Abstract
To understand associations between location of sex and sexual risk, it is most helpful to compare sexual encounters within persons. We systematically reviewed within-subjects comparisons of sexual encounters reported by men who have sex with men (MSM) with respect to location of sex. Within-subjects comparisons of sexual risk and location of sex were eligible if they collected data post-1996 from samples of MSM. We independently screened results and full-text records in duplicate. Of 6,336 deduplicated records, we assessed 138 full-text studies and included six, most of which compared unprotected anal intercourse against other anal intercourse. This small, but high quality, body of evidence suggests that associations between attendance at sex-on-premises venues and person-level sexual risk may be due to overall propensity towards unprotected sex. However, there may be some location factors that promote or are associated with serononconcordant unprotected anal intercourse. Health promoters may wish to focus on person-level characteristics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sex-on-premises venues (SOPV) are indoor locations outside the home where patrons engage in sex, often with casual partners [1]. SOPVs include bathhouses, saunas, sex clubs, porn cinemas and public sex parties. In contrast, public sex environments, also known as ‘cruising locations’ or ‘beats’, are another important class of location for anonymous sexual encounters and include places such as outdoor parks [2]. Both of these classes of locations are in contrast to encounters held in the homes of sexual partners. Across studies, use of SOPVs among men who have sex with men (MSM) appears frequent. One internet-recruited sample of MSM in 38 European countries showed that in the four weeks prior to survey completion, 30.5 % had visited an SOPV [3].
Use of certain locations for sex may be associated with specific sexual behaviours or with sexual risk-taking at the person level, that is, across different people. Qualitative research has long suggested that SOPVs are important places for sexual exploration [4], including where those venues also serve an important social role [5] and where these locations are also venues for substance use [6–8]. Quantitative studies consistently report person-level associations between SOPV attendance and sexual risk behaviour. Indeed, person-level associations between sexual risk behaviour and engagement in anonymous sex in SOPVs are not new [9]. Comparing New York City MSM recruited via various physical and online sites, MSM recruited in bathhouses reported the most encounters with anal intercourse in the last three months [10]. Of MSM sampled in commercial sex venues in Seattle, 14 % reported unprotected anal intercourse (UAI) and 9 % reported UAI with serononconcordant partners at the most recent visit [11]. SOPV attendance and HIV seropositive status may also be associated. This could be due either to increased risk of transmission through attendance at SOPVs, or due to increased attendance among MSM living with HIV, or both. Recently HIV-infected MSM in Seattle were more likely to have met partners through SOPVs than HIV-seronegative MSM [12]. Cross-sectional data from Belgium [13] also showed that MSM sampled in SOPVs were more likely to be HIV-seropositive (14.5 %) than MSM sampled at gay bars (4.9 %) or other social events (1.4 %).
Yet this evidence does not tell us specifically if sexual risk is greater in sex-on-premises venues as compared to other sexual locations. In order to understand ‘location effects’ on sexual risk, it is important to separate out person-level characteristics from the encounter-level characteristic of location of sex. Indeed, all of the above analyses examine person-level rather than encounter-level associations. That is, they examine associations between person-level use of specific sexual venues and person-level sexual risk behaviours, generally over a specific retrospective time period. While these analyses are helpful in understanding behaviours across different people, they are not helpful in understanding what is happening within individual people at the level of the sexual encounter. To understand associations at the level of the sexual encounter, analyses should optimally compare several sexual encounters within respondents [14]. These analyses are known as within-subjects or within-person comparisons, or as ‘case-crossover analyses’, in that they use the person as their own control when encounters vary in terms of location and sexual risk behaviour outcomes. These analyses separate out the effects of person-level characteristics on the outcome variable.
Within-subjects analyses are helpful because they provide information on situational characteristics proximal to a sexual encounter, and may provide a more robust theoretical test of how situational characteristics may be associated with sexual behaviours. Key theories that aim to understand how sexual risk behaviour ‘happens’ focus on the level of the sexual encounter and address the role of situational characteristics, including venue. For example, highly stimulating sexual contexts of the sort experienced in an SOPV may be associated with relaxation of safer sex norms via cognitive escape [15]. Some evidence of the cognitive escape theory exists for substance use and sexual risk behaviour [16, 17]. More generally, specific situational characteristics, such as venue of sex, may interfere with risk appraisals proximal to sexual encounters [18].
