Abstract
The majority of persons infected with HIV live in large metropolitan areas and many such areas have implemented intensified HIV testing programs. A national indicator of HIV testing outcomes is late diagnosis of HIV infection (stage 3, AIDS). Based on National HIV Surveillance System data, 23.3 % of persons with HIV diagnosed in 2012 had a late diagnosis in large MSAs, 26.3 % in smaller MSAs, and 29.6 % in non-metropolitan areas. In the 105 large MSAs, the percentage diagnosed late ranged from 13.2 to 47.4 %. During 2003–2012, the percentage diagnosed late decreased in large MSAs (32.2–23.3 %), with significant decreases in 41 of 105 MSAs overall and among men who have sex with men. Sustained testing efforts may help to continue the decreasing trend in late-stage HIV diagnosis and provide opportunities for early care and treatment and potential reduction in HIV transmission.
Resumen
La mayoría de las personas infectadas con el VIH viven en grandes áreas metropolitanas y muchas de esas áreas han implementado programas intensivos de pruebas de VIH. Un indicador nacional del resultado de las actividades de pruebas de VIH es el diagnóstico tardío de la infección por VIH (clasificación 3, SIDA). Basado en datos del Sistema Nacional de Vigilancia de VIH, el 23.3 % de las personas con VIH diagnosticadas en 2012 en áreas estadísticas metropolitanas (MSA por sus siglas en inglés) grandes, tuvo un diagnóstico tardío, el 26.3 % en las MSA más pequeñas, y 29.6 % en las áreas no metropolitanas. En las 105 MSA grandes, el porcentaje de diagnósticos tardíos oscilo entre 13.2 % y 47.4 %. Del 2003 al 2012, el porcentaje de diagnósticos tardíos disminuyó en las MSA grandes (del 32.3 % al 23.3 %), con una disminución significativa en 41 de las 105 MSA grandes y entre hombres que tienen sexo con hombres. Los esfuerzos continuos en proveer pruebas de VIH pueden ayudar a continuar la tendencia decreciente de diagnósticos tardíos del VIH, y proporcionar oportunidades para la atención y tratamiento oportuno, y la reducción potencial en la transmisión del VIH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Routine screening for human immunodeficiency virus (HIV) infection is recommended for patients in all health-care settings to reduce the number of persons unaware of their infection and to detect HIV infection early [1, 2]. Early diagnosis of HIV infection provides opportunities for prompt linkage to medical care and antiretroviral therapy, which are associated with reduced morbidity and mortality [3]. In recent years there has also been an increased emphasis on HIV testing as part of a comprehensive HIV prevention strategy, along with an increase in federal funding for HIV testing, as more evidence emerged that effective treatment that results in viral suppression can reduce the risk of onward transmission of the virus [4–8]. In addition, persons aware of their infection can benefit from counseling to reduce risk behavior [1].
In the United States, overall the percentage of persons who report having ever been tested for HIV increased from 37 % in 2000 to 45 % in 2010 [10], and HIV testing increased among populations most heavily affected by HIV such as blacks/African Americans (ever tested, 52 % in 2000 and 65 % in 2010) and black men who have sex with men (tested within the past 12 months, 63 % in 2008 and 71 % in 2011) [9, 10]. Yet 24 % of persons with HIV diagnosed in 2012 had stage 3 disease (AIDS) at the time of diagnosis, and this was higher among older compared with younger persons and persons with infection attributed to injection-drug use or heterosexual contact compared with males with infection attributed to male-to-male sexual contact [11]. The percentage of persons with a late diagnosis of HIV infection also varies by geographic area. However, the prevalence of late diagnosis has not been assessed for large urban areas, where more than 80 % of persons with HIV live [12].
To monitor the progress in the implementation of HIV testing interventions, late diagnosis of HIV infection is one of seven core indicators for monitoring HIV services funded by the U.S. Department of Health and Human Services [13], and an indicator of Healthy People 2020 to monitor the health of the Nation [14]. We assessed trends in late diagnosis of HIV infection among persons diagnosed during 2003–2012 overall and by race/ethnicity, age, sex and transmission category. Since the majority of persons with HIV in the United States are residents of large metropolitan areas (MSAs) and many large MSAs have implemented intensified HIV testing programs, we report on trends in late diagnosis by population density of area of residence at diagnosis and in 105 large MSAs [12].
