in HCMC and Hanoi, the two largest cities in Vietnam, using innovative methodologies for recruitment and analysis that utilizes FSWs to recruit and to refer their male clients to this survey.
Methods
Between March 2013 and 2014, separate cross-sectional surveys were conducted in HCMC and Hanoi among FSWs and the male clients that they referred. FSWs were defined as females, aged 18 years and older who self-reported to have exchanged sex for money or material goods in the past month and who were willing to refer their male clients for recruitment into this survey. FSWs were further classified by where they primarily solicited for male clients; FSWs who engaged clients in fixed locations (e.g., bars, karaoke halls, hotels) were classified as ‘venue-based’ FSW, and FSWs who solicited clients from open street locations were classified as ‘street-based’ FSW. Male clients were defined as males, referred by a recruited FSW, aged 18 years and older, who self-reported to have exchanged money or material goods with at least one FSW in the past month.
HIV prevalence among the male clients was the being the primary outcome of interest for this survey; a sample size of 400 male clients of FSWs in each city was calculated based on previous prevalence estimates (6.25%) with ±5% precision and a design effect of 2.0 to account for the potential correlation of HIV prevalence with sampling location [12].
Time-location sampling (TLS) was used to recruit FSWs in both provinces [16]. Briefly, TLS approximates probability sampling of a select population by a random selection of locations (e.g., street, venue-based) from the ‘mapped universe’ or sampling frame of times and locations where the population can be found. For this survey, a sampling frame of these venue-day-time (VDT) locations was created, using trained field staff, through formative mapping of known locations frequented by FSWs and their clients. VDTs were then chosen at random for inclusion in the survey. Once selected, locations were visited by study teams to recruit potential enrollees (i.e., FSWs). At each location, the study team recorded the total number of FSWs, how many were approached and enrolled, and how many refused enrollment. This information was used to calculate the probability of being enrolled based on the probability of a location being selected divided by the probability of an individual being enrolled at a selected location. The inverse of this probability was applied as the survey sampling weight to both the enrolled FSW and their referred male client in the analysis as has been done in other similar surveys of male clients [11]. Refusals rates were determined based on the number of FSWs that were approach for enrolment but refused to accept an invitation coupon summed with those that took a coupon but did not come to a study site divided by the total FSWs approached to participate.
FSWs who agreed to participate in the survey were briefed on the study objectives, eligibility criteria, and methods and were given a single coupon with two sections that could be easily separated; each section had the same random unique number and location information for the nearby study center. One section was to be given by the FSW to a male client whom she would like to refer to the study center, and the second section was for the FSW to retain for her own enrolment. FSWs and their referred male client(s) were not required to visit the study center at the same time; male clients presenting with a study coupon could be enrolled if the referring FSW did not enroll. Upon arrival at a study center, the FSW or the male client submitted their study coupon and were reassessed for eligibility for inclusion in the study in a private room to ensure privacy and confidentiality. Written, informed consent was obtained after a summary of the survey and its objectives were provided. Trained interviewers, associated and supported by the study, confidentially administered the appropriate questionnaire to the FSW or the referred male client. The questionnaire was developed and validated through a series of steps including: literature review for previous surveys, pilot interviews with male clients in Hanoi and HCMC, and focus group discussions with key stakeholders such as HIV prevention and surveillance experts. The questionnaire collected self-reported information on key demographic measures, sexual history and risk behaviors, illegal drug use history, risk behaviors, self-reported HIV status (FSW only), and exposure to key harm-reduction interventions. HIV testing was not conducted among FSWs because at least two other surveys among FSWs in the same provinces (Vietnam sentinel surveillance; 2013 IBBS) were conducting HIV testing among FSWs; investigators for this survey were concerned that biologic testing might, therefore, decrease survey participation.
After completing the questionnaire and receiving pre-testing counseling, biologic specimens were collected from male clients for HIV and opiate testing. HIV test results were provided on-site to clients along with post-test counseling and referral to care and treatment services, as appropriate.