Finally, SOPV-based health promotion has long been an important feature of HIV prevention efforts for these reasons and because of the sexual proximity within these locations of MSM reporting high-risk behaviours and MSM with low-risk sexual preferences [19, 20]. This proximity is important because it may facilitate the mixing of different socio-sexual networks with different prevalences and baseline risk levels for sexually transmitted infections [20]. As opposed to settings such as bars or smartphone apps, proximity in SOPVs as highly stimulating sexual contexts may prevent adequate risk appraisal, as discussed above. Though SOPV-based health promotion interventions are not without challenges, they have been found to be acceptable in large social venues, for example in London [21] and in various American cities [22]. Understanding location-specific sexual risk behaviours could inform future setting-based prevention efforts.
Because of the importance of understanding associations between location of sex and sexual risk, and because of the importance in examining the most robust encounter-level evidence on this association, our objective was to systematically review studies reporting within-subjects comparisons analysing the encounter-level association between location of sex and sexual risk behaviours in MSM.
Methods
Search Methods
In line with our review objective, studies were included if: (a) they conducted within-subjects comparisons of sexual encounters; (b) they only included encounters reported by MSM; and (c) they tested location of sex (as opposed to venue of partner meeting) as a predictor of sexual risk behaviours (generally UAI, but this is discussed below). We included studies reported as full-length journal articles or dissertations. Studies were excluded if they collected data before 1996, the year in which highly active antiretroviral therapy became widely available. Though search methods and inclusion/exclusion criteria were set a priori, we did not register a protocol for this review, as at the time of preparing this review systematic review registers did not accept protocols for reviews of observational studies in epidemiology.
On 9 July 2013, we searched MEDLINE with MEDLINE In-Process & Other Non-Indexed Citations, PsycINFO, Embase, CINAHL, ISI Web of Science, Sociological Abstracts, ASSIA, and Dissertations and Theses A&I, all through last update. We drew studies for this review from a broader evidence synthesis project that studied all within-subjects comparisons of sexual encounters in MSM in order to understand the current state of research on encounter-level determinants of sexual risk. Our search strategy included keyword and subject heading terms for MSM (to narrow results to the population), for encounter-level models (to narrow studies to within-subjects comparisons), and for HIV risk and safer sex outcomes (to capture studies examining sexual risk as an outcome). Studies were limited to after 1996 given the significant shift in the HIV risk landscape following development of antiretroviral therapy. We used the following strategy for MEDLINE, Embase and PsycINFO:
-
1.
(gay or bisexual or homosexual or queer or LGBT* or men who have sex with men or MSM).mp. or exp homosexuality/or exp homosexuality, male/or exp bisexuality/or exp transsexualism/or exp transvestism/
-
2.
(event$ or encounter$ or episode$ or (critical adj2 incident) or conditional logistic regression or multi-day or multiday or diary or association$).mp.
-
3.
(HIV or condom or (safe* adj2 sex*) or (unsafe* adj2 sex*) or (unprotected adj3 intercourse*) or (protected adj3 intercourse*) or risky sex*).mp. or exp sexually transmitted diseases/or exp safe sex/or exp sexual behavior/or exp HIV infections/or exp Acquired Immunodeficiency Syndrome/
-
4.
1 AND 2 AND 3
-
5.
limit 4 to yr=”1996–Current”
We downloaded search results to a reference manager and removed any duplicates. Two reviewers independently screened abstracts to agree on an initial set of records, which were then retrieved in full-text form for comparison against the inclusion and exclusion criteria. The first reviewer extracted data on analyses, sample and design from each included study. The second reviewer checked extraction.
Synthesis Methods
Due to heterogeneity in measurement and analysis approaches among included studies, we did not meta-analyse findings. We undertook post hoc appraisal of included studies and highlight key methodological features in our synthesis; studies were not appraised a priori because of lack of consensus on appraisal tools for this study type.
