Abstract
We assessed the association between marijuana use and retention in HIV care through a retrospective cohort study of patients engaged in care at a large HIV clinic in 2011 and 2012. Two different retention outcomes were assessed: not meeting the Institute of Medicine’s (IOM) retention definition (≥2 provider visits ≥90 days apart in a calendar year) and no-show visits. Any marijuana use and frequency of marijuana use were obtained from a substance use screening questionnaire administered at each clinic visit. Modified Poisson regression was used to estimate risk ratios and 95% confidence intervals for the association between marijuana use and retention outcomes. Marijuana use was reported by 17% of 1791 patients and 21% were not retained (IOM definition). Marijuana use was not associated with the IOM retention outcome, but was associated with missing the next scheduled appointment. A non-linear dose–response was observed for frequency of marijuana use and missed visits, with daily users having the highest risk compared to non-users. Daily marijuana use had a negative impact on HIV clinic attendance. Further research is needed to elucidate the mechanisms by which marijuana use affects this outcome to inform targeted interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Attitudes and laws regarding marijuana use in the United States (US) have been rapidly changing. Currently, 28 states and the District of Columbia have legalized marijuana for medical or recreational use [1]. Beginning in 2012, Alaska, California, Colorado, the District of Columbia, Maine, Massachusetts, Nevada, Oregon, and Washington have either fully implemented or passed legislation for legalized recreational use. In 2015, 8.3% of the US general population (≥12 years) reported marijuana use in the past month, with use being most commonly reported in those 18–25 years old (19.8%) [2]. Furthermore, marijuana use in the US has steadily increased since 2008 [2].
As with other types of non-injection drug use, marijuana use is more common among people living with HIV (PLWH) [3]. The Centers for Disease Control and Prevention’s Medical Monitoring Project, a population-based surveillance system for clinical and behavioral characteristics among PLWH receiving outpatient medical care in the US between 2005 and 2009, reported past year marijuana use in 22% of participants [4]—twice that of the general population. Other studies report 25% marijuana use in the past three months [5, 6], while the Women’s Interagency HIV Study reported 16–29% marijuana use in the past six months across six study sites [7].
The impact of legalization on trends in marijuana use is unclear. However, as marijuana use becomes more accepted, the public health implications of use, including adverse consequences or potential benefits, need to be investigated and clarified [8]. Among PLWH, marijuana has been associated with behavior that can contribute to HIV transmission [9, 10] and may fuel abuse of other drugs in poly-substance using PLWH [11–13], thereby contributing to poorer outcomes. On the other hand, alleviation of a variety of symptoms including anxiety, depression, loss of appetite, nausea, and pain are a commonly reported reason for marijuana use among PLWH [14–18] and controlled trials have demonstrated the utility of cannabis/cannabinoids in the treatment of neuropathic pain from multiple etiologies [19], including HIV-associated neuropathy [20].
The impact of marijuana use on HIV care and treatment outcomes, however, is not well studied and results are inconsistent. Some studies have suggested that marijuana use is associated with worse antiretroviral therapy (ART) adherence [7, 21, 22], while others have not [23, 24], including better adherence among PLWH suffering from nausea [24]. Similarly, cannabis use was found in separate studies to be associated with higher [25] and lower [26] viral loads, and to have no association with viral load [27, 28]. There are even fewer studies of marijuana use and retention in HIV care, again with inconsistent results [29–31]. Therefore, the objective of this study was to assess the association between marijuana use and retention in HIV care in a large clinical cohort in the southeastern US.
Methods
Study Site and Population
We conducted a retrospective cohort study using data from the Vanderbilt Comprehensive Care Clinic (VCCC). The VCCC provides outpatient, primary HIV medical care and non-medical services to over 3000 PLWH in Middle Tennessee and draws patients from the large, urban Nashville area and surrounding rural communities. Laboratory and clinical information is regularly updated, validated, and extracted from patient electronic medical records. For the current study, patients from the VCCC were included if they were ≥18 years old and attended ≥2 medical provider visits between January 1 and December 31, 2011. Demographic and clinical data were obtained from the electronic medical record.
