Abstract
Intimate partner violence (IPV) is associated with risky sexual behavior and STIs among diverse groups of women. IPV was examined as a moderator of efficacy for an HIV/STI intervention. 848 African American women, 18–29, were randomly assigned to an HIV/STI intervention or control condition. Participants completed measures on sociodemographics, IPV, risky sexual behavior and received STI testing. IPV predicted inconsistent condom use and a risky sexual partner over 12-month follow-up. A significant interaction indicated that among women who experienced IPV, those in the intervention were more likely to test positive for Trichomonas vaginalis (TV). Among intervention participants, those who experienced IPV were more likely to test TV-positive than those who did not. In an HIV intervention that did not specifically address IPV, women in the control condition were less likely to acquire TV than those in the intervention. Consideration of contextual/interpersonal factors is essential when developing HIV intervention programs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
African Americans are disproportionately impacted by HIV and other sexually transmitted infections (STIs). Racial disparities persist on STI acquisition among African Americans. In particular, rates of Gonorrhea and Chlamydia are 11 and 6 times as high, respectively, among African American women than their white counterparts [1]. Additionally, in national HIV/AIDS surveillance data, HIV diagnoses among African American women accounted for the largest proportion of HIV diagnoses among women, and HIV rates among African American women have been found to be 20 times as high as that of white women [2]. Furthermore, 44 % of all new HIV infections in 2010 were among African Americans. Among African American women, the largest percentage of new infections was among young women 13–24 years old (23 %) and 25–34 years old (30 %) [2]. Sexual risk-reduction interventions and a comprehensive understanding of risk factors associated with sexual risk behavior are critical to abating the risk of HIV/STIs in this population.
An emerging and intersecting health concern is that women who experience intimate partner violence (IPV), defined as “physical, sexual, or psychological harm by a current or former partner or spouse” [3], may be unable to practice appropriate measures to prevent contracting HIV/STIs. IPV is considered a serious public health concern and is associated with adverse health outcomes, including poor physical, psychological, and sexual health [4–9] as well as overall healthcare costs [10]. Although IPV affects a large proportion of women, the occurrence of IPV is not uniform across groups. African American women have reported experiencing IPV at a rate 35 % higher than Caucasian women, and they were 2.5 times as likely to experience IPV relative to women from other racial/ethnic groups [11].
Previous studies have shown that IPV increases the likelihood of engaging in risky sexual behavior, increasing STI-risk [5–9, 12]. It seems that IPV is not only an immediate threat to women’s health but may also thwart the use of protective sexual health behaviors that prevent disease acquisition. For example, African American women who have reported IPV are more likely to report inconsistent condom use or using condoms less frequently [7, 12], abuse due to condom negotiation [12], multiple and risky sexual partners [7, 13], early age of first sex [13], and having an STI [7, 8]. These findings highlight the public health importance of understanding the implications of IPV on HIV/STI prevention, particularly among young women who are disproportionately more likely to contract HIV/STIs.
While many risk-reduction interventions target important skills, including condom use skills and negotiation, condom negotiation may increase fear of experiencing IPV, particularly among women who have experienced IPV in their relationships [12, 14]. This, in turn, may interfere with a young woman’s ability to enact safer sex practices and thereby heighten her risk for STIs. Furthermore, among young African American women, contextual and structural factors such as the imbalanced male-to-female ratio that supports concurrent partnering, competition for male partners, and reduced relationship power may also negatively influence sexual communication between African American women and men [15, 16], thereby increasing their risk for infection. An increasing number of effective HIV/STI sexual risk-reduction interventions that have reduced HIV-risk behavior and STIs have been developed for African American women [17–19]. A review of randomized controlled trials found that the more effective programs have been theory-driven, emphasized gender-related influences, and utilized multiple sessions to promote condom use during sexual intercourse [19]. However, currently, there do not seem to be published effective or efficacious HIV/STI prevention interventions geared towards also reducing IPV for high-risk young African American women [5, 19].