In our narrative synthesis, we present details of within-subjects comparisons in the studies included in this review. Within-subjects comparisons separate out the effects of encounter-level characteristics from effects of person-level characteristics on the dependent variable (here, sexual risk behaviour) using a variety of methods. Multilevel models (also known as hierarchical linear models or generalised linear mixed effects models) analyse multiple encounters per respondent by dividing variance on the dependent variable into that attributable to person-level variance and that attributable to encounter-level variance. McNemar’s test and conditional logistic regression match encounters reported by the same person that are different on the dependent variable (e.g. one encounter with UAI and one encounter without UAI) to remove person-level confounding on the dependent variable.
Furthermore, our synthesis reports within-subjects comparisons testing the relationship between location of sex and the dependent variable of sexual risk as presented in included studies. Where multivariate models were presented in included studies, we also extracted effects of covariates, and we present those as well. We did not have any a priori expectations as to how location of sex would be defined, but we were careful to ascertain that the location being discussed referred to location of sex as opposed to venue of partner meeting. We report below classifications of locations of sex as reported by, and to the level of detail available, in each included study. We defined the dependent variable of sexual risk behaviour by examining any comparison between any type of unprotected anal intercourse and another sexual behaviour. We believed a priori that this was likely to include three key types of comparisons: UAI versus any other sexual behaviour, UAI versus protected anal intercourse, and comparisons between serononconcordant UAI (i.e. UAI with a partner of unknown HIV serostatus match or of different HIV serostatus) and other types of sexual behaviour. Because we were examining sexual encounters, we presumed that the outcomes captured in included studies were likely to be binary, but we agreed to include studies examining sexual risk using other types of measures.
Results
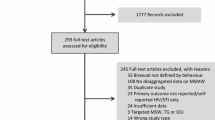
Databases searched identified 11,510 references, reduced to 6,336 records after deduplication across databases. We narrowed this on the basis of screening of title and abstract to 138 studies. At this stage, studies were set aside principally because they were not quantitative investigations, because they did not address MSM specifically, or because they did not examine sexual risk at the encounter level. We examined 138 full-text records and included six documents from six different studies [15, 23–27] (see Fig. 1).
Excluded Studies
Of the 132 studies we excluded, we set aside 101 studies that did not specifically analyse multiple encounters per respondent or location of sex, four studies that examined location of sex but not by comparing multiple events against each other within subjects, five studies that examined differences between partnerships reported by the same respondent, three studies that collected data pre-1996 (and did not report on location of sex), and 16 studies that collected multiple events per respondent but did not examine location of sex.
Three near-eligible studies were excluded from this analysis. Two studies [28, 29] used population-average statistical models. Interpretation of within-subjects comparisons is different from population-average models, including generalised estimating equations [30], in that coefficients of encounter-level characteristics in multilevel models reflect the difference between one encounter and another within the same person, whereas population-average models reflect the average difference between one encounter and another across the entire population. One study [31] tested venue of partner meeting (but not location of sex, as confirmed by contact with the author) as a covariate in within-subjects comparisons, and did not report results.
Characteristics of Included Studies and Analyses
Two studies [24, 26] collected data from Australian samples using in-person interviews (see Table 1). The four remaining studies collected data from samples in the United States with a variety of methods. Sample sizes of MSM ranged from 116 to 1,225. One study [23] focused on MSM living with HIV and one study [24] focused on HIV-seronegative MSM. Two studies [15, 25] examined only Latino populations. The earliest study began data collection in 1999. One study [15] was taken from a dissertation, while all others were published as journal articles.
Studies used multilevel models, McNemar’s test or conditional logistic regressions to compare encounters within respondents. All are standard approaches to within-subjects comparisons. Of note is that McNemar’s test and conditional logistic regressions both require at least one encounter with UAI and at least one encounter without UAI per respondent.
Appraisal of Reporting
Studies were of high quality. All studies clearly stated study hypotheses, presented theoretically and empirically driven analysis strategies, and described study samples. Mechanisms of data collection were clearly reported. Study results were described fully, including confidence intervals for all univariate results where appropriate. One study [23] reported significance, but not effect sizes, for multivariate analyses.
