Abstract
Women who experience intimate partner violence (IPV) are at increased risk for HIV infection. To further the understanding of the dyadic factors that impact condom use among women, we investigated the impact of three relationship factors (i.e., power, fear, and dependence) on the association between HIV-related information, motivation, and behavioral skills [constructs from the information-motivation-behavioral skills (IMB) model] and condom use among abused women. Data from 133 urban, low-income women recruited from several community-based agencies (e.g., domestic violence agencies, women’s health organizations, hospitals, Department of Health and Human Services, and Family Court) showed that these women experienced high levels of IPV and that relationship power, fear of abuse, and partner dependence were all associated with condom use. Multivariable models revealed that fear of abuse and partner dependence moderated the association between IMB constructs and condom use but relationship power did not. Results highlight the critical need to incorporate strategies to address relationship factors in HIV prevention programs with abused women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There are over 1.1 million Americans currently living with HIV infection, of which nearly 25 % are women [1]. In 2010, the incidence of HIV infection among heterosexual women was approximately 8000 (17 % of all new cases) [2]. To reduce the incidence, continued sexual risk reduction is essential, especially among the most vulnerable population sub-groups [3, 4].
Women who experience intimate partner violence (IPV) are at elevated risk for HIV infection [5]. The association between IPV and HIV infection has been shown in both cross-sectional [6] and prospective trials [5]. Approximately 12–22 % of incident HIV infections among women are a result of their experiences of IPV [7, 8]. The World Health Organization recognizes both direct and indirect means of HIV transmission in women with histories of IPV [9]. Direct risk occurs from forced sex (e.g., vaginal trauma) whereas indirect risk stems from inability to negotiate safer sex practices, engaging in sexual risk taking, abusive men’s sexual risk behaviors, and delay in HIV testing.
In order to design effective HIV risk reduction interventions for abused women, we need to better understand factors that influence their sexual risk behaviors (e.g., having more than one sexual partner; having unprotected sex) and subsequent HIV acquisition. Several health behavior models have been used to understand women’s sexual risk behavior [10]. The information-motivation-behavioral skills model (IMB) has been used extensively in HIV prevention interventions. The IMB model postulates that sexual risk behavior is predicted by an individual’s knowledge concerning sexually transmitted diseases (STDs) including HIV, their motivation to engage in sexually safe behaviors, and their skills in negotiating safer sex behaviors with their partner(s) [11]. Although the IMB model predicts HIV risk behavior in a variety of populations, research has highlighted its limitations in predicting sexual risk behavior among abused women. This research suggests the need for considering other contextual factors [12, 13].
Dyadic factors that influence sexual risk behaviors among women include relationship power [13], fear of abuse when negotiating condoms [12], and partner dependence (economic, social, and emotional) [14]. Relationship power refers to the extent to which one person can influence and control their partner’s behavior and dominate decision-making within the dyad [13, 15, 16]. Relationship power is of particular concern in abusive relationships given the potential for violence [12]. Fear of abuse refers to the inability to negotiate safe sex practices based upon fear of potentially adverse responses to such requests [6]. This often results in the inability to negotiate condom use [6]. Partner dependence can be economic, social, and/or emotional and often results in an inability for women to leave their abusive partner [17, 18].
The purpose of the current study is to investigate the role of relationship variables in explaining HIV risk among women with a history of IPV. Specifically, we sought to test two hypotheses: [1] relationship power, fear of abuse when negotiating condoms, and partner dependence will undermine condom use, and [2] these relationship variables will moderate the relation between the constructs of the IMB model and condom use.
Methods
Participants
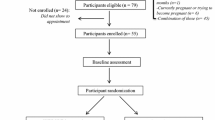
Participants (n = 177) were recruited from community-based agencies (e.g., domestic violence agencies, women’s health organizations, hospitals, Department of Health and Human Services, and Family Court) in upstate New York. All were enrolled in an exploratory clinical trial designed to evaluate a sexual risk reduction intervention for abused women. Criteria for inclusion in the study included: age 18 or older; heterosexual, HIV negative, having experienced IPV (physical, emotional, or sexual) in the past 3 months; and having engaged in risky sexual behavior in the past 3 months.