Given that HIV/STIs disproportionately affect young African American women, it is pertinent to examine factors, such as IPV, that can potentially impact risky sexual behaviors and STI acquisition. In an effort to support the importance of incorporating IPV in HIV/STI prevention interventions [5, 19, 20], the present study examined the moderating role of IPV on the efficacy of an HIV/STI risk reduction intervention to reduce sexual risk behaviors and STI infection longitudinally over a 12-month follow-up period. The main intervention trial found that women in the intervention condition were less likely to have nonviral incident STIs, incident high-risk HPV infection, and concurrent male sex partners. They also were less likely to report multiple male sex partners and more likely to use condoms during oral sex [21]. Therefore, the purpose of the present study is two-fold: (1) to provide a better understanding of the longitudinal, negative impact of IPV on sexual risk behavior and STI acquisition among women who are participating in an HIV/STI intervention and (2) to determine whether IPV moderates the relationship between HIV intervention condition, sexual risk behavior, and STIs.
Methods
Participants
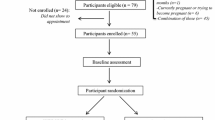
Participants were part of a larger HIV intervention trial tailored for African American women [21]. From October 2002 through March 2006, 9393 members from three Kaiser Permanente Centers having the greatest number of African Americans in Atlanta, GA, were randomly selected using the Kaiser subscriber database. Eligibility criteria included being an African American woman, 18–29 years, unmarried, sexually active in the prior 6 months, and providing written and verbal informed consent. Of these members, 979 (21.8 %) met all eligibility criteria. All 979 eligible women were invited to participate and 848 (86.6 %) completed baseline assessments and were randomized to study conditions. Of the 605 participants allocated to the HIV intervention condition, 441 (72.9 %) completed the 6-month assessment and 452 (74.7 %) completed the 12-month assessment. Of the 243 participants allocated to the comparison, 194 (79.8 %) completed the 6-month assessment and 183 (75.3 %) completed the 12-month assessment. No differences were observed between conditions with participants retained and lost to follow-up at the 6-month assessment (27.10 % [n = 441] vs. 20.20 % [n = 194]) or 12-month assessment (25.30 % [n = 452] vs. 24.7 % [n = 183]). Participants were compensated for travel and child care to attend each intervention session and complete behavioral and biological assessments. The Emory University Institutional Review Board approved the study protocol prior to implementation.
Intervention Methods [21]
The HIV/STI intervention consisted of two 4-hour group sessions, with an average of 10 participants per session, and was facilitated by two trained African American female health educators. The general health promotion (control) condition consisted of one 4-hour group session that emphasized nutrition and exercise. The HIV intervention was informed by CDC-defined evidence-based HIV interventions developed by the study team and applied complementary theoretical frameworks to guide program activities. Social cognitive theory [22] informed HIV intervention content by seeking to enhance participants’ attitudes and skills in abstaining from sexual intercourse, practicing low-risk sexual behaviors (i.e. outercourse), avoiding untreated STIs, using condoms consistently, and refraining from having multiple and concurrent sexual partners. Content regarding avoiding concurrency emphasized valuing one’s body, perceiving one’s body as a temple (a culturally appropriate connotation), informing participants of the heightened risk of STIs, including HIV, when women engage in concurrency, and discussing partner selection strategies that encouraged monogamy (for both the female participant and their male sexual partners).
HIV intervention content was also informed by the theory of gender and power [23], which examines economic forces, power imbalances, gender-related factors, and biological influences affecting women’s HIV risk. Theoretically informed content sought to enhance women’s awareness of power imbalances, such as relationships that threaten their safety, and by teaching women about economic forces which may reduce their self-sufficiency, such as dating male partners who desire pregnancy. The theory informed intervention content by educating participants about gender-related HIV prevention strategies, such as refraining from vaginal douching and enhancing sexual communication and by educating women about biological influences which could reduce HIV risk, such as encouraging participants to have their male sexual partners seek STI testing and treatment, if necessary. HIV prevention strategies were equally emphasized and the benefits of adopting multiple strategies were discussed.
Data Collection
Data collection occurred at baseline and at 6- and 12-month follow-up. At each assessment, participants completed a 40-minute audio computer assisted survey interview (ACASI) assessing sociodemographics, psychosocial factors associated with HIV/STI risk behaviors, and sexual risk behaviors. Subsequently, participants provided two vaginal swab specimens to be tested for STIs.