Retention Outcomes
The primary outcomes of the study were two different retention outcomes assessed in 2012. Consistent with other studies and definitions, only HIV medical provider visits were considered for retention purposes; inpatient visits, emergency department visits, and ancillary services such as nutrition, mental health, or laboratory were not utilized. The first outcome was failure to be retained in the following calendar year (2012) according to the Institute of Medicine (IOM) definition (retained if ≥2 provider visits ≥90 days apart in a calendar year) [32]. Clinic appointment dates and status (completed, canceled, or no show) were obtained for 2012. Irrespective of how many medical provider visits were scheduled, canceled, or missed, a patient was considered retained if he or she met the IOM definition. The second retention outcome was missed visits in 2012. Again utilizing appointment dates and status, a visit was considered to be missed if the status was ‘no show’ and not missed if the status was ‘completed’. Canceled visits were ignored.
Marijuana and Other Substance Use
At each clinic visit, all patients were administered a short screening questionnaire by the clinic nurse after being brought into the exam room. The questionnaire asks how many times in the last seven days a patient missed ART, used specific substances, including marijuana, and smoked cigarettes (Table 1) [28]. The questionnaire is used as part of routine clinical care and was designed to be concise so it would not disrupt the flow of clinic operations but allow for data collection from all patients.
Responses to the substance use and alcohol screening questions were obtained for each clinic visit in 2011 for use in the IOM retention analysis. Only those patients with screening questionnaire responses on at least two different dates in 2011 were used in the analysis. This was done to obtain a better indication of substance use, since infrequent users may report use on some, but not all, questionnaires. Any marijuana use was defined as use at least one time in the past week on at least one screening questionnaire. Frequency of marijuana use was calculated by summing the number of times used in the last seven days across all the screening questionnaires administered to that patient, then dividing by the number of administered screening questionnaires. This provides an indication of the average number of times used per week: zero (non-users), between zero and one (less than weekly use), 1–<7 (weekly use), and ≥7 (daily use). For each of the other illicit substances, we report only any use due to their low prevalence and low frequency of being reported. Use of other illicit substances was further combined into any non-marijuana substance use. Frequency of alcohol use was calculated identically to that of marijuana use.
Similarly, responses to the substance use and alcohol screening questions were obtained for each clinic visit in 2012 for use in the missed-visit analysis. Because the association of interest was on marijuana use and missing the subsequent clinic visit, only marijuana use reported on the current screening questionnaire was utilized, rather than averaging across multiple screening questionnaires. In this way, patients contributed multiple observations to the missed visit analysis equal to the number of completed clinic visits for which marijuana use was assessed. Other illicit substance use was calculated as any use versus no use at each clinic visit, and frequency of alcohol use was calculated identically to that of marijuana use.
Statistical Analysis
The association between marijuana use and IOM-defined retention in the subsequent calendar year was assessed in all patients with at least two medical provider visits in 2011. Modified Poisson regression was used to estimate risk ratios (RR) and 95% confidence intervals (CI) for the association between marijuana use and not being retained in care the following year. Modified Poisson regression was used to avoid potential convergence problems with log linear models and to improve interpretation over logistic regression since the outcome is relatively common [33]. Marijuana use was analyzed both as any use during the calendar year (versus no use) and as frequency of use. Because the latter is a continuous variable, a restricted cubic spline was initially used to relax assumptions of a linear relationship with retention. A four-knot spline was specified, with knots at the 5th, 35th, 65th, and 95th percentile among patients reporting marijuana use, and a Wald test was used to jointly test the contribution of the non-linear terms. If their joint contribution was not statistically significant (p ≥ 0.05), the model was simplified to only include a linear term for frequency of marijuana use. Age (continuous), race/ethnicity, sex, HIV risk category, years since HIV diagnosis (continuous), any non-marijuana substance use, and frequency of alcohol use (continuous) were included in the model to control for confounding. Continuous variables were assessed for linearity in their association with poor retention as described above for marijuana use.