Procedures
A trained research assistant (RA) recruited participants by attending community meetings and support groups as well as by approaching women in the waiting room of social service agencies. Staff at these agencies also referred their clients to the RA. The RA informed interested women about the study procedures and screened them for eligibility. Eligible women who agreed to participate provided contact information and scheduled an appointment to complete the study questionnaire. After signing the informed consent on the day of their appointment, the women filled out a calendar of events for the past 3 months to improve their recall when answering survey questions. They went on to complete an audio, computer-assisted self-interview (ACASI). The participants were compensated for their time and were given a list of community resources. All procedures were approved by the Institutional Review Board of participating institutions.
Measures
Demographics
Participants self-reported their age, sex, race, ethnicity, education, employment status, income, and HIV status.
Information
The brief HIV Knowledge Scale (HIV-KQ-18) was used to assess participants’ HIV-related knowledge [19–21]. Options for answering the 18 questions were “yes,” “no,” and “don’t know.” Examples of the items include “Can coughing and sneezing spread HIV” and “Is there a vaccine that can stop adults from getting HIV.” The percentage of correct responses was calculated with higher percentages indicating higher levels of HIV knowledge (α = 0.84).
Motivation
Condom Attitude Scale was adapted from two existing scales and contains 6-items [22, 23]. These items were rated on 6-point scales (1 = strongly disagree to 6 = strongly agree). Examples of items are “A condom is uncomfortable” and “Sex with a condom can still be pleasurable.” Items were averaged to calculate a condom attitudes score, with higher scores indicating more positive condom attitudes (α = 0.70).
Behavioral Skills
The Self-Efficacy with Steady Partner Scale was used to assess how comfortable the participants felt discussing safer sex practices with their steady partner [24]. This was done through the use of two scenarios with six corresponding questions that covered six areas of self-efficacy (ability to have safer sex conversation, convince partner to engage in safer sex practices, to refuse sex without condoms, to discuss STDs and HIV, to only engage in oral sex, to avoid substance and alcohol use). Each item was rated on an 11-point scale (0-10), which indicated how confident the participant felt about performing each behavior in the given scenarios. We calculated an average across the two scenarios with greater scores indicating more confidence in enacting sexual risk-reduction behaviors (α = 0.86).
Relationship Power
The Sexual Relationship Power Scale (SRPS; 16) was used to measure relationship power and modified as suggested by Pulerwitz and colleagues (19 items; α = 0.91). This measure has two sub-scales. The relationship control subscale consists of 15-items based on a 4-point Likert scale, 1 (Strongly agree) to 4 (Strongly disagree). The score range for this subscale is 15–60. The decision-making dominance subscale consists of 8-items that are scored by 1 (your partner), 2 (both of you equally), and 3 (you). The score range is 8–24. In order to attain the overall score for this measure, the mean scores were calculated for each subscale. The mean scores were then rescaled to a range of 1–4 thus, giving both subscales the same range. The following formula was used for this procedure: (Subscale score-minimum range)/(Maximum of range − Minimum of range) × 3 + 1. Mean scores for the subscales were combined with equal weighting into an overall score. The following formula was used to create the overall Sexual Relationship Power Scale (SRPS): (Overall scale score − minimum of range)/(Maximum of range − Minimum of range) × 3 + 1.
Fear of Abuse
The Fear of Abuse measure assessed individuals’ fear of abuse regarding negotiating condom use with their partner [25, 26]. It consists of 8-items, scored from 0 (never) to 4 (always). Examples of the items are “I have been worried that if I talked about using condoms with my steady partner he would threaten to hit me” and “I have been worried that if I talked about using condoms with my steady partner he would go out with other girls.” The total score was calculated by summing the score for each item. Higher scores indicate a greater fear of abuse in response to suggesting condom use with steady partner (α = 0.95).