Categorisations of Location of Sex
Broadly, studies compared home or private locations against SOPVs, though both specific categorisations of SOPVs and specific categorisations of additional locations varied across studies. Only two studies [15, 24] used similar measurement schemes to categorise location of sex, describing locations as either being respondent’s home, partner’s home or SOPV (see Table 2). However, only one of these two studies [15] defined SOPV, specifying that this category included a bathhouse, a sex club or a sex party. All other studies categorised location of sex in different ways. One study [27] compared encounters held at the respondent’s or partner’s home with encounters held at sex clubs or bathhouses and encounters held at an ‘other’ location, described as hotel, dance club, porn theatre, video arcade or another public place (e.g. a cruising location). Confusingly, another study [26] separated encounters in bathhouses from encounters in other SOPVs, and compared these two types of encounters against encounters in the respondent’s home, in the partner’s home, in cruising locations and in other locations. Finally, one study [25] classed all encounters into ‘public’, i.e. an SOPV or a cruising location, or ‘private’, i.e. the respondent’s or partner’s home or a motel, and another study compared encounters at sex parties or bathhouses (both of which are included as SOPVs in the introduction to this review).
Categorisations of Sexual Risk
Three studies [15, 23, 24] defined sexual encounters as those that included anal intercourse, one study [27] included encounters with oral intercourse as well, and two studies [25, 26] included all sexual behaviour with a partner. Studies that defined sexual encounters as those that included anal intercourse compared unprotected anal intercourse against protected anal intercourse, and one study [23] also compared serononconcordant UAI against all other anal intercourse. Moreover, of those studies [25, 26] that included all sexual behaviour with a partner, one study [25] compared UAI against all other sexual behaviour and the other study [26] separated encounters by PAI, UAI and no anal intercourse, and estimated a multinomial logistic regression with no anal intercourse as the reference category. The final study [27] compared serononconcordant UAI against all other anal intercourse and oral intercourse.
Study Findings
Three studies [15, 23, 24] directly compared UAI against protected anal intercourse (PAI). UAI was not more likely than PAI in non-private settings (SOPVs or sex parties) in any of these univariate analyses, nor was UAI more likely than PAI in respondent’s home or partner’s home in the two studies [15, 24] that tested this category separately. These three studies covered HIV-seropositive and HIV-seronegative populations, as well as Latino MSM. While UAI and PAI encounters were not directly compared in the one study [26] that separated out UAI, PAI and encounters with no anal intercourse, inspection of the results for both multivariate analyses suggests that UAI was more likely than PAI in both SOPVs as defined in this specific study (i.e. not including bathhouses) and ‘beats’ as compared to encounters in the respondent’s home, though this evidence was indirect.
One study [25] compared UAI against all other sexual behaviour in Latino MSM. UAI was significantly more likely in private settings (23.0 % of encounters) than in public settings (14.0 %). This study also compared anal intercourse against all other sexual behaviour and found that anal intercourse was significantly more likely in private settings (80.0 %) than in public settings (55.0 %). The proportion of anal intercourse events involving UAI appeared similar in both public and private settings.
Finally, two studies tested serononconcordant UAI, or UAI with a partner of unknown or different HIV serostatus against other anal intercourse [23] or against other anal intercourse or oral intercourse [27]. Both studies found that serononconcordant UAI was positively associated with encounters in SOPVs, though in multivariate models only the effect reported by the first study [23] remained statistically significant.
Discussion
This systematic review demonstrated little evidence of differences in UAI as compared to PAI between public and private encounters, with the exception of indirect evidence from one study that did not directly compare UAI and PAI, but rather tested each against a category of ‘no anal intercourse’ [26]. However, a critical delimiter in interpreting these findings is the diversity of venue classifications and populations used in included studies.
The findings of this review contextualise and expand the findings of the person-level analyses discussed in the introduction. That is to say, one way of contrasting significant person-level associations between SOPV attendance and sexual risk behaviour [9, 10] and non-significant encounter-level associations is to note that those attending SOPVs may have greater preference for UAI generally, without specific location-related effects on sexual risk behaviour. However, this may not hold for serononconcordant UAI. SOPVs may be preferred for serononconcordant UAI or may somehow facilitate it. How SOPVs are associated with serononconcordant UAI may be linked to how sexual partners communicate in SOPVs. We discuss these interpretations further below.