The association between marijuana use and missing the subsequent visit included a subset of patients who had at least two medical provider visits in 2011 and who also had at least one completed HIV clinic visit in 2012 followed by a scheduled return visit. Modified Poisson regression was again used to estimate RR and 95% CI for the association between marijuana use and missing the subsequent visit. Because this analysis was longitudinal over the calendar year and included multiple observations from each patient, generalized estimating equations were used to account for outcome correlation within participants (exchangeable correlation structure). The analysis was conducted as described above for the IOM retention outcome. A second analysis was conducted to explore the association between marijuana use and missed visits among the subset of patients who were retained in care in 2012 according to the IOM retention definition.
All analyses were conducted using Stata 12.0 (College Station, TX). This study was approved by the Vanderbilt University Medical Center Institutional Review Board.
Results
A total of 1791 patients met the inclusion criteria, having a median of three clinic visits during 2011 [interquartile range (IQR) from two to four]. The median age was 45 years (IQR 36–51), 75% were male, 51% were Caucasian, 38% were African-American, and patients had been diagnosed with HIV for a median of eight years (IQR 4–13) (Table 2). The predominant risk factor for HIV acquisition was men having sex with men (MSM; 56%). Any marijuana use during 2011 was reported by 311 (17%) patients, with the majority reporting weekly use (i.e., frequency of use between one and six times per week). Non-marijuana substance use was reported by 4% of patients and primarily involved cocaine use. Marijuana users tended to be younger (particularly those with more frequent use), male, African-American, and to have had a history of injection drug use (IDU) or other substance use, predominantly cocaine. Alcohol use did not differ substantially between marijuana users and non-users. Provider visits, ART status, and CD4 cell counts also did not differ; however fewer marijuana users were virologically suppressed (HIV RNA < 50 copies/mL), and of patients not suppressed, viral loads were higher among marijuana users and increased substantially with the frequency of use (Table 2).
IOM Retention Analysis
The majority of patients met the IOM definition of retention in HIV care during the following calendar year, while 383 (21%) failed to be retained. After adjusting for age, sex, race, HIV risk category, time since HIV diagnosis, non-marijuana substance use, and frequency of alcohol use, neither any marijuana use (RR = 1.07; 95% CI 0.85–1.33) nor frequency of marijuana use was associated with failing to be retained in care (RR = 1.02; 95% CI 0.98–.06) (Table 3).
Missed Visits Analysis
Of the 1791 patients included in the IOM retention analysis above, 1549 had ≥1 completed clinic visits, ≥1 completed substance use questionnaires, and ≥1 additional scheduled clinic appointments during 2012, and were therefore included in the analysis of missed visits. These patients provided a total of 4183 clinic visits with available substance use data and a scheduled return appointment; 274 (18%) patients had at least one missed visit and 652 (16%) of scheduled appointments were missed.
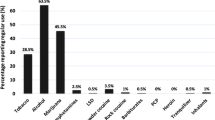
Overall, any reported marijuana use was associated with a 38% increased risk of missing the next scheduled appointment (adjusted RR = 1.38; 95% CI 1.12–1.69) (Table 4). Frequency of marijuana use was also associated with missing a subsequent appointment and demonstrated a non-linear relationship where the highest risk occurred for those reporting daily marijuana use (7–14 times in the past week, Fig. 1). Based on this relationship and compared with never users, patients using marijuana one to two times per week had minimal, if any, risk of missing the next scheduled appointment (Fig. 1; Table 4). More frequent use rapidly increased the risk of missed visits, with patients reporting marijuana use seven times in the past week having a 67% increased risk of missing the next appointment (adjusted RR = 1.67; 95% CI 1.30–2.15). The observed associations remained among the subset of patients retained in care during the same year (IOM definition).