Partner Dependence
The partner dependence scale contains six items that are designed to assess an individual’s economic, safety, or emotional dependence on a partner [14]. Each item is based on a 6-point scale to indicate how strongly they agree with the provided statements. Examples of the items are “I need a partner to pay my bills” and “Having a partner helps me feel special as a person.” To attain the measure total score, the items scores are averaged. A higher score indicates a higher dependence on their partner (α = 0.80).
Intimate Partner Violence
The abuse behavior inventory (ABI) is a 29-item scale constructed to assess sexual, psychological, and physical abuse [27]. Participants responded on a 5-point Likert scale, 0 (never) to 4 (very frequently), how frequently they experienced each type of abuse in the last 3 months. Example items are “Pressured you to have sex in a way that you didn’t like or want”, “Threatened to hit or throw something at you”, and “Became very upset with you because dinner, housework, or laundry was not ready when he wanted it or done the way he thought it should be.” Items were summed to calculate a total scale score (α = 0.96).
Condom Use
The number of episodes of unprotected sex was calculated by summing the reported number of times participants engaged in unprotected anal or vaginal sex with their steady partner in the last 3 months. The proportion of episodes of unprotected sex was calculated using the formula: (unprotected anal + unprotected vaginal sex episodes)/(total vaginal and anal sex episodes).
Data Analyses
All study variables were inspected for outliers. The number of episodes of unprotected sex was trimmed by changing scores that were more than 3 times the interquartile range (IQR) from the 75th percentile to 3 times the IQR plus one. Analyses were conducted on participants who reported having a steady partner in the last 3 months (n = 133). A steady partner was defined as a sexual partner to whom the participant was closest to including their husband, a boyfriend, or a sexual partner that they really cared about. All continuous predictor variables were centered prior to analysis.
To create dichotomous variables for our moderators, we split the women by the mean of each relationship variable, creating low and high groups for each moderator.
To determine potential covariates, we conducted aggregated Pearson scaled logistic regressions and Pearson scaled logistic regression to determine continuous and dichotomous covariates respectively that would be associated with the proportion of episodes of unprotected sex. We used negative binomial regressions for the number of episodes of unprotected sex. Pearson scaled logistic regressions and negative binomial regressions were used to account for overdispersion within the data. Covariates were included in further analyses if significantly associated with the dependent variable at p < 0.05.
To determine whether relationship variables were associated with condom use, we ran aggregated Pearson scaled logistic regression with proportion of episodes of unprotected sex and negative binomial regression with number of episodes of unprotected sex as the outcomes. Two-sample t tests were conducted to determine group differences between women in low and high levels of moderators and the outcome measures (number of episodes of unprotected sex and proportion of number of episodes of unprotected sex).
To determine whether relationship variables moderated the relationship between IMB constructs and proportion of episodes of unprotected sex, we first conducted aggregated Pearson scaled logistic regressions to establish if IMB constructs were related to the proportion of episodes of unprotected sex. In these analyses, proportion of episodes of unprotected sex was the dependent variable, and HIV knowledge, condom attitudes, and self-efficacy with steady partner were the independent variables. Second, we conducted additional aggregated Pearson scaled logistic regression with proportion of episodes of unprotected sex as the dependent variable and the IMB constructs, each of the three moderators, and interaction terms as the independent variables. This resulted in 9 separate models (e.g., a. HIV knowledge, relationship power, and interaction between HIV knowledge and relationship power; b. condom attitudes, relationship power, and interaction between condom attitudes and relationship power; c. self-efficacy with steady partner, relationship power, and interaction between self-efficacy with steady partner and relationship power) with proportion of episodes of unprotected sex as the dependent variable in each of these models.
To determine whether relationship variables moderated the relationship between IMB constructs and number of episodes of unprotected sex, we first conducted negative binomial regressions to establish if IMB constructs were related to number of episodes of unprotected sex in our sample. In these analyses, number of episodes of unprotected sex was the dependent variable, and HIV knowledge, condom attitudes, and self-efficacy with steady partner were the independent variables. Second, we conducted additional negative binomial regressions with number of episodes of unprotected sex as the dependent variable and the IMB constructs, each of the three moderators, and interaction terms as the independent variables. This resulted in 9 separate models (e.g., a. HIV knowledge, relationship power, and interaction between HIV knowledge and relationship power; b. condom attitudes, relationship power, and interaction between condom attitudes and relationship power; c. self-efficacy with steady partner, relationship power, and interaction between self-efficacy with steady partner and relationship power) with number of episodes of unprotected sex as the dependent variable in each of these models.