Measures
Intimate Partner Violence
Lifetime IPV was assessed by asking participants 3 questions: whether any male sexual partner had ever made them have vaginal and/or anal sex when they did not want to, physically abused them (i.e., punched, kicked, slapped, pushed, yanked your hair, or physically hurt you), or verbally abused them (i.e., threatened you, called you names, or swore at you). Male sexual partner was defined as a partner with whom the participant had a sexual relationship or someone with whom the participant had a special or committed relationship.
Self-Reported Sexual Behaviors
Participants reported whether they engaged in consistent condom use during the past 6 months. Consistent condom use was defined as the use of a condom during every episode of vaginal intercourse during the past 6 months and was calculated as the ratio of the number of times participants used a condom to the number of vaginal sex episodes reported during the past 6 months. A ratio of 1.00 indicated consistent condom use. Participants also reported their number of sexual partners during the past 12 months. Finally, the survey assessed whether in the past 6 months participants had engaged in vaginal sex with a man who had recently been released from jail, had an STI, used injection drugs, and/or had a concurrent sexual partner. Reporting yes to any of these items constituted having a risky sexual partner. All self-reported sexual behaviors were examined over the 12-month follow-up period.
Sexually Transmitted Infections
Acquiring an incident STI was defined as a positive laboratory test result for a new Chlamydia, Gonorrhea, or Trichomonas infection at the baseline, 6-month, or 12-month assessments. Participants provided 2 vaginal swabs at each of the 3 assessments. One swab was evaluated for Neisseria gonorrhoeae (GC) and Chlamydia trachomatis (CT) using the Becton–Dickinson ProbeTec ET Chlamydia trachomatis and Neisseria gonorrhoeae Amplified DNA Assay (Sparks, MD). A second vaginal swab was tested for Trichomonas vaginalis (TV) using Taq-Man PCR. The Caliendo Laboratory developed and validated this test which employs a homogenous kinetic PCR to amplify and detect a conserved part of a repeated DNA fragment of TV. All assays were conducted at the Emory University, Department of Pathology, Caliendo Research Laboratory. Women testing positive were provided directly observable single-dose treatment, received risk-reduction counseling per CDC recommendations, and were encouraged to refer sex partners for treatment. The county health department was notified of reportable STIs.
Data Analyses
Descriptive statistics assessed the prevalence of sociodemographics, IPV, sexual behavior, and STIs. IPV was dichotomized into women who reported ever experiencing IPV versus those who did not at baseline. Binary generalized estimating equations (GEE) models were conducted to control for repeated within-subject measurements and allow for a number of observations on participants longitudinally. GEE models assessed the impact of IPV at baseline and interaction effects between HIV/STI intervention group and IPV at baseline on risky sexual behavior and STIs over the 12-month follow-up period. Posthoc pairwise comparisons were conducted in GEE to examine and interpret the significant interactions further. Age and baseline outcome measures were included as covariates. Analyses were conducted in SPSS, v. 18.
Population-averaged (PA) models were used over subject-specific (SS) models due to the preference of the PA interpretation of similar coefficients. For a binary model, the SS interpretation of the coefficient on IPV is the change in likelihood of the outcome when that individual experiences their first IPV. However, for these analyses, the purpose was to discuss the PA interpretation, which is the difference in the likelihood for the average non-IPV versus average IPV person. Since implementation decisions are generally reached through consideration of the intervention’s effectiveness for populations, the PA approach was preferred.
Results
Participant Characteristics
At baseline, 424 (50 %) of the women endorsed ever experiencing IPV by a male sexual partner. There were no differences in experiences of IPV between the intervention (52.1 %) and control (49 %) conditions at baseline. Participants’ average age was 22.04 (SD = 3.61) years. The majority of women reported completing 1–4 years of college (59.3 %), with 25.6 % graduating from high school, 11.2 % completing some high school (9–11th grade), and 3.9 % having graduate school training. In terms of their living situation, 53.5 % reported living with parent(s), 20.2 % living alone, 12.4 % living with a roommate, 5.2 % living with their boyfriend, 5.4 % living with another relative, and 3.3 % living with their children. Additionally, the majority of women obtained their spending money from their job (65.4 %). Participant characteristics on the outcome variables at baseline, 6- and 12-month follow-up are displayed in Table 1.