Relationship between number of times marijuana was used in the past week and risk of missing the next scheduled clinic appointment. Predicted risk (solid line) and 95% CI of the predicted risk (dashed lines) modeled using a restricted cubic spline with knots at 1, 2, 7, and 14 uses in the last 7 days. Predicted risks represent the risk of missing the subsequent clinic appointment for a patient having the median value of each covariate (45 year old White male, living with HIV for 8 years, MSM risk category, no alcohol use, and no non-marijuana illicit substance use); Not shown on the histogram are those reporting no use (n = 3761) and those reporting marijuana use >14 times in the last 7 days (n = 12)
Discussion
The current study of marijuana use and retention in HIV care found that marijuana use was not associated with failing to meet the IOM retention definition of at least two clinic visits at least 90 days apart during the following calendar year. However, within that following year, marijuana use was associated with missing the next scheduled clinic appointment. In particular, daily use (≥7 times per week) resulted in at least a 65% increase in risk of missing the next scheduled visit, while low frequency of use (1–2 times per week) demonstrated little increase in missed visits. This finding persisted among patients who met the IOM retention definition for that year, which is a concern because missed visits have been associated with mortality even when patients are retained according to the IOM definition [34].
Little has been published on the impact of marijuana use on retention in HIV care. Our findings are consistent with two prior studies which found marijuana use to be associated with missed visits, but not with retention measures based on kept visits such as the IOM indicator. A prospective study of 178 female adolescents found that weekly or daily marijuana use was inversely associated with keeping appointment visits (rate ratio = 0.87; 95% CI 0.76–0.99), while less frequent marijuana use was not associated with keeping appointments (rate ratio = 0.91; 95% CI 0.80–1.04) [29]. In contrast, a cross-sectional study of 152 young African-American MSM found that daily marijuana use (odds ratio = 1.31; 95% CI 0.40–4.30) and weekly or less than weekly use (odds ratio = 1.69; 95% CI 0.53–5.38) was associated with better retention using the IOM definition, though estimates were imprecise [31]. Unlike these two studies, however, ours involved a much larger population and better represents the HIV population in the US. Further, because our screening questionnaire asks about the number of times marijuana was used, we explored the dose–response relationship with retention outcomes. Of note, our findings demonstrate that among patients classified as weekly marijuana users (1–6 times per week), the relative risk of missing the next clinic appointment increases rapidly, from 6 to 56% higher risk than non-users, before leveling off among daily users.
The reason for marijuana’s association with missed visits, but not completion of a minimum number of visits (IOM definition), is not altogether surprising because these assess different aspects of retention in HIV care [35]. Visit attendance may be more sensitive to the shorter-term, more immediate effects of marijuana, while the IOM retention definition may be less sensitive, possibly requiring a cumulative or chronic effect of marijuana use that must surpass some threshold before adversely impacting retention, as may occur with substance use disorders. According to the 2015 National Survey on Drug Use and Health, substance use disorder is relatively low among current marijuana users (18% of users), but much more common among current users of cocaine (43%), illicit opioid pain relievers (57%), heroin (100%), and methamphetamine (100%) [2]. We do not have reliable data on marijuana use disorder in our study population and therefore cannot explore retention outcomes between disordered and non-disordered marijuana use. This is an area for future research. Unlike marijuana use, use of other illicit substances is associated with both missed visits [36] and failure to keep a minimum number of visits over a period of time [37, 38], perhaps reflecting that most non-marijuana substance users have a substance use disorder and HIV care is not always considered a high priority [39, 40].
In our setting, where marijuana use of any kind is illegal, heavy marijuana use could be an indicator of lower levels of social stability, though not reaching the level of disruption that may occur with substance use disorders. Social stability refers to a life structure and reliable routine that protects against hazards and helps maintain societal expectations [41]. It is a construct comprised of housing, employment, relationship, and legal status and may also include residential stability, income, and social support. Disruption of this structure and routine can have a detrimental impact on important health behaviors [42, 43]. However, social stability has rarely been evaluated as a risk factor for retention or ART adherence [41, 44], though some studies have evaluated the impact of individual components of social stability [45, 46]. In this case, adjustment for social stability that influences both marijuana use and retention in care may reduce, remove, or otherwise explain the association between marijuana use and retention.