Laboratory
Male clients provided 5 ml of venous blood for HIV testing and 20 ml of urine for opiate testing. HIV infection was determined following Vietnam’s national testing guidelines of an initial rapid test (Abbot, Japan) and confirmation of positive results by EIA-Green HIV ½ (Bio-Rad, US) and Murex ½ (Murex Biotech, UK) at the Vietnam National Institute of Hygiene and Epidemiology (NIHE). Urinalysis was conducted at the data collection point to determine the presence of opiates using the SureStep OPI One Step Opiate Test Device and the SureStep AMP 300 One Step Amphetamine Test Device kits.
Statistical Analysis
Weighted frequencies and proportions were calculated for categorical demographic and self-reported behavioral variables by province; and mean and medians were calculated for continuous variables and by province. Prevalence estimates for HIV among male clients and their referring FSW with 95% confidence intervals (95% CI) were calculated individually and as a male client-FSW pair to estimate the proportion of HIV concordance or discordance in the enrolled “couples”. Male clients were further classified by their relative likelihood of being a ‘bridging population’ in the sexual transmission of HIV between high-risk populations (i.e., FSWs) and non-commercial sex partners (i.e., wife, regular sexual partner, one-time partner) [12]. Male clients were classified as ‘high-risk bridgers’ if they reported inconsistent condom use (i.e., sometimes or never use condom when having sex) with both FSWs and any non-commercial sex partners in the previous 6 months; ‘potential bridgers’ if they reported consistent condom use (i.e., always use condom when having sex) with FSWs and inconsistent condom use with non-commercial partners in the previous 6 months; and ‘low-risk bridgers’ if they reported consistent condom use with FSWs and non-commercial partners in the previous 6 months.
Comparison of categorical data by provinces was done using the Chi square test or Fisher’s exact test where appropriate. An adjusted Wald test was used to compare mean values between Hanoi and Ho Chi Minh City. The Mann–Whitney test was used to compare median values for different groups. The analysis was completed using STATA (v.12.0) [17]. The above-described individual probability ‘survey’ weights were calculated for each FSW and also applied to their referred male client (as described above, [11]).
For univariate and multivariate risk factor analysis, survey weighted odds ratios (OR) and 95% CI were calculated by logistic regression with HIV status as the outcome variable. All independent variables indicating an association with HIV status (p ≤ 0.20) in the univariate analysis were entered into a multivariate logistic regression model using backward step-wise selection and the Wald test after estimation to identify the most parsimonious model.
The study protocol was reviewed and approved by the Hanoi School of Public Health (Vietnam) Ethics Review Board and the Internal Review Board of the U.S. Centers for Disease Control and Prevention.
The survey was implemented by Partners in Health Research with technical and financial support from the US Centers for Disease Control and Prevention.
Results
Demographic and Risk Behaviors
A total of 804 male clients (52% from HCMC) and FSWs (n = 785) were enrolled in this survey from a total of 126 VDTs (53 in Hanoi, 73 in HCMC); enrollment included 784 FSW-client pairs enrolled and 20 male clients whose referring FSW did not enroll. An estimated 44.1 and 27.1% of FSWs in Hanoi and HCMC, respectively, refused to participate in the survey.
The basic demographic and risk behavior information in Hanoi, HCMC, and overall is presented in Table 1. The mean age was 34.4 (33.3–35.4) years for the male clients and 31.4 (30.3–32.5) for the FSWs. Less than 50% of the male clients had an education beyond the ninth grade. The majority reported to be single with 28% (23.3–32.7%) reporting being married or co-habitating with a woman. The median (IQR) duration that male clients reported knowing the referring FSW was 2 (1–5) months, indicating some level of previous interaction prior to this encounter and referral. The proportion of male clients who used condoms—at last sexual encounter and consistently over the past 6 months—was higher with FSWs than with non-commercial (e.g., wife, girlfriend, one-time sex) partners. The majority of male clients (83.5%; 95% CI 79.7–87.4%) reported using a condom the last time they had sex with a FSW; a smaller proportion (66.8%; 95% CI 61.3–72.4%) reported using condoms consistently with FSWs over the previous 6 months. An estimated 53.3% (49.0–57.7%) of male clients where classified as a ‘low-risk bridge’ and 18.7% (15.4–22.1%) as a ‘high-risk bridge’. The proportion of ‘high-risk bridge’ male clients was significantly greater in HCMC compared to Hanoi (24.0 vs. 13.1%; p value = 0.004). Overall 84.4% of male clients who reported having sex with their wife reported using a condom with the FSW at last sex, 93.9% of those who did not use a condom with the FSW also reported to not use condom with their wife. Overall, less than half (35.2%) of male clients reported to have ever been tested for HIV and amongst those that had been tested, 52.4% (45.3–59.5%) reported to have been tested more than one year ago. Among female sex workers, 67.9% (63.5–72.2%) reported to have ever been tested for HIV.