Methods
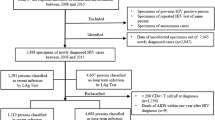
Using data from the Centers for Disease Control and Prevention’s (CDC) National HIV Surveillance System, we determined the percentage of persons aged ≥13 years old with late-stage HIV disease diagnosed in 2012. All U.S. states, the District of Columbia, and Puerto Rico have mandatory reporting of diagnoses of HIV infection and stage 3 disease (AIDS) to state and local health departments. State and local health departments report demographic and clinical information on persons with HIV to CDC without personal identifying information.
Late diagnosis of HIV infection was defined as stage 3 (AIDS) based on CD4 count <200 cells/mL or opportunistic illness within 3 months of HIV diagnosis [15]. Late diagnosis was assessed overall and by race/ethnicity (black/African American, Hispanic/Latino [any race], and white), age group, sex and transmission category, which is a hierarchical classification of reported HIV risk based on the most likely route of transmission (male-to-male sexual contact, injection drug use, male-to-male sexual contact and injection drug use, and heterosexual contact) [12]. Late diagnosis was also assessed by population density of area of residence at diagnosis and in 105 large metropolitan statistical areas (MSAs). Population density was based on the standards of the U.S. Office of Management and Budget, and is defined as populations of area of residence as areas with populations of 500,000 or more, areas with populations of 50,000–499,999, or areas with populations of less than 50,000 (nonmetropolitan areas) [16]. For cases of HIV infection reported without an identified risk factor, HIV transmission category was assigned using multiple imputation [17]. Because surveillance data represent a census of persons with diagnosed HIV, statistical testing is not applied to compare groups. For MSAs, we report on relative percent differences of ≥5 %.
We also determined trends in late diagnosis overall, among men who have sex with men (MSM) who are most affected by HIV, by population density, and in the 105 MSAs during 2003–2012. Change over time was assessed using linear regression to determine the relationship between the percentage of persons with a late diagnosis (dependent variable) and the year of diagnosis of HIV infection (independent variable). We also assessed trends during 2008–2012, after publication of revised testing recommendations (1) and an apparent change in the slope of the trends (Fig. 1). All jurisdictions had implemented name-based HIV reporting by 2008, with transition activities completed and data reported to CDC through June 2014.
Results
Late Diagnosis by MSA
In 2012, 24.0 % of persons received a late diagnosis of HIV infection overall; 23.3 % in large MSAs, 26.3 % in small to medium metropolitan areas, and 29.6 % in nonmetropolitan areas (Table 1). From 2003–2012, late diagnosis significantly decreased overall in large MSAs (32.2 % in 2003; p < 0.01), small to medium metropolitan areas (33.5 in 2003; p < 0.01), and nonmetropolitan areas (33.5 in 2003; p < 0.01); however, from 2008–2012 there was not a statistically significant trend for nonmetropolitan areas (p = 0.06) (Figure). In the 105 large MSAs, the percentage of persons with a late diagnosis of HIV infection in 2012 ranged from <15 % (Birmingham-Hoover, AL; Durham-Chapel Hill, NC) to >40 % (Allentown-Bethlehem-Easton, PA-NJ; Des Moines-West Des Moines, IA; Modesto, CA; New Haven-Milford, CT; Springfield, MA) (Supplemental Table 1). Among MSAs with more than 500 persons with HIV diagnosed in 2012, the percentage of infections diagnosed late varied from 19.7 % in Baltimore-Columbia-Townson, MD to 25.5 % in Philadelphia, PA-NJ-De-MD. During 2003–2012, the percentage diagnosed late decreased significantly (p < 0.05) in 41 individual MSAs and increased in Salt Lake City, UT (Supplemental Table 2). During 2008–2012, late diagnosis decreased (p < 0.05) in 9 MSAs (Lakeland-Winter Haven, FL; New York, NY-NJ-PA; Atlanta-Sandy Springs-Roswell, GA; Bakersfield, CA; Cincinnati, OH-KY-IN; Durham-Chapel Hill, NC; Jacksonville, FL; Raleigh, NC; Washington, DC-VA-MD-WV) and increased in Columbus, OH (data not shown).