A significant interaction between any modifier and IMB construct would indicate that the moderator altered the relationship between the IMB construct and the dependent variables. Given the number of analyses conducted to test each modifier, we applied the Bonferroni multiple comparisons corrections to minimize Type I error (α = 0.05/number of analyses, 3). This results in a p value < 0.0167 for a moderated analysis to be significant.
Results
The mean age of the participants was 35 (SD = 10.2, range = 19–62). Approximately half of the participants were African-American (n = 60, 45 %) and 48 were White (36 %). Approximately one-quarter of participants had a high school education or less (28 %) and the majority were unemployed (n = 89, 67 %) with an annual income of less than $15,000 per year (n = 83, 63 %). Forty-six percent reported never being married (n = 61). Average number of episodes of unprotected sex in the last 3 months was 20 (SD = 24.9) and the average proportion of episodes of unprotected sex in the last 3 months was 73 % (SD = 38 %). Mean HIV knowledge score was 73 % (SD = 21 %), condom attitudes was 4.6 (SD = 0.98), and self-efficacy with steady partner was 6.68 (SD = 2.79). Mean scores on relationship power was 2.30 (SD = 0.66), fear of abuse with steady partner was 11.83 (SD = 10.2), and partner dependence was 3.14 (SD = 1.26). The mean ABI score was 54.6 (SD = 29.28). Sample characteristics are found in Tables 1 and 2.
Bivariate Analyses
Proportion of Episodes of Unprotected Sex
Black participants reported a lower proportion of episodes of unprotected sex compared to White participants (β = −1.79, SE = 0.52, p < 0.0005). Respondents with some college or a college degree reported a greater proportion of episodes of unprotected sex, as compared to participants who had less than high school or a high school degree (β = 1.94, SE = 0.41, p < 0.0001). Those that were unemployed had a greater proportion of unprotected sexual episodes than those that were employed (β = 1.74, SE = 0.36, p < 0.0001). Participants who were married at some point in their lives reported a higher proportion of unprotected sex episodes than those who were single, never married (β = 1.12, SE = 0.37, p = 0.0027). Participants with an income of higher than $15,000 annually had a lower proportion of unprotected sexual episodes compared to participants with an income of lower than $15,000 annually (β = −1.30, SE = 0.46, p = 0.0047). Participants with higher scores on the violence measure had a lower proportion of unprotected sexual episodes compared to participants with lower IPV scores (β = −0.03, SE = 0.01, p < 0.0001). However, we saw no differences in the proportion of episodes of unprotected sex based on age (β = −0.02, SE = 0.03, p = 0.45). Therefore, race, education, employment, marital status, income, and IPV score were included as covariates in all models for the proportion of unprotected sexual episodes.
Number of Episodes of Unprotected Sex
No covariates were associated with number of episodes of unprotected sex (all p values > 0.05, see Supplement I). Therefore, no covariates were included in models predicting number of unprotected sexual episodes.
Relationship Variables and Condom Use
Proportion of Episodes of Unprotected Sex
Aggregated Pearson scaled logistic regression models showed that all three relationship variables were significantly associated with the proportion of episodes of unprotected sex: relationship power (β = −0.89, SE = 0.30, p = 0.003), fear of abuse when negotiating condoms (β = −0.08, SE = 0.02, p < 0.001), and partner dependence (β = −0.49, SE = 0.11, p < 0.01). Low relationship power scores were significantly associated with higher proportion of episodes of unprotected sex (M = 81 %, SD = 33 %) as compared to high relationship power scores (M = 64 %, SD = 42 %; t(119) = 2.51, p = 0.01). Women with high fear of abuse when negotiating condoms reported a higher proportion of episodes of unprotected sex (M = 78 %, SD = 35 %) as compared to women with low fear of abuse (M = 70 %, SD = 39 %; t (115.35) = −1.24, p = 0.22). Women with high partner dependence reported a higher proportion of episodes of unprotected sex (M = 78 %, SD = 36 %) as compared to women with low partner dependence (M = 68 %, SD = 39 %; t (111.02) = −1.33, p = 0.19). However neither the relationship power or partner dependence group differences were significant.