However, differences between studies in interpretations are key. Specifically, distinctions between UAI and PAI reflect a more targeted comparison between two forms of sexual behaviour than analyses comparing UAI against all other sexual behaviour. These analyses may reflect the assumption that the difference between condom use and no condom use in anal intercourse is a critical ‘decision point’ informed by considerations of, for example, pleasure loss [32]. These analyses may also reflect that comparing UAI versus PAI is particularly salient for understanding risk for HIV transmission, given the perception of decreased risk under other forms of intercourse such as fellatio [33].
But because analyses that compare serononconcordant UAI against other sexual behaviour present a comparison that addresses an especially high-risk sexual practice, these analyses may be viewed as aiming to understand how risk appraisal, among other cognitive or affective processes, may be different across situational characteristics [18]. Both studies testing serononconcordant UAI as an outcome [23, 27] showed significant positive associations of this outcome with non-private settings. When viewed in context of the significant differences between settings in probability of any anal intercourse [25], the differences between non-significant findings for UAI and significant findings for serononconcordant UAI suggest that differences between settings in sexual behaviours may come in the ability to make informed decisions about the seroconcordance of partners with whom to engage in UAI, rather than in the decision to engage in UAI or PAI.
This contrast between findings also suggests that patterns of sexual behaviour related to engagement in serononconcordant UAI specifically are related to choice of location. Specifically, risk reduction practices that may make UAI less risky in sex-on-premises venues, such as serosorting (choosing partners believed to be of the same HIV serostatus) or communication around HIV disclosure [34], may be less feasible in highly stimulating sexual contexts, where, as qualitative evidence suggests [35, 36], explicit communication may be unacceptable or unwelcome. However, findings in this review were not able to shed light on other risk reduction strategies that occur in the context of possibly serononconcordant UAI, including strategic positioning (i.e. avoiding receptive UAI if HIV seronegative) or withdrawal before ejaculation [37], both of which cross-sectional evidence demonstrates may be popular at bathhouses specifically [38].
Additional research should be conducted to understand the similarity or dissimilarity of sexual risk behaviour across a range of SOPVs, and to consider the most appropriate way of measuring location of sex. Diversity of SOPVs included in different categorisations in studies included in this review made it difficult to make more specific targeted syntheses across included studies. It may also be that different types of venues may be similar in different settings. For example, while an omnibus classification of public vs private locations as used in one study [25] may have prevented clear comparison with other studies, similarly a classification system that separated bathhouses from other SOPVs without definition of the remaining SOPVs considered [26] was inconsistent with the broad comparisons used in other included studies.
Another opportunity for additional research is to consider how venue-specific sexual risk patterns can inform health promotion. While it is important to tailor setting-based health promotion to the specific contexts in which it occurs [10, 39], health promoters may wish to concentrate on person-level characteristics that are associated with risk behaviour (e.g. insufficient knowledge of safer sex practices or low self-efficacy) as opposed to encounter-level and location-level determinants. Venue-based health promotion should also take into account the different communication norms present between venues, as explicit safer sex messaging has been found to be unacceptable in qualitative [35] and quantitative [40] investigations.
An important point to consider is the degree to which the included evidence may no longer reflect current risk practices in SOPVs and cruising locations. The most recent study included in this systematic review was published in 2010. Longitudinal evidence from repeated cross-sectional surveys in Australia suggests that the advent of smartphone apps and internet sex-seeking sites have changed the prevalence and nature of use of SOPVs [41]. The percentage of MSM reporting using SOPVs to find sexual partners in the last year declined between the years 1998 and 2008, while the percentage reporting using the internet has increased to upwards of 60 % since data was first collected on this in 2001.