Late Diagnosis by Race/Ethnicity
The percentage of persons with a late diagnosis of HIV infection in 2012 was lowest among blacks/African Americans (23.2 %), followed by whites (24.0 %) and Hispanics/Latinos (25.3 %) with a similar distribution in large MSAs but similarly high percentages among the groups in nonmetropolitan areas (Table 2). In 38 of 105 MSAs the percentage diagnosed late was higher among blacks (relative percent difference ≥5 %), and in 58 of 105 MSAs the percentage was higher among Hispanics, compared with whites (Supplemental Table 1). However, there were less than 12 diagnoses among blacks in 19 MSAs (Hispanics, 40 MSAs; whites, 7 MSAs).
Late Diagnosis by Sex and Transmission Category
In 2012, the percentage of persons with a late diagnosis of HIV infection was somewhat lower among males (23.7 %) compared with females (25.1 %) (Table 2). Among males, overall the percentage diagnosed late was lower among males with infection attributed to male-to-male sexual contact (21.6 %) or males with infection attributed to male-to-male sexual contact and injection-drug use (22.3 %) compared with those with infection attributed to injection-drug use (32.8 %) or heterosexual contact (35.5 %), and this pattern was similar for smaller metropolitan areas and nonmetropolitan areas as well as the majority of individual MSAs (Supplemental Table 3). Among MSM, late diagnosis decreased significantly (p < 0.05) in 41 MSAs during 2003–2012 and in 5 MSAs (Dallas, TX; Durham-Chapel Hill, NC; New York, NY-NJ-PA; Portland-South Portland, ME; San Jose-Sunnyvale-Santa Clara, CA) during 2008–2012; late diagnosis increased in 3 MSAs (Columbus, OH; Milwaukee-Waukesha-West Allis, WI; Modesto, CA) (Supplemental Table 2). Differences by risk group were small among females except in nonmetropolitan areas, where 32.9 % of females with infection attributed to injection-drug use had a late diagnosis compared with 27.1 % of females with infection attributed to heterosexual contact (Table 2 and Supplemental Table 4).
Late Diagnosis by Age
The percentage with a late diagnosis of HIV infection increased with age, ranging from 9.4 % for those aged 13–24 years to 38.7 % for those 55 years or older at time of diagnosis overall and with a similar pattern in all areas (Table 2). The percentage diagnosed late was higher in each age group in smaller metropolitan areas and non-metropolitan areas than in the large MSAs.
Discussion
From 2003 to 2012, the percentage of persons with a late diagnosis of HIV infection decreased overall and in many individual areas with a high HIV burden, yet in 2012, overall 1 out of 4 persons had infection diagnosed late and only 19 MSAs had a late diagnosis rate near or below the Healthy People 2020 target of 20.8 % [14]. The majority of HIV diagnoses occurred among MSM and the decrease of late diagnosis among MSM is encouraging. However, the percentage of persons with a late diagnosis of HIV varied widely by MSA, and so did disparities in late diagnosis by race/ethnicity, age, and transmission risk groups.
The observed decrease in the percentage diagnosed late over the 10-year period is parallel to the finding of a decrease in diagnosis delay (the time from infection to diagnosis) during this period [18]. However, a meta-analysis of CD4 cell count at the time of entry to care during 1992–2011 did not find a significant increase in presentation with earlier disease [19]. Additional research is needed to determine whether these disparate findings are due to delays in seeking care after diagnosis. The decrease in late diagnosis may reflect the increase, during the same time, of the percentage of persons ever tested, as well as the increase among blacks, Hispanics or Latinos, and MSM of the percentage tested within the past 12 months [9, 10]. In addition, results based on back-calculation methods using surveillance data indicate a decrease in the percentage of persons living with undiagnosed HIV from 16.5 % in 2007 to 14.0 % in 2011 [11].
Late diagnosis of HIV infection may reflect less uptake of testing in individual areas or among groups, or challenges with accessing care. Generally, HIV testing has been targeted to areas and populations with higher HIV prevalence (1); however, even among MSAs with a large number (>500) of persons with HIV diagnosed per year, the percentage diagnosed late varied. The percentage of persons reporting testing for HIV in 2010 varied by MSA [20], however, little data are available of testing trends for local jurisdictions. During 2007–2010, CDC funded 25 jurisdictions for the expanded testing initiative, and an additional 5 were funded in 2010 [21, 22]. In all directly funded cities (Chicago, Illinois; Houston, Texas; Los Angeles, California; New York, New York; Philadelphia, Pennsylvania; and Washington, D.C.), late diagnoses decreased. Overall, 74 of the 105 MSAs were in jurisdictions that received funding for the expanded testing initiative, and late diagnoses decreased in 30 of 74 (41 %) MSAs in funded jurisdictions compared with 11 of 31 in jurisdictions not funded (35 %). Cooley et al. [22] found testing within the past 12 months increased from 2008 to 2011 among MSM in 20 cities covered by CDC’s National HIV Behavioral Surveillance, with a significant increase in 17 cities with CDC funded expanded HIV testing initiatives but not others. Our results show that among MSM, late diagnoses decreased in 26 of 74 (35 %) of funded compared with 8 of 31 (26 %) of not funded MSAs, but late diagnosis did not decrease in 2 MSAs grouped among the 17 cities with increased testing (New Orleans, Louisiana; San Francisco, California) by Cooley et al. [22].