An estimated 30.7% (26.0–35.4%) of male clients reportedly having ever used illicit drugs (Table 1); among those, 30% self-reported to have ever injected illegal drugs (data not shown). Overall, an estimated 5% (3.2–6.8%) of male clients had positive urinary test for opiates at the time of the survey. Among the 73 male clients who reported ever having injected drugs, the majority (82.1%; 72.4–91.8) indicated that they had not injected in the past month (data not shown).
The proportion of male clients reporting to have ever injected drugs was higher in Hanoi than HCMC (12.0 vs. 6.0%; p value: 0.034) (Table 1). Among those male clients (n = 19) who responded to the question, ‘Have you ever injected drugs with any FSW you have had sex with’, 36.0% (2.4–70.0%) reported to have done so. There was no statistical difference in the proportion of those who reported ever injecting drugs or those testing positive for opiates, by ‘bridging risk’ category (data not shown).
For FSWs, almost half (46.8%; 40.0–53.6%) reported to be single. Overall, the majority of enrolled FSWs solicit their clients on the ‘street’ (43.5%; 34.3–52.7%) or at a defined ‘venue’ (48.3%; 39.1–57.6%). The majority of FSW (67.9%; 63.5–72.2%) had been previously tested for HIV. A higher proportion of FSWs reported to have ever used illegal drugs in HCMC compared to Hanoi (20.6 vs. 9.1%; p value = 0.003) with a similar proportion reporting to have ever injected illegal drugs across the two provinces.
HIV Results
Of the 804 male clients who tested for HIV, 10.2% (7.7–13.5%) had a positive result with a moderately higher HIV prevalence in Hanoi compared to HCMC (13.2 vs. 7.4%; p value = 0.048) (Fig. 1). HIV prevalence was higher among male clients self-reporting a history of illegal drug use (20.7%; 95% CI 15.0–279.9%) and a history of injection drug use (31.4%; 95% CI 20.2–45.3%). Among those male clients who tested positive for the presence of opiates via urinalysis, HIV prevalence was 32.4% (95% CI 20.2–47.7%). In comparison, HIV prevalence among male clients who reported never using illegal drugs was 5.6% (95% CI 3.7–8.4%). HIV prevalence among male clients categorized as low, potential, or high bridging did not differ significantly (10.2 vs. 9.1% vs. 12.6%; p-value = 0.71) (Fig. 2).
Self-reported HIV prevalence was 2.8% (1.4–4.1%) among FSWs that had ever been tested previously for HIV and was similar in Hanoi and HCMC (2.5 vs. 3.2%; p-value = 0.611) (Fig. 3). Among FSW who reported ever having tested for HIV, 3.4% (1.7–5.1%), by report, were HIV-positive. Almost half (42.0%) of FSWs reported to have been tested at least once in the past 6 months with 1.5% (0.6–4.2%) being HIV-positive and was similar across provinces.
HIV Sero-Concordance Between Male Clients and Referring FSWs
Analysis of HIV status among the male client-FSW pairs indicates that 10.2% of these pairs were male client testing HIV-positive with the referring FSW reporting an HIV-negative status (i.e., sero-discordant); inversely, 1.9% of the couples enrolled were the male client testing HIV-negative and the referring FSW, HIV-positive. Together, these indicate that 12.1% of these pairs are HIV sero-discordant and 87.9% (87% HIV negative-negative, 0.9% HIV positive-positive) were sero-concordant as defined by test results among the male clients and self-reported HIV status from FSWs (see Table 2).