Number of Episodes of Unprotected Sex
Negative binomial regression models revealed that partner dependence was significantly associated with the number of episodes of unprotected sex (β = 0.20, SE = 0.10, p = 0.049) but relationship power and fear of abuse when negotiating condoms were not. Women with high partner dependence scores had higher episodes of unprotected sex (M = 21.8, SD = 25.8) than women with low partner dependence (M = 17.8, SD = 24.0; t (124.92) = −0.91, p = 0.37). This difference was not significant.
Moderators of the Relation Between IMB Constructs and Condom Use
Proportion of Episodes of Unprotected Sex
Relationship Power
In the adjusted analyses for the main effects of HIV knowledge and relationship power, and the interaction of HIV knowledge and relationship power, only the main effect for relationship power was significant (β = −1.98, SE = 0.51, p = 0.0001). There was no significant main effect for HIV knowledge or for the interaction of HIV knowledge and relationship power. Similar results were seen in the models for motivation (condom attitudes) and behavioral skills (self-efficacy with main partner) with relationship power being the only significant variable in the models (β = −1.99, SE = 0.52, p = 0.0001 and β = −1.96, SE = 0.48, p < 0.0001, respectively). Results are shown in Table 3.
Fear of Abuse
In the adjusted analyses for the main effects of HIV knowledge and fear of abuse, and the interaction between HIV knowledge and fear of abuse, only the interaction term was significant (β = 0.37, SE = 0.08, p < 0.0001). Further analysis showed that among women who reported high fear of abuse in response to condom negotiation, as HIV knowledge increased there was a significant increase in the proportion of episodes of unprotected sex. This association was not observed among women who reported low fear of abuse in response to condom negotiation. Stratified analyses are shown in Table 4.
Similarly, in the models of condom attitudes and self-efficacy with steady partner, only the interactions between condom attitudes and fear of abuse (β = 0.07, SE = 0.02, p < 0.0001) and self-efficacy with steady partner and fear of abuse (β = 0.03, SE = 0.01, p < 0.0001) were significant. Stratified analyses showed that among women who reported high fear of abuse in response to condom negotiation, as condom attitudes became more favorable there was a significant increase in the proportion of episodes of unprotected sex. This association was not observed among women who reported low fear of abuse in response to condom negotiation. Also, among women who reported high fear of abuse in response to condom negotiation, as self-efficacy with their steady partner increased there was a significant increase in the proportion of episodes of unprotected sex. This association was not observed among women who reported low fear of abuse in response to condom negotiation. Results are shown in Table 5.
Partner Dependence
In the adjusted analyses for the main effects of HIV knowledge and partner dependence, and the interaction between HIV knowledge and partner dependence, only the interaction term was significant (β = 2.84, SE = 0.66, p < 0.0001). Stratified analysis showed that among women who reported high partner dependence, as HIV knowledge increased there was a significant increase in the proportion of episodes of unprotected sex. This association was not observed among women who reported low partner dependence. Stratified analyses are shown in Table 6.
Similarly, in the models of condom attitudes and self-efficacy with steady partner, only the interactions between condom attitudes and partner dependence (β = 0.48, SE = 0.17, p = 0.005) and self-efficacy with steady partner and partner dependence (β = 0.25, SE = 0.05, p < 0.0001) were significant. Further analyses showed that among women who reported high partner dependence, as condom attitudes became more favorable there was a significant increase in the proportion of episodes of unprotected sex. This association was not observed among women who reported low partner dependence. Further, among women who reported high partner dependence, as self-efficacy with their steady partner increased there was a significant increase in the proportion of episodes of unprotected sex. Among women who reported low partner dependence, as self-efficacy with their steady partner increased there was a significant decrease in the proportion of episodes of unprotected sex. Results are shown in Table 7.