On average, persons had been infected with HIV for 5.6 years by the time of diagnosis in 2011, with longer diagnosis delays among older age groups and persons with late-stage infection possibly having been infected for 10 years or more [18]. To reduce the number of persons unaware of their infection, detect HIV early, and ultimately reduce HIV incidence through treatment as prevention, expanding HIV testing in the United States is critical [23]. Besides fully implementing the guidelines for routine HIV screening [1, 2], other approaches suggested include identification through analysis of transmission clusters and partner notification [23]. In addition, persons at high risk for HIV such as MSM should test annually or more frequently (1).
The analyses were subject to limitations in the measure for assessing trend over time. Misclassification of late diagnosis may occur when the date of first HIV diagnosis is inaccurate or reporting of CD4 count <200 cells/mL or opportunistic illness is incomplete. However, stage 3 (AIDS) reporting is mandatory in all U.S. jurisdictions, and overall the proportion with stage 3 at diagnosis was similar in our analysis compared to that for jurisdictions with complete laboratory reporting of all HIV-related tests in 2012 [11]. Assessing trends in late diagnosis over time may also be affected by HIV reporting as it affects the numerator and denominator [24, 25]. This may make stable trends more difficult to interpret as case finding may mask changes in late diagnosis; however, despite this potential limitation, we found significant decreases in late diagnosis, which is supported by modeling results on diagnosis delay [18]. Finally, some cases may have been misclassified as late diagnoses when diagnosis was made shortly after seroconversion, when CD4 counts may temporarily drop to low levels. However, the percentage of persons diagnosed during acute HIV infection is expected to be very small.
In summary, during the past decade, the percentage of persons with a late HIV diagnosis decreased overall and in many individual areas with high HIV burden. However, even in areas with intensified HIV testing interventions, about 1 in 5 persons had advanced disease at the time of HIV diagnosis. In addition, there were disparities by race/ethnicity and transmission risk group in some areas. Sustained testing efforts may help to continue the decreasing trend in late-stage HIV diagnosis. There is evidence that the level of federal funding for testing is correlated with the percentage of persons who reported testing within the past 2 years [26]. Targeting such testing to areas and populations with high HIV burden can provide opportunities for early care and treatment and potential reduction in risk of HIV transmission.
References
Branson BM, Handsfield HH, Lampe MA, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR. 2006;55(9):1–17.
Moyer VA. U.S. preventive services task force. screening for HIV: U.S. Preventive services task force recommendation statement. Ann Intern Med. 2013;159(1):51–60.
Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. Department of Health and Human Services. May 1, 2014:D1-E47. Available at: http://www.aidsinfo.nih.gov/contentfiles/lvguidelines/adultandadolescentgl.pdf.
Centers for Disease Control and Prevention. Expanded testing program—overview. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; August 2011.
Centers for Disease Control and Prevention. High-impact HIV prevention: CDC’s approach to reducing HIV infections in the United States. Available at: http://www.cdc.gov/hiv/policies/hip.html. Accessed March 17, 2015.
Health Resources and Services Administration. HRSA care action: high-impact prevention. Available at: http://hab.hrsa.gov/deliverhivaidscare/files/high_impact_prevention.pdf. Accessed March 17, 2015.
Hutchinson AB, Farnham PG, Duffy N, et al. Return on public health investment: CDC’s expanded HIV testing initiative. J Acquir Immune Defic Syndr. 2012;59(3):281–6.
Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. NEJM. 2011;365(6):493–505.
Centers for Disease Control and Prevention. HIV testing trends in the United States, 2000–2011. Atlanta, GA: U.S. Department of Health and Human Services, January 2013:1–35. Available at: http://www.cdc.gov/hiv/pdf/testing_trends.pdf. Accessed March 17, 2015.