Factors Associated With HIV Status Among Male Clients
In the bivariate analysis (Table 3A), being HIV-positive among male clients was positively associated with being recruited from Hanoi (OR: 1.89), older age (OR 4.05 among those aged ≥30 years compared with those aged 18–24 years), being divorced or separated (OR: 2.16 compared with being single), ever used (OR: 4.39) or injected (OR: 5.15) illicit drugs, testing positive for the presence of opiates (OR: 4.82), not using a condom during last sex with a FSW (OR: 2.11) and being referred by a FSW with a self-reported HIV-positive status (OR: 4.00). Inversely, HIV prevalence was lower among male clients who reported never drinking alcohol (OR: 0.43) or drinking less than once a week (OR: 0.53) compared with those who reported drinking more than once per day.
In the adjusted analysis (Table 3B), having ever using illicit drugs was a key predictor of being HIV-positive (aOR 3.76; 95% CI 1.87–7.56) among male clients. Current drug users, as measured by those testing positive for opiates via urinalysis, were 2.55 times (95% OR 1.02–6.36) more likely to be HIV-positive compared to those who tested negative for opiates. Older male clients (i.e. ≥30 years of age) were 4.91 (95% CI 1.18–20.41) times were more likely to be HIV-positive relative to those male clients aged 18–24 years, and male clients referred by an FSW who self-reported to be HIV-positive where more likely to be HIV-positive (aOR 5.37; 95% CI 1.46–19.75) than those referred by an FSW reporting to be HIV-negative. Not using a condom use at last sex with a FSW continued to be associated with an HIV-positive status (aOR 2.02; 95% CI 1.03–3.98) in the adjusted analysis.
Discussion
Findings from our study indicate a high HIV prevalence among male clients of FSWs—11.1% overall. The HIV prevalence found among our sampled male clients in Hanoi and Ho Chi Minh City are approximately 20 times higher than the corresponding prevalence of the general male population in these locations [1]. In this study, HIV prevalence among male clients was significantly associated with older age of the clients, current or previous illegal drug use, not having used a condom at the last sexual encounter, and the HIV status reported by the referring sex worker. The most significant behavioral factor associated with being HIV-positive among male clients was a reported history of illegal drug use. More specifically, current opiate use, as measured through urinalysis, was positively associated with HIV infection among male clients which is in-line with previous reports that highlight the risk of HIV among PWID in Vietnam [18]. This is important given that 24% of the male clients enrolled reported to have used drugs but were referred by a FSW who reported no previous drug use. While a previous study in Vietnam does indicate that injection drug use among FSW is highly associated with being infected with HIV, our findings indicate that FSWs may also be at increased risk for acquiring HIV from this male client and then subsequent transmission to other clients [19]. The 2013 IBBS in Vietnam estimated that 6.6% of PWID in HCMC and 37.8% of PWID in Hanoi reported to have had sex with a FSW in past 12 months [3]. Together, these data provide some indication of the intersection between FSW, male clients, and injection drug use, supporting previous estimates related to ‘modes of HIV transmission’ in Vietnam that indicate that the vast majority of HIV transmission in Vietnam is attributable to injection drug use behavior, commercial sex work, or transmission from high-risk men to their sexual partners [1, 20].
The strong association between the HIV status of the male client and the self-reported HIV status of the referring FSW indicates that HIV infection among FSWs—in addition to drug use—may be a risk for HIV infection among male clients. Relying on self-reported HIV status among FSWs in our analysis may have under-estimated the true HIV burden among FSWs. In fact, the self-reported HIV prevalence in this study is substantially lower than 2013 IBBS prevalence estimates among FSW in Hanoi and HCMC (between 9.0 and 13.9%) [3], suggesting that self-report might indeed have led to an underestimate of HIV prevalence among FSWs, either because of respondent bias or because the FSWs were truly unaware of their current HIV status. The direction or magnitude by which the association between HIV status of the referring FSW and the male client might be biased by an underestimate of HIV prevalence among FSW is not known. However, the magnitude of the association in our analysis (5.37) suggests than a true association likely exists. Of note, the HIV prevalence among the male clients surveyed in our study is comparable to the 2013 IBBS estimates for FSWs [3].