Given that SOPV use appears to continue at a high level in MSM, this is not to say that SOPVs are no longer important in an era of smartphone-mediated sex seeking. Rather, because SOPVs may no longer be the only venue, or the preferred venue, in which to find casual sexual partners, it is important to note how the differences between SOPV and non-SOPV encounters may have changed over time. Included studies in this systematic review did not examine interactions between person-level characteristics and choice of venue in associations with sexual risk behaviour. These ‘cross-level’ interactions are fertile ground for future research.
This review had several strengths and limitations beyond the relative ‘age’ of the included studies. One strength of this review was its focus on within-subjects comparisons. As stated in the introduction, within-subjects comparisons address person-level confounding, while single-event analyses or person-level global association studies cannot. However, in studies where repeated measures were taken over several measurement occasions (of which one was included [23]), reactivity bias may have affected the results. Included studies also did not draw on probability samples. While this may have been partially addressed by using within-subjects comparisons, it is possible that cross-level interactions between person-level characteristics and location of sex may have biased our results. Because included studies did not present validity or reliability of measurement tools, it was impossible to assess the quality of measurement. Moreover, because of the use of non-probability samples, it is likely that our results may only generalise to groups of higher-risk MSM, as past comparisons between probability samples and community-recruited samples of MSM have shown that community-recruited MSM report higher levels of risk behaviour [42, 43].
Because all studies included here were observational studies, study-level results are susceptible to the biases faced by all observational studies. Biases most salient here include recall bias (especially of specific sexual risk behaviours), social desirability bias (especially for the three studies [15, 24, 26] that used in-person interviews for data collection) and performance bias (especially when included studies queried specific encounters). Because these studies are observational, it is impossible to draw evidence of a causal effect between venue of sex and sexual risk from these studies.
At the review level, rigorous search and screening ensured that all available studies were located. However, like any review, ours may have been subject to publication or retrieval bias. Observational studies may be especially subject to publication bias reflecting the non-publication of non-significant results. However, it should be noted that our overall finding of statistical non-significance arose in spite of this, which strengthens confidence in our conclusions. We included evidence from journal articles and dissertations, the latter forming a critical part of the unpublished literature [44]. No otherwise pertinent and methodologically adequate reports were excluded because they were published in other sources. All studies came from samples recruited in Australia and the United States. While this may improve the ‘internal validity’ of our conclusions, it means that we cannot generalise these findings to MSM living in other countries. This is especially important in considering that MSM in other countries may face structural conditions that might prevent meeting sexual partners in non-SOPV contexts.
References
Smith AMA, Grierson JW, von Doussa H. Gay men’s sex venues, the men who use them, and gay community perceptions: insights from a convenience sample of gay men attending a community festival in Melbourne. Sex Health. 2010;7(2):177–81.
Frankis JS, Flowers P. Public sexual cultures: a systematic review of qualitative research investigating men’s sexual behaviors with men in public spaces. J Homosex. 2009;56(7):861–93.
The EMIS Network. EMIS 2010: the european men-who-have-sex-with-men internet survey. Stockholm: European Centre for Disease Prevention and Control; 2013.
Keogh PG, Weatherburn P. Tales from the backroom: anonymous sex and HIV risk in London’s commercial gay sex venues. Venereology. 2000;13(4):150–5.
O’Byrne P. Examining the intersection of desire, drugs and place among gay men. J Res Nurs. 2011 Sep 6;(September 2011):1–12.
Bourne A, Reid D, Hickson F, Torres Rueda S, Weatherburn P. The Chemsex Study: drug use in sexual settings among gay & bisexual men in Lambeth, Southwark, & Lewisham. London: Sigma Research, London School of Hygiene and Tropical Medicine; 2014.
Slavin S. Drugs, space, and sociality in a gay nightclub in Sydney. J Contemp Ethnogr. 2004;33(3):265–95.
O’Byrne P, Holmes D. Desire, drug use and unsafe sex: a qualitative examination of gay men who attend gay circuit parties. Cult Health Sex. 2011;13(1):1–13.
Keogh PG, Weatherburn P, Hickson F. Anonymous sex among homosexually active men: implications for HIV prevention. Venereology. 2000;13(4):143–8.
Grov C. HIV risk and substance use in men who have sex with men surveyed in bathhouses, bars/clubs, and on Craigslist.org: venue of recruitment matters. AIDS Behav. 2012;16(4):807–17.