Binary GEE Models and Posthoc Pairwise Comparisons
After controlling for age and baseline outcome measures, GEE models revealed that women who reported ever experiencing IPV, relative to those who did not, were more likely to report inconsistent condom use during the past 6 months (72.6 % vs. 62.8 %, p = .04) and having a risky sexual partner during the past 6 months (27.8 % vs. 18.5 %, p = .01) over the 12-month follow-up period. A significant interaction between IPV and study condition on testing positive for Trichomonas vaginalis (TV) also was found (p = .04) (Table 2). As shown in Fig. 1, posthoc pairwise comparisons indicated that among women who did not experience any IPV, those in the control condition were more likely to test positive for TV than those in the intervention condition over the 12-month follow-up period (3.8 % vs. 1.2 %, p = .05). However, among women who reported experiencing IPV, those in the intervention condition were more likely to test positive for TV than those in the control condition over the 12-month follow-up period (3.5 % vs. 1.8 %, p = .05). Finally, among women who received the intervention, those who experienced IPV were more likely to test positive for TV than those who did not experience IPV (3.5 % vs. 1.2 %, p = .05). Due to the small number of women testing positive for Gonorrhea (see Table 1), an interaction effect was not examined. Also, there was not a significant interaction between IPV and study condition on inconsistent condom use, having a risky sexual partner, testing positive for Chlamydia, or testing positive for any STI (Table 2).
Discussion
A common component of many HIV/STI intervention programs for women is to improve their communication and negotiation skills regarding condom use [19, 24, 25]. However, if women are in an abusive relationship, they may not have the ability to utilize these skills in their relationship due to fear of abuse [6, 26]. In this sample of young adult African American women, 50 % reported ever experiencing IPV. Previous studies have reported a wide range of lifetime IPV prevalence rates, from 29 to 52 % among African American female adolescents and women [26–28]. The women in the present study were highly educated and the majority had completed 1–4 years of college. However, the high prevalence of reported IPV is noteworthy and indicates a potentially high-risk sample of women in the present study. The findings from the current study indicated that lifetime IPV was associated with inconsistent condom use and having a risky sexual partner, which corroborates previous findings indicating that IPV is associated with HIV/STI risk behaviors and STI infection [5, 7, 8, 12, 20]. Additionally, to our knowledge, this is the first study to examine the impact of IPV on HIV/STI intervention efficacy in predicting TV infection among young adult African American women.
Interestingly, among women who experienced IPV, the findings were less expected, as those in the intervention condition were more likely to test positive for TV than those in the control condition. For women who did not experience IPV, the HIV/STI intervention led to expected results, in that women were less likely to test positive for TV if they received the intervention. Additionally, within the intervention condition, those who experienced IPV were more likely to test positive for TV than those who did not experience IPV. The results from the main intervention paper found that participants in the intervention condition were 38 % less likely to have a nonviral STI over the 12-month follow-up period [21]. Therefore, these findings indicate that IPV may hinder the use of safe sex practices that prevent disease acquisition. It is possible that although women with IPV histories in the intervention condition may have learned useful skills, these skills may not have been beneficial given the context in which they were applied. For example, women may be fearful that condom negotiation may lead to abuse from their partner [26] and young women may perceive that utilizing these skills may place their relationship at risk. If they experience abuse, then they may be less likely to request or use condoms, leading to riskier behavior and ultimately STI acquisition [7, 29, 30]. Additionally, although the interaction between IPV and HIV/STI intervention condition on the likelihood of reporting a risky sexual partner was not significant (p = .07), the trend of the interaction was similar to the interaction effect for testing positive for TV (in all cases of the aforementioned significant interaction effect). Women reporting a risky sexual partner (i.e., a partner who had recently been released from jail, had an STI, used injection drugs, and/or had a concurrent sexual partner), may have been at higher risk for contracting an STI, despite being enrolled in an HIV risk-reduction intervention. Finally, women who experienced IPV were more likely to use condoms inconsistently and have risky sexual partners, placing them at further risk for STI infection.