Number of Episodes of Unprotected Sex
Analyses for the main effects for the IMB constructs (HIV knowledge, condom attitudes, and self-efficacy with steady partner), the moderators (relationship power, fear of abuse, and partner dependence), and the interaction terms between the moderators and IMB constructs resulted in no significant associations with the number of episodes of unprotected sex (all p > 0.0167, see Supplement II, III, and IV).
Discussion
Given the widespread use of the IMB model in predicting sexual behavior among women and findings highlighting the limitations of this model in conceptualizing sexual risk behavior among abused women, we investigated relational factors and their association with condom use among abused women. Further, we studied how these relationship variables might moderate the impact of IMB constructs on condom use among abused women. Women in this study reported high levels of IPV and a high proportion and number of episodes of unprotected sex with their steady partners.
Consistent with previous research, low relationship power, greater fear of abuse when negotiating condoms, and high partner dependence were associated with a greater proportion of episodes of unprotected sex with a steady partner [6, 14, 28, 29]. These results confirm the importance of attending to relationship factors such as power, fear, and dependence in addition to the experiences of violence in heterosexual relationships and the impact they have on condom use in steady relationships.
Results show that relationship power did not moderate the association between the IMB constructs and condom use in this population. However, given the repeated direct significant associations between relationship power and condom use in these models, we contend that relationship power has a critical impact on abused women’s ability to practice safer sex. The main effects for relationship power consistently showed that as relationship power increased, regardless of abused women’s HIV related information, motivation, or behavioral skills, their proportion of episodes of unprotected sex with a steady partner decreased. This finding has important implications because it suggests that among abused women assessment of relationship power could provide clinically relevant information about their ability to practice safer sex in the context of abusive relationships. Further, given the independent contribution of relationship power on condom use among abused women, it would be essential to incorporate relationship power dynamics in HIV prevention interventions with abused women.
Moderation analysis involving fear of abuse when negotiating safe sex practices confirmed findings of previous research [26, 28]. Results indicated that among women who reported high fear of abuse when negotiating condoms even as their HIV knowledge increased, condom attitudes become more favorable, and self-efficacy with steady partner increased, there was a significant increase in unprotected sex episodes. Among women who experienced high fear of abuse when negotiating condoms, a 5 unit increase in HIV knowledge was associated with 1 unit increase in proportion of episodes of unprotected sex with steady partner in the last 3 months. Similarly, in models involving condom attitudes and self-efficacy as measures of HIV motivation and behavioral skills respectively, among women who experienced high fear for every 1 unit increase in positive attitudes towards condom and for a .44 unit increase in self-efficacy there was 1 unit increase in proportion of episodes of unprotected sex. It is important to note that among abused women even after controlling for their experiences of physical, emotional, and sexual violence, the fear that they experience in response to condom negotiation significantly impacts their practice of safer sex. Despite having high levels of HIV related knowledge, motivation, and behavioral skills that have been deemed necessary for reducing one’s risk for HIV, these constructs are not protective for women who experience high fear.
In the final models involving partner dependence, IMB constructs, and condom use results were similar to those in the previous models involving fear of abuse. Women who reported high partner dependence also reported greater proportion of episodes of unprotected sex even as there was an increase in their HIV related knowledge, positive attitudes towards condoms, and self-efficacy with their steady partner. For every 5 point increase in HIV related knowledge, 1 unit increase in positive attitudes towards condoms, and .47 unit increase in self-efficacy with steady partner, there was a subsequent 1 unit increase in proportion of episodes of unprotected sex in each of these models. These results are in contrast to prior research where partner dependence did not modify the relationship between IMB constructs and condom use [14]. However, Senn and colleagues’ analysis was not focused on abused women.
Our findings have important implications for understanding abused women’s sexual risk-taking behaviors and for the development of risk reduction interventions for this group. The results highlight that relationship dynamics such as relationship power, fear of abuse when negotiating condoms, and partner dependence overpower individual-level determinants of HIV risk among abused women even after controlling for their experiences of physical, emotional, and sexual abuse. The results emphasize the need to not only assess women’s experiences of violence but also the nature of their relationship dynamics and moving beyond activities that enhance women’s HIV related knowledge, motivation, and behavioral skills needed to practice safer sex. Greater attention needs to be paid to developing HIV prevention and intervention programs that integrate women’s experiences of IPV and relationship dynamics.