Of course, in this cross-sectional analysis, the causality of any association—whether male client might have acquired HIV from or transmitted HIV to the FSW or even whether HIV concordance is the result of commercial sex between the FSW and the client—cannot be ascertained. Regardless, a causal association is scientifically plausible in either direction and should be considered in the design of prevention interventions.
The apparent association between male client HIV status and condom use at last encounter with a FSW may require additional study. When sexual activity and condom use with commercial and non-commercial sex partners over the past 6 months are used to classify male clients into low, potential-, and high-risk potential to be ‘bridgers’ for HIV into the general population, an estimated 18.7% of male clients are classified as ‘high-risk bridgers’ meaning that they reported inconsistent condom use with both FSWs and sexual partners who are otherwise low-risk over the past 6 months. Consistent with findings from a 2007 study in other locations in Vietnam with a high concentration of FSWs [12], HIV prevalence did not differ significantly among the three categories. This may indicate a number of issues including reporting bias regarding condom use over time that other factors (e.g., injection drug use) among male clients of FSWs are more associated with HIV status than condom use, or that HIV risk among male clients is similar over time regardless of their reported condom use. Although HIV status among male clients did not differ by “bridging” category, the high HIV prevalence across these categories implies that there is potential for previously uninfected male clients to acquire HIV from FSWs and then to transmit it to their noncommercial partners over time. Similarly, the high HIV prevalence and inconsistent condom use among male clients also means that HIV transmission may occur from an HIV-infected male client to the FSW who might then transmit HIV on to other male clients.
The relatively lower condom use with FSWs over a longer period (i.e. 6 months) compared to at last sex reported in this survey is consistent with findings from other studies indicating potentially increased risk for HIV acquisition and transmission among male clients over longer duration of high risk behavior [5].
Of particular concern is the high proportion (64.7%) of male clients who reported to have never been tested for HIV which is similar to studies in Vietnam and internationally [5, 12, 21]. That 65.2% of the male clients who tested positive for HIV infection in this survey reported never being tested previously for HIV might indicate that they were not aware of that they were HIV-positive, had not accessed HIV care and treatment services, and were not adjusting their behaviors accordingly. This low testing uptake may be the result of a low understanding of the risk of HIV among male clients, distrust or stigma of the health system, as well as limited effective programs that focus such services to this population.
Limitations
This study is subject to several limitations that should be taken into account when interpreting and generalizing its findings and conclusions. A primary limitation is the potential for selection bias among the recruited FSWs and, particularly, the male clients that they referred to the study. For example, FSW and clients with drug-use behaviors or lower income levels may have been disproportionally referred by their FSWs to collect the nominal enrolment incentive thus limiting the generalizability of these findings to the overall male client population but rather to a ‘higher-risk’ male client group. Secondly, as above, relying on self-reported HIV status among FSWs in our analysis may have under-estimated the true HIV burden among FSWs as well as led to inaccurate estimates of sero-concordance and association between the self-reported HIV status of the FSW and the male client referred for the study. Future studies should consider the testing FSWs in addition to their male clients. A third key limitation would be that behavioral data were collected from self-reported responses that may result in information bias particularly related to sensitive and stigmatized behavior such as drug use and sexual behaviors (e.g., condom use). To minimize this, study teams were given intensive training in administering such questionnaires and responses have been compared against other surveys when possible to assist in identifying differences.
Conclusions
We believe that this survey and analysis provides important and specific findings about the HIV burden and risk factors among male clients of FSWs. Previously reported data indicated that 15% of the HIV among women is due to risks associated with female sex work; in Southeast Asia this attributable fraction is estimated to be 7.4% [22]. Previous modelling studies have estimated that 18% of annual new HIV infections in Vietnam are among clients of FSWs, [15] but limited data have been made available to understand HIV risk among clients. Given that, overall, an estimated 5–10% of sexually active males in Vietnam have paid for sex with a FSW, such information is important in focusing interventions for both FSWs and their male clients to ultimately control the HIV epidemic in Vietnam.