There were no significant interaction effects found when examining Chlamydia or a combined variable, “any STI.” A national survey found that African Americans were more likely to be infected with TV than women from other racial/ethnic groups [31]. Although women were treated for STIs at each assessment, previous research has indicated that the reinfection rate for TV may be high, especially given that it is not a reportable STI infection, in contrast to the other bacterial STIs such as Chlamydia and gonorrhea, partner treatment is low [32, 33], and often men are asymptomatic [34]. Additionally, it is possible that the women were asymptomatic [35] and the infection was not detected or treated at 6-month follow-up but was detected at 12-month follow-up [36]. However, it is difficult to determine why these differences existed in the present study without further information on the male sexual partner and his STI history. The finding for TV is clinically significant, as previous research has indicated that TV increases both HIV transmission and acquisition among women, particularly African American women [37]. Findings from the significant main and interaction effects suggest that for a particular group of women, certain core skills that are taught in HIV/STI prevention interventions may not be beneficial for women who potentially lack control in their relationships. In contrast, it potentially could place women at increased risk of engaging in sexual risk behavior and contracting an STI.
Although the current intervention was based on principles from social cognitive theory [22] and the theory of gender and power [23], it seems that HIV/STI interventions for women who have experienced IPV should go beyond improving skills in self-efficacy and female empowerment. Assisting young women who are disproportionately more likely to contract HIV/STIs avoid or terminate abusive sexual partnerships may be an essential element to reducing their risk of infection. Due to potential psychological barriers or fear of abuse, it may be beneficial for HIV/STI prevention interventions to be tailored for women with previous or current experiences of IPV [38]. This could involve inclusion of components on IPV, addressing healthy and unhealthy relationships, and providing specific guidelines on effective condom negotiation and overall safer sex practices for women who may fear abuse from their male sexual partner. There could potentially be two tiers of interventions designed for women—one for women without abuse histories and one for women with abuse histories. The women who have previous or current experiences of IPV could complete a more intensive HIV/STI intervention that would also address IPV reduction. Another potential strategy would be to merge social and community-level interventions for IPV with HIV preventive efforts. For example, it could be beneficial to collaborate with healthcare settings, specifically emergency rooms and domestic violence services. In general, clinicians and practitioners should be trained in how to recognize IPV and its role in negative health outcomes in order to promote more structural and community-level changes.
There were limitations to this study. A crude measure of IPV was utilized, which did not include information regarding the frequency, duration or severity of abuse. Additionally, the IPV measure assessed lifetime IPV and did not assess recent abuse or abuse over a definitive time period. It is difficult to determine whether the findings would be different among women who reported proximal IPV versus distal IPV. Constructs, such as fear of abuse, power dynamics, relational context, and other relational variables associated with aspects of IPV were not assessed. Moreover, the data on IPV and sexual behaviors rely on retrospective self-report data. Participants may have had difficulty recalling important information, and/or they provided socially desirable responses to the sensitive questions (e.g., women may have underreported experiences of IPV). However, it is noteworthy that STI results were biologically confirmed and not based on self-report. Finally, the sample was homogeneous. Thus, the results may have limited generalizability, and replication with diverse ethnic and geographic populations would be needed.
Given that HIV risk-reduction interventions primarily target increasing women’s skills at partner communication, including condom use negotiation, IPV may decrease the use of safe sex practices that prevent disease acquisition. However, an HIV intervention that does not focus on IPV specifically may limit women who experience IPV from enacting safer sex practices. These findings underscore the importance of considering contextual factors when developing HIV intervention programs. It is necessary to take into account the complexities around addressing IPV and to ensure that it does not lead to adverse consequences for women when utilizing skills that they have learned. Additionally, it is important to consider social determinants of health. Any social and/or cultural norms that promote IPV should be challenged, and sociodemographic, community-level, and other contextual or structural factors contributing to IPV should be considered when developing HIV/STI prevention programs for young adult African American women [16, 29]. Finally, from a public health standpoint, it is necessary to address the potential for scaling up such interventions to increase the impact among large groups of women and communities.
References
Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2012 Atlanta, GA: United States Department of Health and Human Services; 2014 [October 07, 2014]. Available from: http://www.cdc.gov/std/stats12/surv2012.pdf.