Reidy WJ, Spielberg F, Wood R, Binson D, Woods WJ, Goldbaum GM. HIV risk associated with gay bathhouses and sex clubs: findings from 2 Seattle surveys of factors related to HIV and sexually transmitted infections. Am J Public Health. 2009;2(99):S165–72.
Thiede H, Jenkins RA, Carey JW, Hutcheson R, Thomas KK, Stall RD, et al. Determinants of recent HIV infection among Seattle-area men who have sex with men. Am J Public Health. 2009;99(Suppl 1):S157–64.
Vanden Berghe W, Nostlinger C, Buve A, Beelaert G, Fransen K, Laga M. A venue-based HIV prevalence and behavioural study among men who have sex with men in Antwerp and Ghent, Flanders, Belgium, October 2009 to March 2010. Eurosurveillance. 2011;16(28).
Leigh BC, Stall R. Substance use and risky sexual behavior for exposure to HIV: issues in methdology, interpretation, and prevention. Am Psychol. 1993;48(10):1035–45.
Wilson PA. Sexual risk-taking and drug use among Latino men: examining episodes of high-risk and low-risk sexual behavior. ProQuest Dissertations and Theses. [United States—New York]: ProQuest Information & Learning; 2004.
McKirnan DJ, Ostrow DG, Hope BY. Sex, drugs and escape: a psychological model of HIV-risk sexual behaviours. AIDS Care. 1996;8(6):655–70.
McKirnan DJ, Vanable PA, Ostrow DG, Hope B. Expectancies of sexual “escape” and sexual risk among drug and alcohol-involved gay and bisexual men. J Subst Abuse. 2001;13(1–2):137–54.
Newcomb ME, Mustanski B. Cognitive influences on sexual risk and risk appraisals in men who have sex with men. Heal Psychol. 2014;33(7):690–8.
Buckley EJ, White DG, Morris C, Elsmore M, Morrall IA, Pugh RN. The effects of community-based sexual health testing and health promotion on gay men’s sexual risk-taking behaviour. Int J Heal Promot Educ. 2010;48(4):123–8.
Wohlfeiler D, Potterat JJ. Using gay men’s sexual networks to reduce sexually transmitted disease (STD)/human immunodeficiency virus (HIV) transmission. Sex Transm Dis. 2005;32(10 Suppl):S48–52.
Bonell CP, Strange V, Allen E, Barnett-Page E. HIV prevention outreach in commercial gay venues in large cities: evaluation findings from London. Health Educ Res. 2006;21(4):452–64.
Kelly JA, Murphy DA, Sikkema KJ, McAuliffe TL, Roffman RA, Solomon LJ, et al. Randomised, controlled, community-level HIV-prevention intervention for sexual-risk behaviour among homosexual men in US cities. Lancet. 1997;350(9090):1500–5.
Wilson PA, Cook S, McGaskey J, Rowe M, Dennis N. Situational predictors of sexual risk episodes among men with HIV who have sex with men. Sex Transm Infect. 2008;84(6):506–8.
Prestage G, Van de Ven P, Grulich A, Kaldor J, Kippax S, Mao L. Contexts for last occasions of unprotected anal intercourse among HIV-negative gay men in Sydney: the health in men cohort. AIDS Care. 2005;17(1):23–32.
Reisen CA, Iracheta MA, Zea MC, Bianchi FT, Poppen PJ. Sex in public and private settings among Latino MSM. AIDS Care. 2010;22(6):697–704.
Smith AMA, Grierson J, Pitts M, Pattison P. Individual characteristics are less important than event characteristics in predicting protected and unprotected anal intercourse among homosexual and bisexual men in Melbourne. Australia Sex Transm Infect. 2006;82(6):474–7.
Colfax GN, Vittinghoff E, Husnik MJ, McKirnan D, Buchbinder S, Koblin B, et al. Substance use and sexual risk: a participant- and episode-level analysis among a cohort of men who have sex with men. Am J Epidemiol. 2004;159(10):1002–12.