Cooley LA, Oster AM, Rose CE, et al. Increases in HIV testing among men who have sex with men—national HIV behavioral surveillance system, 20 U.S. metropolitan statistical areas, 2008 and 2011. PLoS ONE. 2014;9(9):e104162. doi:10.1371/journal.pone.0104162.
Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas—2012. HIV Surveillance Supplemental Report 2014;19(3). http://www.cdc.gov/hiv/library/reports/surveillance/. Published November 2014. Accessed February 4, 2015.
Centers for Disease Control and Prevention. HIV surveillance report, 2013; 25:76. Available at: http://www.cdc.gov/hiv/library/reports/surveillance/. Published February 2015. Accessed May 17, 2015.
Valdiserri RO, Forsyth AD, Yakovchenko V, Koh HK. Measuring what matters: development of standard HIV core indicators across the U.S. Department of Health and Human Services. Public Health Rep. 2013;128(5):354–9.
U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Healthy People 2020 Objectives. HIV-9 Reduce the proportion of persons with a diagnosis of Stage 3 HIV (AIDS) within 3 months of diagnosis of HIV infection. Available at: https://www.healthypeople.gov/2020/topics-objectives/topic/hiv/objectives. Accessed March 17, 2015.
Selik RM, Mokotoff ED, Branson B, Owen SM, Whitmore S, Hall HI. Revised surveillance case definition for HIV infection—United States, 2014. MMWR. 2014;63(RR03):1–10.
Office of Management and Budget. Revised definitions of metropolitan statistical areas, new definitions of micropolitan statistical areas and combined statistical areas, and guidance on uses of the delineations of these areas. OMB Bulletin 13-01. http://go.usa.gov/vSyB. Published February 28, 2013. Accessed December 1, 2014.
McDavid Harrison K, Kajese T, Hall HI, Song R. Risk factor redistribution of the national HIV/AIDS surveillance data: an alternative approach. Public Health Rep. 2008;123(5):618–27.
Hall HI, Song R, Szwarcwald CL, Green T. Time from infection with the human immunodeficiency virus to diagnosis, United States. J Acquir Immune Defic Syndr. 2015;6992:248–51.
Lesko CR, Cole SR, Zinski A, Poole C, Mugavero MJ. A Systematic review and meta-regression of temporal trends in adult CD4+ cell count at presentation to HIV care, 1992–2011. Clin Infect Dis. 2013;57(7):1027–37.
Gray KM, Branson B, Donnell DJ, Beauchamp G, Hu X, Wang Z, El Sadr W, Hall HI. HIV testing in six US cities using behavioral surveillance data for the TLC-Plus (HPTN 065) study. XIX International AIDS Conference. Washington, 2012 [abstract TUPE 293].
Centers for Disease Control and Prevention. Results of the expanded HIV testing initiative—25 Jurisdictions, United States, 2007–2010. MMWR. 2011;60(24):805–10.
Cooley LA, Wejnert C, Rose CE, Paz-Bailey G, National HIV. Behavioral surveillance study group. Increases in recent HIV testing among men who have sex with men coincide with the centers for disease control and prevention’s expanded testing initiative. Clin Infect Dis. 2015;60(3):483–5.
Burns DN, DeGruttola V, Pilcher CD, et al. Toward an endgame: finding and engaging people unaware of their HIV-1 infection in treatment and prevention. AIDS Res Hum Retrovir. 2014;30(4):217–24.
Xia Q, Kobrak P, Wiewel EW, Torian LV. The high proportion of late HIV diagnoses in the USA is likely to stay: findings from a mathematical model. AIDS Care. 2015;27(2):206–12.
Xia Q, Torian LV, Shepard CW. Limitations of Indicators of HIV case Finding. Epidemiology. 2015;26(1):e6–8.
Hayek S; Dietz PM, Van Handel M, et al. Centers for Disease Control and Prevention funding for HIV testing associated with higher state percentage of persons tested. J Public Health Manag Pract. 2015 Feb 12. [Epub ahead of print].
Disclaimer
The findings and conclusions in this study are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hall, H.I., Tang, T. & Espinoza, L. Late Diagnosis of HIV Infection in Metropolitan Areas of the United States and Puerto Rico. AIDS Behav 20, 967–972 (2016). https://doi.org/10.1007/s10461-015-1241-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-015-1241-5