Centers for Disease Control and Prevention. Estimated HIV incidence in the United States, 2007–2010 2012 [September 23, 2014]. Available from: http://www.cdc.gov/hiv/pdf/statistics_hssr_vol_17_no_4.pdf.
Centers for Disease Control and Prevention. Definition of intimate partner violence 2009 [cited 2009 March 17]. Available from: http://www.cdc.gov/ViolencePrevention/intimatepartnerviolence/definitions.html.
Edwards VJ, Black MC, Dhingra S, McKnight-Elly L, Perry GS. Physical and sexual intimate partner violence and reported serious psychological distress in the 2007 BRFSS. Int J Public Health. 2009;54:S37–42.
Gielen AC, Ghandour RM, Burke JG, Mahoney P, McDonnell KA, O’Campo P. HIV/AIDS and intimate partner violence: intersecting women’s health issues in the United States. Trauma Viol Abuse. 2007;8:178–98.
Lichtenstein B. Domestic violence, sexual ownership, and HIV risk in women in the American deep south. Soc Sci Med. 2005;60:701–14.
Seth P, Raiford JL, Robinson L, Wingood GM. Intimate partner violence and other partner-related factors: correlates of sexually transmissible infections and risky sexual behaviours among young adult African American women. Sex Health. 2010;7:25–30.
Wingood GM, Seth P, DiClemente RJ, Robinson LS. Association of sexual abuse with incident high-risk human papillomavirus infection among young African American women. Sex Transm Dis. 2009;36:784–6.
Wu E, El-Bassel N, Witte SS, Gilbert L, Chang M. Intimate partner violence and HIV risk among urban minority women in primary health care settings. AIDS Behav. 2003;7:291–301.
Centers for Disease Control and Prevention. Costs of intimate partner violence against women in the United States. Atlanta: CDC, National Center for Injury Prevention and Control; 2003.
Rennison CM, Welchans S. Intimate partner violence. Washington: U.S. Department of Justice, Bureau of Justice Statistics; 2000.
Wingood GM, DiClemente RJ. The effects of an abusive primary partner on the condom use and sexual negotiation practices of African-American women. Am J Public Health. 1997;87:1016–8.
Fuentes CMM. Pathways from interpersonal violence to sexually transmitted infections: a mixed-method study of diverse women. J Womens Health. 2008;17:1591–603.
Swan H, O’Connell DJ. The impact of intimate partner violence on women’s condom negotiation efficacy. J Interpers Violence. 2012;27:775–92.
Adimora AA, Schoenbach VJ, Doherty IA. HIV and African Americans in the southern United States: sexual networks and social context. Sex Transm Dis. 2006;33(Suppl 7):S39–46.
Raiford JL, Seth P, Braxton ND, DiClemente RJ. Interpersonal- and community-level predictors of intimate partner violence perpetration among African American men. J Urban Health. 2013;90:784–95.
Darbes L, Crepaz N, Lyles C, Kennedy G, Rutherford G. The efficacy of behavioral interventions in reducing HIV risk behaviors and incident sexually transmitted diseases in heterosexual African Americans. AIDS. 2008;22:1177–94.
Weir BW, Bard RS, O’Brien K, Casciato CJ, Stark MJ. Violence against women with HIV risk and recent criminal justice system involvement: prevalence, correlates, and recommendations for intervention. Violence Against Women. 2008;14:944–60.
Wingood GM, DiClemente R. HIV sexual risk reduction interventions for women: a review. Am J Prev Med. 1996;12:209–17.
Weir BW, O’Brien K, Bard RS, Casciato CJ, Maher JE, Dent CW, et al. Reducing HIV and partner violence risk among women with criminal justice system involvement: a randomized controlled trial of two motivational interviewing-based interventions. AIDS Behav. 2009;13:509–22.
Wingood GM, DiClemente RJ, Simpson-Robinson L, Lang DL, Caliendo A, Hardin JW. Efficacy of a trial in reducing incident high-risk HPV, non-viral STIs, and concurrency among African-American women. J Acquir Immune Defic Syndr. 2013;63:S36–43.
Bandura A. Social cognitive theory and exercise of control over HIV infection. In: DiClemente RJ, Peterson JL, editors. Preventing AIDS: theories and methods of behavioral interventions. New York: Plenum Publishing Corp.; 1994. p. 25–59.