Strengths of this study include the use of a diverse and reasonably large sample of community-based women with recent experiences of IPV. The study demographic reflected the population demographic of a medium-sized city in upstate New York; therefore, generalizability may be limited. We included abused women who had engaged in sexual risk behavior in the past 3 months to participate in the study. It is possible that for some abused women the decision to engage in unprotected sex was influenced by their desire to foster intimacy by having unprotected sex or eroticizing unprotected sex. Also, earlier research has shown that having unprotected sex is a sign of trust and commitment in the relationship [30]. Recently, pre-exposure prophylaxis (PrEP) has been recommended for use among populations at high-risk for HIV infection [31]. We did not assess the use of PrEP in this study. While this may limit our findings, we anticipate a low PrEP use in this community-based sample of women. Additional limitations include the reliance upon self-report and use of cross-sectional data. Despite these limitations, our findings highlight the importance of relational factors with respect to condom use among abused women. Women with a history of IPV are at increased risk for HIV infection and steps must be taken to protect this vulnerable population.
References
Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 U.S. dependent areas- 2010. HIV Surveillance Supplemental Report. 2012; 17(3a). www.cdc.gov/hiv/surveillance/resources/reports/2010supp_vol17no3/. Accessed 13 Nov 2013.
Centers for Disease Control and Prevention. Estimated HIV incidence in the United States, 2007–2010. HIV Surveillance Supplemental Report. 2012; 17(4). http://www.cdc.gov/hiv/pdf/statistics_hssr_vol_17_no_4.pdf. Accessed 28 Oct 2013.
Adimora AA, Ramirez C, Auerbach JD, et al. Preventing HIV infection in women. J Acquir Immune Defic Syndr. 2013;63:S168–73.
Sweet T, Polanksy M, Welles SL. Mediation of HIV/STI risk by mental health disorders among persons living in the United States reporting childhood sexual abuse. J Acquir Immune Defic Syndr. 2013;62(1):81–9.
Kouyoumdjian FG, Findlay N, Schwandt M, et al. A systematic review of the relationships between intimate partner violence and HIV/AIDS. PLoS One. 2013;8(11):1–25.
Mittal M, Stockman JK, Seplaki CL, et al. HIV risk among women from domestic violence agencies: prevalence and correlates. J. Assoc Nurses AIDS Care. 2013;24(4):322–30.
Jewkes RK, Dunkle K, Nduna M. et al. Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: A cohort study. Lancet. 2010; 376:41–48.
Kouyoumdjian FG, Calzavara LM, Bondy SJ, et al. Intimate partner violence is associated with incident HIV infection in women in Uganda. AIDS. 2013;27:1331–8.
World Health Organization. Violence against women and HIV/AIDS: Critical intersections—intimate partner violence and HIV/AIDS. Bulletin 1. Geneva Switzerland: World Health Organization; 2004.
Airhihenbuwa CO, Obregon R. A critical assessment of theories/models used in health communication for HIV/AIDS. J Health Commun. 2000;5:S5–15.
Fisher JD, Fisher WA, Shuper PA. Chapter 2: the information-motivation-behavioral skills model of HIV preventive behavior. In: Diclemente RJ, Crosby RA, Kegler MC, editors. Emerging theories in health promotion practice and research. 2nd ed. San Francisco: Jossey-Bass; 2009. p. 21–63.
Mittal M, Senn TE, Carey MP. Intimate partner violence and condom use among women: does the information-motivation-behavioral skills (IMB) model explain sexual risk behavior? AIDS Behav. 2012;16(4):1011–9.
Harvey SM, Bird ST, Galavotti C, et al. Relationship power, sexual decision making, and condom use among women at risk for HIV/STDS. Women Health. 2002;36(4):69–84.
Senn TE, Carey MP, Vanable PA, et al. Partner dependence and sexual risk behavior among STI clinic patients. Am J Health Behav. 2010;34(3):257–66.