Alternatively, the impact of long-term marijuana use on cognitive function could lead to lapses in health seeking behavior. A recent study found high levels of cumulative marijuana use were associated with reduced cognitive function among middle-aged adults, and that current, near daily marijuana use was very common among those with high cumulative use [47]. Further research is needed to elucidate the mechanisms by which marijuana use may impact retention outcomes, which would then inform where and how to target interventions related to marijuana use and retention outcomes. Future research should also focus on how marijuana use and retention impact clinical outcomes in PLWH. There is uncertainty about the impact of marijuana use on ART adherence and viral suppression [7, 21–28]. In our study population, virologic suppression was slightly less common among marijuana users regardless of frequency of use. However, among those not virologically suppressed, median viral loads increased with increasing frequency of use.
This study has limitations, which should be acknowledged. First, data on marijuana use was collected via patient self-report, which could lead to under-reporting; our estimate of any use of 17% is slightly lower than other reports among HIV patients in similar populations. Ongoing evaluation of marijuana use in our patient population suggests the clinical screening underestimates the number of marijuana users as well as the frequency of use among users. If this underestimation is non-differential with regard to retention outcomes, then our results are biased toward the null. Our results are also biased toward the null if under-reporting of marijuana use is greater among those not retained or who miss appointments—a likely scenario. Depending on the degree of under-reporting, the true association between marijuana use and both retention outcomes may be much larger, and marijuana use may be associated with both outcomes, not just missed appointments. Second, in order to obtain more detailed marijuana use data, patients were included if they had a minimum of two clinic visits in 2011, possibly reducing the risk of poor retention in the subsequent year and attenuating the true effects of marijuana use on retention. Third, our analysis excluded individuals who did not have substance use data due to multiple missed appointments. To the extent these appointments were missed because of marijuana use, our results could be attenuated compared to what would be found if substance use data were available from all PLWH regardless of appointment status. Fourth, because marijuana use was only measured at clinic visits, which may be scheduled several months apart, it may not accurately reflect use around the time of the next scheduled visit. For each of these reasons, our findings may be considered conservative estimates. Future research on retention outcomes should measure marijuana use that is independent of whether or not a clinic or study visit is attended. This could be done using techniques such as ecologic momentary assessment or daily diaries [48–51]. Finally, consistent with other retention studies, cancelled visits were not considered missed visits and were ignored in the analysis. While many of these were cancelled by the clinic or provider, some patients may cancel for reasons related to their substance use. However, calling to cancel an appointment indicates continued engagement with the clinic, unlike the lack of contact that constitutes poor retention. As with all observational studies, there may be variables that confound the relationship between marijuana use and retention that we failed to control for. Polysubstance in our study populations was low, so our findings may not be generalizable to other substance using populations.
In conclusion, our findings suggest a negative impact of daily marijuana use on subsequent HIV clinic attendance, and may even underestimate the magnitude of this impact. Given the expansion of legalized medical and recreational marijuana in the United States, further research is needed to elucidate the mechanisms by which marijuana use may affect retention outcomes. This would inform where and how to target interventions: heavy users and/or those with marijuana use disorder (but not all users), or else the social context of regular marijuana users if that, rather than marijuana use itself, proves to be the determinant of missed visits. In the meantime, providers could engage young MSM, a group our data suggest are more likely to be using marijuana daily, to discuss how substance use and related social contexts may hinder HIV care and treatment.
References
National Conference of State Legislatures. State Medical Marijuana Laws: National Conference of State Legislatures. http://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx. Accessed Nov 2016.