Wingood GM, DiClemente RJ. Application of the theory of gender and power to examine HIV-related exposures, risk factors, and effective interventions for women. Health Educ Behav. 2000;27:539–65.
Wingood GM, DiClemente RJ, Harrington KF, Lang DL, Davies SL, Hook EW, et al. Efficacy of an HIV prevention program among female adolescents experiencing gender-based violence. Am J Public Health. 2006;96:1085–90.
Melendez RM, Hoffman S, Exner T, Leu CS, Ehrhardt AA. Intimate partner violence and safer sex negotiation: effects of a gender-specific intervention. Arch Sex Behav. 2003;32:499–511.
Raiford JL, DiClemente RJ, Wingood GM. Effects of fear of abuse and possible STI acquisition on the sexual behavior of young African American women. Am J Public Health. 2009;99:1067–71.
Tjaden P, Thoennes N. Full report of the prevalence, incidence, and consequences of violence against women: Findings from the National Violence Against Women Survey. Washington (DC): Department of Justice (US); 2000 [cited 2007 May 15]. Available from: www.ncjrs.org/txtfiles1/nij/183781.txt.
Breiding MJ, Black MC, Ryan GW. Prevalence and risk factors of intimate partner violence in eighteen U.S. states/territories, 2005. Am J Prev Med. 2008;34:112–8.
Raiford JL, Seth P, DiClemente RJ. What girls won’t do for love: human immunodeficiency virus/sexually transmitted infections risk among young African-American women driven by a relationship imperative. J Adolesc Health. 2013;52:566–71.
Seth P, DiClemente RJ, Lovvorn AE. State of the evidence: intimate partner violence and HIV/STI risk among adolescents. Curr HIV Res. 2014;11:528–35.
Sutton M, Sternberg M, Koumans EH, McQuillan G, Berman S, Markowitz L. The prevalence of Trichomonas vaginalis infection among reproductive-age women in the United States, 2001–2004. Clin Infect Dis. 2007;45:1319–26.
Van Der Pol B, Williams JA, Orr DP, Batteiger BE, Fortenberry JD. Prevalence, incidence, natural history, and response to treatment of Trichomonas vaginalis infection among adolescent women. J Infect Dis. 2005;192:2039–44.
Swartzendruber A, Sales JM, Brown JL, Diclemente RJ, Rose ES. Correlates of incident Trichomonas vaginalis infections among African American female adolescents. Sex Transm Dis. 2014;41:240–5.
Schwebke JR, Desmond RA. A randomized controlled trial of partner notification methods for prevention of trichomoniasis in women. Sex Transm Dis. 2010;37:392–6.
Peterman TA, Tian LH, Metcalf CA, Malotte CK, Paul SM, Douglas JM, et al. Persistent, Undetected Trichomonas vaginalis Infections? Clin Infect Dis. 2009;48:259–60.
Seth P, Sales JM, DiClemente RJ, Wingood GM, Rose ES, Patel SN. Longitudinal examination of alcohol use: a predictor of risky sexual behavior and Trichomonas vaginalis among African-American female adolescents. Sex Transm Dis. 2011;38:96–101.
Kissinger P, Adamski A. Trichomoniasis and HIV interactions: a review. Sex Transm Infect. 2013;89:426–33.
Wyatt GE, Hamilton AB, Myers HF, Ullman JB, Chin D, Sumner LA, et al. Violence prevention among HIV-positive women with histories of violence: healing women in their communities. Womens Health Issues. 2011;21:S255–60.
Acknowledgments
This study was supported by Grant R01-MH062717 from the National Institutes of Health awarded to Dr. Gina Wingood. The authors also would like to acknowledge the statistical consultation from Dr. James Hardin of the University of South Carolina.
CDC Disclaimer
The findings and conclusions in this paper are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Seth, P., Wingood, G.M., Robinson, L.S. et al. Abuse Impedes Prevention: The Intersection of Intimate Partner Violence and HIV/STI Risk Among Young African American Women. AIDS Behav 19, 1438–1445 (2015). https://doi.org/10.1007/s10461-014-0940-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-014-0940-7