Blanc AK. The effect of power in sexual relationships on sexual and reproductive health: an examination of the evidence. Stud Fam Plann. 2001;32(3):189–213.
Pulerwitz J, Amaro H, DeJong W, et al. Relationship power, condom use and HIV risk among women in the USA. AIDS Care. 2002;14(6):789–800.
Anderson KL. Theorizing gender in intimate partner violence research. Sex Roles. 2005;52(11/12):853–65. doi:10.1007/s11199-005-4204-x.
Bornstein RF. The complex relationship between dependency and domestic violence: converging psychological factors and social forces. Am Psychol. 2006;61(6):595–606.
Carey MP, Morrison-Beedy D, Johnson BT. The HIV-knowledge questionnaire: development and evaluation of a reliable, valid, and practical self-administered questionnaire. AIDS Behav. 1997;1:61–74.
Carey MP, Morrison-Beedy D, Johnson BT. The HIV-knowledge questionnaire. In: Davis CM, Yarber WL, Bauserman R, Schreer G, Davis SL, editors. Handbook of sexually-related measures. Thousand Oaks: Sage; 1998. p. 313–5.
Carey MP, Schroder KEE. Development and psychometric evaluation of the brief HIV knowledge questionnaire. AIDS Educ Prev. 2002;14:172–82.
Brown IS. Development of a scale to measure attitude toward the condom as a method on birth control. J Sex Res. 1984;20:255–63.
Sacco WP, Levine B, Reed DL, Thompson K. Attitudes about condom use as an AIDS-relevant behavior: their factor structure and relation to condom use. Psychol Assess. 1991;3(2):265–72.
National Institute of Mental Health Multisite HIV Prevention Trial Group, Murphy DA, Stein JA, Schlenger W, Maibach E. Conceptualizing the multidimensional nature of self-efficacy: assessment of situational context and level of behavioral challenge to maintain safer sex. Health Psychol. 2001;20:281–90.
Wingood GM, DiClemente RJ. Partner influences and gender-related factors associated with noncondom use among young adult African American women. Am J Community Psychol. 1998;26:29–51.
Raiford JL, DiClement RJ, Wingood GM. Effects of fear of abuse and possible STI acquisition on the sexual behavior of young African American women. Am J Public Health. 2009;99:1067–71.
Zink T, Klesges LM, Levin L, Putnam F. Abuse behavior inventory: cutpoint, validity, and characterization of discrepancies. J Interpers Violence. 2007;22:921–31.
Seth P, DiClemente RJ, Lovvorn AE. State of the evidence: intimate partner violence and HIV/STI risk among adolescents. Curr HIV Res. 2013;11:528–35.
Ulibarri MD, Roesch S, Rangel MG, et al. ”Amar te Duele” (“Love hurts”): sexual relationship power, intimate partner violence, depression symptoms and HIV risk among female sex workers who use drugs and their non-commercial, steady partners in Mexico. AIDS Behav. 2014. doi:10.1007/s10461-014-0772-5.
Epperson MW, Platais I, Valera P, Barbieri R, Gilbert L, El-Bassel N. Fear, trust, and negotiationing safety: hIV risks for black female defendants. Affilia. 2009;24(3):257–71.
Pre-Exposure Prophylaxis (PrEP). Centers for Disease Control and Prevention Website. 2015. http://www.cdc.gov/hiv/prevention/research/prep/Updated. Accessed 29 June 2015.
Acknowledgments
We thank the participants who took part in this research and members of the research team. We also gratefully acknowledge Natalie Bea Slopen, ScD, for her review and comments on the manuscript and Xueya Cai, PhD and Kelly Thevenet-Morrison, MS, for their statistical guidance. This research was supported by NIH Grant # K01-MH080660.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
McGrane Minton, H.A., Mittal, M., Elder, H. et al. Relationship Factors and Condom Use Among Women with a History of Intimate Partner Violence. AIDS Behav 20, 225–234 (2016). https://doi.org/10.1007/s10461-015-1189-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-015-1189-5