Center for Behavioral Health Statistics and Quality. Key substance use and mental health indicators in the United States: Results from the 2015 National Survey on Drug Use and Health. HHS Publication No. SMA 16-4984, NSDUH Series H-51. Rockville, MD: Substance Abuse and Mental Health Services Adminstration. 2016. http://www.samhsa.gov/data. Accessed Nov 2016.
Kipp AM, Desruisseau AJ, Qian HZ. Non-injection drug use and HIV disease progression in the era of combination antiretroviral therapy. J Subst Abuse Treat. 2011;40(4):386–96.
Centers for Disease Control and Prevention. Behavioral and clinical characteristics of persons receiving medical care for HIV infection—Medical Monitoring Project, United States, 2009. Morb Mortal Wkly Rep 2014;63(SS-5):1–22.
Allshouse AA, MaWhinney S, Jankowski CM, Kohrt WM, Campbell TB, Erlandson KM. The impact of marijuana use on the successful aging of HIV-infected adults. J Acquir Immune Defic Syndr. 2015;69(2):187–92.
Mimiaga MJ, Reisner SL, Grasso C, et al. Substance use among HIV-infected patients engaged in primary care in the United States: findings from the Centers for AIDS Research Network of Integrated Clinical Systems cohort. Am J Public Health. 2013;103(8):1457–67.
D’Souza G, Matson PA, Grady CD, et al. Medicinal and recreational marijuana use among HIV-infected women in the Women’s Interagency HIV Study (WIHS) Cohort, 1994–2010. J Acquir Immune Defic Syndr. 2012;61:618–26.
Volkow ND, Compton WM, Weiss SR. Adverse health effects of marijuana use. N Engl J Med. 2014;371(9):879.
Van Tieu H, Koblin BA. HIV, alcohol, and noninjection drug use. Curr Opin HIV AIDS. 2009;4(4):314–8.
Kingree JB, Betz H. Risky sexual behavior in relation to marijuana and alcohol use among African-American, male adolescent detainees and their female partners. Drug Alcohol Depend. 2003;72(2):197–203.
Fergusson DM, Boden JM, Horwood LJ. Cannabis use and other illicit drug use: testing the cannabis gateway hypothesis. Addiction. 2006;101(4):556–69.
Kandel DB. Does marijuana use cause the use of other drugs? JAMA. 2003;289(4):482–3.
Parolaro D, Vigano D, Realini N, Rubino T. Role of endocannabinoids in regulating drug dependence. Neuropsychiatr Dis Treat. 2007;3(6):711–21.
Corless IB, Lindgren T, Holzemer W, et al. Marijuana effectiveness as an HIV self-care strategy. Clin Nurs Res. 2009;18(2):172–93.
Furler MD, Einarson TR, Millson M, Walmsley S, Bendayan R. Medicinal and recreational marijuana use by patients infected with HIV. AIDS Patient Care STDs. 2004;18:215–28.
Braitstein P, Kendall T, Chan K, et al. Mary-Jane and her patients: sociodemographic and clinical characteristics of HIV-positive individuals using medical marijuana and antiretroviral agents. AIDS. 2001;15:532–3.
Woolridge E, Barton S, Samuel J, Osorio J, Dougherty A, Holdcroft A. Cannabis use in HIV for pain and other medical symptoms. J Pain Symptom Manag. 2005;29:358–67.
Prentiss D, Power R, Balmas G, Tzuang G, Israelski DM. Patterns of marijuana use among patients with HIV/AIDS followed in a public health care setting. J Acquir Immune Defic Syndr. 2004;35:38–45.
Rahn EJ, Hohmann AG. Cannabinoids as pharmacotherapies for neuropathic pain: from the bench to the bedside. Neurotherapeutics. 2009;6:713–37.
Phillips TJ, Cherry CL, Cox S, Marshall SJ, Rice AS. Pharmacological treatment of painful HIV-associated sensory neuropathy: a systematic review and meta-analysis of randomised controlled trials. PLoS ONE. 2010;5(12):e14433.