Hensel DJ, Rosenberger JG, Novak DS, Reece M. Sexual event-level characteristics of condom use during anal intercourse among HIV-negative men who have sex with men. Sex Transm Dis. 2012;39(7):550–5.
Colfax GN, Mansergh G, Guzman R, Vittinghoff E, Marks G, Rader M, et al. Drug use and sexual risk behavior among gay and bisexual men who attend circuit parties: a venue-based comparison. J Acquir Immune Defic Syndr. 2001;28(4):373–9.
Hu FB, Goldberg J, Hedeker D, Flay BR, Pentz MA. Comparison of population-averaged and subject-specific approaches for analyzing repeated binary outcomes. Am J Epidemiol. 1998;147(7):694–703.
Koblin BA, Murrill C, Camacho M, Xu G, Liu K-L, Raj-Singh S, et al. Amphetamine use and sexual risk among men who have sex with men: results from the National HIV behavioral surveillance study—New York City. Subst Use Misuse. 2007;42(10):1613–28.
Calabrese SK, Reisen CA, Zea MC, Poppen PJ, Bianchi FT. The pleasure principle: the effect of perceived pleasure loss associated with condoms on unprotected anal intercourse among immigrant latino men who have sex with men. AIDS Patient Care STDs. 2012;26(7):430–5.
Mitchell J. HIV-negative and hiv-discordant gay male couples’ use of HIV risk-reduction strategies: differences by partner type and couples’ HIV-status. AIDS Behav. 2013;17(4):1557–69.
McDaid LM, Hart GJ. Serosorting and strategic positioning during unprotected anal intercourse: are risk reduction strategies being employed by gay and bisexual men in Scotland? Sex Transm Dis. 2012;39(9):735–8.
Mimiaga MJ, Reisner SL, Bland S, Cranston K, Isenberg D, Driscoll MA, et al. “It”s a quick way to get what you want’: a formative exploration of HIV risk among urban Massachusetts men who have sex with men who attend sex parties. AIDS Patient Care STDs. 2010;24(10):659–74.
Richters J. Through a hole in a wall: setting and interaction in sex-on-premises venues. Sexualities. 2007;10(3):275–97.
Jin F, Crawford J, Prestage GP, Zablotska I, Imrie J, Kippax SC, et al. Unprotected anal intercourse, risk reduction behaviours, and subsequent HIV infection in a cohort of homosexual men. AIDS. 2009;23(2):243–52.
Binson D, Pollack LM, Blair J, Woods WJ. HIV transmission risk at a gay bathhouse. J Sex Res. 2010;47(6):580–8.
Grov C, Hirshfield S, Remien RH, Humberstone M, Chiasson MA. Exploring the venue’s role in risky sexual behavior among gay and bisexual men: an event-level analysis from a national online survey in the U.S. Arch Sex Behav. 2013;42(2):291–302.
Grov C, Cruz J, Parsons JT. Men who have sex with men’s attitudes toward using color-coded wristbands to facilitate sexual communication at sex parties. Sex Res Soc Policy. 2014;11:11–9.
Zablotska IB, Holt M, Prestage G. Changes in gay men’s participation in gay community life: implications for HIV surveillance and research. 2012. p. 669–75.
Dodds JP, Mercer CH, Mercey DE, Copas AJ, Johnson AM. Men who have sex with men: a comparison of a probability sample survey and a community based study. Sex Transm Infect. 2006;82(1):86–7.
Burt RD, Oster AM, Golden MR, Thiede H. Comparing study populations of men who have sex with men: evaluating consistency within repeat studies and across studies in the Seattle area using different recruitment methodologies [Internet]. Suppl. 2014;3:370–81.
Lefebvre C, Manheimer E, Glanville J. Chapter 6: searching for studies. Cochrane Handb Syst Rev Interv Version. 2008;5(1):1–46.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Melendez-Torres, G.J., Nye, E. & Bonell, C. Is Location of Sex Associated with Sexual Risk Behaviour in Men Who Have Sex with Men? Systematic Review of Within-Subjects Studies. AIDS Behav 20, 1219–1227 (2016). https://doi.org/10.1007/s10461-015-1093-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-015-1093-z