Male clients, particularly those that have a history of injection drug use, are at increased risk of acquiring HIV and potentially transmitting it to their non-commercial and FSW sexual partners. Without an immediate focus of effective HIV testing, prevention, care, and treatment programs on high-burden populations, especially those male clients with a previous or current history of drug use, Vietnam may have difficulty reaching its “90–90–90” targets by 2020 (i.e., 90% of all people living with HIV will know their HIV status; 90% of all people with diagnosed HIV infection will receive sustained antiretroviral therapy; and 90% of all people receiving antiretroviral therapy will have durable viral suppression) as defined in its National Strategy on HIV/AIDS Prevention and Control in Vietnam till 2020 with a vision to 2030. Such programs will likely need to be innovative in order to reach previously neglected populations such as male clients to reduce HIV transmission to the FSWs they engage. Examples of such innovation may include: community-based HIV counseling and testing (e.g., offering such services in or near locations frequented by male clients, self-testing) and incentivizing testing and linkage to antiretroviral treatment. In addition, Vietnam should also continue to expand its evidence-based harm reduction programs for drug use including methadone maintenance treatment [23, 24], needle/syringe exchange, and annual HIV counseling and testing and immediate anti-retroviral therapy (ART) for HIV-infected injection drug users [25,26,27]. Conversely, FSWs should have access to key services such as HIV testing and linkage to care as well as be empowered to demand consistent condom use by their male clients. The findings from this study related to HIV sero-discordance highlight the potential need for providing oral pre-exposure prophylaxis (PrEP) to FSW in Vietnam.
These findings contribute evidence that male clients of FSWs surveyed in this study, which may be a sub-set of the overall male client population, are important contributors to the HIV/AIDS epidemic in Vietnam along with those more traditional key populations of injection drug users and FSWs and should be considered in the design and implementation of HIV control programs as well as estimations and modeling of the HIV/AIDS burden in Vietnam.
References
Vietnam Ministry of Health. Viet Nam HIV/AIDS estimates and projections 2011–2015. Hanoi: Vietnam Ministry of Health; 2012.
Duong CT, Nguyen TH, Hoang TTH, et al. Sexual risk and bridging behaviors among young people in Hai Phong, Vietnam. AIDS Behav. 2008;12:643–51.
Vietnam Ministry of Health. Integrated biological and behavioral surveillance (IBBS) in Vietnam-round III 2013. Hanoi: Vietnam Ministry of Health; 2014.
Vietnam General Statistics Office (GSO). No title. 2015. http://www.gso.gov.vn/Default.aspx?tabid=217.
PSI (PSI) . Behavioral survey of male clients of female sex workers across seven provinces in Vietnam report; 2009.
Vietnam Ministry of Health (MOH). Vietnam HIV/AIDS estimates and projections. Hanoi: Vietnam Ministry of Health; 2012.
World health Organization. Consolidated Strategic Information Guidelines for HIV in the Health Sector. World health Organization; 2015.
Zhang C, Li X, Su S, et al. Prevalence of HIV, syphilis, and HCV infection and associated risk factors among male clients of low-paying female sex workers in a rural county of Guangxi, China: a cross-sectional study. Sex Transm Infect. 2014;90:230–6. http://sti.bmj.com/content/90/3/230.full.pdf.
Fleming PJ, Patterson TL, Chavarin CV, Semple SJ, Eileen CM. Behavioral and psychosocial correlates of HIV testing among male clients of female sex workers in Tijuana, Mexico. AIDS Behav. 2016;. doi:10.1007/s10461-016-1531-6.
Reilly KH, Wang J, Zhu Z, et al. HIV and associated risk factors among male clients of female sex workers in a Chinese Border region. Sex Transm Dis. 2012; 39:750–5. http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00007435-201210000-00003.
Shah NS, Shiraishi RW, Subhachaturas W, et al. Bridging populations-sexual risk behaviors and HIV prevalence in clients and partners of female sex workers, Bangkok, Thailand 2007. J Urban Heal. 2011. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=21336505.
Nguyen NT, Nguyen HT, Trinh HQ, Mills SJ, Detels R. Clients of female sex workers as a bridging population in Vietnam. AIDS Behav. 2009;13:881–91. doi:10.1007/s10461-008-9463-4.