Tucker JS, Burnam MA, Sherbourne CD, Kung F-Y, Gifford AL. Substance use and mental health correlates of nonadherence to antiretroviral medications in a sample of patients with human immunodeficiency virus infection. Am J Med. 2003;114:573–80.
Bonn-Miller MO, Oser ML, Bucossi MM, Trafton JA. Cannabis use and HIV antiretroviral therapy adherence and HIV-related symptoms. J Behav Med. 2014;37(1):1–10.
Rosen MI, Black AC, Arnsten JH, et al. Association between use of specific drugs and antiretroviral adherence: findings from MACH 14. AIDS Behav. 2013;17(1):142–7.
de Jong BC, Prentiss D, McFarland W, Machekano R, Israelski DM. Marijuana use and its association with adherence to antiretroviral therapy among HIV-infected persons with moderate to severe nausea. J Acquir Immune Defic Syndr. 2005;38:43–6.
Ghosn J, Leruez-Ville M, Blanche J, et al. HIV-1 DNA levels in peripheral blood mononuclear cells and cannabis use are associated with intermittent HIV shedding in semen of men who have sex with men on successful antiretroviral regimens. Clin Infect Dis. 2014;58(12):1763–70.
Milloy MJ, Marshall B, Kerr T, et al. High-intensity cannabis use associated with lower plasma human immunodeficiency virus-1 RNA viral load among recently infected people who use injection drugs. Drug Alcohol Review. 2015;34(2):135–40.
Abrams DI, Hilton JF, Leiser RJ, et al. Short-term effects of cannabinoids in patients with HIV-1 infection: a randomized, placebo-controlled clinical trial. Ann Intern Med. 2003;139(4):258–66.
Rasbach DA, Desruisseau AJ, Kipp AM, et al. Active cocaine use is associated with lack of HIV-1 virologic suppression independent of nonadherence to antiretroviral therapy: use of a rapid screening tool during routine clinic visits. AIDS Care. 2013;25(1):109–17.
Dietz E, Clum GA, Chung SE, et al. Adherence to scheduled appointments among HIV-infected female youth in five U.S. cities. J Adolesc Health. 2010;46(3):278–83.
Weber R, Huber M, Battegay M, et al. Influence of noninjecting and injecting drug use on mortality, retention in the cohort, and antiretroviral therapy, in participants in the Swiss HIV Cohort Study. HIV Med. 2015;16(3):137–51.
Morgan E, Khanna AS, Skaathun B, et al. Marijuana use among young black men who have sex with men and the HIV care continuum: findings from the uConnect Cohort. Subst Use Misuse. 2016;51(13):1751–9.
Ford MA, Spicer CM. Monitoring HIV care in the United States: indicators and data systems. Washington, DC: National Academies Press; 2012.
Zou GY, Donner A. Extension of the modified Poisson regression model to prospective studies with correlated binary data. Stat Methods Med Res. 2013;22(6):661–70.
Mugavero MJ, Westfall AO, Cole SR, et al. Beyond core indicators of retention in HIV care: missed clinic visits are independently associated with all-cause mortality. Clin Infect Dis. 2014;59(10):1471–9.
Mugavero MJ, Westfall AO, Zinski A, et al. Measuring retention in HIV care: the elusive gold standard. J Acquir Immune Defic Syndr. 2012;61(5):574–80.
Merlin JS, Westfall AO, Raper JL, et al. Pain, mood, and substance abuse in HIV: implications for clinic visit utilization, antiretroviral therapy adherence, and virologic failure. J Acquir Immune Defic Syndr. 2012;61(2):164–70.
Ulett KB, Willig JH, Lin HY, et al. The therapeutic implications of timely linkage and early retention in HIV care. AIDS Patient Care STDS. 2009;23(1):41–9.
Monroe AK, Lau B, Mugavero MJ, et al. Heavy alcohol use is associated with worse retention in HIV care. J Acquir Immune Defic Syndr. 2016;73(4):419–25.