Go VF, Quan VM, Voytek C, Celentano D, Nam L Van. Intra-couple communication dynamics of HIV risk behavior among injecting drug users and their sexual partners in Northern Vietnam. Drug Alcohol Depend. 2006;84:69–76. http://www.ncbi.nlm.nih.gov/pubmed/16413145. Accessed 12 April 2014.
TD H, Cohen S, Nghi N, et al. Behind the pleasure: sexual decision-making among high-risk men in urban Vietnam, FHI Working Paper. 2006.
UNAIDS UW. Measuring intimate partner transmission of HIV in Viet Nam: a triangulation exercise. 2012.
Raymond HF, Ick T, Grasso M, Vaudrey J, McFarland W. Resource guide: time location sampling (TLS) table of contents C. Choosing a sampling method. San Francisco : San Francisco Department of Public Health; 2007.
StataCorp. Stata Statistical Software: Release 12. 2011.
Nadol P, O’connor S, Duong H, et al. Findings from integrated behavioral and biologic survey among males who inject drugs (MWID)—Vietnam, 2009–2010: evidence of the need for an integrated response to HIV, hepatitis B virus, and hepatitis C virus. PLoS ONE. 2015;10:e0118304. doi:10.1371/journal.pone.0118304.
Le L-VN, Nguyen TA, Tran HV, et al. Correlates of HIV infection among female sex workers in Vietnam: injection drug use remains a key risk factor. Drug Alcohol Depend. 2015;150:46–53.
Vietnam Ministry of Health. Vietnam authority of HIV/AIDS control. Optimizing Viet Nam’s HIV response: an investment case. 2014.
Miller GA, Mendoza W, Krone MR, et al. Clients of female sex workers in Lima, Peru: a bridge population for sexually transmitted disease/HIV transmission? Sex Transm Dis. 2004;31:337–42. http://www.ncbi.nlm.nih.gov/pubmed/15167641.
Pruss-Ustun A, Wolf J, Driscoll T, Degenhardt L, Neira M, Calleja JMG. HIV due to female sex work: regional and global estimates. PLoS ONE. 2013;8:1–7.
Nguyen TTM, Nguyen LT, Pham MD, Vu HH, Mulvey KP. Methadone maintenance therapy in Vietnam: an overview and scaling-up plan. Adv Prev Med. 2012;2012:732484. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3512212&tool=pmcentrez&rendertype=abstract. Accessed 21 June 2013.
Macarthur GJ, Minozzi S, Martin N, et al. Opiate substitution treatment and HIV transmission in people who inject drugs: systematic review and meta-analysis. BMJ. 2012;5945:1–16.
Kato M, Granich R, Duc Bui D, et al. The potential impact of expanding antiretroviral therapy and combination prevention in Vietnam: towards elimination of HIV transmission. J Acquir Immune Defic Syndr. 2013; http://www.ncbi.nlm.nih.gov/pubmed/23714739.
Rodger AJ, Cambiano V, Bruun T, et al. Sexual activity without condoms and risk of HIV transmission in serodifferent couples when the HIV-positive partner is using suppressive antiretroviral therapy. Jama. 2016;316:171. doi:10.1001/jama.2016.5148.
Stover J, Bollinger L, Izazola JA, Loures L, Delay P. What is required to end the AIDS epidemic as a public health threat by 2030 ? The cost and impact of the fast-track approach. PloS ONE. 2016;11:e0154893.
Acknowledgements
The authors would like to thank the Vietnam Provincial HIV/AIDS Committees (PACs) of Hanoi and Ho Chi Minh City who contributed to the completion of this study. We would also like to sincerely thank Dr. Sheryl Lyss, the Vietnam CDC Associate Director for Science, for her technical review and suggested edits to the manuscript.
Disclaimer
The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Funding
This research has been supported by the President’s Emergency Plan for AIDS Relief (PEPFAR) through the U.S. Centers for Disease Control and Prevention under the terms of contract 200-2011-M-42018.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Nadol, P., Hoang, T.V., Le, LV. et al. High HIV Prevalence and Risk Among Male Clients of Female Sex Workers in Hanoi and Ho Chi Minh City, Vietnam. AIDS Behav 21, 2381–2393 (2017). https://doi.org/10.1007/s10461-017-1751-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-017-1751-4