Chitsaz E, Meyer JP, Krishnan A, et al. Contribution of substance use disorders on HIV treatment outcomes and antiretroviral medication adherence among HIV-infected persons entering jail. AIDS Behav. 2013;17(Suppl 2):S118–27.
Meyer JP, Althoff AL, Altice FL. Optimizing care for HIV-infected people who use drugs: evidence-based approaches to overcoming healthcare disparities. Clin Infect Dis. 2013;57(9):1309–17.
German D, Latkin CA. Social stability and health: exploring multidimensional social disadvantage. J Urban Health. 2012;89(1):19–35.
Mugavero MJ. Improving engagement in HIV care: what can we do? Top HIV Med. 2008;16(5):156–61.
Giordano TP. Retention in HIV care: what the clinician needs to know. Top Antivir Med. 2011;19(1):12–6.
Bouhnik AD, Chesney M, Carrieri P, et al. Nonadherence among HIV-infected injecting drug users: the impact of social instability. J Acquir Immune Defic Syndr. 2002;15(31 Suppl 3):S149–53.
Hightow-Weidman LB, Jones K, Wohl AR, et al. Early linkage and retention in care: findings from the outreach, linkage, and retention in care initiative among young men of color who have sex with men. AIDS Patient Care STDS. 2011;25(Suppl 1):S31–8.
Peretti-Watel P, Spire B, Schiltz MA, et al. Vulnerability, unsafe sex and non-adherence to HAART: evidence from a large sample of French HIV/AIDS outpatients. Soc Sci Med. 2006;62(10):2420–33.
Auer R, Vittinghoff E, Yaffe K, et al. Association between lifetime marijuana use and cognitive function in middle age: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. JAMA Int Med. 2016;176(3):352–61.
Schroder KE, Johnson CJ. Interactive voice response technology to measure HIV-related behavior. Curr HIV/AIDS Rep. 2009;6(4):210–6.
Tucker JA, Simpson CA, Huang J, Roth DL, Stewart KE. Utility of an interactive voice response system to assess antiretroviral pharmacotherapy adherence among substance users living with HIV/AIDS in the rural South. AIDS Patient Care STDS. 2013;27(5):280–6.
Shorey RC, Moore TM, McNulty JK, Stuart GL. Do alcohol and marijuana increase the risk for female dating violence victimization? A prospective daily diary investigation. Psychol Violence. 2016;6(4):509–18.
O’Hara RE, Armeli S, Tennen H. Alcohol and cannabis use among college students: substitutes or complements? Addict Behav. 2016;58:1–6.
Acknowledgements
This study was supported by the National Institutes of Health-funded Tennessee Center for AIDS Research (P30-AI110527) and the National Institute on Drug Abuse at the National Institutes of Health (R03-DA039743 to A.M.K). Drs. Kipp and Brinkley-Rubinstein were scholars with the HIV/AIDS, Substance Abuse, and Trauma Training Program (HA-STTP), at the University of California, Los Angeles supported through an award from the National Institute on Drug Abuse at the National Institutes of Health (R25-DA035692). Dr. Brinkley-Rubinstein received additional support through training programs at Brown University funded by the National Institutes of Health (National Institute on Drug Abuse, T32-DA013911; and National Institute for Mental Health, R25-MH083620).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was reviewed and approved by the Vanderbilt University medical Center Institutional Review Board.
Informed Consent
The informed consent process was waived by the Institutional Review Board because all data were collected as part of routine care and the study was a retrospective analysis of existing clinical data.
Rights and permissions
About this article
Cite this article
Kipp, A.M., Rebeiro, P.F., Shepherd, B.E. et al. Daily Marijuana Use is Associated with Missed Clinic Appointments Among HIV-Infected Persons Engaged in HIV Care. AIDS Behav 21, 1996–2004 (2017). https://doi.org/10.1007/s10461-017-1716-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-017-1716-7